Abstract
Objective
Lumbar spine stenosis is a common disease with a prevalence progressively increasing due to the aging of the population. Despite many papers having been published over the last decades, there still remain many doubts regarding its natural history and appropriate treatment. To overcome these problems and reach some globally accepted recommendations, the World Federation of Neurosurgical Society Spine Committee organized a consensus conference on this topic. This paper describes recommendations about the efficacy of surgical decompression, the difference between surgical techniques, and complications of surgery.
Methods
World Federation of Neurosurgical Society Spine Committee aimed to standardize clinical practice worldwide as much as possible and held a 2-round consensus conference on lumbar spinal stenosis. A team of expert spine surgeons reviewed literature regarding surgical treatment from over the last 10 years, and then drafted and voted on some statements based on the presented literature.
Results
Ten statements were voted. The committee agreed on the effectiveness of surgical decompression in patients with moderate-to-severe symptoms or with neurologic deficits. There was no consensus on the best surgical technique and, in particular, about the equivalence of microscopic techniques and an open approach. Regarding complications, we agreed that the most frequent complications are incidental durotomy and general complications in the elderly.
Conclusions
Surgical decompression represents the treatment of choice for symptomatic lumbar spinal stenosis with a low complication rate. However, which surgical technique is the best is still under debate. Further studies with standardized outcome measures are needed to understand the real complication rate and frequency of different unwanted events.
Key words: Complications, Decompressive surgery, Laminectomy, Lumbar spine stenosis, MISS, Spine surgery, Surgical treatment
Abbreviations and Acronyms: ID, Incidental durotomy; LSS, Lumbar spinal stenosis; MIS, Minimally invasive surgery; RCT, Randomized controlled trial; VAS, Visual analogue scale; WFNS, World Federation of Neurosurgical Societies
Introduction
Degenerative lumbar spine stenosis is a slow progressive spinal disease common in the elderly, characterized by ligamentum flavum hypertrophy, bulging of the intervertebral disc, and facet joint thickening with arthropathy eventually leading to compression of the neural elements.
The pathology and clinical presentation have been well known since the 1950s, whereas the first reports of surgical treatment described as decompression of the nerve roots by removal of the posterior bony and ligamentous elements were made in 1977.1,2
In addition, Wiltse et al3 stressed the importance of foraminal decompression in association with central decompression.
Although many papers have been published on surgical treatment and approaches over the years, there still remain many doubts regarding the natural history of lumbar spinal stenosis (LSS), indication of treatment, and surgical approaches. To deal with these issues and try to reach some globally accepted recommendations, the World Federation of Neurosurgical Societies (WFNS) Spine Committee organized a consensus conference on this topic. This paper presents recommendations regarding the efficacy of surgical decompression, the difference between surgical techniques including recent minimally invasive surgeries (MIS), and finally, complications of surgical treatment.
Methods
Three expert spinal surgeons (MF, OLA, CT) reviewed the literature from 2008 to 2018 analyzing different surgical techniques, complications, and results in treating LSS. In particular, each one analyzed an aspect of the surgical treatment: the role of decompressive surgery and comparison of the different surgical techniques, the value of minimally invasive spine surgery, and complications. The following section is not a systematic review or a meta-analysis, but an overview of the available relevant literature.
The quality assessment and clinical relevance criteria used were in accordance with the Agency for Healthcare Research and Quality criteria for diagnostic studies and observational studies and the Cochrane Musculoskeletal Review Group Criteria as used for interventional techniques for randomized trials. Level of evidence was defined as Levels I–IV based on the quality of evidence developed by the US Preventive Services Task Force for therapeutic interventions. Strength of evidence rate was ranked as mild, moderate, or high.
Data sources included relevant literature in the English language identified through searches of Ovid Medline, Cochrane Register of Controlled Trials, Cochrane Database of Systematic Reviews, National Guideline Clearinghouse, PubMed, and EMBASE from 2008 to 2018.
The questions to be answered were as follows:
1. Is decompressive surgery alone an effective treatment for patients with LSS?
2. How effective are the different surgical techniques for decompression?
3. Is MIS superior to open decompression for clinical outcomes?
4. Is MIS associated with lower complication rates than open laminectomy?
5. Is MIS a more cost-effective technique than open laminectomy?
6. What is the overall complication rate for decompressive surgery in LSS and what are the main complications?
7. Are there any risk factors?
8. How can complications affect outcome after decompressive surgery for LSS?
On the basis of the most significant literature, we drafted 13 statements that were presented in Milan in November 2018. After a preliminary voting session, 3 statements were excluded because evidence of the existing literature was too low to make a choice. The final 10 statements were then presented and voted on in the final round in Belgrade in March 2019.
Results
Value of Decompressive Surgery
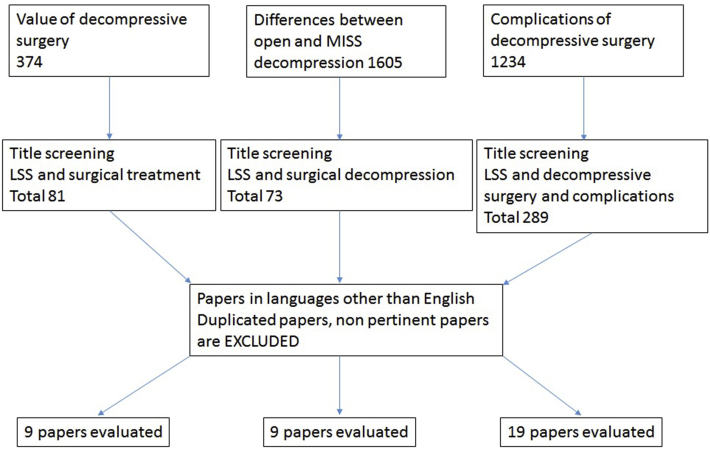
The following key words were used as search items: “surgical treatment” and “lumbar stenosis or spinal stenosis.” The search was done on literature from the last 10 years, in the English language. Only studies including surgical treatment were included in the panel. A total of 374 papers were found with the cited algorithm. A young spine surgeon made a first selection. After excluding papers regarding spondylolisthesis, interspinous process devices, conservative treatment alone and physical therapy, outcome, and complications, a total of 81 papers were left. Case reports, technical notes, and studies with a limited number of patients, short follow-ups, or not well-defined inclusion criteria and follow-up were excluded. Finally, we identified 9 papers considered to be the most significant to argue the statements and the subsequent vote; they are summarized in Tables 1 and 2, whereas the literature review process is summarized in Figure 1.
