Abstract
Objective
To evaluate stress effect of COVID‐19 pandemic and Zagreb earthquakes on symptoms of temporomandibular disorders (TMD).
Materials and Methods
One hundred and two previously diagnosed TMD patients were contacted by email to participate in an online survey about impact of those events on current and/or new symptoms, perceived stress, anxiety and symptom intensity in time‐points at the baseline, following pandemic and following earthquake. We compared data between earthquake‐affected and non‐affected respondents.
Results
Response rate was 79.4%. Effects stress had on deterioration of symptoms were significantly different between earthquake‐affected and non‐affected (p = .024). In earthquake‐affected, numerical pain rating scale (NPRS) scores significantly increased between baseline and after COVID‐19 (p > .001) and between baseline and after earthquakes (p > .05). However, scores insignificantly dropped from COVID‐19 to after earthquakes time‐points. In earthquake‐affected, positive correlation was found between impact of COVID‐19 on stress and NPRS (p < .001) and between earthquakes’ impact on stress and NPRS (p < .001). Earthquake‐affected respondents reported significantly more new behavioral habits when compared to non‐affected (p = .048).
Conclusions
A series of stressful events do not necessarily have a cumulative effect, but are likely to have a complex interaction (e.g., acute stress might trigger the protective mechanisms), which could have decreased pain scores after the earthquakes.
Keywords: COVID‐19, earthquake, pandemic, stress, temporomandibular disorders
1. INTRODUCTION
Stress refers to situations in which one feels that the demands imposed on them exceed the limitations of their ability to adapt. This causes a series of adverse consequences among which is compromised health (Lazarus & Folkman, 1984).
On 11th March 2020, the World Health Organization declared the pandemic status of COVID‐19 diseases, leading to the European Union states imposing the lockdown, Croatia being one among them. Infection prevention became the nation's most important goal, and people had to change their day‐to‐day habits. Additionally, in the morning of 22nd March, Zagreb, Croatian Capital, was hit by 2 earthquakes one being of 5.5 on the Richter scale, followed by another one of 5.0 (University of Zagreb, Seismological Service of the Geophysical Department of the Faculty of Science). The earthquakes caused serious damage across the city, taking one child's life and causing a significant number of people losing their homes. The School of Dental Medicine was also damaged and has been closed since. In the following days, a series of minor earthquakes were recorded in Zagreb and southern Croatia.
Such events create an expected increase in the incidence of adverse stress reactions, especially in susceptible people (Bergiannaki, Psarros, Varsou, Paparrigopoulos, & Soldatos, 2003; Jakovljevic, Bjedov, Jaksic, & Jakovljevic, 2020).
Temporomandibular disorders (TMD) refer to a set of conditions affecting masticatory muscles and the temporomandibular joints. The impact of stressful events on the occurrence and worsening of TMD symptoms is not completely clear but evidence shows a strong connection between the two (Auerbach, Laskin, Frantsve, & Orr, 2001; Canales, Guarda‐Nardini, Rizzatti‐Barbosa, Conti, & Manfredini, 2019; Osiewicz, Lobbezoo, Ciapała, Pytko‐Polończyk, & Manfredini, 2020), with more numerous and/or frequent somatic, psychologic, and behavioral symptoms of stress in TMD patients when compared to control (Beaton, Egan, Nakagawa‐Kogan, & Morrison, 1991; Jivnani et al., 2019).
Assuming that the symptoms may worsen depending on the patient's stressful experiences, we conducted a survey to evaluate the effect of stressful crises (COVID‐19 pandemic and Zagreb earthquakes) on TMD symptoms and behavioral habits (BH).
Our hypotheses were as follows: (a) The stress caused by COVID‐19 pandemic contributed to the onset of new or the increase of existing TMD symptoms; (b) the additional stress (Zagreb earthquakes) worsened the symptoms more in respondents in affected areas, compared to respondents not affected by the earthquake; (c) the stress effect caused the appearance of new BH.
