Abstract
To combat the ongoing COVID‐19 pandemic, Singapore has adopted a rigorous screening approach that involves aggressive contact tracing, rapid isolation of confirmed or suspect cases, and immediate ring‐fencing of emerging local clusters and hotspots. Our screening centre team has been involved in running Singapore's designated screening centre since the end of January this year. With a well‐defined blueprint and substantial pre‐outbreak preparatory work, initial operations at our screening centre commenced within a day on activation and full operational status was attained in 3 days. As of 8 April 2020, the screening centre had screened more than 14,000 patients. We have adopted a “whole‐of‐hospital” approach, enlisting the help from other departments and subspecialties to augment manpower. Meticulous infrastructure planning to facilitate patient flow and strict measures to prevent nosocomial transmission and occupational exposure were instituted to safeguard both the staff and patients. This paper aims to describe our key takeaways in the course of operations and discuss the challenges encountered.
1. INTRODUCTION
Strategies to combat the ongoing COVID‐19 pandemic vary greatly. A proposal briefly floated in the United Kingdom involved an early transition from containment to mitigation. 1 Serious concerns have been expressed regarding this approach, citing the potential catastrophic loss of lives. Many countries such as China have imposed drastic measures such as strict travel bans and the complete lockdown of entire cities. 2 , 3 These strategies are not sustainable in the long term due to its highly deleterious impact on the economy and livelihoods. 4 , 5 This calls for a complementary solution as countries seek to lift their lockdown measures.
Singapore has received significant attention with regard to its crisis management approach to the ongoing COVID‐19 outbreak and is regarded as the “gold standard” by international researchers in a recent study. 6 Singapore diagnosed its first case, a tourist from Wuhan, China, on January 23, 2020. 7 On January 28, 2020, the Ministry of Health decided to activate the National Centre for Infectious Diseases Screening Centre. On January 31, 2020, the country's designated screening centre was fully operational.
The screening centre is housed in National Centre for Infectious Diseases, adjacent to its partnering hospital, Tan Tock Seng Hospital. As the national screening centre, it receives patients referred from primary health care clinics nationwide, walk‐ins, immigration checkpoints, home quarantine, and Government Quarantine Facilities. The screening centre is operational round the clock and is run by the Tan Tock Seng Hospital Emergency Department (ED), in collaboration with National Centre for Infectious Diseases's Infectious Diseases Department. As of 8 April 2020, the screening centre had screened more than 14,000 patients, with daily attendances ranging from 50–500 patients.
This paper aims to describe our experiences in running the screening centre including the pre‐outbreak preparatory phase, infrastructure planning to facilitate patient flow, and coordinating a “whole‐of‐hospital” approach to support our wide‐net surveillance efforts. We will discuss the challenges encountered in the course of operations and solutions used.
2. LESSONS FROM SARS
The Severe Acute Respiratory Syndrome coronavirus (SARS‐CoV) outbreak in 2003 had previously been considered as the biggest health care crisis in Singapore. A total of 238 probable SARS cases were identified, with 33 reported deaths (14% case fatality rate). A total of 97 (41%) health care workers were also infected over the course of the outbreak. 8 The valuable insights gained from tackling the SARS crisis have been factored heavily into our evolved response for future emerging infectious diseases. This includes the importance of a wide‐net surveillance strategy, early identification and isolation of confirmed cases, preventing nosocomial transmission, and occupational exposure as summarized in a previous review. 9 However, the screening centre team is cognizant that although it is important to incorporate these lessons, it is just as important to pay attention to the unique differences of COVID‐19, particularly its increased transmissibility, 10 , 11 albeit decreased fatality rates.
3. PURPOSE‐BUILT INFRASTRUCTURE TO FACILITATE PATIENT FLOW
One of the key lessons from combating the SARS and the 2009 H1N1 outbreaks is recognizing the need for a facility dedicated to the containment of infectious disease outbreaks. The National Centre for Infectious Diseases was built and conceptualized for this purpose. It is a 330‐bed facility with 5 negative pressure wards and 2 intensive care wards. 12 The National Centre for Infectious Diseases also houses a large screening centre that is used for small, medium, and large scale outbreaks and the National Public Health Laboratory equipped with a biosafety‐level 3 containment facility.
The screening centre has a capacity for 22 trolley beds and 99 ambulatory patients when chairs are spaced 2 metres apart. Seating capacity can be increased to 181 when chairs are spaced 1.5 metres apart instead. This is in line with local and international guidelines on droplet precautions. 13 , 14 , 15 It is further divided into 2 areas: a High Risk wing and a Low Risk wing (Figure 1).
