Abstract
Recent reports have shown a strong association between obesity and the severity of COVID-19 infection, even in the absence of other comorbidities. After infecting the host cells, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may cause a hyperinflammatory reaction through the excessive release of cytokines, a condition known as “cytokine storm,” while inducing lymphopenia and a disrupted immune response. Obesity is associated with chronic low-grade inflammation and immune dysregulation, but the exact mechanisms through which it exacerbates COVID-19 infection are not fully clarified. The production of increased amounts of cytokines such as TNFα, IL-1, IL-6, and monocyte chemoattractant protein (MCP-1) lead to oxidative stress and defective function of innate and adaptive immunity, whereas the activation of NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome seems to play a crucial role in the pathogenesis of the infection. Endothelial dysfunction and arterial stiffness could favor the recently discovered infection of the endothelium by SARS-CoV-2, whereas alterations in cardiac structure and function and the prothrombotic microenvironment in obesity could provide a link for the increased cardiovascular events in these patients. The successful use of anti-inflammatory agents such as IL-1 and IL-6 blockers in similar hyperinflammatory settings, like that of rheumatoid arthritis, has triggered the discussion of whether such agents could be administrated in selected patients with COVID-19 disease.
Keywords: arterial stiffness, COVID-19, cytokines, immune system, obesity
INTRODUCTION
Obesity has long been associated with worse prognosis of viral infections (30). Higher mortality rates and a prolonged, more severe clinical course was observed in obese people in the 1957–1960 “Asian” and the 1968 “Hong Kong” influenzas (22, 39), whereas more recently obesity was recognized as a predisposing factor for worse clinical outcomes and death in the 2009 H1N1 pandemic. In accordance with these previous results, recent reports have demonstrated a strong association of worse clinical outcomes in COVID-19 disease with obesity, even in the absence of any other comorbidity. In a study in a single French center, obesity [body mass index (BMI) > 30 kg/m2] and severe obesity (BMI > 35 kg/m2) were present in 47.6% and 28.2% of severe cases, respectively, whereas the need for interventional mechanical ventilation (IMV) increased with BMI categories independently of age, diabetes, and hypertension (31). Petrilli et al. (25) showed that among other factors, BMI > 40 kg/m2 was a strong hospitalization risk factor, with an odds ratio (OR) of 6.2 in an academic health system in New York City. In a retrospective study by Lighter et al. (17), patients aged under 60 yr with a BMI of 30–34 kg/m2 were two and 1.8 times more likely to be admitted to acute and critical care, respectively, compared with individuals with BMI <30 kg/m2, with the risk escalating for BMI >35 kg/m2 (2.2 and 3.6 times, respectively). The unfavorable effects of obesity in the course of viral infections have been attributed to the metabolic derangement and chronic inflammation of the adipose tissue depots leading to blunted macrophage activation and impaired T and B lymphocyte responses. However, whether these mechanisms apply to the novel coronavirus infection remains unclear. In this review, we briefly present the pathophysiology of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. We then discuss the possible mechanisms through which the metabolic and immune derangement in obesity can lead to more severe clinical outcomes, with their understanding being necessary in the search for novel treatment targets in the future.
PROCESS OF VIRAL INFECTION
SARS-CoV-2 consists of four different types of structural proteins: spike (S), nucleocapsid (N), membrane (M), and envelope (E) proteins. The entry into host cells is mediated by the S protein, which comprises two separate subunits: S1 subunit, responsible for binding to the host cell receptor, and S2 subunit, responsible for the fusion between viral and cellular membranes. The cellular receptor for the virus is the angiotensin-converting enzyme 2 (ACE2), which is expressed in type I and type II alveolar epithelial cells in the lungs as well as in many other tissues such as the heart, the endothelium, the kidneys, and the pancreas (23). After binding, serine proteases such as TMPRSS2 mediate the cleavage of the spike, and then proteases such as furin release the spike fusion peptide and facilitate viral entry into the cells through endosomes. The infection results in increased cell apoptosis, which triggers the activation of proinflammatory cytokines and chemokines and the recruitment of inflammatory cells. On the other hand, the virus itself causes increased apoptosis of lymphocytes (CD3, CD4, and CD8 T cells), and the subsequent lymphocytopenia and impaired function of lymphocytes ends up in a fulminant hypercytokinemia known as “cytokine storm” (40). This condition resembles secondary hemophagocytic lymphohistiocytosis (sHLH) or macrophage activation syndrome (MAS), a common finding in severe viral infections and sepsis, which is characterized by excessive circulating levels of IL-6, IL-2, IL-7, TNFα, CXC-chemokine ligand 10 (CXCL10), monocyte chemoattractant protein-1 (MCP-1), macrophage inflammatory protein-1α (MIP1α), and other proinflammatory molecules, and is associated with progression to acute respiratory distress syndrome (ARDS) and multiorgan failure (21).