2. METHODS
The total of 102 of our previously or currently treated TMD patients was contacted via e‐mail and asked to participate in an anonymous online survey. Those are all our previously diagnosed TMD patients whose e‐mail addresses were available from our TMD database. The data collection was initiated on 28th March and closed on 15th April 2020. The online self‐reported questionnaire was formulated using Google forms, with a consent form attached to it. Ethical approval has been obtained for the Croatian Science Foundation grant #IP‐2019–04–6211. We collected data from Zagreb and its surroundings, northern, central, and southern Croatia. The socio‐demographic variables included gender, age, employment status, and area of residence. Respondents were patients previously diagnosed with symptomatic TMD according to diagnostic criteria for temporomandibular disorders (DC/TMD). All patients were diagnosed and treated at The School of Dental Medicine University of Zagreb by an expert in the field of TMD diagnosis and treatment (IZA).
The questionnaire contained multiple‐choice questions related to their current isolation status due to the COVID‐19 pandemic, their perceived stress, and anxiety considering the COVID‐19 escalation and recent earthquakes in Zagreb, questions assessing the existence of the previous symptoms and impact of both events on current and/or new symptoms. Respondents needed to retroactively specify new symptoms that appeared. Spontaneous pain was self‐reported with Numerical pain rating scale (NPRS) before and after the two stressful events; also, current pain was evaluated (0 indicated “no pain,” 10 indicated “worst pain”). Respondents needed to report their coping mechanisms and about BH that appeared over the last 2 weeks.
Descriptive statistics were conducted to assess frequency, means, and standard deviations. Differences between stress impact for Zagreb and the rest of the respondents were analyzed with the Chi‐Square test. Changes in NPRS over “time” were analyzed with repeated‐measures ANOVA and post hoc tests. Spearman correlation was used to assess the association between stress impact (expressed through four‐point scale) and increase of pain.
3. RESULTS
Out of 102 contacted subjects, 81 of them have participated in the survey. The demographic data of respondents are presented in Table 1.
TABLE 1.
Sample characteristics, symptoms severity before COVID‐19, functioning related to COVID‐19 and new self‐reported behaviors
|
Affected by earthquakes (n = 53) |
Not affected by earthquakes (n = 28) |
Total (n = 81) |
||||
|---|---|---|---|---|---|---|
| Count | % | Count | % | Count | % | |
| Sex | ||||||
| Male | 7 | 13.2 | 0 | 7 | 8.6 | |
| Female | 46 | 86.8 | 28 | 100 | 74 | 91.4 |
| Employment status | ||||||
| Pupil | 0 | 0 | 4 | 14.3 | 4 | 4.9 |
| Pre‐graduate student | 9 | 16.9 | 7 | 25 | 16 | 19.8 |
| Currently employed | 40 | 75.5 | 13 | 46.4 | 53 | 65.4 |
| Currently unemployed regardless of present situation | 2 | 3.8 | 4 | 14.3 | 6 | 7.4 |
| Currently unemployed due to present situation | 2 | 3.8 | 0 | 0 | 2 | 2.5 |
| Retired | 0 | 0 | 0 | 0 | 0 | 0 |
| Symptoms related to tmd pain before COVID−19 pandemic | ||||||
| Non‐existent | 7 | 13.2 | 5 | 17.8 | 12 | 14.8 |
| Mild | 18 | 33.9 | 8 | 28.6 | 26 | 32.1 |
| Moderate | 17 | 32.1 | 7 | 25.1 | 24 | 29.6 |
| Strong but bearable | 11 | 20.8 | 5 | 17.8 | 15 | 19.8 |
| Strong and unbearable | 3 | 10.7 | 3 | 3.7 | ||
| Isolation status due to COVID−19 pandemic | ||||||
| Practicing physical distancing and working from home | 44 | 83 | 19 | 67.8 | 63 | 77.8 |
| Have not changed routine much, a significant amount of social contacts per day | 4 | 7.5 | 4 | 14.3 | 8 | 9.9 |
| Self‐isolating by will | 3 | 5.7 | 3 | 10.7 | 6 | 7.4 |
| Necessary self‐isolation | 0 | 0 | 1 | 3.6 | 1 | 1.2 |
| Missing data | 2 | 3.8 | 1 | 3.6 | 3 | 3.7 |
| New behavioral habits a | ||||||
| Yes—intermittent sleep | 27 | 43.5 | 9 | 32.1 | 36 | 40 |
| Yes—oral parafunctions (teeth clenching/grinding, nail/lip/cheek/tongue biting) | 18 | 29.1 | 4 | 14.3 | 22 | 24.4 |
| No | 17 | 27.4 | 15 | 53.6 | 32 | 35.6 |
New behavioral habits that appeared in respondents at the time they have already experienced both stressors; the percentage is calculated from total mentions, n = 90 (in 81 respondents).