FIGURE 1.
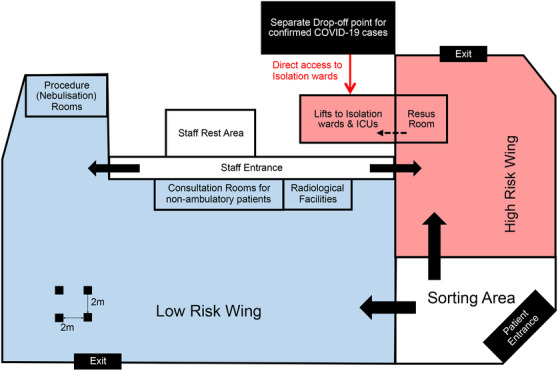
Schematic representation of the floor layout of the National Centre for Infectious Diseases Screening Centre (not to scale)
The screening centre is located in the Central Region of Singapore, 16 providing easy access to members of the public for screening. Within each area, there are negative‐pressure isolation rooms, procedure rooms, radiology facilities, and pharmacies. Individual consultation rooms are available for non‐ambulatory patients. The screening centre also houses a resuscitation room in each wing with full resuscitation capabilities and staffed round the clock by specialist emergency physicians. Each of the resuscitation rooms is directly connected via a lift to the intensive care units in the facility. The air regime in both wings is supplied by high‐efficiency particulate air 17 (HEPA) filtered air handling units. The staff rest area uses a positive‐pressure air regime whereas the resuscitation room and procedure rooms in the High Risk and Low Risk wings, respectively, use a negative‐pressure air regime, because some of our patients may require procedures at risk of aerosolization such as nebulization. These quality assurance measures are crucial for staff and patient safety and promote both staff and public confidence.
The infrastructure is meticulously designed to facilitate patient flow as shown in Figure 2.
FIGURE 2.
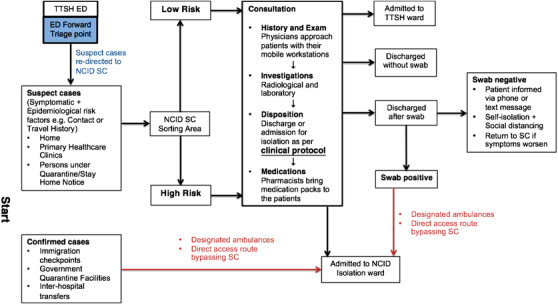
Schematic diagram illustrating patient flow within the National Centre for Infectious Diseases Screening Centre (SC)
The majority of the patients are self‐referred or are referred from primary health care clinics. The screening centre also receives confirmed cases of COVID‐19 referred from immigration checkpoints, government quarantine facilities, or other hospitals. Direct access routes are set up to receive these patients and they are transferred directly to their isolation rooms in the National Centre for Infectious Diseases, bypassing the screening centre. A forward triage point is also set up at Tan Tock Seng Hospital ED to divert suspect cases to the National Centre for Infectious Diseases screening centre to segregate high risk cases away from Tan Tock Seng Hospital.
On arrival at the screening centre, ambulatory patients are given a surgical mask at the entrance. At the sorting area, patients are promptly directed to the High or Low risk wing based on a rapid assessment of their different epidemiological risk factors as stipulated on the sorting form. Each patient is assigned a seat number that is recorded for contact tracing purposes. Contact tracing is also facilitated by a real‐time location system 18 patient tracker tagged to each patient and closed‐circuit television monitoring. Patients are instructed to remain seated and any patient movement within the screening centre is under strict staff supervision. Non‐ambulatory patients conveyed by ambulances are placed in trolleys and are directly sited in consultation rooms after the initial sorting. These consultation rooms are also used for physical examinations as necessary, ensuring that patients’ privacy is respected. Unstable patients are attended to immediately in the resuscitation room.
All staff entering the screening centre are required to wear full personal protective equipment (PPE). This consists of a hair cap, goggles, N95 mask, disposable gowns with knitted cuffs, and gloves. 19 They are also tagged with real‐time location system to facilitate contact tracing. Physicians will approach patients in their seats with their mobile workstations for consultation. Radiological and laboratory investigations are performed in in‐house facilities. Risk stratification and final disposition of patients are based on the clinical protocol. This protocol is regularly updated in collaboration with the Infectious Diseases Department, based on the latest updates from Tan Tock Seng Hospital Department of Clinical Epidemiology (DCE) and circulars published by the Ministry of Health. We have adopted a wide‐net surveillance approach that will be further elaborated on later. At the end of the consultation, pharmacists will bring medication packs to the patients who are to be discharged. These steps are undertaken to ensure that patients remain in their seats as much as possible. Movement is kept to a minimum throughout the course of the consultation to reduce interaction among patients at usual chokepoints such as queues at the pharmacy, toilets, and radiology facilities. The flow is also designed so that the patients go through a single entry and exit point to minimize criss‐crossing of patient flows.