Table 1.
Papers Comparing Surgical Versus Nonsurgical Treatment
| Thomé et al 20084 | Review article | Surgical superior to nonsurgical Surgery indicated after 3 months of conservative treatment If adequate decompression microsurgical techniques equal to open laminectomy |
| SPORT study group 20085 | Randomized observational study | Relief of symptoms faster with surgery Surgery is superior in long term |
| Watters et al 20086 Kreiner et al 20137 |
Review article | Surgery is superior in patients with moderate-to-severe symptoms Surgery is superior in long term |
| Zaina et al 20168 | Metanalysis of RCTs | No benefit of surgery with respect to nonsurgical treatment |
RCT, randomized controlled trial.
Table 2.
Papers Comparing Different Surgical Techniques
| Overdevest et al 20159 | Metanalysis | 10 RCTs 733 patients 3 surgical techniques |
Advantages of microscopic techniques with respect to back pain and postoperative instability |
| Costa et al 200710 | Retrospective study | 473 patients | 87.9% good outcome |
| Phan and Mobbs 201611 | Systematic review | 12 papers 5 RCTs and 7 observational studies |
Advantages of microscopic techniques: lower BP, shorter hospitalization Complications similar to open approach |
RCT, randomized controlled trial; BP, back pain.
Figure 1.
Literature review process. MISS, minimally invasive spine surgery; LSS, lumbar spinal stenosis.
Most of the studies concluded that surgical treatment is an effective option in the treatment of LSS and particularly in cases with prolonged and progressively worsening symptoms in the legs.
Thomé et al4 stated in their review that, because of the changing societal age structure, the incidence of symptomatic LSS is increasing and the decision of whether to use conservative or surgical treatment crucially depends on the spontaneous disease course. However, this course is still not well known or investigated. After analyzing the literature, they reached the conclusion that although only a few evidence-based insights into the treatment options of LSS exist, surgical treatment makes sense, and is indicated, for relevant and therapy-resistant symptoms.4
The Spine Patient Outcomes Research Trial supports these results. The Commitee of the SPORT trials analyzed a large group of 289 patients in a randomized cohort and 365 patients in an observational cohort. Surgery resulted in a faster and significantly better alleviation of complaints than conservative treatment, especially in the longer term. Interestingly, patients who did not have surgery also experienced a reduction in symptoms, albeit at a slower rate.5
North America Spine Society guidelines published in 2008, and updated in 2011, suggested some conclusions based on the review of existing studies; most of them with recommendation grade B or C. In particular, decompressive surgery is suggested to improve outcomes in patients with moderate-to-severe symptoms of LSS, whereas medical and/or interventional treatment may be considered for patients with mild symptoms. But there is still insufficient evidence for this group of patients because they are not considered candidates for surgery and, consequently, they are often not included in studies. Decompression alone is suggested for patients with leg predominant symptoms without instability. Surgical treatment may be considered to provide long-term improvement for patients with degenerative LSS and may be considered as treatment also in patients aged 75 or older.6,7,12 However, some studies also reached opposite conclusions. A Cochrane Systematic Review published in 2016 analyzed 5 randomized controlled trials (RCTs) with a total of 643 patients randomized between surgical and conservative treatment. Those studies reached the conclusion that current evidence comparing surgical versus nonsurgical care for LSS is of low quality. For this reason, the authors could not conclude whether a surgical or a conservative approach was better for LSS, and no recommendations to guide clinical practice were provided. Moreover, the authors underlined that due to the high rate of side effects associated with surgery, clinicians should be cautious when proposing surgery for LSS, and patients should be properly informed of the risks. This review also highlighted the dearth of high-quality studies comparing surgical versus nonsurgical treatment options. In particular, studies with detailed protocols and descriptions of nonsurgical treatments are lacking.8
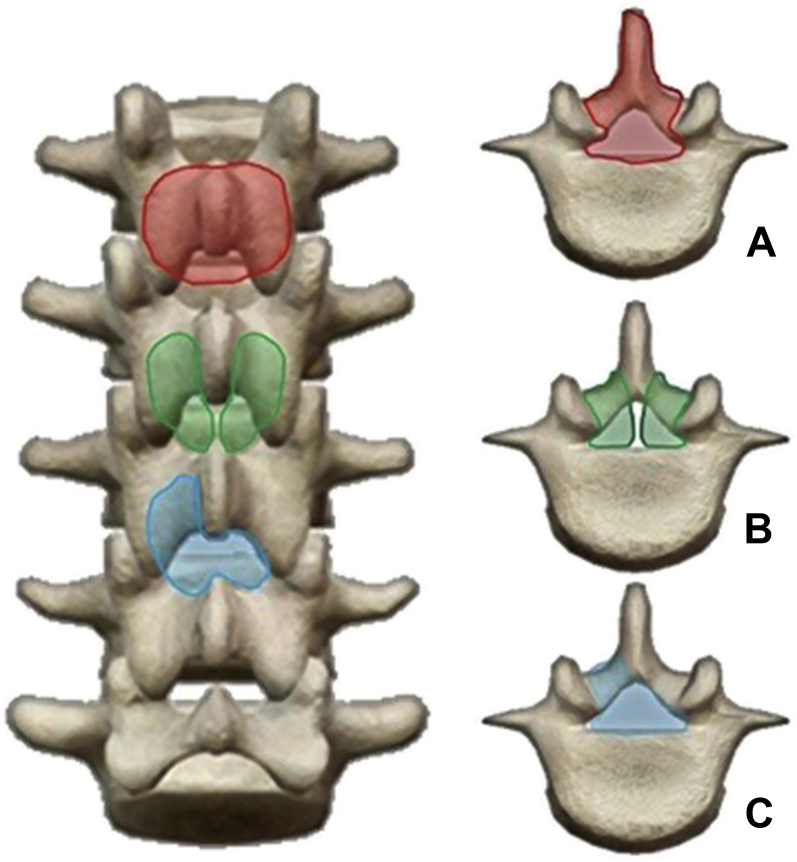
The existing studies of different surgical techniques concluded that microscopic techniques represent an effective surgical treatment of LSS and are feasible in the majority of patients, but there was insufficient evidence to support their superiority to standard laminectomy (Figure 2).