OBESITY AS A RISK FACTOR FOR COVID-19: POSSIBLE MECHANISMS
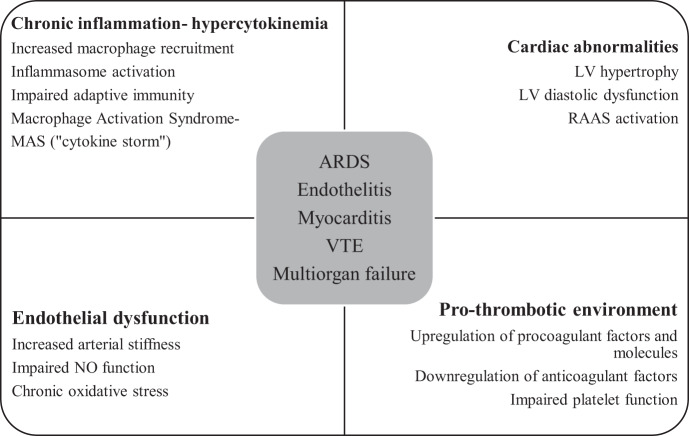
As we mentioned above, the association of obesity with prolonged recovery and worse clinical outcomes in viral infections has long been known. In recent years, as the role of adipose tissue as a distinct endocrine organ is being elucidated, obesity has been considered an independent risk factor for increased susceptibility to infections, sepsis, and higher mortality (9). This increased risk has been attributed to the state of chronic, low-grade inflammation that characterizes obesity, which results in metabolic and immune derangement. As the pathophysiology of SARS-CoV-2 infection is being unraveled, the links between the severity of clinical presentation and the dysmetabolic background are revealed (Fig. 1).
Fig. 1.
Possible mechanisms through which obesity leads to worse COVID-19 outcomes. ARDS, acute respiratory distress syndrome; LV, left ventricle; MAS, macrophage activation syndrome; NO, nitric oxide; RAAS, renin-angiotensin-aldosterone system; VTE, venous thromboembolism.
Chronic Inflammation and Immune Dysregulation
The dysfunctional hypertrophic adipocytes in obesity produce an excessive amount of cytokines such as IL-6, IL-8, monocyte chemoattractant protein-1 (MCP-1/CCL2), leptin, and plasminogen activator inhibitor-1 (PAI-1), among others, which leads to the increased recruitment of macrophages, especially polarized M1 macrophages (12, 19). These cells, in turn, produce high amounts of proinflammatory molecules like IL-1β, IL-6, IL-8, TNFα, and MCP-1 (18), an effect that is enhanced also by the action of the increased circulating levels of free fatty acids (FFAs) through the NF-κB pathway (35). The cumulative effect of these actions is a state of chronic inflammation and hypercytokinemia, which leads to defective innate immunity and creates a conducive ground for the hyperinflammatory response mediated through MAS in severe COVID-19 cases (10). The adaptive immunity is also adversely affected in obesity, with several studies showing a decline in naïve CD4+ T cells, as well as an imbalance of CD4+ T helper cells toward Th17 and Th22 proinflammatory subsets (9, 20). Similarly, in patients with COVID-19, peripheral counts of CD4+ and CD8+ T cells are low, but with a higher ratio of proinflammatory Th17 cells (10). Even more interestingly, the presence of increased levels of IL-1β in patients with COVID-19 infection suggests that cell pyroptosis, mediated through the activation of the NOD-like receptor family pyrin domain-containing 3 (NLRP3) inflammasome, might be strongly involved in the pathogenesis of the infection (13). The role of inflammasome activation has already been pointed out in studies on other coronavirus infections, where it was demonstrated that Viroporin 3a activated the NLRP3 inflammasome during the SARS-CoV infection (8), whereas another study on MERS-CoV infection revealed increased amounts of pyroptotic markers (caspase-1 and IL-1β) in the patient group (15). Even more importantly, in a study by Grailer et al. (11) in mice, the presence of acute lung injury (ALI) after airway