The majority of patients are discharged after a swab test for COVID‐19 has been performed and are advised to observe proper hand hygiene, masking up, self‐isolation, and social distancing. Backend tracing ensures that patients are subsequently informed of the results of the swab tests. Positive cases will be conveyed back immediately to the National Centre for Infectious Diseases via designated ambulances (Figure 2) and admitted via the direct access routes.
4. WIDE‐NET SURVEILLANCE APPROACH AND CLOSE MONITORING OF LOCAL HOTSPOTS
The key direction for the screening centre is to limit community transmission of COVID‐19. This is particularly important due to the increased transmissibility of the virus, relative to the other coronaviruses, SARS‐CoV and Middle‐East Respiratory Syndrome (MERS‐CoV). Core to this strategy is the wide‐net surveillance approach adopted. This approach involves extensive epidemiological mapping from new positive cases to identify close contacts, new clusters, and hotspots.
Hotspots are stratified into high and low risk depending on the number of positive cases and the probable degree of spread. The duration of monitoring is from the time of the first positive case detected up to 2 incubation periods (28 days). Symptomatic patients from high risk hotspots are sorted to the High Risk wing in the screening centre. The hotspot list is updated on a daily basis.
Close contacts, as identified by contact tracing teams from Ministry of Health working round the clock, are swiftly notified and instructed to practice self‐isolation and social distancing; a proportion may be quarantined according to the risk assessment. They are also reminded to return to the screening centre promptly for evaluation and testing should they develop symptoms. As the country's designated screening centre, the National Centre for Infectious Diseases screening centre had screened more than 14,000 patients as of 8 April 2020, which is ∼70% of the country's screening workload.
Rapid isolation of confirmed cases and close contacts limit community transmission, as part of efforts to “flatten” the epidemic curve and avoid an epidemic peak that overwhelms health care services. 20 We are of the belief that the wide‐net surveillance approach has contributed to a ratio of 1.8 undetected cases for every detected COVID‐19 patient, 1 one of the lowest in the world.
5. PRE‐OUTBREAK PREPARATORY PHASE AND TIMELINE
The Tan Tock Seng Hospital ED, one of the busiest EDs in Singapore, screens, manages, and treats emerging infectious diseases suspect cases on a daily basis based on information provided by the Tan Tock Seng Hospital DCE that performs horizon scanning and surveillance of local clusters and global infectious disease threats on a daily basis.
On December 31, 2019, China informed the World Health Organization of a novel viral pneumonia in the city of Wuhan, China. Screening for travelers from China within the last 14 days for suspect COVID‐19 cases started on January 2, 2020. As the number of patients increased, the ED overflow protocols were implemented.
At its peak, ∼60 patients were screened at the ED per day in addition to the usual ED attendances. The decision was then made by Ministry of Health to activate the National Centre for Infectious Diseases Screening Centre on January 28, 2020 (D) once patient numbers met the threshold capacity. The screening centre commenced its operations on January 29, 2020 (D+1) and was fully operational by January 31, 2020 (D+3).
The screening centre was able to attain full operational status within a short span of 3 days due to the pre‐outbreak preparatory work and planning as laid out in Figure 3.
FIGURE 3.
