Abstract
In March 2020, we treated a cohort of 26 critically ill hospitalized SARS‐CoV‐2–infected patients who underwent electroencephalography to assess unexplained altered mental status, loss of consciousness, or poor arousal and responsiveness. Of the 26 patients studied, 5 patients had electroencephalograms that showed periodic discharges consisting of high‐amplitude frontal monomorphic delta waves with absence of epileptic activity. These findings may suggest central nervous system injury potentially related to COVID‐19 in these patients. ANN NEUROL 2020;88:626–630
The new coronavirus, SARS‐CoV‐2 (ie, COVID‐19), is the latest of the coronavirus diseases found to afflict humans with severe respiratory infection, respiratory distress, and possibly death. However, as we gain more knowledge about this particular virus, we recognize potentially devastating involvement of other organs such as the heart and the brain. 1 , 2 Although genetically related to the other forms of coronavirus, particularly the previous SARS coronavirus (SARS‐CoV‐1) that resulted in severe acute respiratory distress, COVID‐19 has proven to be far more contagious than the other coronaviruses. 3 , 4 Other coronaviruses have been reported to be neurotropic. 5 , 6 , 7 For example, like SARS‐CoV‐1 virus, the SARS‐CoV‐2 virus has an affinity to the angiotensin‐converting enzyme 2 (ACE2) receptors that allow entry of the virus into the cells coated with such receptors. 8 ACE2 receptors are naturally found in the heart, lungs, kidneys, and central nervous system (CNS) in particular. 8 It has been suggested that the SARS‐CoV‐2 virus may enter the brain through the olfactory epithelium deep in the nasal passages and other tissues possessing the ACE2 receptors. 8 , 9 However, only a single case of presumed SARS‐CoV‐2 encephalitis has been reported in which the analysis of the cerebrospinal fluid (CSF) revealed the presence of SARS‐CoV‐2 RNA sequences. The brain computed tomography (CT) scan in that case was normal, and no electroencephalography (EEG) was performed. The patient was discharged from the intensive care unit (ICU) without evidence of any neurological sequalae. 10
COVID‐19 may be strongly associated with various neurological symptoms including hyposmia/anosmia (30–33% of patients 11 , 12 ), dysgeusia, headache, and myalgia. Unexplained altered mental status or consciousness disturbances are observed in 13% of the patients. 8 Despite the high frequency of encephalopathy associated with SARS‐CoV‐2, no EEG abnormalities were recorded in early reports. 13 We therefore wish to place our observations on record of an unusual number of cases of SARS‐CoV‐2 encephalopathy with focal EEG findings suggesting brain injury.
Patients and Methods
Between March 18 and 31, 2020, EEGs were performed on 26 severe COVID‐19–infected patients hospitalized in several ICU departments in the Paris area. The patients were diagnosed as being COVID‐19–positive by semiquantitative reverse‐transcriptase polymerase chain reaction (PCR) analysis from nasopharyngeal swab specimens obtained in the emergency department or at the time of hospitalization. The EEGs were requested to assess the etiology of mental status changes or poor responsiveness of the patients, or to determine the presence of status epilepticus in nonarousable patients.
The clinical data and EEGs presented were based upon retrospective chart review and descriptive assessment of the patients during their hospitalization. The patient data collected for this report were performed as a “health data study” referred by the code MR‐004 (National Commission on Information Technology and Freedoms), which is a French national centralized authority (institutional review board equivalent) for this type of study report. The authors also confirm that informed consent for all medical examinations and use of the anonymized data has been obtained by the patients' health care providers from either the patient or, in the majority of the cases, from a family member.
The EEGs were performed over a 30‐minute period in accordance with the International 10–20 system using a 9‐electrode placement configuration. The 9 electrodes consisted of Cz, FP2, C4, O2, T4, FP1, C3, O1, and T3, with reference in FPz and ground in Oz. The EEG recording was obtained with intermittent light (photic) stimulation, with the EEG recording parameters consisting of low filter at 0.530HZ, high filter at 70HZ, recording speed at 30 seconds, and gain at 100μV. Due to the patients' COVID‐19 infection, disposable needle electrodes were used for the EEGs.
Results
Of the original cohort of 26 patients, 19 showed EEGs consisting of diffuse and nonspecific theta and alpha wave activity, with some including diffuse delta wave activity without focal or periodic features, and 2 had isoelectric EEGs consistent with brain death (see Supplementary Table S1). Five patients, however, had evidence of generalized periodic discharges. The 5 patients highlighted in this report consisted of 4 men (Patients 1, 2, 3, and 4) and 1 woman (Patient 5) with a mean age of 67 years, with ages ranging from 58 to 70 years (Table).