instillation of lipopolysaccharide (LPS) was dependent on availability of NLRP3 and caspase-1, which are known features of the NLRP3 inflammasome. As numerous studies both in humans and animal models have shown, NLRP3 expression is increased in obesity, rendering it a pivotal factor in recruitment of macrophages and immune activation (16, 27). Therefore, agents that inhibit its action, such as colchicine, seem promising in the treatment of specific COVID-19 patients. In addition, agents such as anakinra, an IL-1 blocker, and tocilizumab, an IL-6 blocker, which have proven beneficial in the treatment of rheumatoid arthritis, which is accompanied as well by an excessive cytokine release, have been tested in randomized controlled trials (RCTs) in severe cases of COVID-19, with favorable results and unremarkable adverse events so far (29, 37).
Endothelial Dysfunction and Arterial Stiffness
A recent report by Varga et al. (34) pointed out for the first time the role of the endothelium in the pathogenesis of COVID-19. More specifically, postmortem histology of three patients with severe infection revealed viral inclusion structures in endothelial cells, accumulation of inflammatory cells associated with the endothelium, congestion of the small lung vessels, and endothelitis of the submucosal vessels of the small intestine, implying that the virus uses the ACE2 receptors expressed on endothelial cells in a pattern similar to that of alveolar infection, and therefore, the clinical presentation might be worse in vulnerable patients with preexisting endothelial dysfunction. Obesity is such a typical example, and the mechanisms that lead to vascular abnormalities are various. The hyperinsulinemia and insulin resistance that is a common feature of obesity leads to reduction in the insulin-stimulated phosphoinositide 3-kinase (PI3K) endothelial nitric oxidase synthase (eNOS) signaling pathway, reducing the vasculoprotective effects of nitric oxide (NO) and its anti-inflammatory actions (4). Increased oxidative stress due to RAAS-induced activation of NADPH oxidase, xanthine oxidase, and mitochondrial oxidative stress results in increased destruction of NO, and its decreased bioavailability further induces macrophage activation (3). The chronic exposure of endothelial cells to the increased circulating levels of leptin observed in obesity leads to a decreased NO production and increased MCP-1 expression, which further enhances leukocyte infiltration into vascular cells (5, 32). Perivascular adipose tissue (PVAT), exerting anticontractile effects on the endothelium in lean individuals, contributes to vasoconstriction and endothelial malfunction in obesity via increased secretion of TNFα, IL-6, reactive oxygen species (ROS), and chemerin while downregulating NO production (26). Consistent with the favorable results in hypercytokinemia and acute hyperinflammatory state, the administration of tocilizumab to rheumatoid arthritis patients has been shown to improve pulse wave velocity and brachial blood pressure, which were used as indices of vascular function, and a similar benefit in COVID-19 patients could thus be presumed (14).
