Abstract
Background
Fasting the month of Ramadan should be achieved by every pubescent Muslim unless they have an excuse. Fasting involves complete abstinence of oral intake throughout daytime. Patients who have hypothyroidism usually require levothyroxine (L-thyroxine) replacement, which is typically given on an empty stomach away from meals. Taking L-thyroxine replacement without feeding is challenging during the nighttime of Ramadan, in addition to being prohibited during daytime.
Objectives
This study aimed to determine the best time of L-thyroxine intake during Ramadan.
Methods
Fifty patients who were taking L-thyroxine treatment for primary hypothyroidism were involved in this prospective study for three months including the fasting and pre-fasting months. The patients were divided into three groups with different times of L-thyroxine intake. In the group one (pre-iftar), the patients were asked to take L-thyroxine at the time of iftar (the sunset meal) but to delay any oral intake for at least 30 minutes. In the group two (post-iftar), the patients were asked to take L-thyroxine two hours after iftar. The patients in the last group (pre-suhoor) were asked not to eat in the last two hours before suhoor (the predawn meal) and to take L-thyroxine tablet one hour prior to suhoor.
Results
When thyroid stimulating hormone (TSH) levels were compared before and after Ramadan, there were no significant differences neither within each group nor among all the study groups. Moreover, the frequencies of the TSH control after Ramadan showed no significant differences within each of the study groups (P = 0.18, 0.75, 1.0 for pre-suhoor, pre-iftar, and post-iftar respectively). Similarly, comparison among the groups of the study showed no significant differences regardless of whether the patients had controlled or uncontrolled TSH prior to Ramadan (P = 0.75 and 0.67, respectively). In the patients with controlled TSH before Ramadan, 8 out of 10 (pre-suhoor), 8 out of 12 (pre-iftar), and 4 out of 6 (post-iftar) maintained their control after Ramadan. While in the patients with uncontrolled TSH before Ramadan, 7 out of 10 (pre-suhoor), 6 out of 8 (pre-iftar), and 2 out of 4 (post-iftar) achieved controlled TSH after Ramadan.
Conclusions
No significant differences in TSH control were observed in patients taking L-thyroxine at pre-iftar, post-iftar, or pre-suhoor time in Ramadan.
Keywords: Hypothyroidism, Thyroxine, Ramadan, Fasting
1. Background
The lunar month of Ramadan is one of the five obligatory Islamic pillars. It should be pursuit by every pubescent Muslim with few exceptions such as travelers, medically ill patients and pregnant women (1). Several millions of Muslims around the world fast the month of Ramadan every year, starting from dawn (suhoor) to sunset (iftar). During this period, they abstain from eating, drinking, smoking and sexual activity (1, 2).
People who fast Ramadan constitute a large number; thus, it is of interest to perform studies to examine the effect of fasting on various metabolic parameters (3).
Hypothyroidism represents the most common thyroid disorder with a higher frequency in women and the elderly. It has a broad spectrum of clinical presentations ranging from asymptomatic conditions to more serious and severe conditions such as myxedema coma (4).
Typically, levothyroxine (L-thyroxine) is the primary treatment for hypothyroidism, which has a low cost and few side effects. Optimally, L-thyroxine should be taken on an empty stomach at least 30 minutes before a meal (5). Unfortunately, a large number of patients fail to demonstrate a clinical and biochemical response, even though they take their typical dose. This poor response is mostly due to noncompliance with levothyroxine therapy (6). Several other factors have been highlighted by studies as causes of treatment failure such as celiac disease (7), lactose intolerance (8) and concomitant intake of food such as fiber-rich food, soy protein, grapefruit and coffee which interfere with L-thyroxine absorption (9, 10). In addition, some drugs are known to affect L-thyroxine absorption, leaving patients with a suboptimal response like calcium carbonate (11) and ferrous sulfate (12).
There is a great debate regarding the best timing for administration of L-thyroxine. Some studies have shown that there is no difference between taking L-thyroxine at bedtime or in the morning (13-15).
Up to our knowledge, there are very few studies conducted to examine the best time of L-thyroxine administration during Ramadan.
2. Objectives
This study aimed to determine the best time of L-thyroxine intake during Ramadan.
3. Methods
3.1. Setting
This was a three-month prospective study conducted between April-June 2018. Patients attending the Faiha Specialized Diabetes, Endocrine, and Metabolism Center (FDEMC) in Basrah (Southern of Iraq) were enrolled in the study after providing consent. All the enrolled patients were already using L-thyroxine for hypothyroidism treatment. The inclusion criteria were adults with primary hypothyroidism.