TABLE 1.
Clinical Profile of Patients with Evidence of EEG Periodic Discharges
| Patient | Age, yr | Gender | Medical History | Intervention | Days Intubated at Time of EEG | EEG Interpretation | Clinical Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 58 | M | Coma, face and eye myoclonus |
Ventilator, deep sedation (propofol, fentanyl), ECMO, lumbar puncture |
4 | Generalized bilateral frontal intermittent symmetric biphasic delta, theta activity | Died 8 days after EEG performed |
| 2 | 70 | M | Delayed awakening, cardiac arrest | Ventilator, not sedated | 8 | Generalized bilateral frontal high‐amplitude symmetric biphasic delta, theta activity | Died 3 days after EEG performed |
| 3 | 70 | M |
Poor arousal epilepsy? |
Ventilator, mild sedation (midazolam), CT scan | 6 | Lateralized right focal frontal high‐amplitude symmetric biphasic delta symmetric | Remains hospitalized in ICU |
| 4 | 70 | M | Coma, face myoclonus | Ventilator, deep sedation (propofol, fentanyl), renal dialysis | 12 | Generalized biphasic delta asymmetric frontal predominance | Died 9 days after EEG performed |
| 5 | 67 | F | Confusion, lethargy | MRI, lumbar puncture | N/A | Generalized frontal slowing, symmetric biphasic delta, theta activity | Remains hospitalized on ward, significant cognitive deficit |
CT = computed tomography; ECMO = extracorporeal membrane oxygenation; EEG = electroencephalographic; F = female; ICU = intensive care unit; M = male; MRI = magnetic resonance imaging; N/A = not applicable.
Four of the 5 patients were intubated and poorly responsive or unresponsive, and the EEGs were obtained from 4 days to 12 days after they were intubated (Patients 1, 2, 3, and 4). Two of the patients were deeply sedated with propofol and fentanyl (Patients 1 and 4) and 1 patient was mildly sedated with midazolam (Patient 3). The other 2 patients were not sedated (Patients 2 and 5). One of the patients (Patient 2) had anoxia associated with a cardiac arrest prior to intubation. The other 3 patients on ventilators were intubated because of unresponsiveness in combination with hypoxia (Patients 1, 3, and 4). The fifth patient (Patient 5) was not intubated and received the EEG study after presenting with sudden unexplained confusion, lethargy, and significant cognitive impairment. In addition, 3 of the patients (Patients 1, 3, and 4) demonstrated brief myoclonic seizure activity while sedated. Lumbar punctures were obtained in 2 of the patients (Patients 1 and 5) that were reported to be “normal” (opening pressure and protein quantification were not available) with no evidence of cells, or presence of coronavirus or herpes simplex virus on PCR. A brain CT scan was performed on 1 patient (Patient 3) reporting no specific abnormalities other than “a cyst in the occipital area,” and brain magnetic resonance imaging (MRI) was performed in another patient (Patient 5) that was reported to show diffuse white matter hyperintensity (both image results were by report, and the actual images were not available). One patient (Patient 1) was receiving extracorporeal membrane oxygenation for severe hypoxemia, and another patient (Patient 4) was receiving dialysis for acute renal failure. Three of the patients died in the ICU (Patients 1, 2, and 4), and 2 patients remained hospitalized as of April 20, 2020 (Patients 3 and 5).
EEG Interpretation
The EEG recordings (Fig) reveal a background rhythm that is clearly abnormal, showing generalized slowing and theta activity consistent with sedation. They also show bilateral diffuse frontocentral slow wave activity with high‐amplitude generalized periodic discharges with frontal involvement. The EEGs display monomorphic biphasic delta activity or generalized rhythmic delta activity (GRDA) with <4‐second intervals (see Fig A, B, D, and E, representing Patients 1, 2, 4, and 5 respectively) or lateralized periodic discharges (LPDs) of a 1‐ to 2‐second period with right frontal predominance (see Fig C, representing Patient 3).
FIGURE: 1.
