Abstract
Dysfunctional sleep beliefs are strongly involved in sleep difficulties, which in turn negatively predict psychological health and well-being. In contrast, psychological capital (PsyCap) is a positive cognitive resource, comprising four dimensions (hope, self-efficacy, resilience, and optimism), that positively predicts psychological well-being. Significant associations between sleep beliefs and well-being, and PsyCap and well-being are detailed; however, research on their interrelations (among sleep beliefs, well-being, and PsyCap) remains scarce. This cross-sectional study aimed to elucidate the relationships among the variables. The convenience sample consisted of 123 Australian working adults. Participants completed an online survey comprising four empirically established measures (Dysfunctional Beliefs and Attitudes about Sleep Scale, Psychological Well-being Scale, Psychological Capital Questionnaire, and a social desirability scale). Hypotheses were derived from Conservation of Resources (COR) theory, which underlines the importance of cognitive mechanisms that guide adaptive psychological responses. Results were consistent with hypotheses: dysfunctional sleep beliefs significantly and negatively predicted PsyCap, and PsyCap mediated the relationship between sleep beliefs and well-being. Findings suggested that PsyCap, which can be developed, may help buffer the adverse effects of sleep beliefs to benefit well-being. Replication of model coefficients in larger samples and future testing of PsyCap training within sleep-hygiene practices are recommended.
Keywords: Psychology, Dysfunctional sleep beliefs, Psychological well-being, Psychological capital, Conservation of Resources theory
Psychology; Dysfunctional sleep beliefs; Psychological well-being; Psychological capital; Conservation of Resources theory.
1. Introduction
Sleep difficulties and associated daytime consequences are reported by one-third of the global adult population (Linton et al., 2015; Yang et al., 2014). Persistent sleep disturbances are linked to long-term adverse effects on well-being, such as increased risk for anxiety, depression, and suicide (Cunnington et al., 2013; Norra et al., 2011). Employees with sleep issues report increased fatigue, higher occupational accident rates, and lower job satisfaction (Gingerich et al., 2018; Rosekind et al., 2010). Maladaptive sleep-related cognitions are associated with self-reported sleep difficulties (Brown et al., 2002; Jin et al., 2018; Morin et al., 2002), which in turn, present strong negative links to psychological well-being (Hamilton et al., 2007; Kao et al., 2008; Phelan et al., 2010). In contrast, psychological capital (PsyCap) is a cognitive resource that positively predicts psychological well-being (Avey et al., 2010; Luthans and Youssef-Morgan, 2017). While associations between sleep beliefs and well-being, and between PsyCap and well-being have been identified, research on sleep beliefs and positive psychological functioning remains scarce. There has been no examination of how dysfunctional sleep beliefs and PsyCap are related, and what their impacts might be on well-being. Given the negative influence of dysfunctional sleep beliefs on psychological well-being, and the positive effects of PsyCap on psychological well-being, we examined their interrelations.
1.1. Sleep beliefs and well-being
Self-reported sleep difficulties are associated with maladaptive sleep cognitions (Bluestein et al., 2011; Lundh, 2005). Dysfunctional sleep beliefs describe excessive, negatively toned cognitions that anticipate and emphasise the adverse consequences of inadequate sleep (Calkins et al., 2013). Sleep beliefs can play a significant role in sleep difficulties by transforming standard variations in sleep patterns into clinical sleep issues such as insomnia (Carney and Edinger, 2006; Jin et al., 2018; Morin et al., 2002). For example, the belief that a poor night of sleep will have detrimental daytime consequences can influence sleep-related anxiety and sleep-disruptive practices (e.g., daytime napping, increased caffeine intake), which in turn, compound sleep difficulties (Sánchez-Ortuño and Edinger, 2010).
The relationship between self-reported sleep disturbances and subjective well-being is well-established. In a large study, 3,643 adults reported how often they experienced difficulties getting to sleep, had trouble staying asleep, and had used medication to aid sleep in the previous 30 days (Hamilton et al., 2007). Participants with lower levels of subjective well-being reported more sleep disturbance, independent of age, gender, somatic symptoms, and cognitive disorders. Lemola et al. (2013) used a longitudinal research design to examine the relationships among variability in sleep duration (observed using actigraphy), self-reported sleep quality, and subjective well-being. In their sample of 128 adults, sleep quality partially mediated the relationship between variability in sleep duration and well-being. Daily variability in sleep duration was also related to poor subjective sleep quality and poor subjective well-being. Outcome studies have demonstrated the positive influence of mindfulness-based interventions on the self-regulation of sleep behaviour and well-being (Howell et al., 2010; Ong et al., 2008). Moreover, recent research has suggested that parental dysfunctional sleep beliefs have negative consequences for the mental health of adolescent offspring (Peltz and Rogge, 2019). Poorer parental sleep-related cognitions are associated with increased arguments about bedtime and poorer-quality sleep, which, in turn, increase the risk of anxiety and depression symptoms in adolescents (Peltz and Rogge, 2019).
Equally, adaptive sleep beliefs are linked to higher self-reported sleep quality and lower daytime functioning impairment (Brown et al., 2002; Gellis and Lichstein, 2009). In a longitudinal study of 518 women, higher psychological well-being predicted lower baseline depression scores and reduced the likelihood of disturbed sleep 10 years following baseline measures (Phelan et al., 2010). In a large Taiwanese study, involving more than 36,000 participants, higher daytime sleepiness ratings and shorter self-reported sleep duration independently predicted lower psychological well-being (Kao et al., 2008). Since psychological factors, such as optimism and adaptive acceptance of poor sleep, can influence subjective sleep appraisals independent of actual sleep performance (Edinger et al., 2000; Fichten et al., 1995), adaptive sleep cognitions appear instrumental to good psychological well-being. We examined this aspect further in the current study.
1.2. Psychological capital (PsyCap) and well-being
Positive psychology recognises that positive cognitions play an integral role in shaping mental health. Positivity is linked to better psychological and physiological outcomes (Alarcon et al., 2013; Lyubomirsky et al., 2005). PsyCap is a construct from the field of positive psychology with strong positive links to psychological well-being. PsyCap represents the shared commonalities among its four core dimensions of hope, self-efficacy, resilience, and optimism (Luthans, 2002; Luthans et al., 2007). As a composite construct, PsyCap has stronger positive associations with psychological well-being than any of its individual dimensions (Avey et al., 2010; Stajkovic, 2006). PsyCap also significantly predicts employee engagement, job satisfaction, and social responsibility better than its four core components independently (Bakker et al., 2008; Luthans and Youssef-Morgan, 2017). Accordingly, PsyCap was examined as a higher-order construct in the current study.