Patients with central hypothyroidism, those who made dose adjustment during the time of the study and those with conditions known to affect either the thyroid function test or L-thyroxine absorption and metabolism like acute illness, severe chronic disease, celiac disease, intake of certain medications like ferrous sulfate, calcium carbonate, bile acid sequestrants, aluminum hydroxide antacids, activated charcoal, sucralfate, proton pump inhibitors, cholestyramine, colestipol, steroids, and certain materials like soya products were excluded from the study.
3.2. Participants
Thyroid stimulating hormone (TSH) values within one month before Ramadan (April) were measured in all the participants and repeated again within one month after Ramadan (June) for comparison.
In pre-Ramadan visit, the patients were advised to participate in the study and choose any group of L-thyroxine intake times. During Ramadan (May, 2018), the patients were divided into three groups. In the group one (pre-iftar), the patients were instructed to take L-thyroxine at the time of iftar (the sunset meal) but to delay any oral intake for at least 30 minutes. In the group two (post-iftar), the patients were asked to take L-thyroxine two hours after iftar. The patients in the last group (pre-suhoor) were asked to take L-thyroxine tablet one hour before suhoor (the predawn meal) but to avoid oral consumption one hour before tablet intake.
3.3. Biochemical Analysis
All laboratory tests were performed via the electrochemiluminescent method. To this end, Cobas e 411 analyzers from Roche Diagnostics (Germany) were used with a TSH measuring range between 0.005 - 100.0 µIU/mL and a reference range between 0.27- 4.2 µIU/mL, which specified the intra-assay precision of 0.1 - 4 µU/mL (< 5% CV). Moreover, free thyroxine (free T4) was also used with a measuring range between 0.023 - 7.77 ng/dL and a reference range between 0.93 - 1.7 ng/dL, which specified the intra-assay precision of 25 - 100 pmol/L (< 3% CV). For statistical analysis, all data were computed and analyzed using SPSS (version 23.0, SPSS Inc., Chicago, IL, USA).
Ethical approval was granted from the Ethical Committee of the Basrah Health Directorate.
3.4. Definitions
Patients who had the TSH value between 0.27 - 4.2 µIU/mL were considered to be controlled whereas those with the TSH value > 4.2 µIU/mL were considered to be uncontrolled.
3.5. Statistical Analysis
SPSS version 23.0. was used for analysis. Qualitative variables were summarized as numbers (N) and percentages (%), while quantitative variables were summarized as mean and standard deviation (M ± SD). The one-way ANOVA test was used for comparison of age, BMI, and TSH level. Moreover, the chi-square test was used to compare gender and TSH control among the three study groups. The paired t-test was used in each of the study groups for TSH level analysis during pre- and post-Ramadan visits, and the one-way ANOVA test was used to compare the TSH level among the study groups. Further, the McNemar test was used to examine the TSH control before and after Ramadan within each study group, while the chi-square test was used for TSH control comparison before and after Ramadan among the study groups. For all the performed tests, results were considered statistically significant if P value < 0.05.
4. Results
Table 1 summarizes the general characteristics of the studied patients. From a total of 50 patients enrolled in the study, 42 were females with a comparable female to male ratio among all the groups. There was no significant difference in the mean age, BMI, and TSH among the groups.
Table 1. General Characteristics of the Study Patientsa.
| Values | P Value | ||||
|---|---|---|---|---|---|
| Overall (N = 50) | Pre-Suhoor (N = 20) | Pre-Iftar (N = 20) | Post-Iftar (N = 10) | ||
| Age, y | 44.12 ± 13.72 | 41.30 ± 14.93 | 47.15 ± 11.52 | 43.70 ± 15.72 | 0.43 |
| Gender (women), N | 42 | 16 | 17 | 9 | 0.77 |
| BMI, kg/m 2 | 32.21 ± 6.66 | 31.89 ± 7.54 | 30.94 ± 5.08 | 35.59 ± 7.31 | 0.22 |
| TSH, µIU/mL | |||||
| Before Ramadan | 3.82 ± 3.03 | 4.32 ± 3.12 | 2.97 ± 2.61 | 4.51 ± 3.53 | 0.27 |
| After Ramadan | 3.23 ± 3.27 | 3.12 ± 3.43 | 2.95 ± 2.31 | 4.01 ± 4.61 | 0.70 |
| Controlled TSH before Ramadan, N | 28 | 10 | 12 | 6 | 0.78 |
Abbreviation: BMI, body mass index.
aValues are expressed as mean ± SD.
bP value results obtained using the ANOVA test.
