Abstract
This study concerns what lay people believe is the best way to allocate scarce medical resources. A sample of 515 individuals completed a short questionnaire asking them to rank‐order eight different ethical positions with respect to the allocation of scarce resources. They showed a strong preference for the ‘saves most lives’ and ‘sickest first’ options, with ‘reciprocity’ and a ‘lottery’ being least favoured. There was a reasonable degree of unanimity amongst respondents and comparatively few correlations with individual difference factors such as demography. The preference results are compared to expert recommendations (Emanuel et al., 2020, N. Engl. J. Med., 382, 2049) made in light of the current coronavirus pandemic, and differences are highlighted. Implications for scare medical resource allocations are discussed, and limitations of the study acknowledged.
Keywords: ethics, lottery, resource allocation, utilitarianism
Statement of contribution.
What is already known on this subject?
There are differences in allocation preferences for scarce medical resources between lay individuals, medical professionals and ethicists. During the current Coronavirus pandemic medical professionals and ethicists have provided allocation frameworks based on their views but the views of the general public have not been investigated.
What does this study add?
Lay people’s preferences for the allocation of scarce medical resources (assessed prior to the pandemic) show a relatively high level of agreement and are little influenced by individual differences.
There is disagreement in the preference order between ethicists and lay individuals – particularly with respect to the ‘sickest first’ and ‘youngest first’ allocation criteria.
A discussion of how allocation methods are perceived in relation to the current Covid‐19 crisis.
In all countries, whether developed or developing, the demand for a medical resource frequently exceeds the supply. In developed countries, societies are dealing with the scarcity of specific, highly sought after medical resources, whereas in developing countries, the scarcity is usually more widespread. Allocation of scarce medical resources is a highly contentious issue: To whom should these resources be allocated, by which criteria; and who makes the decision? (Cillo et al., 2012; Guindo et al., 2012
; Keller, Kwo, & Helft, 2014; Krütli, Rosemann, Törnblom, & Smieszek, 2016). There is a World Health Organization (WHO, 2014) report on this issue and many literature reviews (e.g., Scheunemann & Lewis, 2011). This issue has suddenly become a topic of great significance because of the COVID‐19 crisis and the universal shortage of particular medical resources such as intensive care beds and ventilators (Boreskie, Boreskie, & Melady, 2020; Rosenbaum, 2020).
There have been a number of systematic studies of scarce resource allocation focussing on attributes of the potential recipients of the resource by Furnham and his colleagues (e.g., Furnham, Ariffin, & McClelland, 2007; Furnham, Thomas, & Petrides, 2002; Furnham, Thomson, & McClelland, 2002; Nguyen Huynh, Furnham, & McClelland, 2020; Selvaraj, McClelland, & Furnham, 2019). In contrast, this study is specifically concerned with the preferences of the public for a particular system or principle to use when allocating scarce resources.
The issue of scarce medical resource allocation is of interest not only to ethicists, but also to psychologists, philosophers, policymakers, and the general public (Persad, 2017) especially given the current situation, and there is a growing applied and theoretical literature on this issue. Essentially, two philosophical principles, utilitarianism and egalitarianism, have been used to understand the ethics behind resource allocation methods (Lamb, 1990). There are, however, a number of other identifiable principles which will be explored in this paper.
Utilitarianism is a consequentialist theory which focuses on the outcomes of actions rather than the actions themselves. Here, the best/most ideal, action is one that brings about maximum happiness defined as ‘pleasure and the absence of pain’ (Mill, 1863, p. 10). Thus, utilitarianism would mean allocation to the person whose health and well‐being would bring about most happiness in society, thus giving rise to individual judgements of social worth (Banks, 1995).
Egalitarianism, which is a deontological theory, focuses on the act rather than the outcome, and the morality of the act is determined by a known and accepted set of rules (Broad, 1930). The theory asserts that all individuals are equal in terms of social worth. However, with scarce resources, some sort of selection usually has to be made.
Persad, Wertheimer, and Emanuel (2009) demonstrated that these two philosophical perspectives were insufficient to capture the complexity that surrounds the issue of resource allocation. They specified eight primary ethical principles for medical resource allocation. The two utilitarian allocation principles are based on saving the most number of lives and the most number of life‐years (also referred to as prognosis), respectively. The lottery and first‐come, first‐served methods are more individualistic and reflect an egalitarian approach to the allocation of resources. Prioritarianism, or prioritizing the disadvantaged, gives rise to two possible allocation methods: sickest first and youngest first. A consideration of the ethical principles underpinning the allocation of resources is of critical importance given the current COVID‐19 pandemic.
The mortality rates for COVID‐19 are much higher for vulnerable populations, in particular those individuals over the age of 80 years and those with underlying health conditions (Wu & McGoogan, 2020). Consequently, due to the limited supply of ventilators, doctors in some of the hardest hit regions of Italy have had to allocate ventilators to younger patients, on the principle that their prognosis is more favourable. However, this method of allocation is not the preferred choice of medical professionals, but it seemed necessary given the circumstances faced by the doctors (Rosenbaum, 2020).