Cardiovascular Events and Thrombosis
Another serious consideration in SARS-CoV-2 infection is its cardiovascular manifestations. Acute cardiac injury is highly prevalent in patients with COVID-19 and is associated with worse clinical outcomes (13, 41). Although the relatively high rate of heart failure (23%) that was observed in patients with COVID-19 could not be explicitly attributed to exacerbation of a preexisting condition or a new cardiomyopathy (7, 41), the presence of acute myocarditis was the definite cause of death in 7% of patients in a case series of 150 patients with COVID-19, whereas in other studies, postmortem histology revealed fulminant myocarditis with the presence of inflammatory mononuclear infiltrates in myocardial tissue (28, 38). The risk of venous thromboembolism also seems important, as in a significant percentage of patients with severe infection, elevated levels of D-dimers have been observed, whereas ∼71% of patients met clinical criteria for disseminated intravascular coagulation (DIC) (33, 41). Obesity is a well-established risk factor for cardiovascular disease (CVD) both per se and through its common comorbidities, such as insulin resistance (IR), diabetes mellitus (DM), and hypertension. The most common alteration in cardiac morphology in obesity is left ventricular (LV) hypertrophy, with hypertension and IR being important determinants of the LV mass (1, 2). In addition, obesity is associated with activation of the renin-angiotensin-aldosterone system (RAAS), which leads to increased levels of angiotensin II, with direct effects on the myocardium (36). Apart from structural changes, obesity is associated with LV diastolic dysfunction and heart failure (1, 2, 24). Chronic inflammation by the proinflammatory cytokines mentioned above leads to upregulation of procoagulant factors (like the tissue factor) and adhesion molecules (like P-selectin), downregulation of anticoagulant regulatory proteins (such as tissue factor pathway inhibitor, antithrombin, and the protein C anticoagulation system), increased thrombin generation, and enhanced platelet activation, thus increasing the risk for thrombosis (6). Again, in patients with rheumatoid arthritis, the administration of anakinra (mainly) and tocilizumab resulted in a simultaneous improvement in oxidative stress and myocardial deformation, rendering these agents a potential treatment option for patients with COVID-19 and cardiovascular manifestations (14).
CONCLUSIONS
Obesity has emerged as a major risk factor for worse COVID-19 outcomes. Chronic inflammation and oxidative stress, hypercytokinemia, immune dysregulation, endothelial dysfunction, and cardiovascular abnormalities are all possible mechanisms through which the excess in adipose tissue could lead to the acute hyperinflammatory state that characterizes severe SARS-CoV-2 infections and is responsible for its complications. The lessons learned from other diseases with a similar inflammatory profile, such as rheumatoid arthritis, provide useful insights into the better understanding of these mechanisms and, above all, propose that patients with obesity could be appropriate candidates for the use of agents such as colchicine and anti-IL-1 and anti-IL-6 compounds early in the course of the disease, benefiting from the amelioration of their preexisting, proinflammatory state. Of course, large RCTs are necessary to further clarify the pathways through which metabolic derangement leads to worse COVID-19 outcomes and establish the ideal treatment regimen for each individual patient.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
E.K. drafted manuscript; E.K., I.I., F.K., K.B., A. Kountouri, A.R., L.P., A. Kokkinos, and V.L. edited and revised manuscript; E.K., I.I., F.K., K.B., A. Kountouri, A.R., L.P., A. Kokkinos, and V.L. approved final version of manuscript.
REFERENCES
- 1.Alpert MA, Lavie CJ, Agrawal H, Aggarwal KB, Kumar SA. Obesity and heart failure: epidemiology, pathophysiology, clinical manifestations, and management. Transl Res 164: 345–356, 2014. doi: 10.1016/j.trsl.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 2.Alpert MA. Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci 321: 225–236, 2001. doi: 10.1097/00000441-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Aroor AR, Jia G, Sowers JR. Cellular mechanisms underlying obesity-induced arterial stiffness. Am J Physiol Regul Integr Comp Physiol 314: R387–R398, 2018. doi: 10.1152/ajpregu.00235.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Avogaro A, de Kreutzenberg SV, Fadini GP. Oxidative stress and vascular disease in diabetes: is the dichotomization of insulin signaling still valid? Free Radic Biol Med 44: 1209–1215, 2008. doi: 10.1016/j.freeradbiomed.2007.12.021. [DOI] [PubMed] [Google Scholar]