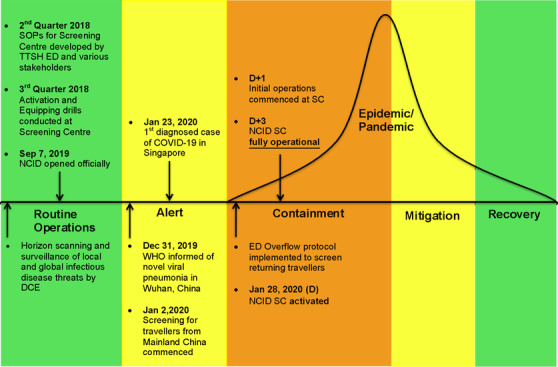
Disease response phases in Tan Tock Seng Hospital, Singapore
As early as the second quarter of 2018, the Tan Tock Seng Hospital ED, in collaboration with the various stakeholders, developed standard operating procedures in the following domains, including medical, nursing, operations, logistics, pharmacy, radiology, security, housekeeping, food and beverage, transport, and mortuary. As stipulated in the standard operating procedures, a 3‐day equipping and activation period (D+3) is allotted for the setting up of equipment and logistics, enhancing existing clinical protocols and work instructions, manpower mobilization, and staff training specific to the unique features of the COVID‐19 outbreak. Training sessions were conducted to familiarize ED staff from medical, nursing, and operations on the workflows and the layout of the screening centre. Activation and equipping drills were conducted in the third quarter of 2018 to assess our operational readiness, evaluate workflows, and refine work processes.
6. WHOLE‐OF‐HOSPITAL APPROACH
To sustain round the clock operations, we adopted a “whole‐of‐hospital” approach and recruited the assistance of doctors from the other departments including General Surgery, Orthopedic Surgery, Hand Surgery, Neurosurgery, Radiology, Pathology, Ophthalmology, Otorhinolaryngology, and Urology who took up roles as medical officers in the screening centre. Nursing and administrative staff were also recruited from the different departments and clinics. Non‐emergency surgeries and outpatient consultations were postponed to support manpower augmentation. The ED, in consultation with the Infectious Diseases Department, remained the nexus, providing timely updates on the clinical protocol in response to new clinical and epidemiological information and workflow adjustments. Senior emergency physicians also provided operational and clinical oversight, as our colleagues from the other departments may not be as familiar with managing the various conditions encountered in the ambulatory setting. A standby roster was created to cover for manpower shortages during surge and staff illness. All conferences, non‐urgent courses, and leave were restricted.
Part of our efforts to systematically strengthen our capacity to manage an emerging infectious diseases outbreak is to ensure that all hospital staff are trained in the correct use of PPE. All staff working at the screening centre (including security, IT support, housekeeping, and facilities) were required to undergo respirator mask fit testing. As part of our preparation, we conducted a series of just‐in‐time (JIT) training sessions for all the screening centre staff. These JIT training sessions include PPE refresher sessions, a physical walkthrough of the facility, and familiarization with clinical protocols and work instructions. Augmented medical personnel are assigned a 10‐day rotation in the screening centre.
7. CHALLENGES
Over the course of operations, the screening team encountered several challenges, mainly in the area of communications, surges in patient attendance, and staff morale. These challenges and the respective solutions used will be further elaborated on in the subsequent paragraphs.
7.1. Communications—the crucial link
The main challenges encountered in the domain of communications are 2‐fold: the rapid influx of information due to the constantly evolving situation, and the necessity to minimize person‐to‐person contact as part of social distancing measures.
Right from the onset, communication protocols and reporting channels were established between the main groups of stakeholders—ground staff including senior and junior physicians, augmented medical staff, nursing and operations personnel, and the various leadership groups including the respective leadership teams from National Centre for Infectious Diseases, Tan Tock Seng Hospital and Ministry of Health. This is to ensure a smooth flow of information between the policymakers, hospital senior management, department leaders, and senior and junior physicians.
Essential meetings, such as end‐of‐day debrief sessions at the senior management level, are allowed to proceed with proper precautions observed, including the use of surgical masks and social distancing measures. Conversely, all non‐essential meetings have been put on hold. In its place, different‐tiered encrypted communication platforms were created to disseminate information to the different stakeholders depending on the sensitivity of information. Immediate dissemination of information of positive cases to the frontline and contact tracing staff is key to faster activity mapping of patients and timely identification of possible close contacts and developing new clusters and hotspots in the community. As the wide‐net surveillance approach necessitates frequent updates to the clinical protocol, staff briefings at the start of every shift were conducted to communicate the latest changes.
Communication at the inter‐agency level is essential to facilitate rapid dissemination of information such as close contact lists and persons under quarantine (PUQ) lists. This also includes operational details such as arranging designated ambulances to admit confirmed cases to isolation wards in the National Centre for Infectious Diseases swiftly.
7.2. Surges in patient attendance
Sudden increases in patient attendance (Figure 4) posed a challenge to manpower allocation and planning. These spikes tended to coincide with external events such as revisions of case suspect definition by the Ministry of Health; when the Singapore government raised our Disease Outbreak Response System Condition (DORSCON) 21 level to orange; when a new (large) cluster was identified in the local community, or the week after a travel advisory was issued for overseas Singaporeans to return. 22 Pre‐planned contingency procedures were promptly enacted and manpower was augmented from our standby roster, which was made possible due to the “whole‐of‐hospital” approach that we adopted. Seating arrangements were revised (chairs spaced 1.5 meters apart instead of 2 meters) to increase seating capacity from 99 to 181.