The relationship between PsyCap and several cognitive constructs, including psychological well-being, have been examined. Higher PsyCap levels are associated with higher levels of well-being, engagement, and organisational commitment (e.g., Avey et al., 2010; Hicks and Knies, 2015; Luthans and Youssef-Morgan, 2017). Conversely, meta-analysis indicates that lower PsyCap levels predict deleterious emotional states such as cynicism, anxiety, and exhaustion (Avey et al., 2011). Avey et al. (2010) observed small, nonetheless significant, variances over time in a longitudinal assessment of PsyCap and two measures of psychological well-being; the Index of Psychological Wellbeing based on Berkman's (1971) original scale and the 12-item General Health Questionnaire (GHQ-12; Goldberg, 1972; Goldberg and Hillier, 1979). Such findings have delineated the significant positive association between PsyCap, as a high-order construct, and psychological well-being.
Current conceptualisations of PsyCap, however, are not without controversy. Some social psychology and personality researchers suggest that PsyCap and its core components are dispositional or trait-like variables that offer limited scope for training (Carver et al., 2010). In contrast, clinical psychology researchers emphasise PsyCap-based intervention for coping strategies and enhanced functioning (Salanova and Ortega-Maldonado, 2019). Luthans et al. (2007), based on research in organisations, have argued that although the four core competencies that comprise PsyCap show stability over time, each competency can be developed, suggesting that PsyCap is more state-like than trait-like, and therefore open to change. The goal of PsyCap training is to promote positive thought patterns that challenge and replace long-standing assumptions and beliefs (Luthans and Youssef-Morgan, 2017; Luthans et al., 2010). Longitudinal studies support changes in PsyCap (Avey et al., 2010; Peterson et al., 2011). Experimental studies have also demonstrated the development of PsyCap through relatively short training programs (Dello Russo and Stoykova, 2015; Demerouti et al., 2011; Ertosun et al., 2015; Luthans et al., 2014), and web-based intervention (Luthans et al., 2008). Furthermore, a recent meta-analysis comprising 41 experimental studies suggested the overall effect of PsyCap intervention was significant, although small (Lupșa et al., 2019). As a positive psychological resource, PsyCap can be considered an asset (Luthans et al., 2014). Together, this research suggests that increases in PsyCap can be developed and can benefit psychological well-being.
The mediational effect of PsyCap has been examined in organisational-based samples (Heled et al., 2016; Luthans et al., 2008). PsyCap was a significant mediator of the relationship between empowering leadership and psychological well-being (Gyu Park et al., 2017) and three dimensions of burnout (i.e., emotional exhaustion, depersonalisation, personal accomplishment; Moyer et al., 2017). However, to date, only one known study has examined the mediating effect of PsyCap within the sleep domain. Hystad and Eid (2016) assessed the effect of PsyCap on sleep quality, fatigue, and duration at sea in seafarers. More than 740 seafarers, working in the offshore re-supply industry or onboard combined cargo and passenger ships, completed self-report questionnaires. PsyCap was a strong negative predictor of fatigue and positive predictor of high sleep quality (assessed using the Pittsburgh Sleep Quality Index: PSQI; Buysse et al., 1989). In this study, PsyCap was considered a valuable positive resource for seafarers to cope with their isolated and confined working environments and to maintain their general health and well-being.
Extending consideration of the implications of this knowledge, it is possible that a positive psychological construct, such as PsyCap, could play an instrumental role in the relationship between sleep beliefs and well-being. Individuals with higher dysfunctional sleep beliefs express an uncontrollability of their sleep and a preoccupation with the negative consequences of poor sleep (Morin et al., 1993). It seems reasonable to suggest that individuals with higher PsyCap may reject negative sleep cognitions more effectively than individuals with lower PsyCap. That is, dysfunctional sleep beliefs may be negatively related to PsyCap. Moreover, sleep beliefs may influence well-being through the positive cognitive resource of PsyCap. These hypotheses, that dysfunctional sleep beliefs are negatively related to PsyCap, and that PsyCap mediates the relationship between sleep beliefs and well-being, were examined in our current study.
1.3. Theoretical underpinning and study hypotheses
Conservation of Resources (COR) theory (Hobfoll, 2002) suggests that individuals are motivated to build, maintain, and protect four types of resources: personal characteristics (e.g., well-being), physical objects (e.g., home), conditions (e.g., marital status), and energy (e.g., knowledge). In particular, COR theory emphasises the cognitive mechanisms that individuals draw on to positively adapt when their resources are under threat (Querstret et al., 2015). In line with COR theory, PsyCap is considered a positive cognitive mechanism that helps to safeguard individuals against workplace stress and guide their pursuit of optimal psychological functioning (Avey et al., 2011).
Drawing on COR theory (Hobfoll, 2002) and our review of the literature, we proposed that PsyCap would be a positive cognitive resource that buffers the potential threat of sleep beliefs on well-being. We already had evidence of the relations between sleep beliefs and well-being, and between PsyCap and well-being, but not as to whether sleep beliefs were significantly negatively related to PsyCap. We also knew that poor sleep beliefs can affect daily functioning and perceptions of overall well-being; and that higher levels of PsyCap can result in a more positive interpretation of experiences and behaviours. However, we wanted to explore whether PsyCap reduced the negative impact of sleep beliefs on individuals’ sense of well-being. Therefore, to examine the nature of the relationships among key study variables as indicated above, we proposed the following:
H1. That dysfunctional sleep beliefs are significantly and negatively related to PsyCap.
H2. That PsyCap mediates the negative impact of dysfunctional sleep beliefs on well-being.
2. Method
2.1. Participants and procedure
The convenience sample consisted of 123 Australian working adults aged between 20 and 72 years (M = 42.9, SD = 9.9), comprising 67.5% women and 32.5% men. Participants were employed in either full-time (57.7%), part-time (27.6%), or casual/contract positions (14.6%) from a range of occupational sectors, including health (19.5%), government (18.7%), and education (17.9%). Approximately 74.0% of participants had completed tertiary education. Ethical approval was received from Bond University Human Research Ethics Committee before study commencement. This study used a relational survey method. The community participants were recruited via workplace-based email contacts and social media to complete a voluntary and anonymous self-report online survey, which required opt-in consent and a minimum of 18 years of age to participate.