Two further potential criteria for allocation were classified by Persad et al. (2009) under the heading ‘social usefulness’: instrumental value and reciprocity. These are defined thus: Instrumental value prioritizes those with specific skills and usefulness such as scientists producing a vaccine, front‐line health care workers treating critically ill patients, or key workers who are essential to maintain vital infrastructure. In normal circumstances, this would also include those who had agreed to improve their health following treatment (e.g., stopped smoking and lost weight) and thus would require fewer resources in the future. Reciprocity prioritizes those who have been useful to society in the past, such as giving blood or organ donation. Persad et al. suggested that the majority of these principles for allocation are morally justifiable but insufficient on their own. However, they consider the first‐come, first‐served and sickest first allocation methods to be inherently flawed and unfair in comparison to the other six principles, as the former incorporates irrelevant factors such as the wealth of the individual, and the later ignores prognosis.
Krütli et al. (2016) explored how lay people, general practitioners (GPs), medical students, and other health professionals evaluated the fairness of the following allocation principles for scarce medical resources: ‘sickest first’, ‘waiting list’, ‘prognosis’, ‘behaviour’ (i.e., prioritizing those who do not undertake risky behaviours that may negatively impact their condition), ‘instrumental value’, ‘combination of criteria’ (i.e., ‘youngest first’, ‘prognosis’, and ‘lottery’ principles), ‘reciprocity’ ‘youngest first’, ‘lottery’, and ‘monetary contribution’. Participants rated the allocation principles in three different patient scenarios (donor organs, hospital beds during an epidemic, and joint replacements).
Krütli et al. (2016) found that although GPs displayed different response patterns across the allocation scenarios, lay people were very consistent, and clearly favoured ‘sickest first’ followed by ‘waiting list’. These results are at odds with current conclusions proposed by some ethicists (e.g., Persad et al., 2009), who suggest that neither of these principles are morally justifiable. The ‘sickest first’ allocation method is prioritizing those who have the most need for the resources but not those that are most likely to survive, and wealthy individuals can in principle place themselves on multiple waiting lists to take advantage of the ‘first‐come, first‐served’ principle. Many countries have adopted specific protocols that delineate which groups of individuals should be prioritized in a situation of scarcity. For example, the Swiss Federal Office for Public Health would prioritize health care workers, followed by individuals at higher risk of adverse outcomes and then individuals who are integral to the running of crucial services – in a situation for administering a vaccine against pandemic influenza. This protocol prioritizes instrumental value and then prognosis. Organ donation, however, prioritizes the sickest first and then prognosis (Krütli et al., 2016).
Emanuel et al. (2020) suggest there are four values that underlie allocation protocols: ‘maximizing the benefits produced by scarce resources, treating people equally, promoting and rewarding instrumental value, and giving priority to the worst off’ (p. 2). Further, they stress that an individual's wealth should in no way influence his or her priority in relation to the receipt of medical resources. There are a number of ways that these values can be put into practice. Maximizing benefits can be operationalized by both the ‘Saving the most lives’ or ‘Prognosis’ allocation methods; treating people equally can be achieved through the ‘lottery’ allocation method or on a ‘first‐come, first‐served’ basis; instrumental value can be both retrospective (‘reciprocity’) and prospective; and prioritizing the worst off is captured by the ‘sickest first’ and ‘youngest first’ criteria. Emanual et al. recommend that in the current COVID‐19 pandemic, maximizing benefits should be the most important value for allocating medical resources when treating patients.
The current crisis has meant that there is much debate surrounding medical ethics and ethical decision‐making (Pauls, Migneault, & Bakewell, 2020). With many health care systems across the world struggling to meet the demand in the current crisis, medical professionals have had to make life and death decisions about the allocation of medical resources. The majority of research and debate has focused on establishing an allocation framework based on the views of medical practitioners and ethicists. However, with the exception of Krütli et al. (2016), there has been little serious investigation into the beliefs of lay individuals with respect to the allocation of scarce resources. This study aims to do just this.
Method
Participants
In total, 515 participants completed the questionnaire, of which 50% were female (age range: 18–70 years, M = 22.6 years, SD = 10.15). In all, 44.7% had a degree and 63% were single (21% married, 17% co‐habiting). Participants competently spoke an average of 1.94 languages (SD = 0.82), and 46.4% of the sample had children. Additionally, they rated themselves on the following scales: How religious are you? (Not at all 1 to Very 8); M = 2.09 (SD = 2.75); How would you describe your political beliefs? (Very Left Wing 1 to Very Right Wing 8); M = 5.38 (SD = 1.97); How Optimistic are you? (Not at all 1 to Very 8); M = 5.68 (SD = 1.94). They also rated themselves on how healthy they were from very poor (1) to very good (100); M = 68.62 (SD = 19.53). They also rated whether they thought alternative medicine worked on a 7 point (Disagree 1 to Agree 7); M = 4.11 (SD = 2.49). Asked if they believed in life after death 53.8% said no, and 45.8% yes.