After comparing the TSH level before and after Ramadan, as shown in Table 2, no significant differences were observed among the study groups. Although the patients in the pre-suhoor group showed the highest mean reduction in the TSH level after Ramadan (1.20 ± 4.0 µIU/mL), the overall comparison ratio was not significant among the groups.
Table 2. Paired t-Test Comparison of the TSH Level Before and After Ramadan Within Each Study Group.
| L-thyroxine Intake Time | Difference in TSH (Before, After Ramadan) | Paired t-Test P Valueb | ANOVA Test P Valuec |
|---|---|---|---|
| Pre-suhoor | 1.20 ± 4.0 | 0.19 | 0.69 |
| Pre-iftar | 0.02 ± 4.0 | 0.97 | |
| Post-iftar | 0.50 ± 5.6 | 0.78 |
aValues are expressed as mean ± SD.
bPaired t-test for difference in the TSH level before and after Ramadan within each group.
cThe ANOVA test for the mean difference in the TSH level among the groups.
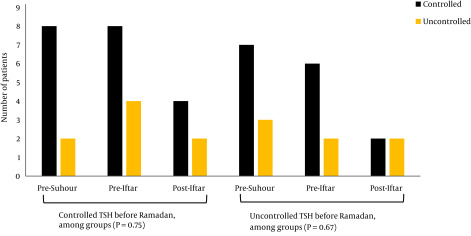
Table 3 presents the effect of different times of L-thyroxine intake during Ramadan on the TSH control. Within each group of the patients, no significant differences were detected in the TSH control level (P = 0.18, 0.75, 1.0 for pre-suhoor, pre-iftar, and post-iftar, respectively). In the controlled patients before Ramadan, 8 out of 10 (pre-suhoor), 8 out of 12 (pre-iftar), and 4 out of 6 (post-iftar) maintained their control after Ramadan. While for the uncontrolled patients before Ramadan, 7 out of 10 (pre-suhoor), 6 out of 8 (pre-iftar), and 2 out of 4 (post-iftar) achieved controlled TSH after Ramadan. Comparison of the groups showed no significant differences in the achievement rate of the TSH control during pre-suhoor, pre-iftar, and post-iftar, whether patients were controlled or uncontrolled before Ramadan (P = 0.75 and 0.67, respectively), as shown in Figure 1.
Table 3. The TSH Control Before and After Ramadan According to the Time of L-Thyroxin Intake.
| L-Thyroxine Intake Time | The TSH Control Before and After Ramadan | McNemar P Value | ||
|---|---|---|---|---|
| Before Ramadan | After Ramadan | |||
| Controlled | Uncontrolled | |||
| Overall | Controlled | 20 | 8 | 0.21 |
| Uncontrolled | 15 | 7 | ||
| Pre-suhoor | Controlled | 8 | 2 | 0.18 |
| Uncontrolled | 7 | 3 | ||
| Pre-iftar | Controlled | 8 | 4 | 0.75 |
| Uncontrolled | 6 | 2 | ||
| Post-iftar | Controlled | 4 | 2 | 1.0 |
| Uncontrolled | 2 | 2 | ||
Figure 1. The TSH control after Ramadan in different times of L-thyroxine intake.
5. Discussion
There have been contradictory results with regard to the best timing to take L-thyroxine in Ramadan. Some studies supported L-thyroxine intake at bedtime (13, 14), while other studies supported L-thyroxine intake during early morning fasting (16). Yet, some other studies found no timing difference in this regard (17). The optimum timing of L-thyroxine consumption in Ramadan is still undetermined. In our study, we did not find a significant difference in the effect of taking L-thyroxine at three different times during Ramadan, i.e. pre-iftar, post-iftar, and pre-suhoor. Moreover, we documented a non-significant overall reduction in the TSH level after Ramadan, which remained within the normal reference limit.
Two studies reported a significant rise in the TSH level after Ramadan in healthy subjects not taking L-thyroxine (18) and in hypothyroid patients consuming L-thyroxine (15). It appears that Ramadan fasting per se affects the TSH level, even in healthy people. Hadjzadeh et al. (19) in their review suggested to increase the dose of L-thyroxine routinely in Ramadan by 25 - 50 microgram per day. However, in our study, we demonstrated a non-significant reduction in the TSH level after Ramadan. Another interesting finding in our study was that the pre-suhoor group showed statistically non-significantly better results than the other groups in terms of the magnitude of TSH reduction before and after Ramadan.