2.2. Measures
Demographic questions were asked regarding gender, age, highest education level, and employment status. Four empirically established scales were also completed (see next sections).
2.2.1. Dysfunctional Beliefs and Attitudes about Sleep Scale (DBAS-16; Morin et al., 2007)
The DBAS-16 is widely used to assess the strength of endorsement of sleep-disruptive beliefs (Carney et al., 2010). Adapted from the original 30-item DBAS (Morin, 1993), the DBAS-16 consists of 16 items that represent four factors of sleep-related cognitions: 1) insomnia consequences; 2) worry and helplessness; 3) expectations; and 4) attributions of insomnia. Respondents rate their agreement with each statement on a 10-point Likert scale anchored by strongly disagree (1) and strongly agree (10). The mean DBAS-16 score is the sum of total item scores divided by 16. Higher DBAS-16 scores (≥6) indicate stronger endorsement of dysfunctional sleep beliefs. The DBAS-16 significantly correlates with self-report measures of insomnia severity and depression, supporting the scale's convergent validity (Morin et al., 2007). The DBAS-16 has good internal consistency in good sleepers and insomnia patient groups (α = .80 and .82, respectively; Carney et al., 2007), and presented a good alpha of .86 in the current sample.
2.2.2. Psychological Capital Questionnaire (PCQ-24; Luthans et al., 2007)
The PCQ-24 is a standard measure of PsyCap within organisational psychology (Dawkins et al., 2013), comprising selected items from empirically established measures of hope (Snyder et al., 1996), optimism (Scheier and Carver, 1985), resilience (Wagnild and Young, 1993), and self-efficacy (Parker, 1998). To reflect the state-like quality of PsyCap, respondents consider how they feel “right now” when responding to 24 statements using a 6-point Likert scale ranging from strongly disagree (1) to strongly agree (6). Three negatively framed questions are reverse scored, and item scores are summed to produce a total score. Higher PCQ-24 scores indicate higher levels of PsyCap. The PCQ-24 has excellent internal reliability in employee and academic samples (α = .89 and .91, respectively; Luthans et al., 2008), presenting an excellent alpha of .93 in the current sample.
2.2.3. Psychological well-being scale (PWB-42; Ryff, 1989)
The PWB-42 assesses six dimensions of psychological well-being: autonomy, self-acceptance, positive interpersonal relations, personal growth, life purpose, and environmental mastery. Respondents rate their response to seven statements per dimension, ranging from disagree strongly (1) to agree strongly (6). Twenty positively worded items and 22 negatively worded items (reverse scored) are summed to produce a total PWB-42 score, with higher scores indicating higher psychological well-being. The PWB-42 has been used extensively to examine psychological well-being correlates (e.g., changing sleep patterns, sleep habits, subjective sleep quality; Friedman et al., 2007). The PWB-42 presented excellent internal consistency in the current study (α = .93), consistent with previous reliabilities (e.g., α = .93; Gibson and Hicks, 2018).
2.2.4. Marlowe-Crowne social desirability scale (MCSDS-13; Crowne and Marlowe, 1960)
Social desirability response bias was operationalised using the 13-item MCSDS. The scale has good internal reliability (α = .77; Barger, 2002), with an adequate alpha of .73 in the current sample.
3. Results
3.1. Preliminary analyses
The final sample of 123 exceeded the minimum size determined by a priori power analysis using three predictors (i.e., PsyCap, sleep beliefs, and their interaction) to detect a medium effect (α = .05, β = .20). The assumptions of normality, linearity, and homoscedasticity of residuals were met. The absence of significant multivariate outliers, and tolerance values and bivariate correlations between key study variables, suggested that multicollinearity would not interfere with the interpretation of regression analyses. Further, predictor data was mean centred prior to analyses to help control for multicollinearity (Aiken and West, 1991; Cohen et al., 2014).
Sample descriptive statistics and zero-order correlations are presented in Table 1. Significant relationships between the variables were in the expected direction. Of note was the significant negative correlation between dysfunctional sleep beliefs and psychological capital (PsyCap) as this relationship had not previously been examined to the authors’ knowledge.
Table 1.
Means, standard deviations, and zero-order correlations between key study variables (N = 123).
| Variable | M | SD | 1. | 2. | 3. | 4. |
|---|---|---|---|---|---|---|
| 1. Dysfunctional Sleep Beliefs | 4.16 | 1.47 | - | |||
| 2. Psychological Capital | 112.90 | 15.15 | -.46∗∗∗ | - | ||
| 3. Psychological Well-being | 190.63 | 24.42 | -.37∗∗∗ | .74∗∗∗ | - | |
| 4. Social Desirability | 8.03 | 2.92 | -.35∗∗∗ | .34∗∗∗ | .33∗∗∗ | - |
∗p < .05. ∗∗p < .01. ∗∗∗p < .001.
3.2. Covariates - gender and social desirability
Gender differences among key study variables were analysed using four independent samples t-tests (two-tailed). Results indicated that there were no statistically significant gender differences (for the 83 women and 40 men in the sample) for any of the four variables: though women had slightly lower PsyCap levels than men, t(121) = -1.16, p = .247; and slightly higher dysfunctional sleep beliefs, t(121) = 1.84, p = .068; higher psychological well-being, t(121) = 0.32, p = .748; and, higher social desirability scores, t(121) = 1.08, p = .284. Though these differences are all nonsignificant, it has been traditional to include gender as a covariate or variate in similar studies (e.g., Ered et al., 2018; Stratman and Youssef-Morgan, 2019; Tian et al., 2020); and, also given that in sum gender differences might still be affecting results, we decided to control for gender in the regression models. In addition, we also controlled for social desirability, given social desirability was significantly associated with each of psychological well-being, r(121) = .33, p < .001, PsyCap, r(121) = .34, p < .001, and dysfunctional sleep beliefs, r(121) = -.35, p < .001, though not with gender in this study, thus satisfying also the criterion of covariate independence (Tabachnick and Fidell, 2014).