Questionnaire
Medical people often have to make difficult ethical choices when they have to choose who to treat because there are too many people wanting treatments that are limited. As a consequence, ethicists have come up with different systems, strategies, or principles. A recent study suggests there are essentially eight principles that may be used to allocate scarce medical interventions. These are listed below: In this questionnaire, we are interested in your views and which principles you personally would advocate. We would like you to rank order these. Please read through all eight then put a 1 (meaning most preferred) against the one you think is best/fairest. Then, put a 2 against the principle you think next fairest. Continue until you have ranked all eight.
RANK (1–8)
_____ Lottery: the random allocation of interventions, through drawing recipients blindly.
_____First‐come, first‐served: allocating interventions based on the order of request, or requirement.
_____Sickest first: prioritizing those with the worst future prospects if left untreated.
_____Youngest first: prioritizing those who have had the least life years, and thus have the potential to live longer if cured.
_____Save the most lives: aiming to save the most individual lives possible, through offering all people treatment.
_____Prognosis or life‐years: aiming to save the most life‐years, thus prioritizing those with positive prognoses, and excluding those with poor prognoses.
_____Instrumental value: prioritizing those with specific skills and usefulness – for example, those producing a vaccine, or those who have agreed to improve their health following treatment and thus requiring fewer resources (stop smoking, lose weight, etc.)
_____Reciprocity – prioritizing those who have been useful in the past – for example, past organ donors.
Results
Complete rank data for the eight ethical principles were provided by 468 participants. Individuals who incorrectly gave multiple ethical principles the same level of preference were removed, as well as those that had missing data. There was no evidence to suggest that data were missing other than at random, Little's MCAR test, χ2(20) = 20.15, p = .449. Table 1 shows the mean rank position of each of the eight principles (ordered from lowest – most preferred to highest – least preferred) for participants with complete data. To obtain a measure of the extent to which participants were in agreement about the relative importance of the eight ethical principles, Kendall's coefficient of concordance was computed and was found to be significant, W = .40, χ2(7) = 1305.73, p < .001. This indicates a moderate level of agreement amongst the participants.
Table 1.
The mean rank position of the eight ethical principles
| Ethical principle | M (SD) | 95% CI |
|---|---|---|
| Save the most lives | 2.28 (1.52) | 2.14–2.42 |
| Sickest first | 2.69 (1.85) | 2.52–2.86 |
| Youngest first | 3.66 (1.73) | 3.50–3.82 |
| Prognosis – or life years | 4.24 (1.77) | 4.08–4.40 |
| First‐come, first‐served | 5.19 (1.92) | 5.02–5.36 |
| Instrumental value | 5.47 (1.86) | 5.30–5.64 |
| Reciprocity | 5.92 (1.59) | 5.78–6.06 |
| Lottery | 6.56 (1.97) | 6.38–6.74 |
The confidence intervals shown in Table 1 show that the only principles with overlapping confidence intervals were ‘first‐come, first‐served’ and ‘instrumental value’. However, when examining the distribution of the difference between the rankings, the 95% confidence interval did not capture zero. Therefore, it can be concluded that all of the mean rankings for the eight principles are significantly different from one another.
Individual correlates
Table 2 shows the distribution of first choice of most preferred mechanism for medical resource allocation. The most popular choice was ‘Save the most lives’, followed by ‘Sickest first’ and then ‘Youngest first’. These three choices will be examined further. Due to the infrequent selection of the other choices as most preferred, the sample sizes were not adequate for data analysis, and these choices were re‐coded and placed in a category labelled ‘Other’.
Table 2.
Frequency of most preferred ethical principle
| First choice | Frequency | Per cent |
|---|---|---|
| Lottery | 11 | 2.4 |
| First‐come, first‐served | 12 | 2.6 |
| Sickest first | 151 | 32.3 |
| Youngest first | 45 | 9.6 |
| Save the most lives | 196 | 41.9 |
| Prognosis or life‐years | 24 | 5.1 |
| Instrumental value | 24 | 5.1 |
| Reciprocity | 5 | 1.1 |
| Total | 468 | 100 |
Table 2 shows the first choices of the participants. We ran a multinomial logistic regression to investigate which aspects of individuals influenced their most preferred solution for the allocation of medical resources. Specifically, we investigated which individual differences lead individuals to prefer an allocation method that is not the most common preferred allocation method (in this sample, the most common first choice was ‘Save the most lives’). We used eight individual difference criteria as predictors: sex, age, education, ratings of health, religious beliefs, political beliefs, belief in the efficacy of alternative medicine, and belief in life after death. The reference category was set to be ‘Save the most lives’. The likelihood ratio test statistic suggests that final model contains non‐zero predictors: χ2(24) = 54.49, p < .001. The model compares each category: sickest first, young first, and other, to the reference category.
Table 3 shows the parameter estimates for each predictor variable with each comparison in the model. The multinomial regression model made three comparisons: those individuals that selected ‘Sickest first’ to the most common choice, those individuals that selected ‘Youngest first’ to the most common choice, and those individuals that selected any of the other five options to the most common choice. Table 4 shows which predictors have a significant effect in the overall model compared to the nested models in Table 3, and the majority of predictors investigated are significant or close to significance.