The mean age was 33.6 (SD 11.4) with no statistically significant difference between men and women (p > .05). Fifty‐three respondents were from Zagreb (area affected by earthquakes) and its surroundings and 28 from the rest of Croatia.
When respondents from areas affected by earthquakes were evaluated, 7.5% rated the current situation as the strongest stress they have ever experienced, 30.2% considered it significantly stressful, the majority of participants (47.2%) considered it moderately stressful, 13.2% mildly stressful, while 1.9% considered situation not stressful at all. Of all respondents not affected by the earthquakes, none considered situation as the strongest stress, 21.4% considered the current situation significantly stressful, for 50%, it was moderately stressful, 25% rated the current situation as mildly stressful, while for 3.6%, it was not stressful at all.
When respondents needed to choose which situation caused more stress (COVID‐19 pandemic, earthquakes, both the same or one enhanced the stress of another), the majority of respondents from affected areas believed that the earthquakes have increased the stress associated with the COVID‐19 pandemic (34% out of 53 respondents), whereas, in respondents not affected by the earthquakes, the strongest stress was triggered by the COVID‐19 pandemic (42.9%).
Effects stress had on the deterioration of the symptoms were significantly different between respondents from areas affected by the earthquakes and respondents from not affected areas. Thus, the independent negative impact of COVID‐19 pandemic was 54.7% vs 28.6%, respectively (p = .025) and of earthquakes was 50.9% vs 25%, respectively (p = .024).
Fourteen respondents from areas affected by earthquakes (26.4%) reported the appearance of new symptoms after COVID‐19 escalation, and 22 (41.5%) reported the appearance of new symptoms after earthquakes.
Among respondents from not affected areas, 21.4% reported the appearance of new symptoms after COVID‐19 and 32.1% after earthquakes. There was no significant difference between number of patients with new symptoms with respect to the area affected by earthquake (p > .05). The most commonly reported new symptom was pain in the jaw joints (in front of or near the ear), followed by joint clicking and pain elsewhere in the head and face.
Mean NPRS for participants from areas affected by earthquakes before COVID‐19 pandemic was 2.9 (SD 2.5); immediately after escalation of pandemic, it was 3.7 (SD 2.4); immediately after the earthquakes, it was 3.5 (SD 2.6); and the most recent NPRS was 3.4 (SD 2.8). In participants from non‐affected areas, mean NPRS before COVID‐19 pandemic was 4.1 (SD 2.7); immediately after the escalation of pandemic, it was 4.3 (SD 2.9); immediately after the earthquakes, it was 4.1 (SD 2.7); and the most recent NPRS was 3.9 (SD 2.9). Figure 1 shows NPRS score changes for respondents from areas affected by the earthquakes and respondents from the non‐affected areas, as well as the pooled data and relevant statistical significances.
FIGURE 1.