- 5.Beyer AM, Guo DF, Rahmouni K. Prolonged treatment with angiotensin 1-7 improves endothelial function in diet-induced obesity. J Hypertens 31: 730–738, 2013. doi: 10.1097/HJH.0b013e32835ecbe5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blokhin IO, Lentz SR. Mechanisms of thrombosis in obesity. Curr Opin Hematol 20: 437–444, 2013. doi: 10.1097/MOH.0b013e3283634443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buzon J, Roignot O, Lemoine S, Perez P, Kimmoun A, Levy B, Novy E. Takotsubo Cardiomyopathy Triggered by Influenza A Virus. Intern Med 54: 2017–2019, 2015. doi: 10.2169/internalmedicine.54.3606. [DOI] [PubMed] [Google Scholar]
- 8.Chen IY, Moriyama M, Chang MF, Ichinohe T. Severe Acute Respiratory Syndrome Coronavirus Viroporin 3a Activates the NLRP3 Inflammasome. Front Microbiol 10: 50, 2019. doi: 10.3389/fmicb.2019.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frydrych LM, Bian G, O’Lone DE, Ward PA, Delano MJ. Obesity and type 2 diabetes mellitus drive immune dysfunction, infection development, and sepsis mortality. J Leukoc Biol 104: 525–534, 2018. doi: 10.1002/JLB.5VMR0118-021RR. [DOI] [PubMed] [Google Scholar]
- 10.Giamarellos-Bourboulis EJ, Netea MG, Rovina N, Akinosoglou K, Antoniadou A, Antonakos N, Damoraki G, Gkavogianni T, Adami ME, Katsaounou P, Ntaganou M, Kyriakopoulou M, Dimopoulos G, Koutsodimitropoulos I, Velissaris D, Koufargyris P, Karageorgos A, Katrini K, Lekakis V, Lupse M, Kotsaki A, Renieris G, Theodoulou D, Panou V, Koukaki E, Koulouris N, Gogos C, Koutsoukou A. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe. In press. doi: 10.1016/j.chom.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grailer JJ, Canning BA, Kalbitz M, Haggadone MD, Dhond RM, Andjelkovic AV, Zetoune FS, Ward PA. Critical role for the NLRP3 inflammasome during acute lung injury. J Immunol 192: 5974–5983, 2014. doi: 10.4049/jimmunol.1400368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guilherme A, Virbasius JV, Puri V, Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol 9: 367–377, 2008. doi: 10.1038/nrm2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497–506, 2020. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ikonomidis I, Pavlidis G, Katsimbri P, Andreadou I, Triantafyllidi H, Tsoumani M, Varoudi M, Vlastos D, Makavos G, Kostelli G, Βenas D, Lekakis J, Parissis J, Boumpas D, Alexopoulos D, Iliodromitis E. Differential effects of inhibition of interleukin 1 and 6 on myocardial, coronary and vascular function. Clin Res Cardiol 108: 1093–1101, 2019. doi: 10.1007/s00392-019-01443-9. [DOI] [PubMed] [Google Scholar]
- 15.Jiang Y, Li J, Teng Y, Sun H, Tian G, He L, Li P, Chen Y, Guo Y, Li J, Zhao G, Zhou Y, Sun S. Complement receptor C5aR1 inhibition reduces pyroptosis in hDPP4-transgenic mice Infected with MERS-CoV. Viruses 11: 39, 2019. doi: 10.3390/v11010039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kousathana F, Georgitsi M, Lambadiari V, Giamarellos-Bourboulis EJ, Dimitriadis G, Mouktaroudi M. Defective production of interleukin-1 beta in patients with type 2 diabetes mellitus: Restoration by proper glycemic control. Cytokine 90: 177–184, 2017. doi: 10.1016/j.cyto.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 17.Lighter J, Phillips M, Hochman S, Sterling S, Johnson D, Francois F, Stachel A. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clin Infect Dis. In press. doi: 10.1093/cid/ciaa415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest 117: 175–184, 2007. doi: 10.1172/JCI29881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maurizi G, Della Guardia L, Maurizi A, Poloni A. Adipocytes properties and crosstalk with immune system in obesity-related inflammation. J Cell Physiol 233: 88–97, 2018. doi: 10.1002/jcp.25855. [DOI] [PubMed] [Google Scholar]