Table 3.
Parameter estimates for predictors in each comparison model
| B | SE | Wald | df | Sig. | Exp(B) | 95% Confidence interval for exp(B) | ||
|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||||
| Sickest first | ||||||||
| Intercept | −1.619 | 0.686 | 5.564 | 1 | 0.018 | |||
| Gender | 0.636 | 0.238 | 7.157 | 1 | 0.007 | 1.888 | 1.185 | 3.008 |
| Age | 0.015 | 0.012 | 1.633 | 1 | 0.201 | 1.015 | 0.992 | 1.040 |
| Education | 0.118 | 0.231 | 0.258 | 1 | 0.611 | 1.125 | 0.715 | 1.770 |
| Ratings of health | 0.009 | 0.006 | 2.303 | 1 | 0.129 | 1.009 | 0.997 | 1.021 |
| Religious beliefs | −0.039 | 0.050 | 0.606 | 1 | 0.436 | 0.962 | 0.871 | 1.061 |
| Political beliefs | 0.025 | 0.064 | 0.154 | 1 | 0.695 | 1.025 | 0.904 | 1.163 |
| Efficacy of Alt Med | −0.096 | 0.052 | 3.430 | 1 | 0.064 | 0.909 | 0.821 | 1.006 |
| Life after death | 0.508 | 0.275 | 3.401 | 1 | 0.065 | 1.662 | 0.969 | 2.850 |
| Youngest first | ||||||||
| Intercept | −3.223 | 1.097 | 8.627 | 1 | 0.003 | |||
| Gender | −0.088 | 0.371 | 0.057 | 1 | 0.812 | 0.915 | 0.442 | 1.895 |
| Age | 0.030 | 0.017 | 3.315 | 1 | 0.069 | 1.031 | 0.998 | 1.065 |
| Education | −0.230 | 0.361 | 0.406 | 1 | 0.524 | 0.795 | 0.392 | 1.611 |
| Ratings of health | 0.028 | 0.010 | 7.491 | 1 | 0.006 | 1.029 | 1.008 | 1.050 |
| Religious beliefs | −0.194 | 0.083 | 5.382 | 1 | 0.020 | 0.824 | 0.700 | 0.970 |
| Political beliefs | −0.140 | 0.094 | 2.198 | 1 | 0.138 | 0.869 | 0.723 | 1.046 |
| Efficacy of Alt Med | −0.021 | 0.079 | 0.068 | 1 | 0.794 | 0.980 | 0.839 | 1.143 |
| Life after death | 0.423 | 0.413 | 1.050 | 1 | 0.305 | 1.527 | 0.680 | 3.432 |
| Other | ||||||||
| Intercept | −1.116 | 0.834 | 1.788 | 1 | 0.181 | |||
| Gender | −0.122 | 0.304 | 0.161 | 1 | 0.688 | 0.885 | 0.488 | 1.606 |
| Age | 0.029 | 0.015 | 3.813 | 1 | 0.051 | 1.030 | 1.000 | 1.060 |
| Education | 0.617 | 0.294 | 4.406 | 1 | 0.036 | 1.854 | 1.042 | 3.298 |
| Ratings of health | 0.005 | 0.007 | 0.486 | 1 | 0.486 | 1.005 | 0.991 | 1.020 |
| Religious beliefs | −0.106 | 0.066 | 2.609 | 1 | 0.106 | 0.899 | 0.790 | 1.023 |
| Political beliefs | −0.147 | 0.079 | 3.469 | 1 | 0.063 | 0.864 | 0.740 | 1.008 |
| Efficacy of Alt Med | −0.178 | 0.068 | 6.969 | 1 | 0.008 | 0.837 | 0.733 | 0.955 |
| Life after death | 0.923 | 0.346 | 7.132 | 1 | 0.008 | 2.518 | 1.278 | 4.957 |
The reference category is as follows: Save the most lives.
Table 4.
Likelihood ratio tests of each predictor in final model
| Effect | Model fitting criteria | −2 Log likelihood of reduced model | Likelihood ratio tests | Sig. | ||
|---|---|---|---|---|---|---|
| AIC of reduced model | BIC of reduced model | Chi‐square | df | |||
| Gender | 1159.86 | 1259.17 | 1111.86 | 10.059 | 3 | 0.018 |
| Age | 1155.38 | 1254.69 | 1107.38 | 5.581 | 3 | 0.134 |
| Education | 1155.64 | 1254.95 | 1107.64 | 5.840 | 3 | 0.120 |
| Ratings of health | 1158.92 | 1258.23 | 1110.92 | 9.124 | 3 | 0.028 |
| Religious beliefs | 1157.09 | 1256.39 | 1109.09 | 7.285 | 3 | 0.063 |
| Political beliefs | 1156.40 | 1255.70 | 1108.40 | 6.596 | 3 | 0.086 |
| Efficacy of Alt Med | 1158.45 | 1257.76 | 1110.45 | 8.654 | 3 | 0.034 |
| Life after death | 1158.00 | 1257.30 | 1110.00 | 8.198 | 3 | 0.042 |
Comparing ‘Sickest first’ to ‘Save the most lives’
The only significant predictor was Gender but whether participants believed in life after death and the efficacy of alternative medicine were quite close to significance (p = .065 and p = .064, respectively). The odds ratio for females relative to males is 1.89 for preferring ‘Sickest first relative to ‘Save the most lives’ given all other predictor variables in the model are held constant. In other words, females are 1.89 times more likely than males to prefer ‘Sickest first’ to ‘Save the most lives’, p = .007.