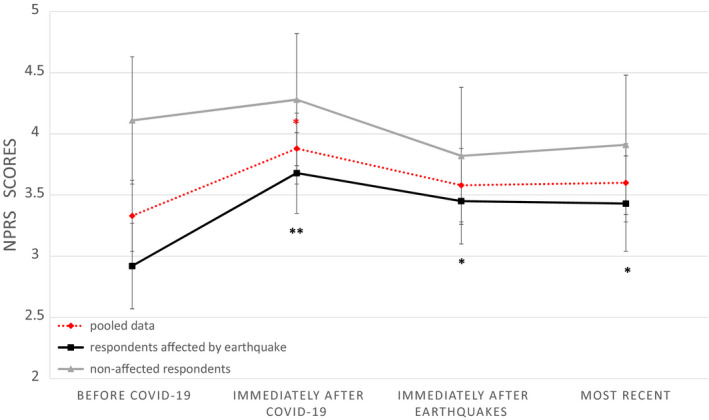
Changes in Numerical pain rating scale (NPRS) from baseline to three control points. NPRS of all respondents ("pooled data") is marked with dotted red line; NPRS of respondents from the areas affected by the earthquakes (respondents from Zagreb) is marked black; NPRS of respondents from non‐affected areas (non‐Zagreb respondents) is marked gray. Whiskers represent standard errors. Asterisk indicates a post hoc significant difference (within‐group comparisons, compared to baseline); *p < .05, **p < .001
In respondents from areas affected by the earthquakes, a positive correlation was found between the COVID‐19 impact on stress and NPRS immediately after COVID‐19 (r = .49, p < .001), as well as between the earthquake impact on stress and NPRS immediately after an earthquake (r = .54, p < .001), whereas no correlation was observed for unaffected areas.
List of new BH that respondents developed is presented in Table 1. Respondents from areas affected by earthquakes reported significantly more new BH when compared to respondents from non‐affected areas (p = .048).
4. DISCUSSION
Our study showed that the COVID‐19 pandemic appears to be generally more stressful than earthquakes. The pandemic has created an unprecedented amount of confusion and stress in various fields, causing an avalanche of information that could have further intensified the effect of stress (Jakovljevic et al., 2020). Therefore, it is understandable that most of the respondents experience such uncertain and novel situations as moderately to extremely stressful.
Moreover, we encountered a significant increase in spontaneous pain after the pandemic escalation, followed by a decrease in pain in spite of additional stressful event. Understandably, the earthquakes had a stronger emotional impact on directly exposed respondents (Bergiannaki et al., 2003; Galea et al., 2002). However, our hypothesis that additional stress would intensify the TMD‐related pain in respondents from affected areas was not confirmed. The pain intensity did not increase but rather dropped following earthquakes, showing that in Zagreb, the pandemic had more effect on pain intensity.
This (insignificant) decrease in NPRS scores is undoubtedly an unexpected and interesting finding contributing to the theory that a series of stressful events do not necessarily have a cumulative effect, but are more likely to have a much more complex interaction (Frodl & O'Keane, 2013). This interaction could have various interpretations.
National Crisis Headquarters' activities and their effort to direct the individuals through COVID‐19 pandemic could have prepared the organism for spontaneous and unexpected outcomes of any kind; also, a quick reaction of authorities to earthquake crisis may have helped in the reduction of overwhelming emotional reactions and accompanying somatization among some of the respondents after an earthquake. (Cvetković et al., 2015; Greenberg et al., 1993).
Additional explanation for our results could as well lie in the fact that immediately following a disaster such as an earthquake, psychological and somatic reactions experienced by victims tend to ease off within hours (Bergiannaki et al., 2003). The latter may explain why our respondents may not have perceived the earthquake effect as stressful as the pandemic since an event that lasts only for a shorter period might be disregarded while there is another superimposed stressor that keeps on compromising regular daily existence. Despite the fact that the somatic consequences of the earthquake could have been felt in the coming days, it is possible that respondents related their experience to the stress that emerged first and continues.
Conversely, we might observe the earthquakes as catastrophic events that diverted thoughts in respondents from affected areas from TMD symptoms to thoughts such as extreme fear from additional disasters (fight‐or‐flight model), and to empathy in non‐affected respondents for the affected city and people. According to this theory, the earthquakes "obscured" the somatization effect of the COVID‐19 pandemic. Stress can both increase and decrease body's lines of defenses, depending on a diversity of factors such as duration of the stressful event or the severity of the consequences caused by the stressor (Dragoş & Tănăsescu, 2010). With that in mind, acute stress might trigger the protective mechanisms in respondents from affected areas that could explain lower pain scores after the earthquakes. Due to the devastating effects of the earthquakes, we are more inclined to latter theories.