- 20.McLaughlin T, Ackerman SE, Shen L, Engleman E. Role of innate and adaptive immunity in obesity-associated metabolic disease. J Clin Invest 127: 5–13, 2017. doi: 10.1172/JCI88876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK . COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 395: 1033–1034, 2020. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moser JS, Galindo-Fraga A, Ortiz-Hernández AA, Gu W, Hunsberger S, Galán-Herrera JF, Guerrero ML, Ruiz-Palacios GM, Beigel JH; La Red ILI 002 Study Group . Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respir Viruses 13: 3–9, 2019. doi: 10.1111/irv.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab 318: E736–E741, 2020. doi: 10.1152/ajpendo.00124.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pascual M, Pascual DA, Soria F, Vicente T, Hernández AM, Tébar FJ, Valdés M. Effects of isolated obesity on systolic and diastolic left ventricular function. Heart 89: 1152–1156, 2003. doi: 10.1136/heart.89.10.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petrilli C, Jones S, Yang J, Rajagopalan H, O’Donnell LF, Chernyak Y, Tobin K, Cerfolio RJ, Francois F, Horwitz LI. Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. medRxiv. In press. doi: 10.1101/2020.04.08.20057794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ray S, Miglio C, Eden T, Del Rio D. Assessment of vascular and endothelial dysfunction in nutritional studies. Nutr Metab Cardiovasc Dis 24: 940–946, 2014. doi: 10.1016/j.numecd.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 27.Rheinheimer J, de Souza BM, Cardoso NS, Bauer AC, Crispim D. Current role of the NLRP3 inflammasome on obesity and insulin resistance: A systematic review. Metabolism 74: 1–9, 2017. doi: 10.1016/j.metabol.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 28.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 46: 846–848, 2020. [Erratum in: Intensive Care Med. In press.] doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shakoory B, Carcillo JA, Chatham WW, Amdur RL, Zhao H, Dinarello CA, Cron RQ, Opal SM. Interleukin-1 receptor blockade is associated with reduced mortality in sepsis patients with features of macrophage activation syndrome. Crit Care Med 44: 275–281, 2016. doi: 10.1097/CCM.0000000000001402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Short KR, Kedzierska K, van de Sandt CE. Back to the future: lessons learned from the 1918 influenza pandemic. Front Cell Infect Microbiol 8: 343, 2018. doi: 10.3389/fcimb.2018.00343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, Labreuche J, Mathieu D, Pattou F, Jourdain M; Lille Intensive Care COVID-19 and Obesity study group . High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring). In press. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sprague AH, Khalil RA. Inflammatory cytokines in vascular dysfunction and vascular disease. Biochem Pharmacol 78: 539–552, 2009. doi: 10.1016/j.bcp.2009.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 18: 844–847, 2020. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 395: 1417–1418, 2020. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang C, Ha X, Li W, Xu P, Gu Y, Wang T, Wang Y, Xie J, Zhang J. Correlation of TLR4 and KLF7 in inflammation induced by obesity. Inflammation 40: 42–51, 2017. doi: 10.1007/s10753-016-0450-z. [DOI] [PubMed] [Google Scholar]
- 36.Wong C, Marwick TH. Obesity cardiomyopathy: pathogenesis and pathophysiology. Nat Clin Pract Cardiovasc Med 4: 436–443, 2007. doi: 10.1038/ncpcardio0943. [DOI] [PubMed] [Google Scholar]
- 37.Xu X, Han M, Li T, Sun W, Wang D, Fu B, Zhou Y, Zheng X, Yang Y, Li X, Zhang X, Pan A, Wei H. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci USA 117: 10970–10975, 2020. doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 8: 420–422, 2020. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang L, Chan KP, Lee RS, Chan WM, Lai HK, Thach TQ, Chan KH, Lam TH, Peiris JS, Wong CM. Obesity and influenza associated mortality: evidence from an elderly cohort in Hong Kong. Prev Med 56: 118–123, 2013. doi: 10.1016/j.ypmed.2012.11.017. [DOI] [PubMed] [Google Scholar]
- 40.Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, Akdis CA, Gao YD. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. In press. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 41.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395: 1054–1062, 2020. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]