Figure 2.
(A) Standard posterior approach with open laminectomy and facets sparing; (B) bilateral laminotomy; and (C) unilateral laminotomy with bilateral decompression; (B, C) consent posterior element preservation.
Overdevest et al9 compared the effectiveness of novel microscopic techniques of posterior decompression (that limit the extent of bony decompression or avoid removal of posterior midline structures) versus conventional facet-preserving laminectomy for the treatment of patients with degenerative lumbar stenosis. They identified 10 RCTs to reach the conclusion that microscopic techniques compared with conventional laminectomy on functional disability, perceived recovery, and leg pain is of low or very low quality. Therefore, further research is necessary to establish whether these techniques offer a safe and effective alternative to conventional laminectomy. The proposed advantages of these techniques regarding the incidence of iatrogenic instability and postoperative back pain are plausible, but poor methodology and poor reporting of outcome measures among included studies limit definitive conclusions.9
Costa et al10 conducted a retrospective study in a consecutive series of 473 patients treated with unilateral microdecompression over a 5-year period (2000–2004). They concluded that unilateral laminotomy to achieve bilateral decompression provides an adequate and safe decompression of the spinal canal in patients with LSS. Evaluation of the long-term follow-up data obtained showed very favorable results for overall clinical improvement and satisfaction, as well as a low rate of morbidity (no significant segmental instability requiring reoperation was shown), confirming the feasibility of this minimally invasive approach in elderly and younger patients alike.10
Phan and Mobbs,11 in their systematic review and meta-analysis, compared classical open decompression to unilateral laminectomy for bilateral decompression and reached the conclusion that this microsurgical technique provides some advantage in terms of blood loss reduction, less disruption of muscular and ligamentous structures reducing pain and risk of instability, and short hospitalization times. However, the evidence supporting that was of moderate quality, and those findings warrant verification in large prospective registries and randomized trials.11
According to these literature reviews, the WFNS Spine Committee proposed and voted on the statements as follows:
Statement 1: Surgical decompression is an effective option in patients with moderate-to-severe symptoms. All expressed a positive vote to this statement with a strong consensus (90% voted 5 of the Linkert scale LS, 10% voted 3 of LS).
Statement 2: Microscopic techniques are equal to standard laminectomy to achieve adequate spinal canal decompression. This statement did not reach a consensus (12% voted 1 of LS, 25% voted 2 of LS, 12% voted 3 of LS, 13% voted 4 of LS, and 38% voted 5 of LS).
Statement 3: Unilateral laminotomy with bilateral decompression or bilateral laminotomy is not inferior to standard laminectomy for the treatment of LSS. This statement did not reach a consensus (10% voted 1 of LS, 27% voted 2 of LS, 11% voted 3 of LS, 12% voted 4 of LS, and 40% voted 5 of LS).
Differences Between Open and Minimally Invasive Spine Surgery Decompression
The following key words were used as search items: “surgical decompression” and “lumbar stenosis or spinal stenosis.” The search was done on literature from the last 10 years in the English language. There were a total of 73 papers found corresponding to the cited algorithm. After applying the filters, we identified 9 papers considered to be the most significant to argue the statements and the subsequent voting (literature review process is summarized in Figure 1).
Mobbs et al13 published an RCT, including 54 patients, comparing the outcomes after minimally invasive unilateral laminectomy and open laminectomy for isolated lumbar stenosis. The strong points of this study were the inclusion of a control group, the similarity of the baseline patients characteristics in the 2 groups, the lack of learning curve bias as the same senior surgeon performed all operations, and the quite homogeneous group of patients after excluding concomitant fusion or instrumentation, discectomy, spondylolisthesis, degenerative scoliosis, instability, or previous index level surgery. Nevertheless, only 54 of 79 (68.4% of originally randomized) patients were followed for a rather short term. Concerning the results, the primary clinical outcomes—mean visual analogue scale (VAS) and oswestry disability index—were significantly lower postoperatively in both groups. As for surrogate outcomes, postoperative length of stay (55.1 vs. 100.8 hours, P < 0.01), time to mobilization (15.6 vs. 33.3 hours, P < 0.001), opioid use (51.9% vs. 15.4%, P < 0.01), and mean blood loss (P < 0.01) were significantly in favor of MIS decompression.13
On the nihilistic side regarding MIS techniques, Ang et al,14 in a retrospective study enrolling 113 patients, concluded that for a single-level lumbar decompression the functional benefit observed at 6 months after surgery dissipated at a longer follow-up (24 months).
A systematic review published by Ng and Cheung,15 including 10 RCTs, stated that there was no conclusive evidence that MIS had better improvement in pain and outcome scores, like the VAS, short form survey-36 items, and Japanese Orthopaedic Association scores, or reduced the reoperation rate compared with open surgery. However, the same study supported, with weak evidence, that MIS reduced operating time, duration of hospital stay, and CPK-MM levels. Still, the conclusions of that systematic review should be regarded with extreme caution, as there was a very poor standardization of the MIS technique definition, including a myriad of different MIS techniques in the same pool. The lesson learned from that study is that MIS techniques should not be studied as a conceptual group, as one given MIS procedure is very different from another in terms of indications, preoperative risks, and learning curve.15
In a meta-analysis including 16 studies, some of them fusion-related, Chang et al16 confirmed that MIS was associated with better VAS for back pain (P = 0.01), shorter length of hospital stay (P < 0.001), and lower blood loss (P < 0.001).
