Editor,
A 59‐year‐old man was admitted to hospital for a severe respiratory failure and then intubated due to worsening of his respiratory condition. During his hospital stay, he received multiple empirical broad‐spectrum antibiotics (cefepime, piperacillin/tazobactam, linezolid, gentamicin and meropenem plus amikacin). The patient had no known history of drug allergies. A test to detect SARS‐CoV‐2 by real‐time reverse transcription polymerase chain reaction (RT‐PCR) assay of a throat swab was positive. Blood cell count showed severe eosinophilia (from 1.3 to 4.60 × 10) that decreased abruptly to 0.47 × 10 after introduction of methylprednisolone 1 mg/kg/day. On day 35 postadmission, while on therapy only with corticosteroids, he developed a symmetrically distributed maculopapular purpuric exanthema on the face, trunk and extremities (Fig. 1a,b). Mucous membranes were spared. No lymphadenopathies were present. Laboratory data including liver function, cryoglobulins, antinuclear antibody, and anti‐neutrophil cytoplasmic antibody test results were all normal. A skin biopsy found a superficial and deep perivascular neutrophilic infiltrate (Fig. 2a) with sparse leucocytoclasis, red blood cell extravasation and fibrinoid necrosis of vessel walls (Fig. 2b). The patient’s conditions worsened for neurological complications in the form of confusional state and absences.
Figure 1.

The patient developed a symmetrically distributed maculopapular purpuric exanthema on the trunk (a) and extremities (b).
Figure 2.
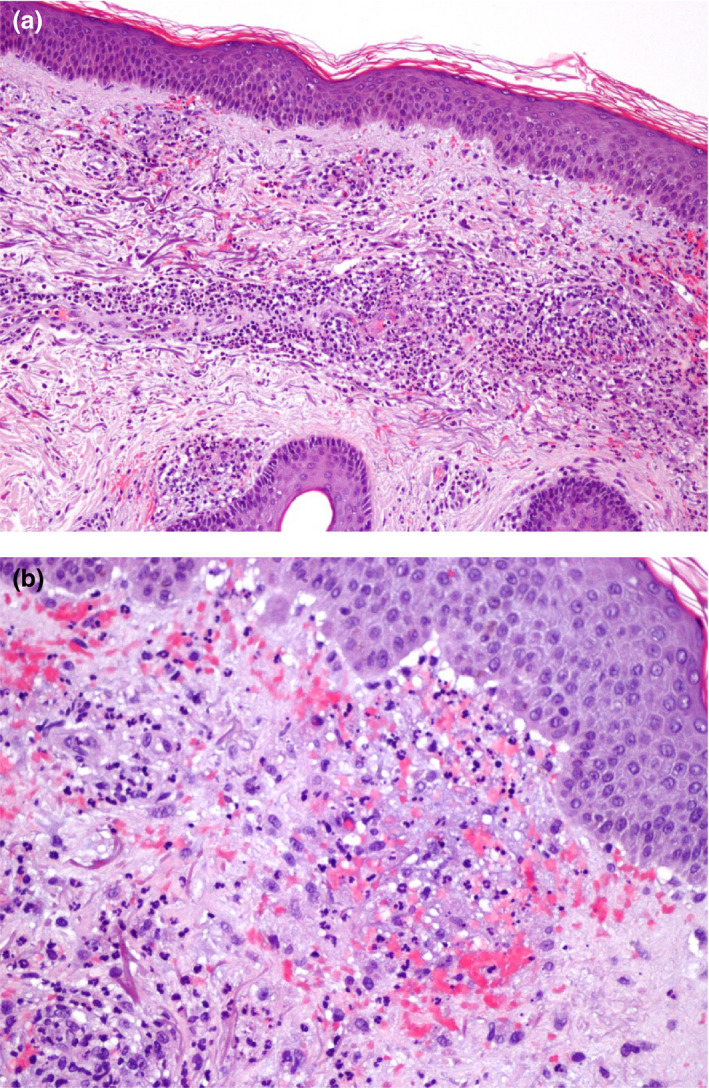
Skin biopsy revealed a dermal perivascular neutrophilic infiltrate (a; Haematoxylin–Eosin, 10×) with sparse leucocytoclasis, red blood cell extravasation and fibrinoid necrosis (b; Haematoxylin–Eosin, 40×).