The results should be interpreted taking into account a discrepancy found between the frequency of individual cases of symptoms’ worsening due to two stressful events (in less than half of respondents) and a significant increase in pain in those individual cases, explaining that those who experienced a deterioration, although in minority, had a considerable increase of NPRS scores.
The effect of stress is also evident through the emergence of new BH. These habits have been shown to be significantly more common in subjects directly affected by both stressors (in respondents from affected areas). The correlation between the perception of stressful situations and spontaneous pain, as well as the onset of new BH, may indicate somatization in patients with TMD. Since we do not know which event predominantly caused BH in respondents, we cannot draw a certain conclusion from this finding.
Additionally, we need to call attention to an excellent response rate, as most of them were willing to respond (79.4%). We maintain good rapport with our TMD patients' cohort. Our interest in patients' health in stressful and unfamiliar times surely affected their readiness to partake in the survey. They probably reacted as to a kind of surrogate clinical appointment, as regular appointments were impossible at the time.
The limitations of study include the following: (a) the retrospective format in which respondents subjectively recall levels of pain in three time periods; (b) the lack of standardization and validation of the questionnaire, for it was the urgent reaction to unexpected occurrences; (c) the unmeasurable possibility that stressful events may have affected pain‐coping thresholds instead of the pain itself; (d) the highly selected group of respondents that makes our results difficult to generalize; and finally, (e) the uncontrolled study conditions typical for anonymous surveys.
This evaluation could, nevertheless, reveal psychological and psycho‐emotional information relevant to the patient's pain and disability problems. Our findings may reflect the paradigm of typical reaction of TMD to repeated stress. Thus, this could help clinicians understand patients’ needs in times of enhanced stress and to understand the effects stressful events might have on patients with the TMD diagnosis.
CONFLICT OF INTEREST
The authors declare that they have no potential conflicts of interest.
AUTHOR CONTRIBUTION
Ema Vrbanović : Conceptualization; Data curation; Investigation; Methodology; Visualization; Writing‐original draft; Writing‐review & editing. Iva Žilić Alajbeg: Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Visualization; Writing‐original draft; Writing‐review & editing. Ivan Alajbeg: Formal analysis; Investigation; Methodology; Supervision; Visualization; Writing‐original draft; Writing‐review & editing.
ACKNOWLEDGMENTS
This work has been fully supported by the Croatian Science Foundation Project “Genetic polymorphisms and their association with temporomandibular disorders” (No. IP‐2019‐04‐6211), Operational Program “Efficient Human Resources 2014‐2020,” and European Social Fund within the “Young Researchers' Career Development Project—Training of Doctoral Students.”
Vrbanović E, Alajbeg IZ, Alajbeg I. COVID‐19 pandemic and Zagreb earthquakes as stressors in patients with temporomandibular disorders. Oral Dis.2021;27(Suppl. 3):688–693. 10.1111/odi.13488
DATA AVAILABILITY STATEMENT
The layout of the questionnaire (in Croatian) is available at: https://drive.google.com/file/d/1Edf0D7EScO_MCqTS9k8IRGfisXuDOXGx/view?usp=sharing. The datasets generated and analyzed during the study are not publicly available; however, all data from this study are available from the corresponding author on reasonable request.
