Dear Editor,
We read with great interest the article by Schwartz et al 1 about generalized pustular figurate erythema (GPFE) related to hydroxychloroquine. The rapid spread of the new coronavirus has been associated with the need to use off‐label treatments in patients with Coronavirus Disease 2019 (COVID‐19). Hydroxychloroquine is an immunomodulator drug widely used in dermatology. It has demonstrated antiviral effects due to interference with the fusion process of the virus. In addition, chloroquine alters the glycosylation of the cellular receptors of coronaviruses and both of these agents are theoretically similar in their antiviral activity. 2 Widespread use of this medication is expected to be associated with an increased incidence of adverse effects.
Herein we report a case of acute generalized exanthematous pustulosis (AGEP)/drug reaction with eosinophilia and systemic symptoms (DRESS) overlap, following hydroxychloroquine administration. A 75‐year‐old female patient was admitted owing to a bilateral pneumonia by SARS‐coV‐2 infection. Hydroxychloroquine was started on admission. After 20 days, the patient developed a pruriginous rash consisting of non‐follicular pustules on an erythematous and edematous base located in flexural regions with facial edema (Figure 1). No mucosal involvement nor fever were present. Laboratory investigations showed mild leukocytosis and marked eosinophilia (2.24 × 109/L; ref. level < 0.6), with no liver enzymes abnormalities. Histological examination of a 4 mm punch biopsy revealed non‐follicular subcorneal pustules and mild‐moderate diffuse spongiosis with neutrophilic exocytosis in the epidermis. The underlying dermis exhibited moderate superficial edema with mild mixed interstitial inflammation (lymphocytes and neutrophils), as well as images of neutrophilic inflammation of eccrine ducts. Clinical and pathological findings were compatible with AGEP. The patient was started on intravenous metilprednisolone and progressively resolved within 3 to 4 weeks with widespread desquamation (Figure 2).
FIGURE 1.
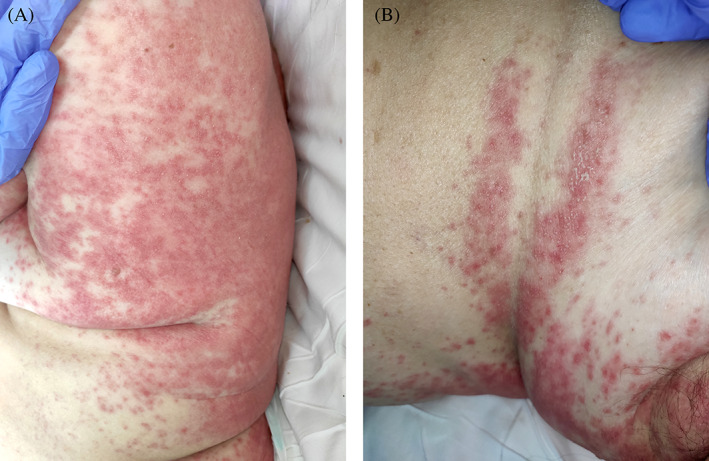
A, Millimetric non‐follicular sterile pustules arising over an oedematous erythema affecting mainly the upper trunk and folds. B, View of the same elementary lesions in the infra‐mammary fold at higher magnification
FIGURE 2.