Taking L-thyroxine on an empty stomach one hour before iftar is challenging for those who choose to fast. Intake of tablets or drinking water before the time of iftar will break the fast. Likewise, taking L-thyroxine one hour before suhoor may be not feasible for many people as waking up at that time is difficult and most people prefer to sleep until the time of suhoor. The sleep pattern is naturally disturbed in Ramadan because of the suhoor meal and thus adding extra-disturbance is regarded undesirable by patients. One study found that bedtime L-thyroxine intake was convenient and effective during Ramadan (20). In addition, two studies found that L-thyroxine intake was better at bedtime than in the morning (16, 17). Furthermore, early restoration of euthyroidism was documented in those taking L-thyroxine at evening time (17). Therefore, taking L-thyroxine after iftar may be more convenient to some patients during Ramadan. In our study, we did not document any difference in the intake time of L-thyroxine between the three studied groups. Hence, we recommend ingesting the tablet at any of the three specified times, namely before iftar, two hours after iftar and before suhoor, at patients’ convenience. This may offer patients flexibility in choosing the preferred time.
The strength of this study is due to the fact that it was carried out in a routine clinical setting and it compared L-thyroxine intake at three different times, which gave the patients as well as the investigators flexibility to choose the proper time.
There were some limitations in the study. First, the time interval was less than six weeks for TSH measurement in some patients. Second, the study design concentrated on patient convenience rather than on pharmacological properties of L-thyroxine. Third, symptomatology or quality of life measures were not considered. Fourth, the study was conducted in a single center. Fifth, no comparison was made in terms of the TSH profile with normal individuals. Finally, although we instructed the participants to take L-thyroxine at least two hours after iftar, we could not confirm neither the exact interval between iftar and L-thyroxine intake in the post-iftar group nor all the interferences of L-thyroxine absorption.
5.1. Conclusions
No significant differences were observed in maintaining or achieving new TSH control during Ramadan, whether L-thyroxin was taken at pre-iftar, post-iftar, or pre-suhoor time. Thus, different times of thyroxine intake during Ramadan are accepted.
Footnotes
Authors' Contribution: Ammar Mohammed Saeed Almomin and Ibrahim Abbood Zaboon designed the study. All authors abstracted and analyzed data. Ibrahim Hani Hussein, Ibrahim Abbood Zaboon, Haider Ayad Alidrisi, Nassar Taha Yaseen Alibrahim, Majid Alabbood, and Dheyaa Kadhim Al-Waeli wrote the manuscript. Ammar Mohammed Saeed Almomin, Haider Ayad Alidrisi, Hussein Ali Nwayyir, and Abbas Ali Mansour contributed to the development of the protocol. Ibrahim Abbood Zaboon, Haider Ayad Alidrisi, and Ammar Mohammed Saeed Almomin abstracted data, and prepared the manuscript.
Conflict of Interests: None.
Funding/Support: None.
Contributor Information
Ibrahim Abbood Zaboon, Email: dr.ibraheem2@gmail.com.
Haider Ayad Alidrisi, Email: haider.alidrisi@fdemc.iq.
Ibrahim Hani Hussein, Email: almttoryibrahim@gmail.com.
Majid Alabbood, Email: majid.alabbood@uobasrah.edu.
Nassar Taha Yaseen Alibrahim, Email: nassar.yaseen@fdemc.iq.
Ammar Mohammed Saeed Almomin, Email: ammar.almomin75@gmail.com.
Dheyaa Kadhim Al-Waeli, Email: dhiaa.alwaeli@fdemc.iq.
Ali Hussein Ali Alhamza, Email: ali.alhamza@fdemc.iq.
Adel Gassab Mohammed, Email: adel.gassab@fdemc.iq.
Hussein Ali Nwayyir, Email: hussein.nwayyir@fdemc.iq.
Ahmed Jaafer Hindi Al-Ali, Email: ahmadjha979@yahoo.com.
Abbas Ali Mansour, Email: abbas.mansour@fdemc.iq.