The odds ratio for those believing in life after death relative to those that do not believe is 1.66 for preferring ‘Sickest first’ relative to ‘Save the most lives’ given all other predictor variables in the model are held constant. Thus, participants believing in life after death are 1.66 times more likely than those that do not believe in life after death to prefer ‘Sickest first’ to ‘Save the most lives’, p = .065.
The odds ratio for those believing in the efficacy of alternative medicine relative to those that do not believe in the efficacy of alternative medicine is .91 for preferring ‘Sickest first’ relative to ‘Save the most lives’ given all other predictor variables in the model are held constant. In other words, participants believing efficacy of alternative medicine are more likely than those that do not believe in its efficacy to prefer ‘Save the most lives’ to ‘Sickest first’, p = .064.
Comparing ‘Youngest first’ to ‘Save the most lives’
The significant predictors were how religious participants viewed themselves and their self‐perception of their physical health. The odds ratio for more religious participants relative to less religious participants is .82 for preferring ‘Youngest first’ relative to ‘Save the most lives’ given all other predictor variables in the model are held constant. Thus, those participants that are more religious are more likely than those less religious to prefer ‘Save the most lives’ to ‘Youngest first’, p = .020.
The odds ratio for those perceiving their physical health to be good relative to those that do not is 1.03 for preferring ‘Youngest first’ relative to ‘Save the most lives’ given all other predictor variables in the model are held constant. Therefore, participants perceiving their physical health to be better are 1.03 times more likely than those that do not perceive their physical health to be good to prefer ‘Youngest first’ to ‘Save the most lives’, p = .006.
Comparing ‘Other’ to ‘Save the most lives’
The significant predictors were as follows: participants’ belief in alternative medicine, belief in life after death, and whether or not they had a university degree. Age was also very close to significance, p = .051. The odds ratio for those participants who had a greater belief in the success of alternative medicine relative to those that do not is .84 for preferring ‘Other’ relative to ‘Save the most lives’ given all other predictor variables in the model are held constant. In other words, those participants that believe in alternative medicine are more likely than those that do not to prefer ‘Save the most lives’ to ‘Other’, p = .008.
The odds ratio for those believing in life after death relative to those that do not is 2.52 for preferring ‘Other’ relative to ‘Save the most lives’ given all other predictor variables in the model are held constant. So, participants believing in life after death are 2.52 times more likely than those that do not believe in life after death to prefer ‘Other’ allocations for medical resources to ‘Save the most lives’, p = .008.
The odds ratio for those with a university degree relative to those that do not is 1.85 for preferring ‘Other’ relative to ‘Save the most lives’ given all other predictor variables in the model are held constant. In other words, participants with a university degree are 1.85 times more likely than those without a degree to prefer ‘Other’ allocations for medical resources to ‘Save the most lives’ p = .036.
The odds ratio for older individuals compared to younger individuals is 1.03 for preferring ‘Other’ relative to ‘Save the most lives’ given all other predictor variables in the model are held constant. In other words, participants who are older are 1.03 times more likely than those that are younger to prefer ‘Other’ allocations for medical resources to ‘Save the most lives’ p = .051.
Discussion
There are two important results from this study. The first is the degree of public consensus evident in Tables 1 and 2. This shows considerable agreement about which principles are most and least favoured. The preference for ‘save the most lives’ seen in this lay sample is the same first preference suggested by experts in the field (Emanuel et al., 2020). The results also indicate that people tend to be utilitarians rather than egalitarians. Very few participants in the current sample chose the instrumental categories of ‘instrumental value’ or ‘reciprocity’ as an highly rated choice, which is consistent with the findings of Krütli et al. (2016) for both lay and GP participants, but at odds to what the experts suggest in their recent recommendations (Emanuel et al., 2020).
Emanuel et al. (2020) provided six recommendations for allocating medical resources in the current crisis. The first is that maximizing benefits is the most important value, and therefore, the priority should be allocating resources to save the most lives and providing more years of life. The second recommendation is that front‐line care health workers should be given priority because they are essential to deal with the crisis and therefore have instrumental value. The third recommendation is that if patients have a similar prognosis then an allocation method that ensures equality (such as a lottery method) should be used instead of first‐come, first‐served. Their fourth recommendation is specific to what we currently know about the coronavirus which is that it appears not to have significant negative effects on children and young people. Therefore, they recommend that the youngest are not prioritized – in particular for vaccines – when (or if) they become available. The fifth recommendation centres on prioritizing anyone who has participated in research to find vaccines or therapies to combat the virus. These individuals are providing a wider benefit whilst also putting themselves at risk and therefore should be rewarded. The final recommendation is that resources should be allocated equally between patients with COVID‐19 and patients with other life‐threatening illnesses.