3.3. Mediation analysis
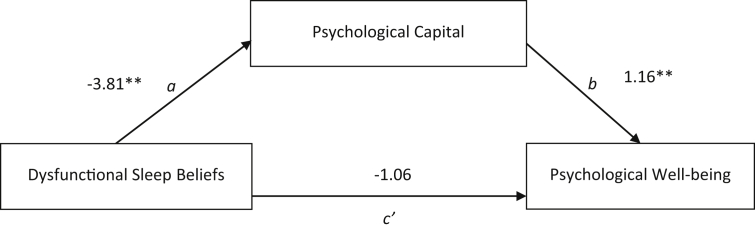
A mediation analysis was conducted in SPSS using the PROCESS macro Version 3.4 (Hayes, 2012) to assess the total effect (c), direct effect (c'), and bootstrapped bias-corrected 95% confidence intervals (CI) of the indirect effect (ab) based on 5,000 bootstrapped samples. Alpha was set at .05 to determine the statistical significance of each path. The mediation model is displayed in Figure 1.
Figure. 1.
Mediation of dysfunctional sleep beliefs and psychological well-being by psychological capital.
The relationship between sleep beliefs and well-being (path c) was significant and negative, after controlling for gender and social desirability; B = -5.48, SE = 1.62, p = .001, 95% CI [-8.69, -2.27]. Sleep beliefs accounted for 18.5% of variance in well-being; R2 = .18, F (3, 119) = 8.98, p < .001. Additionally, social desirability covariate accounted for significant variance in the model, B = 1.78, SE = 0.75, p = .020, 95% CI [0.29, 3.26], the gender covariate accounted for nonsignificant variance, B = 3.08, SE = 4.42, p = .488, 95% CI [-5.68, 11.83].
The relationship between sleep beliefs and PsyCap (path a) was significant and negative, such that higher dysfunctional sleep beliefs scores were associated with lower PsyCap scores; B = -3.81, SE = 0.96, p < .001, 95% CI [-5.71, -1.91]. Therefore, the first hypothesis was supported since sleep beliefs and PsyCap were significantly and negatively related. The relationship between PsyCap and well-being (path b) was significant and positive, indicating that higher levels of PsyCap were associated with higher levels of well-being; B = 1.16, SE = 0.11, p < .001, 95% CI [0.94, 1.38]. The mediation model accounted for 56.8% of variance in well-being; R2 = .57, F (4, 119) = 38.78, p < .001 after controlling for gender, B = 5.65, SE = 3.24, p = .084, 95% CI [-0.78, 12.07], and social desirability, B = 0.43, SE = 0.56, p = .448, 95% CI [-0.69, 1.55]. The second hypothesis, predicting that the direct effect of sleep beliefs predicted unique variance in well-being holding the levels of PsyCap consistent (path c’), was supported by the model: B = -1.06, SE = 1.26, p = .401, 95% CI [-3.56, 1.43]. PsyCap significantly mediated the relationship between sleep beliefs and well-being. The indirect effect (path ab) of the relationship between sleep beliefs and well-being through PsyCap was significant: B = -4.42, SE = 1.16, boot 95% CI [-6.77, -2.10]. Results of the effect size estimate suggested that -0.18 coefficient change in the ab coefficient would result in a 1 SD increase in well-being. Of note, mediation analysis using the PROCESS macro (Hayes, 2012) yielded the same result as Baron and Kenny's (1986) approach to mediation and Sobel's (1982) test of significance. Unstandardised (B) regression coefficients, 95% confidence intervals, and R2 values for the mediation model are presented in Table 2.
Table 2.
Results from mediation analysis.
| B | SE | t | p | Bootstrapped 95% CI |
R2 |
||
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Predicting Mediator: PsyCap | .24 | ||||||
| Constant | 123.09 | 6.87 | 17.92 | <.001 | 109.49 | 136.69 | |
| Main Predictor | |||||||
| Dysfunctional Sleep Beliefs | -3.81 | 0.96 | -3.98 | <.001 | -5.71 | -1.91 | |
| Controls | |||||||
| Gender | -2.21 | 2.61 | -0.85 | .399 | -7.39 | 2.96 | |
| Social Desirability | 1.16 | 0.44 | 2.61 | .010 | .281 | 2.04 | |
| Predicting Outcome: Well-being | .57 | ||||||
| Constant | 51.29 | 16.33 | 3.14 | .002 | 18.95 | 83.63 | |
| Main Predictors | |||||||
| Dysfunctional Sleep Beliefs | -1.06 | 1.26 | -0.84 | .401 | -3.56 | 1.43 | |
| PsyCap | 1.16 | 0.11 | 10.23 | <.001 | 0.94 | 1.38 | |
| Controls | |||||||
| Gender | 5.65 | 3.24 | 1.74 | .084 | -0.77 | 12.07 | |
| Social Desirability | 0.43 | 0.56 | 0.76 | .448 | -0.69 | 1.55 | |
| Direct Effect | |||||||
| Sleep Beliefs → Well-being | -1.06 | 1.26 | -0.84 | .401 | -3.56 | 1.43 | |
| Indirect Effect | |||||||
| Sleep Beliefs → PsyCap → Well-being | -4.42 | 1.16 | - | - | -6.77 | -2.10 | |
Note. This mediation model was tested using model 4 of the PROCESS macro in SPSS. Bootstrapped 95% CI = 95% confidence interval derived from 5,000 bootstrapped models. SE = standard error; LL = lower limit; UL = upper limit. Unstandardised coefficients (B) are reported.
4. Discussion
The present study identified a notable gap in the literature regarding the interrelations between dysfunctional sleep beliefs, psychological capital (PsyCap), and psychological well-being. Consistent with the first hypothesis, dysfunctional sleep beliefs were significantly and negatively related to PsyCap. This finding contributes new understanding of both constructs. In support of the second hypothesis, PsyCap mediated the impact of dysfunctional sleep beliefs on psychological well-being. Results of the mediated model assessed suggested that: higher dysfunctional sleep beliefs predicted lower well-being; PsyCap positively predicted well-being; and, the strength of the relationship between sleep beliefs and well-being was nonsignificant when PsyCap was entered into the model.
While the relationship between dysfunctional sleep beliefs and PsyCap has not been previously reported in the literature, this negative linear relationship had been inferred. Prior research has identified negative links between dysfunctional sleep beliefs and various forms of cognitive appraisals, including subjective appraisals of sleep quality and well-being (Brown et al., 2002; Edinger et al., 2000; Lemola et al., 2013). Based on such prior findings, it seemed plausible that maladaptive sleep appraisals would negatively predict a positive cognitive resource such as PsyCap. Present results supported this hypothesis. Therefore, the current finding has added to the knowledge of both sleep beliefs and PsyCap constructs. Further, since training programs can help modify dysfunctional sleep beliefs (Morin et al., 2002; Thakral et al., 2020), future experimental research could explore whether PsyCap training, in particular, can minimise the anticipated impact of poor sleep quality as part of targeted sleep education programs. The process of minimising dysfunctional sleep beliefs may support the development of more realistic and optimistic sleep expectations (Avey et al., 2009), which, in turn, could help to reduce sleep difficulties and improve psychological well-being.