Drug reaction with eosinophilia and systemic symptoms syndrome (DRESS) was considered in our patient for skin eruption and blood eosinophilia that integrate two criteria for the diagnosis 1 ; however, histopathology showing a classical picture of leucocytoclastic vasculitis was not consistent with DRESS. In fact, different histopathologic patterns were described in DRESS including spongiotic, erythema multiforme‐like, or lichenoid but no vasculitis. 2 Despite an antibiotic allergy was considered, it is known that severe COVID‐19 induces endothelial damage and vasculopathic changes. 3 Although some reports have showed purpuric eruptions as skin manifestations in patients with COVID‐19, 4 histopathology was rarely performed and, in any case, leucocytoclastic vasculitis has never been described. A petechial skin eruption resembling dengue fever was described in a COVID‐19 patient in Thailand. 5 A morbilliform rash with purpuric features was observed in a 32‐year‐old woman occurring 6 days after the development of COVID‐19. 6 Another young patient with severe lung disease showed at first a vasculitic purpura of legs followed by a fleeting erythematous rash. 7 In all these cases, the diagnosis was only made on clinical grounds as skin biopsy was not performed. A symmetric periflexural eruption with confluent erythematous macules, papules and petechiae sparing the inguinal folds, face, palms, soles and mucosa was reported in a 48‐year‐old man in whom histopathology showed a superficial, perivascular lymphocytic infiltrate with haemorrhages and papillary oedema without sign of vasculitis or thrombotic vasculopathy. 8 On the contrary, a pauci‐inflammatory thrombogenic vasculopathy with complement deposition of C5b‐9 and C4d in involved purpuric skin and normal skin was described in three patients with lung disease due to COVID‐19 pneumonia. 3 Finally, a purpuric, non‐blanching, pruritic and painful rash involving the trunk and extremities was observed in a 57‐year‐old woman. The authors reported that a biopsy specimen showed a vasculitis but no further details were added. 9 Our patient was the first in whom a generalized purpuric eruption showed typical microscopic features of leucocytoclastic vasculitis in the setting of COVID‐19. He also had severe lung disease and developed neurological complications. Although we cannot prove it, a central nervous system vasculitis due to invasion of SARS‐CoV‐2, similar to SARS and MERS viruses, could be hypothesized. 10 In conclusion, this case report illustrates the potential of COVID‐19 infections to trigger severe drug‐related cutaneous leucocytoclastic vasculitis and possibly systemic vasculitis.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgement
The patient in this manuscript has given written informed consent to the publication of his case details.
References
- 1. Grandolfo M, Romita P, Bonamonte D, et al. Drug reaction with eosinophilia and systemic symptoms syndrome to hydroxychloroquine, an old drug in the spotlight in the COVID‐19 Era [published online ahead of print, 2020 May 2]. Dermatol Ther 2020; 10.1111/dth.13499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gonçalo MM, Cardoso JC, Gouveia MP et al. Histopathology of the Exanthema in DRESS Is Not Specific but May Indicate Severity of Systemic Involvement. Am J Dermatopathol 2016; 38: 423–433. 10.1097/DAD.0000000000000439. [DOI] [PubMed] [Google Scholar]
- 3. Magro C, Mulvey JJ, Berlin D et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID‐19 infection: A report of five cases. Transl Res 2020; 5244: 1–13. https://doi.org/10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wollina U, Karadağ AS, Rowland‐Payne C, Chiriac A, Lotti T. Cutaneous signs in COVID‐19 patients: A review [published online ahead of print, 2020 May 10]. Dermatol Ther 2020; 10.1111/dth.13549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Joob B, Wiwanitkit V. COVID‐19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol 2020; 82: e177. 10.1016/jaad.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moreno R, Villa E, Avellana Moreno V, Estela Villa C, Aparicio M, Fontanella A. Cutaneous manifestation of COVID‐19 in Images: A Case Report. J Eur Acad Dermatol Venereol 2020; 10.1111/jdv.16531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Diaz‐Guimaraens B, Dominguez‐Santas M, Suarez‐Valle A, et al. Petechial skin rash associated with severe acute respiratory syndrome coronavirus 2 infection [published online ahead of print, 2020 Apr 30]. JAMA Dermatol 2020; 10.1001/jamadermatol.2020.1741. [DOI] [PubMed] [Google Scholar]
- 8. Ramirez AV, Efe D, Fischer M. Drug‐induced vasculitis in a patient with COVID‐19 [published online ahead of print, 2020 May 7]. J Eur Acad Dermatol Venereol 2020; 10.1111/jdv.16588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Castelnovo L, Capelli F, Tamburello A, Maria Faggioli PM, Mazzone A. Symmetric cutaneous vasculitis in COVID‐19 pneumonia [published online ahead of print, 2020 May 7]. J Eur Acad Dermatol Venereol 2020; 10.1111/jdv.16589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Carod‐Artal FJ. Neurological complications of coronavirus and COVID‐19. Complicaciones neurológicas por coronavirus y COVID‐19. Rev Neurol 2020; 70: 311–322. 10.33588/rn.7009.2020179. [DOI] [PubMed] [Google Scholar]