A pictorial representation of the decision‐making flow guided by expert suggestions from Emanuel et al. (2020) is shown in Figure 1, and the mean rank‐ordered preferences in the current sample are in Figure 2. As can be seen, at the first level, there is agreement: Both groups prefer to save the most lives with a population. However, at the next level, divergence of opinion is evident. The experts continue to wish to maximize benefits of the resources with a preference for maximizing ‘life‐years’, however, the lay sample in this study shift to prioritizing those who are worst off. An important caveat is that the expert opinion is based on the current COVID‐19 crisis and therefore incorporates into the decision‐making factors that are specific to the current pandemic, such as the reduced severity of symptoms in the young. The lay sample was collected prior to the emergence of COVID‐19.
Figure 1.
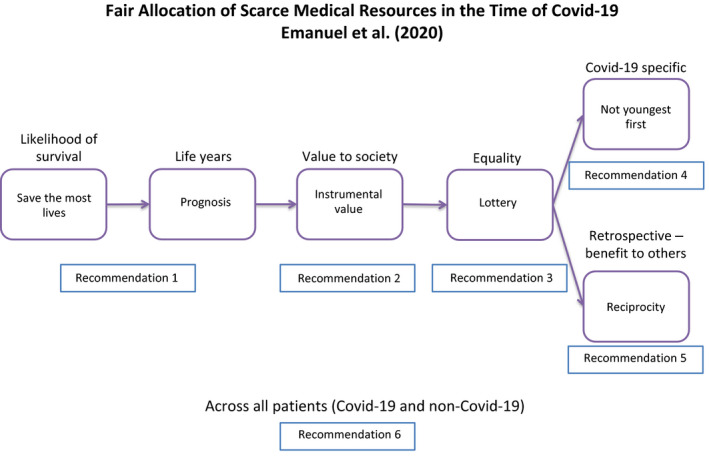
A pictorial representation of expert suggests for resource allocation based on Emanuel et al. (2020).
Figure 2.
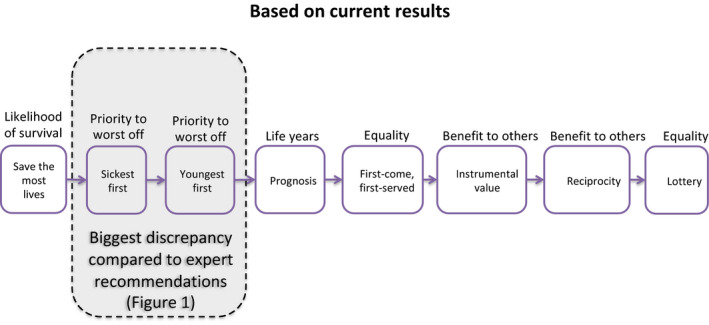
A pictorial representation of preferences for resource allocation based on results of current study.
The second main finding is that there are relatively few individual difference metrics which can predict the participants’ preferences. Studies which have looked not at the principles of allocation, but the recipients of allocation, show that individuals are happy to make very clear choices dependent on the recipients demography (sex, age, education), lifestyle (smoking, drinking), ideology (political and religious beliefs), and social group (class, ethnicity, foreignness) (e.g., Furnham et al., 2007). Equally, they are relatively happy to prioritize according to the medical condition, particularly the extent to which the problem is primarily caused by the patient themselves (i.e., by their lifestyle) or whether it is seen to be beyond the control of the patient (Nguyen Huynh et al., 2020).
Yet in this study, where we examined a wide range of individual difference factors, few seemed to impact on the preference for an allocation principle. We did find some differences: Women prefer ‘Sickest first’ over ‘Save the most lives’. Religious individuals preferred to save the most lives rather than focusing on the young. Older and better‐educated people were more likely to favour some less popular principles.
The results could be interpreted partly in terms of self‐interest. In general, women live longer than men, and young people are likely to live longer than older people. Those who rated themselves as having good physical health (normally age‐related) showed a preference for ‘youngest first’ over ‘save the most lives’.
There are a number of implications that follow from research in this area. In most countries, it is politicians who allocate financial resources, but it is medical staff (perhaps informed by ethical committees) who make decisions about individual patients. Informal conversations with doctors suggest that few articulate clear ethical principles in their daily work and that there is disagreement between them. Studies such as this at least given them information about what the public favours. The doctors dealing with the COVID‐19 crisis have highlighted their discomfort and concern with the decisions they have had to make in the allocation of ventilators in northern Italy when capacity was overwhelmed (Rosenbaum, 2020), and with many medical professionals requesting guidance on how they should be making allocation decisions in such circumstances (Townsend & Eburn, 2020).