Our findings are consistent with prior research that has detailed the relationships between PsyCap and psychological well-being (e.g., Avey et al., 2010; Luthans and Youssef-Morgan, 2017), and between sleep beliefs and positive psychological functioning (e.g., Brown et al., 2002; Gellis and Lichstein, 2009). Moreover, our novel study has indicated support for unique relations among PsyCap, sleep beliefs, and psychological well-being. Current results are consistent with Conservation of Resources (COR) theory (Hobfoll, 2002). COR theory suggests that positive cognitive mechanisms provide adaptive psychological responses when primary resources, such as well-being, are threatened (Querstret et al., 2015). Present findings support prior research that has drawn on COR theory to delineate the role of PsyCap in protecting against stress and anxiety (Avey et al., 2010). In the current sample, PsyCap significantly mediated the threat posed by dysfunctional sleep beliefs to the primary resource of psychological well-being. This strong evidence of mediation has provided preliminary nonexperimental support to justify future evaluation. Replication of path coefficient results may confirm that findings were not a result of sampling error.
To address the issue of collinearity between correlated predictor variables, data was mean centred (Aiken and West, 1991). Consequently, results of the mediation model examined may be seen to suggest a causal effect of PsyCap in reducing the negative impact of sleep beliefs on well-being. However, due to the cross-sectional correlational design of the present study, such causal inferences cannot be made from present findings. Future research could use an experimental design to assess whether PsyCap directly impacts the appraisal of dysfunctional sleep-related cognitions, which would help to control for construct overlaps and confirm the relevance of PsyCap interventions in addressing sleep problems.
4.1. Methodological considerations
The current study had several strengths. Firstly, PsyCap has not previously been studied in this context, and the study provides strong evidence on the relationships examined. Secondly, the community sample represented a cross-section of employment types and organisational industries, outside more commonly assessed university students and clinical samples. Therefore, the current composite sample was suitable for identifying general trends. Thirdly, constructs were operationalised using self-reported data generated from validated measures, which provided an additional strength of the current study. Finally, the current study controlled for social desirability response bias using the MCSDS-13 (Crowne and Marlowe, 1960).
The current research had limitations. Although the Dysfunctional Beliefs and Attitudes about Sleep Scale (DBAS-16; Morin et al., 2007), Psychological Capital Questionnaire (PCQ-24; Luthans et al., 2007), and Psychological Well-being Scale (PWB-42; Ryff, 1989) are multidimensional instruments, total scale scores were analysed. Study variables were assessed as higher-order constructs in line with the research presented. Further, analysis of the total scores enabled a clear examination of the relationships between key study variables. It could be, however, that sub-variables within PsyCap and psychological well-being are especially relevant. Further studies with larger numbers may be needed to examine this possibility. Another potential limitation in our study is that variables were measured concurrently using the same medium, which can lead to common method variance (Podsakoff et al., 2003). Although the current study employed empirically established scales to address this potential threat to internal validity, temporal separation of independent and dependent variable data collection may have reduced the threat of artificial covariance (Podsakoff et al., 2003).
The current study presented potential confounds. Previous research has proposed that unhelpful sleep beliefs influence stress reactivity (Drake et al., 2004; Palagini et al., 2016). Given the associations between sleep-related cognitions and stress, and the role of stress when resources are under threat, as highlighted in Conservation of Resources theory (Hobfoll, 2002), sleep reactivity could have been assessed and included as a covariate in regression analyses. Furthermore, low psychological well-being has strong links to mood disorders and anxiety (Morin et al., 2007). Notably, 50% of adults with depression have comorbid insomnia and associated sleep disturbance (Britt et al., 2010). Further studies addressing depression and anxiety comorbidities may help to increase the generalisability of the study findings to non-clinical populations.
4.2. Future directions
The present research has contributed new insight to the literature. Current results have delineated a previously unreported relationship between dysfunctional sleep beliefs and psychological capital (PsyCap) and identified the mediating effect of PsyCap on the relationship between sleep beliefs and well-being. The literature suggests that PsyCap's impact can vary based on specific sample attributes such as employment industry. For example, PsyCap tends to influence employee outcomes more in service industries than within industrial sectors (Avey et al., 2011; Luthans and Youssef-Morgan, 2017). Therefore, the current study may warrant replication in specific samples (e.g., employee, organisation-based) to aid the generalisability of findings. Furthermore, since training programs can develop PsyCap (Dello Russo and Stoykova, 2015; Eidelman et al., 2016; Luthans et al., 2014), future experimental research could explore the efficacy of PsyCap training within sleep-hygiene education programs. Such intervention may help develop more adaptive sleep expectations, reduce sleep difficulties, and enhance psychological well-being outcomes.
5. Conclusion
In the present study, dysfunctional sleep beliefs significantly and negatively predicted PsyCap (involving resilience, hope, optimism, and self-efficacy), and PsyCap mediated the relationship between sleep beliefs and well-being. Findings support Conservation of Resources theory, in which the positive cognitive resource of PsyCap reduced the negative impact of sleep beliefs on well-being.