Phan and Mobbs,11 in a systematic review and meta-analysis, enrolling 12 studies of high methodological quality as defined by Furlan et al,17 showed that MIS cohorts had higher patient satisfaction rates than open cohorts (84.0% vs. 75.4%, P = 0.03), whereas back pain VAS scores were lower (P < 0.00001). MIS operative duration was 11 minutes longer than the open approach (P = 0.001); however, this may not have clinical significance. There was less blood loss (P < 0.00001) and shorter hospital stay (2.1 days; P < 0.0001). That study provides moderate quality supporting MIS for superior satisfaction rates, reduced hospitalization, reduced blood loss, and longer procedures. However, it has to be stressed that the study included 5 RTC and 7 observational studies, reflecting a potential selection bias, with a small number of patients in each study, different follow-up periods, mixing tubular with mini-open studies as representatives of the MIS technique, a lack of standardized definition for quality and patient satisfaction outcomes, as well as an important surgeon heterogeneity in terms of experience and case load.11 Even if the benefits of both approaches were similar, then, maybe, the associated complication rate would distinguish open from MIS decompression in lumbar stenosis. When arguing about complication rates, the MIS group is associated with higher rates of inadvertent durotomies and reoperations within 2 years according to Ang et al,14 who advised that MS advantages should be carefully weighed against the potential complications. However, for Nerland et al,18 the number of patients experiencing complications was equal (14.6% vs. 10.6%, P = 0.23) in propensity matching group analysis. Phan and Mobbs11 found a similar risk ratio for dural injury (1.6% vs. 5.8%; P = 0.02), cerebrospinal fluid leak, which was confirmed by Chang et al,16 who also pointed out nonsignificantly different wound infection rates. Epstein clearly showed a higher overall incidence of nerve root injuries, radiculitis using MIS approaches. Regarding reoperations, it seems that MIS has a protective effect resulting in fewer reoperations as a result of a diminished development of postop iatrogenic spondylolisthesis after lumbar stenosis decompression.11,14,16, 18, 19, 20, 21
After analyzing the benefits and the complications of open versus MIS decompression, it seems logical to elaborate the cost-effectiveness of each technique. By enrolling a large sample of patients (n = 885), with follow-up for 1 year after surgery over a period of 5 years, Nederland et al, in their prospective observational study comparing the effectiveness of open versus MIS decompression, concluded that 1-year effectiveness of microdecompression is equivalent to laminectomy in the surgical treatment of central lumbar stenosis. In a US-based cost-utility retrospective study, with 54 patients (27 open and 27 MIS) followed for 2 years, Parker et al21 concluded that functional gain and cost were equivalent for multilevel decompression. MIS and open techniques were equivalent in 2-year quality adjusted life years gained (0.72 vs. 0.71, P = 0.99) and showed similar 2-year costs ($23,109 vs. $25,420; P = 0.21) translating equivalent utilization of health care resources in terms of care visits, physical therapy, diagnostic imaging, and postoperative medication. The limited sample size, the recall bias as patient phone interview for outcome was conducted retrospectively, the cost source based on Medicare national allowable payment, and the variability across providers hampered strong conclusions.19
According to those literature reviews, the WFNS Spine Committee proposed and voted on the statements as follows:
Statement 4: MIS has some advantages over open decompression for early clinical outcomes (blood losses, wound pain, and hospital stay). This statement reached a strong positive consensus (50% voted grade 4 of LS, 10% voted grade 3, and 10% voted grade 1).
Statement 5: MIS is associated with lower complication rates than open approach. This statement reached a strong positive consensus (40% voted grade 5, 20% grade 4, 30% grade 3, and 10% grade1).
Statement 6: MIS is a more cost-effective technique than open laminectomy. This statement did not reach a consensus (40% voted grade 5, 20% grade 3, 20% grade 2, and 20% grade 1).
Complications of Decompressive Surgery
By searching the key words “decompressive surgery” and “and complications” between 2008 and 2018, a total of 1234 papers were found. After applying the filters, we identified 289 papers, of which 19 were considered to be the most significant to argue the statements and the subsequent voting (literature review process is summarized in Figure 1).
The literature regarding complications in spine surgery and, in detail, in decompressive surgery is thriving. Recently, literature has received more papers regarding complications in the elderly. Despite this, it is challenging to evaluate the overall complication rate because its value can vary greatly between different studies due to the heterogeneity of posterior spine surgery procedures analyzed, of outcome and follow-up parameters.