There are also implications for the study of medical ethics. Krütli et al. (2016) concluded ‘A number of ethicists reject ‘sickest first’ and ‘waiting list’ as morally unjustifiable allocation principles, whereas those allocation principles received the highest fairness endorsements by lay people and to some extent also by health professionals. Decision‐makers are advised to consider whether or not to give ethicists, health professionals, and the general public an equal voice when attempting to arrive at maximally endorsed allocations of scarce medical resources’ (p. 2). In the current pandemic crisis, there is a great deal of discussion about the most appropriate way to arrive at a just medical resources allocation principle (e.g., Boreskie et al., 2020; Pauls et al., 2020; Solnica, Barski, & Jotkowitz, 2020) but little or no empirical data to suggest what the public think.
An important insight for policymakers in the current crisis is that at the first level of decision‐making there is universal agreement between the experts and lay people but as Figures 1 and 2 show there is quite a significant deviation at the second level. This suggests that the general public may struggle to agree with decision‐making that is being made at this level and beyond. Although the decisions made concerning medical resources may seem unfair at the level of the individual, it must be borne in mind that such decisions may have to be made (particularly if available resources are overwhelmed) in order to save the most lives in the population.
For example, the ageist approach evident in Italy (Rosenbaum, 2020) is a distressing criteria but the situation is not that clear cut. Other healthcare professionals highlight the fact that age may appear to be a criterion but other factors, which tend to be confounded with age, are the actual decision criteria, such as frailty and polymorbidity (Boreskie et al., 2020). Multiple factors are involved in triaging patients and regardless of whether or not medical resources are strained those factors relating to patients likelihood of survival are the ones that will save the most lives at the population level (Pauls et al., 2020).
Medical resource allocation principles are applied at the population level, but decision‐making at the individual level may not always reflect population‐level principles. As an example, in the current crisis if a medical professional had a single ventilator and two patients with similar symptoms and prognosis that needed the ventilator to survive. If one patient was a 13‐year‐old child and the other an 85‐year‐old adult, most individuals would give the ventilator to the child: youngest‐first. However, when a COVID‐19 vaccine is developed, initially there will not be enough vaccine to vaccinate everyone. Consequently, the most at‐risk groups such as the elderly would likely be targeted first. Indeed, in the UK, the seasonal flu jab is available – only to the elderly (or those with a health condition) for free on the NHS. So not youngest first – but oldest first.
There were a number of limitations in this study. It was run in 2019 before the COVID‐19 virus pandemic. There is, however, no reason to assume that people have or would change their views on allocation, though recent public debate and personal experiences with the pandemic may have influenced their preferred philosophy. For example, it appears that in general, the young are far less adversely affected by the virus than the old, which might influence a decision to allocate resources to the youngest as a matter of principle, in the event of a shortage. Thus, future research should examine what effect the current situation is having on individual's decision‐making in relation to allocation of medical resources – and the allocation of personal protective equipment.
A second limitation, statistical rather than theoretical, was the use of a rank‐order methodology which limits the type of analysis that can be undertaken. Researchers in the area point out that if people are given ratings rather than rankings they often choose not to make distinctions between patients with different characteristics, whereas ranking forces participants to make such distinctions. Indeed, often people who take part in these studies express some anxiety at being ‘asked to play God’, yet do not suggest who should be making these crucial ethical decisions (Furnham, Thomas, et al., 2002; Furnham, Thomson, et al., 2002). But such decisions are being made by doctors across the world because of the COVID‐19 pandemic – and an ethical framework which is acceptable to both health professionals and the lay public is urgently needed.
Conflicts of interest
All authors declare no conflict of interest.
Author contributions
Adrian Furnham (Conceptualization; Resources; Writing – original draft); Alastair McClelland (Data curation; Methodology); Simmy Grover (Formal analysis; Visualization; Writing – review and editing).
Ethics permission code
CEHP/514/2017.
Data availability statement
An SPSS file of the data is available on request from the first author.