Declarations
Author contribution statement
D.L. Sabot, R.E. Hicks: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- Aiken L.S., West S.G. Sage; 1991. Multiple Regression: Testing and Interpreting Interactions. [Google Scholar]
- Alarcon G.M., Bowling N.A., Khazon S. Great expectations: a meta-analytic examination of optimism and hope. Pers. Indiv. Differ. 2013;54(7):821–827. [Google Scholar]
- Avey J.B., Luthans F., Jensen S. Psychological capital: a positive resource for combating employee stress and turnover. Hum. Resour. Manag. 2009;48(5):677–693. [Google Scholar]
- Avey J.B., Luthans F., Smith R.M., Palmer N.F. Impact of positive psychological capital on employee well-being over time. J. Occup. Health Psychol. 2010;15(1):7–28. doi: 10.1037/a0016998. [DOI] [PubMed] [Google Scholar]
- Avey J.B., Reichard R.J., Luthans F., Mhatre K.H. Meta-analysis of the impact of positive psychological capital on employee attitudes, behaviors, and performance. Hum. Resour. Dev. Q. 2011;22(2):127–152. [Google Scholar]
- Bakker A.B., Schaufeli W.B., Leiter M.P., Taris T.W. Work engagement: an emerging concept in occupational health psychology. Work. Stress. 2008;22(3):187–200. [PubMed] [Google Scholar]
- Barger S.D. The Marlowe-Crowne affair: short forms, psychometric structure, and social desirability. J. Pers. Assess. 2002;79(2):286–305. doi: 10.1207/S15327752JPA7902_11. [DOI] [PubMed] [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Berkman P.L. Life stress and psychological well-being: a replication of Langner's analysis in the midtown Manhattan study. J. Health Soc. Behav. 1971;12(1):35–45. [PubMed] [Google Scholar]
- Bluestein D., Healey A., Rutledge C. Acceptability of behavioral treatments for insomnia. J. Am. Board Fam. Med. 2011;24(3):272–280. doi: 10.3122/jabfm.2011.03.100246. [DOI] [PubMed] [Google Scholar]
- Britt H., Miller G.C., Charles J., Henderson J., Bayram C., Pan Y., Valenti L., Harrison C., O’Halloran J., Fahridin S. Vol. 27. General Practice Series; 2010. https://www.aihw.gov.au/getmedia/9fa2809a-5c69-4f30-8162-912cddd9dccc/12118.rtf.aspx?inline=true (General Practice Activity in Australia 2009–10). [Google Scholar]
- Brown F., Buboltz W., Soper B. Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behav. Med. 2002;28(1):33–38. doi: 10.1080/08964280209596396. [DOI] [PubMed] [Google Scholar]
- Buysse D., Reynolds C., Monk T., Berman S., Kupfer D. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatr. Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Calkins A., Hearon B., Capozzoli M., Otto M. Psychosocial predictors of sleep dysfunction: the role of anxiety sensitivity, dysfunctional beliefs, and neuroticism. Behav. Sleep Med. 2013;11(2):133–143. doi: 10.1080/15402002.2011.643968. [DOI] [PubMed] [Google Scholar]
- Carney C.E., Edinger J.D. Identifying critical beliefs about sleep in primary insomnia. Sleep. 2006;29(3):342–350. doi: 10.1093/sleep/29.3.342. [DOI] [PubMed] [Google Scholar]
- Carney C.E., Edinger J.D., Manber R., Garson C., Segal Z.V. Beliefs about sleep in disorders characterized by sleep and mood disturbance. J. Psychosom. Res. 2007;62(2):179–188. doi: 10.1016/j.jpsychores.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Carney C.E., Edinger J.D., Morin C.M., Manber R., Rybarczyk B., Stepanski E.J., Wright H., Lack L. Examining maladaptive beliefs about sleep across insomnia patient groups. J. Psychosom. Res. 2010;68(1):57–65. doi: 10.1016/j.jpsychores.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver C.S., Scheier M.F., Segerstrom S.C. Optimism. Clin. Psychol. Rev. 2010;30(7):879–889. doi: 10.1016/j.cpr.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen P., West S.G., Aiken L.S. Psychology Press; 2014. Applied Multiple Regression/correlation Analysis for the Behavioral Sciences. [Google Scholar]
- Crowne D.P., Marlowe D. A new scale of social desirability independent of psychopathology. J. Consult. Psychol. 1960;24(4):349–354. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- Cunnington D., Junge M.F., Fernando A.T. Insomnia: prevalence, consequences and effective treatment. Med. J. Aust. 2013;199:S36–S40. doi: 10.5694/mja13.10718. [DOI] [PubMed] [Google Scholar]
- Dawkins S., Martin A., Scott J., Sanderson K. Building on the positives: a psychometric review and critical analysis of the construct of psychological capital. J. Occup. Organ. Psychol. 2013;86(3):348–370. [Google Scholar]
- Dello Russo S., Stoykova P. Psychological capital intervention (PCI): a replication and extension. Hum. Resour. Dev. Q. 2015;26(3):329–347. [Google Scholar]
- Demerouti E., van Eeuwijk E., Snelder M., Wild U. Assessing the effects of a “personal effectiveness” training on psychological capital, assertiveness and self-awareness using self-other agreement. Career Dev. Int. 2011;16(1):60–81. [Google Scholar]
- Drake C., Richardson G., Roehrs T., Scofield H., Roth T. Vulnerability to stress-related sleep disturbance and hyperarousal. Sleep. 2004;27(2):285–291. doi: 10.1093/sleep/27.2.285. [DOI] [PubMed] [Google Scholar]
- Edinger J.D., Fins A.I., Glenn D.M., Sullivan R.J., Jr., Bastian L.A., Marsh G.R., Dailey D., Hope T.V., Young M., Shaw E., Vasilas D. Insomnia and the eye of the beholder: are there clinical markers of objective sleep disturbances among adults with and without insomnia complaints? J. Consult. Clin. Psychol. 2000;68(4):586–593. [PubMed] [Google Scholar]
- Eidelman P., Talbot L., Ivers H., Bélanger L., Morin C.M., Harvey A.G. Change in dysfunctional beliefs about sleep in behavior therapy, cognitive therapy, and cognitive-behavioral therapy for insomnia. Behav. Ther. 2016;47(1):102–115. doi: 10.1016/j.beth.2015.10.002. [DOI] [PubMed] [Google Scholar]
- Ered A., Cooper S., Ellman L. Sleep quality, psychological symptoms, and psychotic-like experiences. J. Psychiatr. Res. 2018;98:95–98. doi: 10.1016/j.jpsychires.2017.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertosun Ö.G., Erdil O., Deniz N., Alpkan L. Positive psychological capital development: a field study by the Solomon four group design. Int. Bus. Res. 2015;8(10):102–111. [Google Scholar]