FIGURE 4.
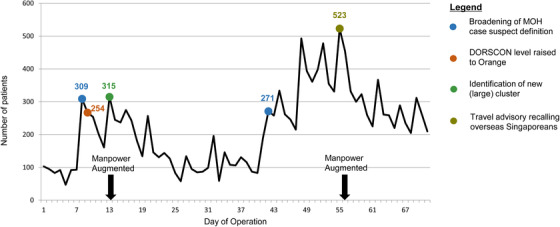
Daily attendances at the National Centre for Infectious Diseases Screening Centre (Information updated as of 8 April 2020)
7.3. Staff wellbeing
The leadership team is well aware of the potential psychological and physical stresses experienced by the screening centre staff during the outbreak. 23 , 24 Multiple measures have been put in place to promote staff wellbeing. This includes regular breaks during shifts, availability of rest areas adhering to social distancing measures, and provision of food, snacks, and beverages round the clock. A clear system was put in place for staff who report in sick with special arrangements made to expedite staff consultation and follow‐up. Accommodation allowances were made available during this period to the screening centre staff who may prefer to isolate themselves from their family members such as those who are elderly with underlying comorbidities. Led by the Department of Psychiatry, teams of staff support staff were formed to cater to the psychological and emotional wellbeing of our staff, and a special helpline was set up.
8. CONCLUSION
In the past decade alone, the international community has experienced 2 major pandemics: the 2009 H1N1 pandemic and the current COVID‐19 pandemic. With a population density of 8,358/km2, as well as her status as a major transport hub for international travel, Singapore is inherently vulnerable to the threat of infectious diseases outbreaks, similar to many major cities such as New York City (10,194/km2), Paris (21,498/km2), and Manila (42,857/km2). 25
The importance of a swift and coordinated response to curb rapid transmission cannot be overstated. In our experience, the aforementioned strategies as summarized in Table 1 have been indispensable to our outbreak response. These include a pre‐outbreak response plan with detailed standard operating procedures, a purpose‐built infrastructure, meticulously designed layout and patient flow, a wide‐net surveillance strategy, and a “whole‐of‐hospital” approach to manpower augmentation. Early data from a recent local study 26 have demonstrated the efficacy of these containment strategies whereby the 7‐day moving average of the interval from symptom onset to isolation declined significantly for both imported and local cases, from 9.0 and 18.0 days to 0.9 and 3.1 days. We hope these strategies and planning blueprints can be adapted for use by other countries in their outbreak response, especially densely populated cities that share similar demographic features as Singapore.
TABLE 1.
Summary of strategies adopted in the National Centre for Infectious Diseases Screening Centre
| Pre outbreak preparation |
|
| Layout and patient flow |
|
| Wide‐net surveillance |
|
| Manpower |
|
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Manauis CM, Loh M, Kwan J, et al. Bracing for impact: operational upshots from the National Centre for Infectious Diseases Screening Centre (Singapore) during the COVID‐19 outbreak. JACEP Open. 2020;1:549–556. 10.1002/emp2.12134
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Mike Wells, MBBCh, PhD.
REFERENCES
- 1. Hunter D. Covid‐19 and the stiff upper lip — the Pandemic response in the United Kingdom. N Engl J Med. 2020;382(16). 10.1056/nejmp2005755 [DOI] [PubMed] [Google Scholar]
- 2. Leung K, Wu JT, Liu D, Leung GM. First‐wave COVID‐19 transmissibility and severity in China outside Hubei after control measures, and second‐wave scenario planning: a modelling impact assessment. Lancet North Am Ed. 2020;395(10233):1382‐1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hartley DM, Perencevich EN. Public health interventions for COVID‐19. JAMA. 2020. 10.1001/jama.2020.5910 [DOI] [PubMed] [Google Scholar]
- 4. The economic impact of COVID‐19 on Asia‐Pacific. Oxford Economics. https://www.oxfordeconomics.com/recent-releases/The-Economic-Impact-of-COVID-19-on-Asia-Pacific. Accessed May 12, 2020.
- 5. Politicians in America and Europe scramble to help small firms. The Economist. https://www.economist.com/finance-and-economics/2020/05/02/politicians-in-america-and-europe-scramble-to-help-small-firms. Accessed May 12, 2020.