References
- Banks, G. J. (1995). Legal & ethical safeguards: Protection of society's most vulnerable participants in a commercialized organ transplantation system. American Journal of Law & Medicine, 21, 45–110. [PubMed] [Google Scholar]
- Boreskie, K. F. , Boreskie, P. E. , & Melady, D. (2020). Age is just a number–and so is frailty: Strategies to inform resource allocation during the COVID‐19 pandemic. Canadian Journal of Emergency Medicine, 2020, 1–3. 10.1017/cem.2020.358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broad, C. D. (1930). Five types of ethical theory. London, UK: Routledge. [Google Scholar]
- Cillo, U. , Burra, P. , Mazzaferro, V. , Belli, L. , Pinna, A. D. , Spada, M. , Nanni Costa, A. , & Toniutto, P. , (2015). A multistep, consensus‐based approach to organ allocation in liver transplantation: Toward a “blended principle model”. American Journal of Transplantation, 15(10), 2552–2561. 10.1111/ajt.13408 [DOI] [PubMed] [Google Scholar]
- Emanuel, E. J. , Persad, G. , Upshur, R. , Thome, B. , Parker, M. , Glickman, A. , … Phillips, J. P. (2020). Fair allocation of scarce medical resources in the time of Covid‐19. New England Journal of Medicine, 382, 2049–2055. 10.1056/NEJMsb2005114 [DOI] [PubMed] [Google Scholar]
- Furnham, A. , Ariffin, A. , & McClelland, A. (2007). Factors affecting allocation of scarce medical resources across life‐threatening medical conditions. Journal of Applied Social Psychology, 37, 2903–2921. 10.1111/j.1559-1816.2007.00287.x [DOI] [Google Scholar]
- Furnham, A. , Thomas, C. , & Petrides, K. V. (2002). Patient characteristics and the allocation of scarce medical resources. Psychology, Health & Medicine, 7, 99–106. 10.1080/13548500120101595 [DOI] [Google Scholar]
- Furnham, A. , Thomson, K. , & McClelland, A. (2002). The allocation of scarce medical resources across medical conditions. Psychology and Psychotherapy, 75, 189–203. 10.1348/147608302169643 [DOI] [PubMed] [Google Scholar]
- Guindo, L. A. , Wagner, M. , Baltussen, R. , Rindress, D. , van Til, J. , Kind, P. , & Goetghebeur, M. M. (2012). From efficacy to equity: Literature review of decision criteria for resource allocation and healthcare decisionmaking. Cost Effectiveness and Resource Allocation, 10(1), 9. 10.1186/1478-7547-10-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller, E. , Kwo, P. , & Helft, P. (2014). Ethical considerations surrounding survival benefit‐based liver allocation. Liver Transportation, 20, 140–146. 10.1002/lt.23780 [DOI] [PubMed] [Google Scholar]
- Krütli, P. , Rosemann, T. , Törnblom, K. Y. , & Smieszek, T. (2016). How to fairly allocate scarce medical resources: Ethical argumentation under scrutiny by health professionals and lay people. PLoS One, 11(7), e0159086. 10.1371/journal.pone.0159086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb, D. (1990). Organ transplants and ethics. New York, NY: Routledge. [Google Scholar]
- Mill, J. S. (1863). Utilitarianism. London, UK: Parker, Son and Bourn. [Google Scholar]
- Nguyen Huynh, A. , Furnham, A. , & McClelland, A. (2020). A cross‐cultural investigation of the lifestyle factors affecting laypeople's allocation of a scarce medical resource. Health, 12, 141–157. 10.4236/health.2020.122013 [DOI] [Google Scholar]
- Pauls, M. A. , Migneault, D. , & Bakewell, F. (2020). Ethical considerations in the allocation of critical care resources when capacity is overwhelmed. Canadian Journal of Emergency Medicine, 1–6. 10.1017/cem.2020.354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persad, G. (2017). Public preferences about fairness and the ethics of allowing scarce medical interventions. In Tracer D., &Li M., (Eds.), Interdisciplinary perspectives on fairness, equity and justice, vol. 2020, pp. 1–6. Berlin, Germany: Springer. 10.1007/978-3-319-58993-0_4 [DOI] [Google Scholar]
- Persad, G. , Wertheimer, A. , & Emanuel, E. J. (2009). Principles for allocation of scarce medical interventions. The Lancet, 373(9661), 423–431. 10.1016/s0140-6736(09)60137-9 [DOI] [PubMed] [Google Scholar]
- Rosenbaum, L. (2020). Facing Covid‐19 in Italy—Ethics, logistics, and therapeutics on the epidemic's front line. New England Journal of Medicine, 382, 1873–1875. 10.1056/NEJMp2005492 [DOI] [PubMed] [Google Scholar]
- Scheunemann, L. , & Lewis, D. (2011). The ethics and reality of rationing in medicine. Chest, 140, 1625–1632. 10.1378/chest.11-0622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvaraj, D. , McClelland, A. , & Furnham, A. (2019). Allocating scarce medical resources: Using social usefulness as a criterion. Ethics and Behaviour, 29, 274–281. 10.1080/10508422.2017.1404909 [DOI] [Google Scholar]
- Solnica, A. , Barski, L. , & Jotkowitz, A. (2020). Allocation of scarce resources during the COVID‐19 pandemic: a Jewish ethical perspective. Journal of Medical Ethics, medethics–2020. 10.1136/medethics-2020-106242 [DOI] [PubMed] [Google Scholar]
- Townsend, R. , & Eburn, M. (2020). COVID‐19–Legal and ethical implications for your practice. Australasian Journal of Paramedicine, 17(1), 1–3 10.33151/ajp.17.796 [DOI] [Google Scholar]
- WHO (2014). Making fair choices on the path to universal health coverage. Final report of the WHO Consultative Group on Equity and Universal Health Coverage. Geneva, Switzerland: Author. [Google Scholar]
- Wu, Z. , & McGoogan, J. M. (2020). Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA, 323, 1239. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
An SPSS file of the data is available on request from the first author.