- Fichten C., Creti S., Amsel L., Brender R., Weinstein W., Libman N. Poor sleepers who do not complain of insomnia: myths and realities about psychological and lifestyle characteristics of older good and poor sleepers. J. Behav. Med. 1995;18(2):189–223. doi: 10.1007/BF01857869. [DOI] [PubMed] [Google Scholar]
- Friedman E.M., Love G.D., Davidson R., Urry H., Rosencranz M., Singer B.H., Ryff C.D. Socioeconomic status predicts subjective and objective sleep quality in aging women. Psychosom. Med. 2007;69(7):682–691. doi: 10.1097/PSY.0b013e31814ceada. [DOI] [PubMed] [Google Scholar]
- Gellis L., Lichstein K. Sleep hygiene practices of good and poor sleepers in the United States: an internet-based study. Behav. Ther. 2009;40(1):1–9. doi: 10.1016/j.beth.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Gibson A., Hicks R.E. Psychological capital and core self-evaluations in the workplace: impacts on well-being. Int. J. Psychol. Stud. 2018;10(2):15–24. [Google Scholar]
- Gingerich S.B., Seaverson E.L., Anderson D.R. Association between sleep and productivity loss among 598,676 employees from multiple industries. Am. J. Health Promot. 2018;32(4):1091–1094. doi: 10.1177/0890117117722517. [DOI] [PubMed] [Google Scholar]
- Goldberg D.P. Oxford University Press; 1972. The Detection of Psychiatric Illness by Questionnaire. [Google Scholar]
- Goldberg D.P., Hillier V.F. A scaled version of the general health questionnaire. Psychol. Med. 1979;9(1):139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- Gyu Park J., Sik Kim J., Yoon S., Joo B. The effects of empowering leadership on psychological well-being and job engagement. Leader. Organ. Dev. J. 2017;38(3):350–367. [Google Scholar]
- Hamilton N.A., Gallagher M.W., Preacher K.J., Stevens N., Nelson C.A., Karlson C., McCurdy D. Insomnia and well-being. J. Consult. Clin. Psychol. 2007;75(6):939–946. doi: 10.1037/0022-006X.75.6.939. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. 2012. PROCESS: A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling.http://www.afhayes.com/public/process2012.pdf [Whitepaper] [Google Scholar]
- Heled E., Somech A., Waters L. Psychological capital as a team phenomenon: mediating the relationship between learning climate and outcomes at the individual and team levels. J. Posit. Psychol. 2016;11(3):303–314. [Google Scholar]
- Hicks R.E., Knies E.M. Psychological capital, adaptability, coping with change, and employee engagement in a multinational company. J. Int. Bus. Discipl. 2015;10(2):36–51. https://faculty.utrgv.edu/louis.falk/jibd/JIBDnov15.pdf [Google Scholar]
- Hobfoll S.E. Social and psychological resources and adaptation. Rev. Gen. Psychol. 2002;6(4):307–324. [Google Scholar]
- Howell A.J., Digdon N.L., Buro K. Mindfulness predicts sleep-related self-regulation and well-being. Pers. Indiv. Differ. 2010;48(4):419–424. [Google Scholar]
- Hystad S.W., Eid J. Sleep and fatigue among seafarers: the role of environmental stressors, duration at sea and psychological capital. Safety Health Work. 2016;7(4):363–371. doi: 10.1016/j.shaw.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin L., Zhou J., Peng H., Ding S., Yuan H. Investigation on dysfunctional beliefs and attitudes about sleep in Chinese college students. Neuropsychiatric Dis. Treat. 2018;14:1425–1432. doi: 10.2147/NDT.S155722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kao C.C., Huang C.J., Wang M.Y., Tsai P.S. Insomnia: prevalence and its impact on excessive daytime sleepiness and psychological well-being in the adult Taiwanese population. Qual. Life Res. 2008;17(8):1073–1080. doi: 10.1007/s11136-008-9383-9. [DOI] [PubMed] [Google Scholar]
- Lemola S., Ledermann T., Friedman E., Gamble K. Variability of sleep duration is related to subjective sleep quality and subjective well-being: an actigraphy study. PloS One. 2013;8(8) doi: 10.1371/journal.pone.0071292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linton S.J., Kecklund G., Franklin K.A., Leissner L.C., Sivertsen B., Lindberg E., Svensson A.C., Hansson S.O., Sundin Ö., Hetta J., Björkelund C., Hall C. The effect of the work environment on future sleep disturbances: a systematic review. Sleep Med. Rev. 2015;23(2):10–19. doi: 10.1016/j.smrv.2014.10.010. [DOI] [PubMed] [Google Scholar]
- Lundh L. The role of acceptance and mindfulness in the treatment of insomnia. J. Cognit. Psychother. 2005;19(1):29–39. [Google Scholar]
- Lupșa D., Vîrga D., Maricuțoiu L., Rusu A. Increasing psychological capital: a pre-registered meta-analysis of controlled interventions. Appl. Psychol. 2019 [Google Scholar]
- Luthans F. The need for and meaning of positive organizational behavior. J. Organ. Behav.: Int. J. Indus. Occu. Organ. Psychol. Behav. 2002;23(6):695–706. [Google Scholar]
- Luthans F., Avey J., Avolio B., Peterson S. The development and resulting performance impact of positive psychological capital. Hum. Resour. Dev. Q. 2010;21(1):41–67. [Google Scholar]
- Luthans F., Avolio B.J., Avey J.B., Norman S.M. Positive psychological capital: measurement and relationship with performance and satisfaction. Person. Psychol. 2007;60(3):541–572. [Google Scholar]
- Luthans B.C., Luthans K.W., Avey J.B. Building the leaders of tomorrow: the development of academic psychological capital. J. Leader. Organ Stud. 2014;21(2):191–199. [Google Scholar]
- Luthans F., Norman S.M., Avolio B.J., Avey J.B. The mediating role of psychological capital in the supportive organizational climate-employee performance relationship. J. Organ. Behav.: Int. J. Indus. Occu. Organ. Psychol. Behav. 2008;29(2):219–238. [Google Scholar]
- Luthans F., Youssef-Morgan C.M. Psychological capital: an evidence-based positive approach. Ann. Rev. Organ. Psychol. Organ. Behav. 2017;4:339–366. [Google Scholar]
- Lyubomirsky S., King L., Diener E. The benefits of frequent positive affect: does happiness lead to success? Psychol. Bull. 2005;131(6):803–855. doi: 10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- Morin C.M. Guilford Press; 1993. Treatment Manuals for Practitioners. Insomnia: Psychological Assessment and Management. [Google Scholar]
