Dear Editor,
During the COVID‐19 pandemic, the need to use special protective equipment to prevent contagion has been recognized as a fundamental element in the development of professional activity. The use of masks, gloves, and protective suits for many hours during the workday is the key to the development of this type of contact dermatitis. Health personnel are the main group of professionals at risk, with primary involvement of the nasal dorsum, cheeks, forehead and hands. 1 In fact, skin injuries related to the use of PPE are one of the most published topics in recent months. 2 From the 16 March 2020 to the 8 May 2020, our Contact Eczema Unit has been the reference consultation for the care of all health professionals in our hospital. A direct referral circuit was been created in collaboration with the Public Health Department. The performance of a specific guideline (Data S1) for the treatment of the different body areas affected by dermatitis concerning the use of PPE was disclosed in the services with the greatest impact: the Emergency Unit, Critic Care Unit, Internal Medicine and Infectious Disease Unit with confirmed COVID‐19 infection. A series of general recommendations were established for all workers (Table 1), as well as specific care by area. The number of registered workers in our hospital is 3200 people. From 16 March 2020 to 8 May 2020 (54 days), a total of 408 people have attended. The sex distribution was 87 men and 321 women have been treated. The incidence of hospital workers attended was 12.75%. The most frequent location was the hands (47%), followed by facial involvement (25.7%). Eczema, acne and rosacea were the most frequent skin diseases identified. We were observed that the 18.8% (77 patients) of the patients attended showed worsening of previously diagnosed skin diseases. We observed a marked reduction of face‐to‐face consultations in favor of teledermatology. In fact, the COVID‐19 pandemic has brought about a change in the format of dermatological consultations. 3 The rest of results are collected in Table 2.
TABLE 1.
General Skincare tips during the COVID‐19 pandemic
|
1. Avoid using makeup and other similar cosmetics during the working day 2. Avoid wearing jewelry and other decorative materials during the workday 3. Use cotton gloves as the first layer, and on top put the vinyl or nitrile gloves. 4. Change gloves every 30‐40 min, whenever possible. 5. Handwashing with mild syndet soaps or oils, fragrance‐free, and with the fewest preservatives possible. 6. Shower with warm water, short baths of no more than 10 min in length 7. Light touch drying of the skin after the shower, avoiding intense skin friction 8. Apply an emollient cream after the bath to the entire body surface. 9. Wash the scalp with mild or balancing shampoo. 10. Hands must be cared for more thoroughly. Among the care, a good rinse during hand washing is essential, and the application of emollient creams 2‐3 times a day. The best time to apply it will be right after breakfast (before the workday), after eating (after the workday), and before going to bed (at this time higher fat emollients can be applied to increase the hydration of the skin). |
TABLE 2.
Epidemiological data of professionals attended by sex, location of dermatitis, personal or telematic assistance, demographic of employees, and pre‐existing skin disease
| Professionals attendance | Attendance in person | Telematic assistance | Total |
|---|---|---|---|
| Male | 31 | 56 | 87 (21.3%) |
| Female | 129 | 192 | 321 (78.7%) |
| Location of skin lesion | Attendance in person | Telematic assistance | Employees profession | Pre‐existing skin diseases | Total |
|---|---|---|---|---|---|
| Hands |
Male: 15 Female: 60 |
Male: 22 Female: 95 |
C: 30 W: 12 NA: 50 N: 60 D: 40 |
CHE: 3 ACD: 0 AD: 7 ACD: 0 P: 1 |
192 (47.1%) |
| Face |
Male: 5 Female: 35 |
Male: 20 Female: 45 |
C: 32 W: 5 NA: 28 N: 33 D: 7 |
AD: 5 ACD: 0 R: 25 A: 3 SD: 4 P: 0 |
105 (25%) |
| Body |
Male: 10 Female: 22 |
Male: 11 Female: 43 |
C: 21 W: 8 NA: 17 N: 24 D: 16 |
AD: 20 ACD: 0 P: 2 |
86 (21.1%) |
| Scalp |
Male: 1 Female: 12 |
Male: 3 Female: 9 |
C: 3 W: 4 NA: 7 N: 9 D: 2 |
AD: 0 ACD: 0 SD: 6 P: 1 |
25 (6.1%) |
Abbreviations: C, cleaner; W, watchman; NA, nursing assistant; N, nurse; D, doctors; CHE, chronic hand eczema; AD, atopic dermatitis; R, rosacea; A, acne; SD, seborrheic dermatitis; P, psoriasis; ACD, allergic contact dermatitis.