Imagama et al22 presented a retrospective review of all posterior surgeries with or without fusion performed in a 10-year period with a total of 918 patients. They analyzed the frequency and severity of perioperative complications and all minor adverse events. Furthermore, the incidence of intraoperative complications was compared between junior (<10 years of experience in spine surgery) and senior (≥10 years of experience) surgeons. They found an overall rate of 15.7%; of them, 2.4% were intraoperative, whereas 13.3% were postoperative. Predictably, the complication rate was higher in elderly patients and in longer and more complicated operations (instrumented surgery). The absence of a relationship between the experience of the surgeon and incidence of intraoperative complications may be due to the greater effect of invasive surgery performed by experienced surgeons. They concluded that surgical indications should be cautious and do not exclude invasive surgery in elderly patients.22
Deyo et al23 examined different surgical techniques for lumbar decompression and fusion and their association with complications and resource use. They carried out a retrospective cohort analysis of complications such as wound complications, cardiopulmonary adverse events and mortality for decompression alone, simple fusion (1 or 2 disk levels, single surgical approach), or complex fusion (more than 2 disk levels or combined anterior and posterior approach). They found that life-threatening complications increased with increasing surgical invasiveness, from 2.3% among patients having decompression alone to 5.6% among those having complex fusions. A similar pattern was observed for rehospitalization within 30 days, which occurred for 7.8% of patients undergoing decompression and 13.0% having a complex fusion. They concluded that compared with decompression, simple fusion and complex fusion were associated with increased risk of major complications, 30-day mortality, and resource use.23
Other papers individually analyzed the different complications. One of the most frequent, that particularly affects minimally invasive surgical technique, is incidental durotomy (ID). The Spine Patient Outcomes Research Trial study group analyzed the incidence of this complication among 490 patients who underwent first-time open laminectomy with or without fusion. They found a rate of 9% for this complication. No significant differences were observed in age; sex; race; body mass index; the prevalence of smoking, diabetes mellitus, and hypertension; decompression level; number of levels decompressed; or whether an additional fusion was performed. The durotomy group had significantly increased operative duration, operative blood loss, and inpatient stay. However, there were no differences in incidence of nerve root injury, mortality, additional surgeries, or primary outcomes at yearly follow-ups to 4 years. They concluded that ID during first-time lumbar laminectomy for spinal stenosis did not impact long-term outcomes in affected patients.24
Ulrich et al25 did a prospective multicenter cohort study with the aim of assessing whether ID during first-time LSS decompression surgery without fusion had an impact on long-term outcome. A total of 167 patients met the inclusion criteria; 9% of those patients had an ID. Baseline characteristics were similar between the durotomy and no-durotomy group. All patients improved over time. Their conclusions were similar to Deyo et al: ID did not have a negative effect on long-term outcome and quality of life.25
Kothe et al26 made a comparative analysis between a cohort of patients who underwent ID with respect to a cohort of patients without dural laceration. They made a prospective multicenter study that included 800 patients with LSS who underwent exclusive decompression surgery with a follow-up preoperatively, as well as 3 and 12 months after surgery. They found that intraoperative dura lesions occurred in 6.5%. As in the previous reported paper, they found that both cohorts did not reveal any differences regarding patient demographics, risk factors, or comorbidities at baseline. The length of the hospital stay was significantly longer for the Dura+ cohort. Otherwise, in contrast with previously cited papers, they demonstrated a significantly greater improvement in VAS back pain in patients without ID, but the differences for the remaining outcome measures were not statistically significant.26
Strömqvist et al27 did a retrospective analysis of almost 64,500 surgical procedures to evaluate whether ID affects outcomes after degenerative spine surgery and the incidence of ID with different diagnoses and different surgical procedures. The aim was to overcome the conflicting evidence presented regarding whether or not outcomes are affected by the presence of an ID. They found an overall incidence of ID of 5.0% (higher rate in decompressive surgery and in patients who underwent previous spinal surgery). They concluded that the outcome at 1 year after surgery was not affected to a clinically relevant extent when an ID was obtained. However, ID was associated with a higher degree of patient dissatisfaction and a longer hospital length of stay.27
McMahon et al28 reached very similar conclusions. They found a rate of 3.5% for ID and identified risk factors that can increase the likelihood of a durotomy, including location of the spinal procedure, type of procedure performed, and the implementation of a new procedure. The years of physician training or resident experience did not appear to be a major risk.28
Many others studied the different risk factors of ID with the aim of minimizing its occurrence.29,30
Another frequent perioperative complication of spine surgery is the development of epidural hematoma with or without neurologic symptoms. Fujiwara et al31 studied the development of postsurgical epidural hematoma and its correlation with hypertension. The study included a total of 2468 patients who underwent microscopic posterior decompression surgery for LSS and found a reoperation rate of 0.6% for this complication. They demonstrated that the preoperative high blood pressure value was the most essential risk factor for postsurgical epidural hematoma and concluded that the management of preoperative blood pressure and postoperative drainage would be crucial for its prevention.31
As mentioned previously, Overdevest et al9 performed a literature review including prospective controlled trials to compare the effectiveness of techniques of posterior decompression that limit the extent of bony decompression or avoid removal of posterior midline structures of the lumbar spine versus conventional facet-preserving laminectomy for the treatment of patients with degenerative lumbar stenosis. A total of 4 high-quality RCTs and 6 low-quality RCTs met the search criteria of this review with a total of 733 participants. Three studies (173 participants) compared unilateral laminotomy for bilateral decompression versus conventional laminectomy. Four studies (382 participants) compared bilateral laminotomy versus conventional laminectomy (1 study included 3 treatment groups and compared unilateral and bilateral laminotomy vs. conventional laminectomy). Finally, 4 studies (218 participants) compared a split-spinous process laminotomy versus conventional laminectomy. Evidence of low or very low quality suggests that different techniques of posterior decompression and conventional laminectomy have similar effects on functional disability and leg pain. They found no evidence to show that the incidence of complications, length of the procedure, length of hospital stay, and postoperative walking distance differed between techniques of posterior decompression. Differences in postoperative low-back pain were too small to be significant. Therefore, they concluded that the effects of unilateral laminotomy for bilateral decompression, bilateral laminotomy, and split-spinous process laminotomy compared with conventional laminectomy on functional disability, perceived recovery, and leg pain are of low or very low quality. The proposed advantages of these techniques regarding the incidence of iatrogenic instability and postoperative back pain are plausible, but poor methodology and poor reporting of outcome measures and lack of long-term outcome results among included studies limit definitive conclusions.9
Kim et al32 did a study to evaluate, in particular, the reoperation rate after decompression or decompression and fusion for the treatment of LSS and to compare the reoperation rates between decompression and fusion surgeries. They performed a retrospective cohort study using national health insurance data of a cohort of patients who underwent initial surgery for lumbar stenosis without spondylolisthesis in 2003 with a total of 11,027 patients selected with a follow-up of 5 years. The primary end-point was any type of second lumbar surgery. They found that fusion surgery was performed in 20% of patients. The cumulative reoperation rate was 4.7% at 3 months, 7.2% at 1 year, 9.4% at 2 years, 11.2% at 3 years, 12.5% at 4 years, and 14.2% at 5 years. The adjusted reoperation rate did not differ between decompression and fusion surgeries, and the calculated reoperation rate was expected to be 22.9% at 10 years. They concluded that the reoperation rate was not different between decompression and fusion surgeries, and with current surgical trends, the reoperation rate is progressively higher than in the past, and consideration of this problem is required.32
As stated previously, many recent studies have been focused on outcome and complications in the elderly due to an increasing demographic aging of the general population with degenerative spine disease.