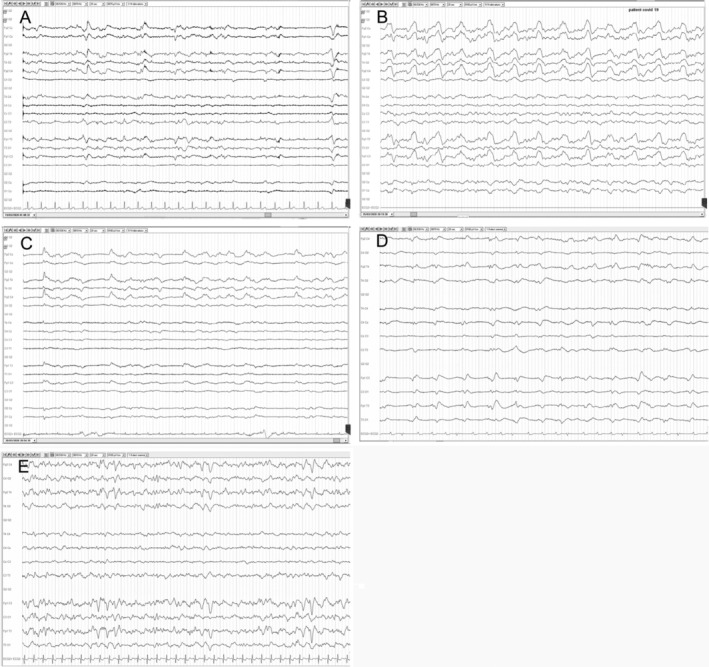
Electroencephalographic (EEG) recordings of Patients 1 through 5. The panels display EEG recordings of 20 seconds for each patient. In each panel, the EEG channels are shown with an electrocardiographic recording at the bottom. Nomenclature is in accordance with the International 10–20 montage. The EEGs reveal a pattern of slow waves with periodic discharges in the frontal regions. (A) Scalp EEG in a reference montage from Patient 1 reveals generalized rhythmic delta activity (GRDA) with intermittent biphasic delta waves in bilateral frontal regions that are symmetric and monomorphic with low‐voltage rhythmic background activity. (B) Scalp EEG in a reference montage from Patient 2 reveals GRDA with frequent high‐amplitude biphasic delta waves in bilateral frontal regions that are symmetric and polymorphic with low‐voltage rhythmic theta background activity. (C) Scalp EEG in a reference montage from Patient 3 reveals lateralized periodic discharges of high‐amplitude monomorphic delta activity with right frontal region predominance and low‐voltage rhythmic theta background activity. (D) Scalp EEG in a reference montage from Patient 4 reveals GRDA with intermittent low‐amplitude slow biphasic delta waves in bilateral frontal regions that are slightly asymmetric and monomorphic with low‐voltage continuous background activity. (E) Scalp EEG in a reference montage from Patient 5 reveals GRDA with intermittent high‐amplitude biphasic delta waves in bilateral frontal regions that are symmetric and monomorphic with intermittent low‐voltage rhythmic theta background activity.
The EEG abnormalities can be summarized as generalized or LPDs that primarily consist of symmetric slow monomorphic biphasic delta waves of high amplitude occurring in short repetition of <4 seconds. The periodic discharges are located primarily in the frontal region without evidence of paroxysmal epileptic activity.
Discussion
The significance of GRDA and LPD EEG findings in the presence of mental status abnormalities may be related to a host of etiologies. Clearly the background slowing and theta activity demonstrated in the EEGs could be related to sedation, somnolence, coma, anoxia or hypoxia, and other CNS‐depressive entities. However, the presence of the monomorphic biphasic high‐amplitude delta waves associated with occasional myoclonic muscular activity could also possibly be indicative of brain injury related to anoxia, severe hypoxia, anesthesia, or the direct effects of COVID‐19 itself. The reported onset of loss of consciousness or confusion and cognitive impairment in COVID‐19–infected patients with EEGs revealing biphasic delta periodic discharges may suggest an injury or localized brain defect attributable to encephalopathy related to a unique and acute CNS process. Although potentially complicated by the severity of multiorgan disfunction, the focal encephalopathy may be due to possible vascular, infectious, or parainfectious inflammatory processes in the brain. 14 However, the lack of pleiomorphism in the CSF and lack of evidence of viral infection of the brain by PCR would suggest that the discharges are not the result of direct brain infection or autoimmune encephalitis (although such EEG patterns, most prominent in Patients 1 and 5, have been seen in subacute sclerosing panencephalitis due to measles 15 , 16 ).