The clinical spectrum of irritative contact eczema is quite varied, 4 affecting different body areas depending on the equipment we consider. It has been reported that more than 70% of health professionals have presented skin disorders. 5 The hands are the most frequent location (Figure 1A,B). The use of gloves and the frequent washing (exceeds 20 times a day) with soaps or hydro‐alcoholic solutions are the main factor regarding an irritating hand eczema. 6 Recent studies have reported that less than a third of health care professionals properly hydrate their hands. 7 On the face and ears, the continuous use of masks and protective glasses are the main source of contact for the appearance of eczema in these areas. The main facial area affected appears to be the chin and mandibular area, followed by the ears and eyelids (Figure 2A). Those patients with a history of seborrheic dermatitis (Figure 3A,B), acne, atopic dermatitis (Figure 1C‐E) or rosacea (Figure 3C) may experience an aggravation or flare‐up of the underlying dermatoses. In the trunk, the areas of folds such as the armpits (Figure 2B) are also seen affected by occlusion, friction, and increased sweating related to personal protective suits. This protective equipment may lead to exacerbation of some skin conditions such as atopic dermatitis. The scalp can also be affected by the continuous use of caps. Occlusion with plastic or rubber caps are responsible for the development of local inflammatory reactions. They can appear de novo, or cause an outbreak of seborrheic dermatitis, psoriasis, or atopic dermatitis. Itching and peeling are the main manifestations of the inflammatory reaction on the scalp.
FIGURE 1.
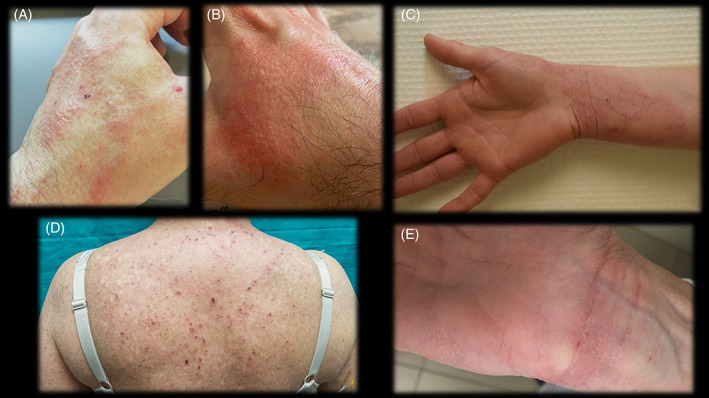
A and B, Irritant contact dermatitis on the back of the hand with erythematous papules. C, Irritant contact dermatitis on the ventral aspect of the wrist due to the use of gloves. D, Aggravated atopic dermatitis (located on the back) caused by the use of personal protective clothing. E, Aggravated atopic dermatitis (on the ventral aspect of the wrist) caused by the use of personal protective gloves
FIGURE 2.