Gerhardt et al33 assessed complication rates of lumbar decompression in regard to neurologic outcome and medical conditions in patients aged 80 years or older in a retrospective single-center series. They retrospectively collected data on 244 patients who underwent decompressive surgery for LSS or disc herniation in a 10-year period. They found a rate of new transient, postoperative, neurologic deficits of 2.5%, and a rate of intraoperative complications of 22.5% from mild to moderate, no severe surgical complications occurred. Two hundred and fifteen patients (88%) had relevant medical disorders.
The rate of medical complications was 7.7%, of which 73.3% were severe and 26.3% were mild (such as pulmonary embolisms, pneumonias, myocardial infarctions, postoperative renal failure, and urinary tract infections). Medical complications necessitating intensive care unit treatment and that resulted in a lethal outcome were 0.8%. They concluded that despite their age, the vast majority of octogenarians and nonagenarians benefited from lumbar decompression surgery. Mild-to-moderate intraoperative complications were relatively frequent, whereas severe intraoperative complications did not occur. The majority of medical complications were severe, but the incidence was acceptable, and the postoperative outcome was still favorable for most patients.33
Proietti et al34 conducted a retrospective study of 338 patients considering general and specific complications of spine surgery. They found that an age of over 65 years was not a predisposing factor in developing intra- and perioperative complications, despite the risk of developing general complications being progressively higher in patients over the age of 75 years with more than 4 comorbidities. On this basis, importance was given to the preoperative risk assessment based on the magnitude of surgery planned. In particular, they found greater complications in patients operated on for instrumented surgery and aged over 69 years. A long surgical time (>4 hours) and the use of conventional open surgery have demonstrated a consistent risk factor in developing superficial and deep wound infections. Major complications are more often seen in complex surgical treatments for severe deformities, in revision surgery and in anterior approaches with an occurrence of 58.3%.
In detail, the greater age of patients in a lumbar stenosis group may be the cause of a major incidence of unintended durotomy associated with the presence of significant scar adhesions typical of degenerative process of the lumbar stenosis (4.5 vs. 3.1%). Deep venous thrombosis and pulmonary embolism are significant potential complications in spinal surgery. A limited number of reports have documented these events in relatively small populations of patients. The true incidence of thromboembolic complications in spinal surgery still remains unknown today.
It was concluded that several factors have to be considered in surgical planning to avoid complications and exclusion of patients is not justified only due to age, but a systematic preoperative clinical evaluation should be performed to stratify risks and to guide decision making to obtain the best possible clinical results at lower risk.34
According to these literature reviews, the WFNS Spine Committee proposed and voted on the statements as follows:
Statement 7: Overall complication rate for lumbar decompressive surgery is approximatively 20% and reoperation rates are estimated around 10% in 5 years. This statement did not reach a consensus (20% voted grade 4, 30% grade 3, 10% grade 2, and 40% grade 1).
Statement 8: Cardiopulmonary complications and stroke in this elderly population occur in about 2% and mortality is 0.5%. This statement reached a strong positive consensus (40% voted grade 5, 10% grade 4, 40% grade 3, and 10% grade 2).
Statement 9: New neurologic injury and postoperative hematoma after decompressive surgery are rare (≈1%). All expressed a positive vote with a strong positive consensus (40% grade 5, 30% grade 4, and 30% grade 3).
Statement 10: Incidental durotomy is common (almost 10%) and depends on established risk factors and has only a minor effect on outcome. This statement reached a strong positive consensus (30% voted grade 5, 10% grade 4, 40% grade 3, and 20% grade 1).
The WFNS Spine Committee Recommendations for Decompressive Surgery are summarized in Table 3.
Table 3.
WFNS Spine Committee Recommendations on Decompressive Surgery, Minimally Invasive Techniques, and Complications
| Efficacy of decompression • Surgical decompression is an effective option in patients with moderate-to-severe symptoms |
| Role of MISS in the treatment of LSS • Minimally invasive surgery (MIS) has some advantages over open decompression for early clinical outcomes (blood losses, wound pain, and hospital stay) • MIS is associated with lower complication rates than open approach |
| Complications of decompressive surgery • Cardiopulmonary complications and stroke in the elderly population occur in approximately 2% and mortality is 0.5% • New neurologic injury and postoperative hematoma after decompressive surgery are rare (approximately 1%) • Incidental durotomy is common (almost 10%) and depends on established risk factors and has only a minor effect on outcome |
MISS, minimally invasive spine surgery; LSS, lumbar spinal stenosis.
Discussion and Conclusions
All the members of the Committee agreed about the utility of surgical decompression for the treatment of symptomatic LSS. However, the clinical onset is often referred as mild, moderate, or severe, but there is wide heterogeneity in this classification. As stated in the North America Spine Society guidelines, the severity of symptoms is based on the extent of leg pain and pain-related disability (numbness and neurologic deficits in the lower extremities and buttocks, and bladder/bowel dysfunction). In addition, the above symptoms were required to be induced or exacerbated by walking or prolonged standing and relieved by lumbar flexion, sitting, and recumbency.12
Moreover, simply defining the correlation between radiological findings and clinical symptoms of LSS can be challenging: in fact, sometimes there is no direct correlation. There is the same problem with the lack of standardization in outcome measures.
Furthermore, in most studies, patients with LSS alone or in association with spondylolisthesis or instability are not considered separately, and this makes reaching any significant conclusion very difficult.
All of these represent serious drawbacks, as reported in most of the cited studies; this represents an important limit to comparing the literature effectively.
Despite this, as previously discussed, there is strong agreement regarding the effectiveness of the surgical treatment with the aim of decompressing the nervous structures for the relief of neurogenic claudication and radicular pain or lower limbs weakness, in particular in patients with moderate-to-severe symptoms.