REFERENCES
- Auerbach, S. M. , Laskin, D. M. , Frantsve, L. M. , & Orr, T. (2001). Depression, pain, exposure to stressful life events, and long‐term outcomes in temporomandibular disorder patients. Journal of Oral and Maxillofacial Surgery, 59(6), 628–633. 10.1053/joms.2001.23371 [DOI] [PubMed] [Google Scholar]
- Beaton, R. D. , Egan, K. J. , Nakagawa‐Kogan, H. , & Morrison, K. N. (1991). Self‐reported symptoms of stress with temporomandibular disorders: Comparisons to healthy men and women. Journal of Prosthetic Dentistry, 65(2), 289–293. 10.1016/0022-3913(91)90177-x [DOI] [PubMed] [Google Scholar]
- Bergiannaki, J. D. , Psarros, C. , Varsou, E. , Paparrigopoulos, T. , & Soldatos, C. R. (2003). Protracted acute stress reaction following an earthquake. Acta Psychiatrica Scandinavica, 107(1), 18–24. 10.1034/j.1600-0447.2003.01467.x [DOI] [PubMed] [Google Scholar]
- Canales, G. T. , Guarda‐Nardini, L. , Rizzatti‐Barbosa, C. M. , Conti, P. C. R. , & Manfredini, D. (2019). Distribution of depression, somatization and pain‐related impairment in patients with chronic temporomandibular disorders. Journal of Applied Oral Science, 27, e20180210. 10.1590/1678-7757-2018-0210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cvetković, V. , Dragićević, S. , Petrović, M. , Mijaković, S. , Jakovljević, V. , & Gačić, J. (2015). Knowledge and perception of secondary school students in Belgrade about earthquakes as natural disasters. Polish Journal of Environmental Studies, 24(4), 1553–1561. 10.15244/pjoes/39702 [DOI] [Google Scholar]
- Dragoş, D. , & Tănăsescu, M. D. (2010). The effect of stress on the defense systems. Journal of Medicine and Life, 3(1), 10–18. [PMC free article] [PubMed] [Google Scholar]
- Frodl, T. , & O'Keane, V. (2013). How does the brain deal with cumulative stress? A review with focus on developmental stress, HPA axis function and hippocampal structure in humans. Neurobiology of Disease, 52, 24–37. 10.1016/j.nbd.2012.03.012 [DOI] [PubMed] [Google Scholar]
- Galea, S. , Ahern, J. , Resnick, H. , Kilpatrick, D. , Bucuvalas, M. , Gold, J. , & Vlahov, D. (2002). Psychological sequelae of the september 11 terrorist attacks in New York City. The New England Journal of Medicine, 346(13), 982–987. 10.1056/NEJMsa013404 [DOI] [PubMed] [Google Scholar]
- Greenberg, J. , Pyszczynski, T. , Solomon, S. , Pinel, E. , Simon, L. , & Jordan, K. (1993). Effects of self‐esteem on vulnerability‐denying defensive distortions: Further evidence of an anxiety‐buffering function of self‐esteem. Journal of Experimental Social Psychology, 29(3), 229–251. 10.1006/jesp.1993.1010 [DOI] [Google Scholar]
- Jakovljevic, M. , Bjedov, S. , Jaksic, N. , & Jakovljevic, I. (2020). COVID‐19 pandemia and public and global mental health from the perspective of global health security. Psychiatria Danubina, 32(1), 6–14. 10.24869/psyd.2020.6 [DOI] [PubMed] [Google Scholar]
- Jivnani, H. M. , Tripathi, S. , Shanker, R. , Singh, B. P. , Agrawal, K. K. , & Singhal, R. (2019). A study to determine the prevalence of temporomandibular disorders in a young adult population and its association with psychological and functional occlusal parameters. Journal of Prosthodontics, 28(1), e445–e449. 10.1111/jopr.12704 [DOI] [PubMed] [Google Scholar]
- Lazarus, R. S. , & Folkman, S. (1984). Stress Appraisal and Coping. New York, NY: Springer. [Google Scholar]
- Osiewicz, M. , Lobbezoo, F. , Ciapała, B. , Pytko‐Polończyk, J. , & Manfredini, D. (2020). Pain predictors in a population of temporomandibular disorders patients. Journal of Clinical Medicine, 9(2), 452. 10.3390/jcm9020452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of Zagreb (2020). Seismological service of the Geophysical Department of the Faculty of Science. [Earthquakes in Zagreb from March 22 to April 14, 2020] (in Croatian). April 19 2020, Retrieved from https://www.pmf.unizg.hr/geof/seizmoloska_sluzba/o_zagrebackom_potresu_2020?@=1lrg6#news_97581 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The layout of the questionnaire (in Croatian) is available at: https://drive.google.com/file/d/1Edf0D7EScO_MCqTS9k8IRGfisXuDOXGx/view?usp=sharing. The datasets generated and analyzed during the study are not publicly available; however, all data from this study are available from the corresponding author on reasonable request.