References
- 1.Azizi F. Medical aspects of Islamic fasting. Med J Islam Republ Iran. 1996;10(3):241–6. [Google Scholar]
- 2.Reilly T, Waterhouse J. Altered sleep-wake cycles and food intake: The Ramadan model. Physiol Behav. 2007;90(2-3):219–28. doi: 10.1016/j.physbeh.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 3.Dewanti L, Watanabe C, Sulistiawati. Ohtsuka R. Unexpected changes in blood pressure and hematological parameters among fasting and nonfasting workers during Ramadan in Indonesia. Eur J Clin Nutr. 2006;60(7):877–81. doi: 10.1038/sj.ejcn.1602393. [DOI] [PubMed] [Google Scholar]
- 4.Golden SH, Robinson KA, Saldanha I, Anton B, Ladenson PW. Clinical review: Prevalence and incidence of endocrine and metabolic disorders in the United States: A comprehensive review. J Clin Endocrinol Metab. 2009;94(6):1853–78. doi: 10.1210/jc.2008-2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, et al. Guidelines for the treatment of hypothyroidism: Prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid. 2014;24(12):1670–751. doi: 10.1089/thy.2014.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ain KB, Refetoff S, Fein HG, Weintraub BD. Pseudomalabsorption of levothyroxine. JAMA. 1991;266(15):2118–20. [PubMed] [Google Scholar]
- 7.McDermott JH, Coss A, Walsh CH. Celiac disease presenting as resistant hypothyroidism. Thyroid. 2005;15(4):386–8. doi: 10.1089/thy.2005.15.386. [DOI] [PubMed] [Google Scholar]
- 8.Munoz-Torres M, Varsavsky M, Alonso G. Lactose intolerance revealed by severe resistance to treatment with levothyroxine. Thyroid. 2006;16(11):1171–3. doi: 10.1089/thy.2006.16.1171. [DOI] [PubMed] [Google Scholar]
- 9.Perez CL, Araki FS, Graf H, de Carvalho GA. Serum thyrotropin levels following levothyroxine administration at breakfast. Thyroid. 2013;23(7):779–84. doi: 10.1089/thy.2012.0435. [DOI] [PubMed] [Google Scholar]
- 10.Bell DS, Ovalle F. Use of soy protein supplement and resultant need for increased dose of levothyroxine. Endocr Pract. 2001;7(3):193–4. doi: 10.4158/EP.7.3.193. [DOI] [PubMed] [Google Scholar]
- 11.Singh N, Singh PN, Hershman JM. Effect of calcium carbonate on the absorption of levothyroxine. JAMA. 2000;283(21):2822–5. doi: 10.1001/jama.283.21.2822. [DOI] [PubMed] [Google Scholar]
- 12.Campbell NR, Hasinoff BB, Stalts H, Rao B, Wong NC. Ferrous sulfate reduces thyroxine efficacy in patients with hypothyroidism. Ann Intern Med. 1992;117(12):1010–3. doi: 10.7326/0003-4819-117-12-1010. [DOI] [PubMed] [Google Scholar]
- 13.Bolk N, Visser TJ, Kalsbeek A, van Domburg RT, Berghout A. Effects of evening vs morning thyroxine ingestion on serum thyroid hormone profiles in hypothyroid patients. Clin Endocrinol (Oxf). 2007;66(1):43–8. doi: 10.1111/j.1365-2265.2006.02681.x. [DOI] [PubMed] [Google Scholar]
- 14.Banerjee M, Hossain S, Mondal S, Maiti A. A comparative study on effect of evening versus morning intake of levothyroxine in patients of hypothyroidism. Thyroid Res Pract. 2018;15(2) doi: 10.4103/trp.trp_11_18. [DOI] [Google Scholar]
- 15.Sheikh A, Mawani M, Mahar SA. Impact of Ramadan fasting on thyroid status and quality of life in patients with primary hypothyroidism: A prospective cohort study from Karachi, Pakistan. Endocr Pract. 2018;24(10):882–8. doi: 10.4158/EP-2018-0038. [DOI] [PubMed] [Google Scholar]
- 16.Bach-Huynh TG, Nayak B, Loh J, Soldin S, Jonklaas J. Timing of levothyroxine administration affects serum thyrotropin concentration. J Clin Endocrinol Metab. 2009;94(10):3905–12. doi: 10.1210/jc.2009-0860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rajput R, Chatterjee S, Rajput M. Can levothyroxine be taken as evening dose? Comparative evaluation of morning versus evening dose of levothyroxine in treatment of hypothyroidism. J Thyroid Res. 2011;2011:505239. doi: 10.4061/2011/505239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sajid KM, Akhtar M, Malik GQ. Ramadan fasting and thyroid hormone profile. J Pak Med Assoc. 1991;41(9):213–6. [PubMed] [Google Scholar]
- 19.Hadjzadeh MAR, Pakdel R, Hayatdavoudi P, Nematy M. Hypothyroidism and ramadan fasting. J Fast Health. 2014;2(2):80–3. [Google Scholar]
- 20.Azizi F. Islamic fasting and thyroid hormones. Int J Endocrinol Metab. 2015;13(2):e29248. doi: 10.5812/ijem.13(2)2015.29248. [DOI] [PMC free article] [PubMed] [Google Scholar]