The question is very different regarding the most appropriate surgical technique and in particular, whether microsurgical ones are equal or inferior to standard laminectomy or which microsurgical technique is better. In fact, the results of statements 2 and 3 show that the committee was divided in half. This is mainly due to many microsurgical and minimally invasive techniques being described with no standardization in the technique itself and, as stated by Ng and Cheung,15 the different techniques should not be studied as a conceptual group, but one given MIS procedure is very different from another in terms of indications, preoperative risks, and learning curve.
For example, unilateral laminectomy for bilateral decompression was first described in 1997 by Foley and Smith,35 and it is has been the most widely used for 10 to 15 years but, despite all the papers available, only moderate evidence recommends its use over open laminectomy.11 Similar conclusions are available for all the different techniques for posterior decompression in LSS.
Analyzing the literature up to today, it is nearly impossible to define what the best surgical approach is; for this reason, personal experience and skill with specific techniques must be considered as one of the main factors in choosing one of them. Further RCTs are needed to compare the efficacy of open and MIS techniques.
The analysis of posterior approaches for lumbar surgery and associated complications shows a progressive increasing of the overall rate, accordingly with the higher age of the treated population. However, definitions of intraoperative, perioperative, and postoperative complications have not been established, and previous reports have varied in the definition of, and focus on, intraoperative or major postoperative complications.
In general, different studies show an incidence of dural tears among 10% and an overall complication rate of 20%. The committee disagreed with these percentages based on their personal experience; in detail, they argued that these percentages are too high in respect to the real incidence of complications in daily practice (Table 4).
Table 4.
Complications of Decompressive Surgery
| Intraoperative | Neurological deficits | 1%–2% |
| Dural injury | 10% | |
| Infection | ±2% | |
| Delayed surgical | Hematoma | 0.6% |
| Instability | ±20% | |
| Reoperation | ±15% | |
| Medical | Deep venous thrombosis Pulmonary embolism Postoperative anemia Cerebral ischemia Urinary infections Ileus and other minors |
5%–10% |
In conclusion, to the best of our knowledge, the surgical treatment for LSS by decompression alone is an effective treatment. Which surgical technique is the best is still debatable. MIS decompression for isolated lumbar stenosis achieves at least the same clinical outcomes and cost-efficiency as the open technique, however, with a favorable impact on surrogate end-points for outcome, such as blood loss, hospital stay, and wound infection. Our suggestion is to use the one you are most confident with.
The statement that did not reach a consensus will be discussed again in the future to overcome existing doubts.
Declaration of competing interest
The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
CRediT authorship contribution statement
Francesco Costa: Conceptualization, Methodology, Validation, Writing - review & editing. Oscar L. Alves: Data curation, Writing - original draft. Carla D. Anania: Writing - original draft, Writing - review & editing. Mehmet Zileli: Writing - original draft, Writing - review & editing, Validation. Maurizio Fornari: Conceptualization, Methodology, Writing - review & editing.
Acknowledgments
A special thank you to Claudius Thomé for his important contribution to literature review and statement draft about the topic of complications of posterior decompressive surgery. We also thank him for his participation in the first voting session in Milan.
References
- 1.Verbiest H. Results of surgical treatment of idiopathic developmental stenosis of the lumbar vertebral canal. A review of twenty-seven years' experience. J Bone Joint Surg Br. 1977;59:181–188. doi: 10.1302/0301-620X.59B2.141452. [DOI] [PubMed] [Google Scholar]
- 2.Wilson E.S., Brill R.F. Spinal stenosis. The narrow lumbar spinal canal syndrome. Clin Orthop Relat Res. 1977;122:244–248. [PubMed] [Google Scholar]
- 3.Wiltse L.L., Kirkaldy-Willis W.H., McIvor G.W. The treatment of spinal stenosis. Clin Orthop Relat Res. 1976;115:83–91. [PubMed] [Google Scholar]
- 4.Thomé C., Börm W., Meyer F. Degenerative lumbar spinal stenosis. current strategies in diagnosis and treatment. Dtsch Arztebl Int. 2008;105:373–379. doi: 10.3238/arztebl.2008.0373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinstein J.N., Tosteson T.D., Lurie J.D. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358:794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watters W.C., 3rd, Baisden J., Gilbert T.J., North American Spine Society Degenerative lumbar spinal stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. 2008;8:305–310. doi: 10.1016/j.spinee.2007.10.033. [DOI] [PubMed] [Google Scholar]
- 7.Kreiner D.S., Shaffer W.O., Baisden J.L., North American Spine Society An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update) Spine J. 2013;13:734–743. doi: 10.1016/j.spinee.2012.11.059. [DOI] [PubMed] [Google Scholar]
- 8.Zaina F., Tomkins-Lane C., Carragee E., Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;1:CD010264. doi: 10.1002/14651858.CD010264.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Overdevest G., Vleggeert-Lankamp C., Jacobs W., Thomé C., Gunzburg R., Peul W. Effectiveness of posterior decompression techniques compared with conventional laminectomy for lumbar stenosis. Eur Spine J. 2015;24:2244–2263. doi: 10.1007/s00586-015-4098-4. [DOI] [PubMed] [Google Scholar]
- 10.Costa F., Sassi M., Cardia A. Degenerative lumbar spinal stenosis: analysis of results in a series of 374 patients treated with unilateral laminotomy for bilateral microdecompression. J Neurosurg Spine. 2007;7:579–586. doi: 10.3171/SPI-07/12/579. [DOI] [PubMed] [Google Scholar]
- 11.Phan K., Mobbs R.J. Minimally invasive versus open laminectomy for lumbar stenosis: a systematic review and meta-analysis. Spine. 2016;41:E91–E100. doi: 10.1097/BRS.0000000000001161. [DOI] [PubMed] [Google Scholar]
- 12.NASS Diagnosis and treatment of degenerative lumbar spinal stenosis (revised 2011) https://www.spine.org/Research-Clinical-Care/Quality-Improvement/Clinical-Guidelines Available at: Accessed October 20, 2018.