- Morin C.M., Stone J., Trinkle D., Mercer J., Remsberg S. Dysfunctional beliefs and attitudes about sleep among older adults with and without insomnia complaints. Psychol. Aging. 1993;8(3):463–467. doi: 10.1037//0882-7974.8.3.463. [DOI] [PubMed] [Google Scholar]
- Morin C.M., Blais F., Savard J. Are changes in beliefs and attitudes about sleep related to sleep improvements in the treatment of insomnia? Behav. Res. Ther. 2002;40(7):741–752. doi: 10.1016/s0005-7967(01)00055-9. [DOI] [PubMed] [Google Scholar]
- Morin C.M., Vallières A., Ivers H. Dysfunctional beliefs and attitudes about sleep (DBAS): validation of a brief version (DBAS-16) Sleep. 2007;30(11):1547–1554. doi: 10.1093/sleep/30.11.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer F., Aziz S., Wuensch K. From workaholism to burnout: psychological capital as a mediator. Int. J. Workplace Health Manag. 2017;10(3):213–227. [Google Scholar]
- Norra C., Richter N., Juckel G. Sleep disturbances and suicidality: a common association to look for in clinical practise and preventive care. Eur. Assoc. Predict. Prevent. Personal. Med. (EPMA) J. 2011;2(3):295–307. doi: 10.1007/s13167-011-0101-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong J., Shapiro S., Manber R. Combining mindfulness meditation with cognitive-behavior therapy for insomnia: a treatment-development study. Behav. Ther. 2008;39(2):171–182. doi: 10.1016/j.beth.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palagini L., Faraguna U., Mauri M., Gronchi A., Morin C.M., Riemann D. Association between stress-related sleep reactivity and cognitive processes in insomnia disorder and insomnia subgroups: preliminary results. Sleep Med. 2016;14(6):101–107. doi: 10.1016/j.sleep.2015.10.020. [DOI] [PubMed] [Google Scholar]
- Parker S.K. Enhancing role breadth self-efficacy: the roles of job enrichment and other organizational interventions. J. Appl. Psychol. 1998;83(6):835–852. doi: 10.1037/0021-9010.83.6.835. [DOI] [PubMed] [Google Scholar]
- Peltz J., Rogge R. The moderating role of parents’ dysfunctional sleep-related beliefs among associations between adolescents’ pre-bedtime conflict, sleep quality, and their mental health. J. Clin. Sleep Med. 2019;15(2):265–274. doi: 10.5664/jcsm.7630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson S., Luthans F., Avolio B., Walumbwa F., Zhang Z. Psychological capital and employee performance: a latent growth modeling approach. Person. Psychol. 2011;64(2):427–450. [Google Scholar]
- Phelan C.H., Love G.D., Ryff C.D., Brown R.L., Heidrich S.M. Psychosocial predictors of changing sleep patterns in aging women: a multiple pathway approach. Psychol. Aging. 2010;25(4):858–866. doi: 10.1037/a0019622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsakoff P.M., MacKenzie S.B., Lee J.Y., Podsakoff N.P. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Querstret D., Cropley M., Kruger P., Heron R. Assessing the effect of a cognitive behaviour therapy (CBT)-based workshop on work-related rumination, fatigue, and sleep. Eur. J. Work. Organ. Psychol. 2015;25(1):1–18. [Google Scholar]
- Rosekind M.R., Gregory K.B., Mallis M.M., Brandt S.L., Seal B., Lerner D. The cost of poor sleep: workplace productivity loss and associated costs. J. Occup. Environ. Med. 2010;52(1):91–98. doi: 10.1097/JOM.0b013e3181c78c30. [DOI] [PubMed] [Google Scholar]
- Ryff C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Pers. Soc. Psychol. 1989;57(6):1069–1081. [Google Scholar]
- Salanova M., Ortega-Maldonado A. Psychological capital development in organizations: an integrative review of evidence-based intervention programs. In: Van Zyl L., Rothmann Sr S., editors. Positive Psychological Intervention Design and Protocols for Multi-Cultural Contexts. Springer; Cham: 2019. [Google Scholar]
- Sánchez-Ortuño M., Edinger J. A penny for your thoughts: patterns of sleep-related beliefs, insomnia symptoms and treatment outcome. Behav. Res. Ther. 2010;48(2):125–133. doi: 10.1016/j.brat.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier M.F., Carver C.S. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4(3):219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- Snyder C.R., Sympson S.C., Ybasco F.C., Borders T.F., Babyak M.A., Higgins R.L. Development and validation of the state hope scale. J. Pers. Soc. Psychol. 1996;70(2):321–335. doi: 10.1037//0022-3514.70.2.321. [DOI] [PubMed] [Google Scholar]
- Sobel M.E. Asymptotic confidence intervals for indirect effects in structural equation models. Socio. Methodol. 1982;13:290–312. [Google Scholar]
- Stajkovic A. Development of a core confidence-higher order construct. J. Appl. Psychol. 2006;91(6):1208–1224. doi: 10.1037/0021-9010.91.6.1208. [DOI] [PubMed] [Google Scholar]
- Stratman J., Youssef-Morgan C. Can positivity promote safety? Psychological capital development combats cynicism and unsafe behavior. Saf. Sci. 2019;116:13–25. [Google Scholar]
- Tabachnick B.G., Fidell L.S. sixth ed. Pearson Education; 2014. Using Multivariate Statistics. [Google Scholar]
- Thakral M., Von Korff M., McCurry S.M., Morin C.M., Vitiello M.V. Changes in dysfunctional beliefs about sleep after cognitive behavioral therapy for insomnia: a systematic literature review and meta-analysis. Sleep Med. Rev. 2020;49:101230. doi: 10.1016/j.smrv.2019.101230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian F., Shu Q., Cui Q., Wang L., Liu C., Wu H. The mediating role of psychological capital in the relationship between occupational stress and fatigue: a cross-sectional study among 1,104 Chinese physicians. Front. Publ. Health. 2020;8(12) doi: 10.3389/fpubh.2020.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagnild G.M., Young H.M. Development and psychometric evaluation of the resilience scale. J. Nurs. Meas. 1993;1(2):165–178. https://www.ncbi.nlm.nih.gov/pubmed/7850498 [PubMed] [Google Scholar]
- Yang C.M., Hung C.Y., Lee H.C. Stress-related sleep vulnerability and maladaptive sleep beliefs predict insomnia at long-term follow-up. J. Clin. Sleep Med. 2014;10(9):997–1001. doi: 10.5664/jcsm.4036. [DOI] [PMC free article] [PubMed] [Google Scholar]