Another possible source of focal brain injury could be the vasculopathy and coagulopathy that is seen in many COVID‐19 patients. 17 Unfortunately, unless patients have evidence of focal brain injury on examination, many hospitals are not performing routine MRI on COVID‐19 patients, as this risks increased exposure and requires subsequent decontamination of the scanner. Therefore, although EEG assessment alone may not directly provide a diagnosis or confirm the etiology for the unexplained alteration of a patient's mental state or lack of responsiveness, the appearance of lateralized frontal or bilateral frontal periodic discharges with abnormal background may be an important clue that the patient has suffered from a brain injury. 18
When hospitalized patients infected with SARS‐CoV‐2 (COVID‐19) present with an unexplained loss of consciousness, confusion or altered mental status, impaired arousal, and abnormal paroxysmal movements (myoclonus), it is suggested that EEG be performed as part of the diagnostic assessment of the patient to determine an etiology and to identify potentially treatable CNS disorders. Such studies will also further enhance our knowledge to better understand the growing number of new and unusual neurologic illnesses possibly associated with COVID‐19.
Author Contributions
H.V. contributed to the conception and design of the study. H.V., D.C., B.S.L., C.S., V.P., L.M., O.P., and S.M. contributed to the acquisition and analysis of the data. H.V., D.C., B.L., and P.‐Y.F. contributed to drafting the text and preparing the figure.
Potential Conflicts of Interest
H.V., B.S.L., D.C., S.M., and P.‐Y.F. are employees of BioSerenity, the company that performed the EEG recordings and collected the EEG recording data at the Paris hospital units. There are no other conflicts of interest to report.
Supporting information
Supplementary Table S1: Clinical Profile of Patients with No Evidence of EEG Periodic Discharges
Acknowledgments
We thank the technicians and staff at the Paris hospitals who collected and conducted the EEG examinations.
References
- 1. Steardo L, Steardo L Jr, Zorec R, Verkhratsky A. Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID‐19. Acta Physiol (Oxf) 2020;229:e13473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID‐19). JAMA Cardiol (in press). 2020; 10.1001/jamacardio.2020.1096. Accessed April 5, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fauci AS, Lane HC, Redfield RR. Covid‐19—navigating the uncharted. N Engl J Med 2020;382:1268–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Andersen KG, Rambaut A, Lipkin WI, et al. The proximal origin of SARS‐CoV‐2. Nat Med 2020;26:450–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Talbot P, Jouvenne P. Neurotropic potential of coronaviruses. Medecine/Sciences 1992;8:119. [Google Scholar]
- 6. Desforges M, Le Coupanec A, Dubeau P, et al. Human coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? Viruses 2020;12:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arbour N, Day R, Newcombe J, Talbot PJ. Neuroinvasion by human respiratory coronaviruses. J Virol 2000;74:8913–8921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID‐19 virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci 2020;11:995–998. [DOI] [PubMed] [Google Scholar]
- 9. Netland J, Meyerholz DK, Moore S, et al. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol 2008;82:7264–7275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ye M, Ren Y, Lv T. Encephalitis as a clinical manifestation of COVID‐19. Brain Behav Immun (in press). 10.1016/j.bbi.2020.04.017. Accessed April 14, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hopkins C, Surda P, Kumar N. Presentation of new onset anosmia during the COVID‐19 pandemic. Rhinology 2020;10:1–4. 10.4193/Rhin20.116. [DOI] [PubMed] [Google Scholar]
- 12. Giacomelli A, Pezzati L, Conti F, et al. Self‐reported olfactory and taste disorders in patients with severe acute respiratory coronavirus 2 infection: a cross‐sectional study. Clin Infect Dis (in press). 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mao L, Wang M, Chen S, et al. Neurological manifestations of hospitalized patients with COVID‐19 in Wuhan, China: a retrospective case series study. JAMA Neurol 2020;77(6):683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Reichard RR, Kashani KB, Boire NA, et al. Neuropathology of COVID‐19: a spectrum of vascular and acute disseminated encephalomyelitis (ADEM)‐like pathology. Acta Neuropathol 2020;140(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Markand ON, Panszi JG. The electroencephalogram in subacute sclerosing panencephalitis. Arch Neurol 1975;32:719–726. [DOI] [PubMed] [Google Scholar]
- 16. Honarmand S, Glaser CA, Chow E, et al. Subacute sclerosing panencephalitis in the differential diagnosis of encephalitis. Neurology 2004;63:1489–1493. [DOI] [PubMed] [Google Scholar]
- 17. Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID‐19 infection: a report of five cases. Transl Res 2020;220:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Smith SJ. EEG in neurological conditions other than epilepsy: when does it help, what does it add? J Neurol Neurosurg Psychiatry 2005;76:ii8–ii12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Clinical Profile of Patients with No Evidence of EEG Periodic Discharges