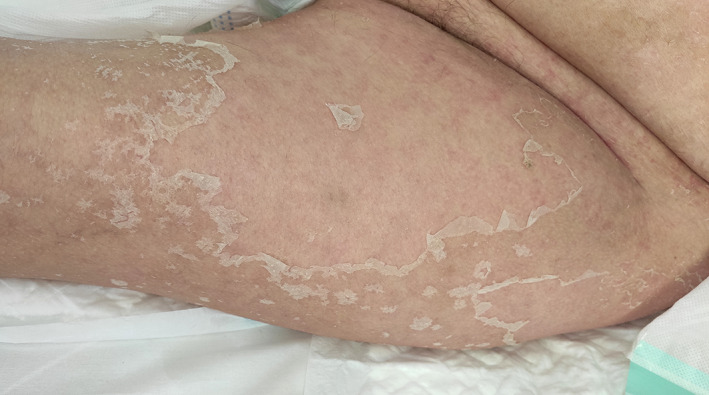
Evolution of the rash after 3 weeks with widespread desquamation
Skin manifestations of SARS‐CoV‐2 infection are not yet fully categorized. 3 It is likely that some of these exanthems correspond to drug reactions. GPFE has been described as a severe cutaneous drug reaction to hydroxychloroquine. Its longer latency period after drug intake (11‐21 days compared to 48 hours in typical AGEP), 4 , 5 longer duration (hypothesized to be due to his long half‐life which is approximately 40‐50 days), 4 targetoid morphology and recalcitrance to therapy (in contrast with the autorresolution within 15 days with the discontinuation of the causative drug in AGEP) are the main features. 1 Our case had morphological and histological findings consistent with AGEP, but also other overlapping features of DRESS (marked eosinophilia, long latency period). The absence of targetoid appearance or arciform distribution does not suggest that we are dealing with another entity, but a wider variety of possible clinical manifestations.
Histologically, a peculiar finding was the identification of neutrophilic eccrine ductitis, some of them coinciding on the subcorneal pustules. This could be explained by a concomitant miliaria pustulosa, a rare variant of miliaria rubra with neutrophilic infiltration, 6 favored by prolonged bedding. Other explanation is to be caused by the hydroxychloroquine. This seems improbable as neutrophilic eccrine hidradenitis present inflammation at the level of the glands 6 and it has not been described with this drug. Finally, considering the detection of SARS‐CoV‐2 in epithelial cells of eccrine glands by immunohistochemical techniques, 7 one possible hypothesis is that the neutrophilic inflammation of the AGEP spread through the eccrine ducts where the virus could be replicating. Since it is not possible to make conclusions with a single patient, more studies are needed.
The use of this medication has exponentially increased due to the pandemic. Although this is a rare adverse event with around 20 reported cases in the literature, 1 dermatologists must be aware of its existence given the current emergency health situation. The notification of new cases will allow a better characterization of the clinical presentation and management of these patients.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
All human and animal studies are approved by an Institutional Review Board.
REFERENCES
- 1. Schwartz RA, Janniger CK. Generalized pustular figurate erythema: a newly delineated severe cutaneous drug reaction linked with hydroxychloroquine. Dermatol Ther. 2020;33:e13380. 10.1111/dth.13380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sahraei Z, Shabani M, Shokouhi S, Saffaei A. Aminoquinolines against coronavirus disease 2019 (COVID‐19): chloroquine or hydroxychloroquine. Int J Antimicrob Agents. 2020;55(4):105945. 10.1016/j.ijantimicag.2020.105945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Galván Casas C, Català A, Carretero Hernández G, et al. Classification of the cutaneous manifestations of COVID‐19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020. 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mohaghegh F, Jelvan M, Rajabi P. A case of prolonged generalized exanthematous pustulosis caused by hydroxychloroquine—literature review. Clin Case Rep. 2018;6:2391‐2395. 10.1002/ccr3.1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Duman H, Topal IO, Kocaturk E, Cure K, Mansuroglu I. Acute generalized exanthematous pustulosis induced by hydroxychloroquine: a case with atypical clinical presentation. An Bras Dermatol. 2017;92(3):404‐406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nagai H, Nishigori C. Neutrophilic superficial eccrine ductitis: proposal of a new disease concept. Pediatr Dermatol. 2018;35:e105‐e109. 10.1111/pde.13386. [DOI] [PubMed] [Google Scholar]
- 7. Torrelo A, Andina D, Santonja C, et al. Erythema multiforme‐like lesions in children and COVID‐19. Pediatr Dermatol. 2020. [published online ahead of print, 2020 May 23]. 10.1111/pde.14246. [DOI] [PMC free article] [PubMed] [Google Scholar]