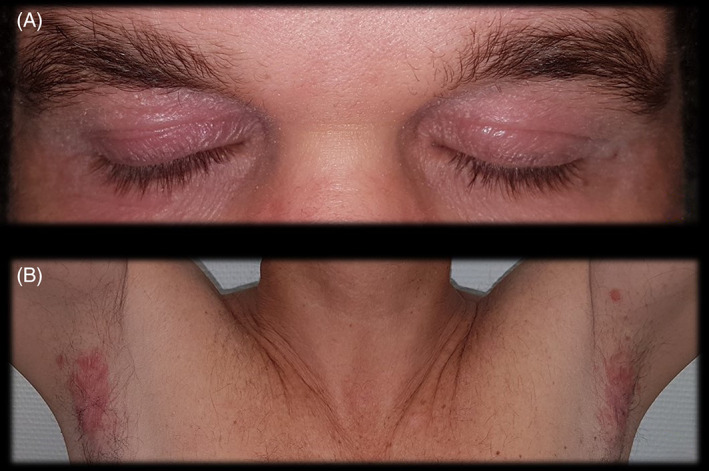
A, Irritant contact dermatitis on the eyelids caused by the use of protective glasses. B, Irritant contact dermatitis on the armpits caused by the use of personal protective clothing
FIGURE 3.

A and B, Aggravated seborrheic dermatitis by the use of a mask and personal protective glasses. C, Inflammatory rosacea outbreak caused by personal protective mask
Correct suitable daily skincare is important, as well as avoiding tight clothing as much as possible, which causes continuous friction of the area, and occlusion with alteration of perspiration. It is important to note that not all products on the market present the same characteristics, since those compounds with multiple preservatives and fragrances with high allergenic behavior can develop an allergic contact eczema in a susceptible patient. 8
PPE are essential to prevent disease transmission by the COVID‐19. The use of these equipment has caused the development of irritating contact eczemas in many professionals; therefore, careful skin care is essential to alleviate the eczematous process, and avoid its unfavorable evolution. It has been shown that the secondary skin effects of PPE can be so severe that they can influence the work performance of health care professionals. Recommending specific products for each of the situations will be important in the education and care of the skin of health professionals, who currently need it so much.
Supporting information
Data S1 Supporting Information.
REFERENCES
- 1. Abtahi‐Naeini B. Frequent hand washing amidst the COVID‐19 outbreak: prevention of hand irritant contact dermatitis and other considerations. Health Sci Rep. 2020;3:e163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Elston DM. Occupational skin disease among healthcare workers during the coronavirus (COVID‐19) epidemic. J Am Acad Dermatol. 2020;82:1085‐1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beiu C, Mihai M, Popa L, Cima L, Popescu MN. Frequent hand washing for COVID‐19 prevention can cause hand dermatitis: management tips. Cureus. 2020;12(4):e7506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lin P, Zhu S, Huang Y, et al. Adverse skin reactions among healthcare workers during the coronavirus disease 2019 outbreak: a survey in Wuhan and its surrounding regions [Epub ahead of print, 2020 April 7]. Br J Dermatol. 2020. 10.1111/bjd.19089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cavanagh G, Wambier CG. Rational hand hygiene during the coronavirus 2019 (COVID‐19) pandemic. J Am Acad Dermatol. 2020;82(6):e211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gisondi P, Piaserico S, Conti A, Naldi L. Dermatologists and SARS‐CoV‐2: the impact of the pandemic on daily practice [Epub ahead of print, 2020 April 22]. J Eur Acad Dermatol Venereol. 2020;34(6):1196–1201. 10.1111/jdv.16515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Patruno C, Fabbrocini G, Stingeni L, Napolitano M. The role of occupational dermatology in the COVID‐19 outbreak [Epub ahead of print, 2020 April 21]. Contact Dermatitis. 2020 Apr 21. 10.1111/cod.13568. [Online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Balato A, Ayala F, Bruze M, et al. European task force on contact dermatitis statement on coronavirus 19 disease (COVID‐19) outbreak and the risk of adverse cutaneous reactions [Epub ahead of print, 2020 April 30]. J Eur Acad Dermatol Venereol. 2020 Apr 30. 10.1111/jdv.16557. [Online ahead of print]. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1 Supporting Information.