- 13.Mobbs R.J., Li J., Sivabalan P., Raley D., Rao P.J. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine. 2014;21:179–186. doi: 10.3171/2014.4.SPINE13420. [DOI] [PubMed] [Google Scholar]
- 14.Ang C.L., Phak-Boon Tow B., Fook S. Minimally invasive compared with open lumbar laminotomy: no functional benefits at 6 or 24 months after surgery. Spine J. 2015;15:1705–1712. doi: 10.1016/j.spinee.2013.07.461. [DOI] [PubMed] [Google Scholar]
- 15.Ng K.K.M., Cheung J.P.Y. Is minimally invasive surgery superior to open surgery for treatment of lumbar spinal stenosis? A systematic review. J Orthop Surg (Hong Kong) 2017;25 doi: 10.1177/2309499017716254. 2309499017716254. [DOI] [PubMed] [Google Scholar]
- 16.Chang F., Zhang T., Gao G. Comparison of the minimally invasive and conventional open surgery approach in the treatment of lumbar stenosis: a systematic review and a meta-analysis. Ann Acad Med Singapore. 2017;46:124–137. [PubMed] [Google Scholar]
- 17.Furlan A.D., Pennick V., Bombardier C. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine. 2009;34:1929–1941. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 18.Nerland U.S., Jakola A.S., Solheim O. Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ. 2015;350:h1603. doi: 10.1136/bmj.h1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epstein N.E. More nerve root injuries occur with minimally invasive lumbar surgery: Let's tell someone. Surg Neurol Int. 2016;7(Suppl 3):S96–S101. doi: 10.4103/2152-7806.174896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guha D., Heary R.F., Shamji M.F. Iatrogenic spondylolisthesis following laminectomy for degenerative lumbar stenosis: systematic review and current concepts. Neurosurg Focus. 2015;39:E9. doi: 10.3171/2015.7.FOCUS15259. [DOI] [PubMed] [Google Scholar]
- 21.Parker S.L., Adogwa O., Davis B.J. Cost-utility analysis of minimally invasive versus open multilevel hemilaminectomy for lumbar stenosis. J Spinal Disord Tech. 2013;26:42–47. doi: 10.1097/BSD.0b013e318232313d. [DOI] [PubMed] [Google Scholar]
- 22.Imagama S., Kawakami N., Tsuji T. Perioperative complications and adverse events after lumbar spinal surgery: evaluation of 1012 operations at a single center. J Orthop Sci. 2011;16:510–515. doi: 10.1007/s00776-011-0123-6. [DOI] [PubMed] [Google Scholar]
- 23.Deyo R.A., Mirza S.K., Martin B.I., Kreuter W., Goodman D.C., Jarvik J.G. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–1265. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Desai A., Ball P.A., Bekelis K. SPORT: does incidental durotomy affect longterm outcomes in cases of spinal stenosis? Neurosurgery. 2015;76(Suppl 1):S57–S63. doi: 10.1227/01.neu.0000462078.58454.f4. [discussion: S63] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ulrich N.H., Burgstaller J.M., Brunner F., LSOS Study Group The impact of incidental durotomy on the outcome of decompression surgery in degenerative lumbar spinal canal stenosis: analysis of the Lumbar Spinal Outcome Study (LSOS) data—a Swiss prospective multi-center cohort study. BMC Musculoskelet Disord. 2016;17:170. doi: 10.1186/s12891-016-1022-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kothe R., Quante M., Engler N. The effect of incidental dural lesions on outcome after decompression surgery for lumbar spinal stenosis: results of a multi-center study with 800 patients. Eur Spine J. 2017;26:2504–2511. doi: 10.1007/s00586-016-4571-8. [DOI] [PubMed] [Google Scholar]
- 27.Strömqvist F.1, Sigmundsson F.G., Strömqvist B., Jönsson B., Karlsson M.K. Incidental durotomy in degenerative lumbar spine surgery—a register study of 64,431 operations. Spine J. 2019;19:624–630. doi: 10.1016/j.spinee.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 28.McMahon P., Dididze M., Levi A.D. Incidental durotomy after spinal surgery: a prospective study in an academic institution. J Neurosurg Spine. 2012;17:30–36. doi: 10.3171/2012.3.SPINE11939. [DOI] [PubMed] [Google Scholar]
- 29.Burks C.A., Werner B.C., Yang S., Shimer A.L. Obesity is associated with an increased rate of incidental durotomy in lumbar spine surgery. Spine (Phila Pa 1976) 2015;40:500–504. doi: 10.1097/BRS.0000000000000784. [DOI] [PubMed] [Google Scholar]
- 30.Smorgick Y., Baker K.C., Herkowitz H. Predisposing factors for dural tear in patients undergoing lumbar spine surgery. J Neurosurg Spine. 2015;22:483–486. doi: 10.3171/2015.1.SPINE13864. [DOI] [PubMed] [Google Scholar]
- 31.Fujiwara Y., Manabe H., Izumi B. The impact of hypertension on the occurrence of postoperative spinal epidural hematoma following single level microscopic posterior lumbar decompression surgery in a single institute. Eur Spine J. 2017;26:2606–2615. doi: 10.1007/s00586-017-5165-9. [DOI] [PubMed] [Google Scholar]
- 32.Kim C.H., Chung C.K., Park C.S. Reoperation rate after surgery for lumbar spinal stenosis without spondylolisthesis: a nationwide cohort study. Spine J. 2013;13:1230–1237. doi: 10.1016/j.spinee.2013.06.069. [DOI] [PubMed] [Google Scholar]
- 33.Gerhardt J., Bette S., Janssen I., Gempt J., Meyer B., Ryang Y.M. Is eighty the new sixty? Outcomes and complications after lumbar decompression surgery in elderly patients over 80 years of age. World Neurosurg. 2018;112:e555–e560. doi: 10.1016/j.wneu.2018.01.082. [DOI] [PubMed] [Google Scholar]
- 34.Proietti L., Scaramuzzo L., Schiro G.R., Sessa S., Logroscino C.A. Complications in lumbar spine surgery: a retrospective analysis. Indian J Orthop. 2013;47:340–345. doi: 10.4103/0019-5413.114909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Foley K.T., Smith M.M. Microendoscopic discectomy. Tech Neurosurg. 1997;3:301–307. [Google Scholar]