- 6. Niehus R, De Salazar P, Taylor A, Lipsitch M. Using observational data to quantify bias of traveller‐derived COVID‐19 prevalence estimates in Wuhan, China. Lancet Infect Dis. 2020. 10.1016/S1473-3099(20)30229-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. News Highlights. Ministry of Health. https://www.moh.gov.sg/news-highlights/details/confirmed-imported-case-of-novel-coronavirus-infection-in-singapore-multi-ministry-taskforce-ramps-up-precautionary-measures. Accessed May 12, 2020.
- 8. Goh K, Chew S. Epidemiology of emerging infectious diseases in Singapore, with special reference to SARS. Popul Dyn Infect Dis Asia. 2006:287‐303. 10.1142/9789812773395_0015 [DOI] [Google Scholar]
- 9. Chorh‐Chuan T. SARS in Singapore ‐ Key lessons from an epidemic. Ann Acad Med Singapore. 2006;35(5):345‐354. [PubMed] [Google Scholar]
- 10. Kucharski A, Russell T, Diamond C, et al. Early dynamics of transmission and control of COVID‐19: a mathematical modelling study. Lancet Infect Dis. 2020. 10.1016/s1473-3099(20)30144-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wilder‐Smith A, Chiew C, Lee V. Can we contain the COVID‐19 outbreak with the same measures as for SARS?. Lancet Infect Dis. 2020. 10.1016/s1473-3099(20)30129-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wong J, Leo Y, Tan C. COVID‐19 in Singapore—Current Experience. JAMA. 2020. 10.1001/jama.2020.2467 [DOI] [PubMed] [Google Scholar]
- 13. Who.int. https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf. Published 2020. Accessed March 12, 2020.
- 14. Public Health Preparedness Clinic (PHPC). Primarycarepages.sg. https://www.primarycarepages.sg/practice-management/moh-national-schemes/public-health-preparedness-clinic-(phpc). Published 2020. Accessed March 12, 2020.
- 15. Favero M. Prevention and control of nosocomial infections, 3rd ed, RP Wenzel; Baltimore MD: Lippincott Williams & Wilkins; 1997; 1,000 pages. Infect Control Hosp Epidemiol. 1999;20(12):834‐834. [Google Scholar]
- 16. Healthcity Novena. https://www.ttsh.com.sg/About-TTSH/healthcitynovena/Pages/default.aspx. Accessed May 12, 2020.
- 17. Environmental Guidelines . Centers for Disease Control and Prevention. https://www.cdc.gov/infectioncontrol/guidelines/environmental/index.html. Published July 23, 2019. Accessed April 4, 2020.
- 18. Hellmich T, Clements C, El‐Sherif N, et al. Contact tracing with a real‐time location system: a case study of increasing relative effectiveness in an emergency department. Am J Infect Control. 2017;45(12):1308‐1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Personal protective equipment. World Health Organization. https://www.who.int/medical_devices/meddev_ppe/en/. Published May 31, 2018. Accessed April 1, 2020.
- 20. Anderson R, Heesterbeek H, Klinkenberg D, Hollingsworth T. How will country‐based mitigation measures influence the course of the COVID‐19 epidemic? Lancet North Am Ed. 2020. 10.1016/s0140-6736(20)30567-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Disease Outbreak Response System Condition’ (DORSCON) is a colour‐coded framework adopted by the government of Singapore to reflect the current disease situation. The various levels, in ascending order of severity, are green, yellow, orange and red.
- 22. Press Releases. https://www.moe.gov.sg/news/press-releases/advisory-for-singaporean-students-studying-overseas. Accessed April 2, 2020.
- 23. Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID‐19 pandemic. Eur Heart J. 2020:204887262092279. 10.1177/2048872620922795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tan BYQ, Chew NWS, Lee GKH, et al. Psychological impact of the COVID‐19 pandemic on health care workers in Singapore [published online ahead of print, 2020 Apr 6]. Ann Intern Med. 2020;M20‐1083. 10.7326/M20-1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. List of world cities by population density. Wikipedia. https://en.wikipedia.org/wiki/List_of_world_cities_by_population_density. Published April 12, 2020. Accessed May 12, 2020.
- 26. Ng Y, Li Z, Chua YX, et al. Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID‐19 in Singapore — January 2–February 29, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(11):307‐311. [DOI] [PMC free article] [PubMed] [Google Scholar]


