On 23 March 2020 the United Kingdom went into lockdown to reduce transmission of COVID‐19. In order to focus on acute care capacity and maintain social distancing, there was simultaneous widespread change in the depth and breadth of National Health Service (NHS) services and a reduction in preventative care for people with diabetes [1]. We are aware of numerous mainstream media reports of reductions in the numbers of people seeking care for non‐COVID emergencies and a reported reduction in referrals for suspected malignancy.
The incidence of diabetic foot ulcer in England has been estimated at between 2 and 6% [2, 3], with considerable human and financial costs to the NHS of ~ 1% of its entire budget [3].
Delays in access to specialist care appear to worsen ulcer severity and lead to an increase in amputation [4]. Prognosis for people with diabetes post major amputation is comparable with systemic malignancy [5].
The Diabetes Care for You service provides consultant‐led specialist multi‐professional holistic out‐of‐hospital diabetes care for people within the area covered by the Brighton & Hove/High Weald Lewes and Havens clinical commissioning groups (CCGs), in line with NHS England national sample service specification for diabetes [6], and includes a well‐developed foot protection service and treatment for people with diabetes who are at increased risk for non‐ischaemic foot ulcers. We have continued active foot care clinics and increased domiciliary visits for people with foot ulcers in line with national guidance [7].
The latest full‐year National Diabetes Core Audit (NDA) data report [8] that there are 2100 people with type 1 diabetes and 17 045 with type 2 diabetes across these CCGs; comparative numbers for England are 247 350 and 3 033 505 respectively, meaning our population of people with diabetes is 0.58% of the total for England.
We evaluated routinely collected data from our SystmOne electronic patient record and processed the data using Microsoft® Excel® to assess the impact of COVID‐19 on new diabetic foot ulcer events in our service.
The incidence of new diabetic foot ulcers within our service has shown month to month variation over the last 2 years, with a mean of 48 new ulcers per month (Fig. 1). We did not see an incidence > 2 sd below the mean until April 2020. There was also a 52% reduction in new diabetic foot ulcer events in our service in April 2020 compared with April 2019.
FIGURE 1.
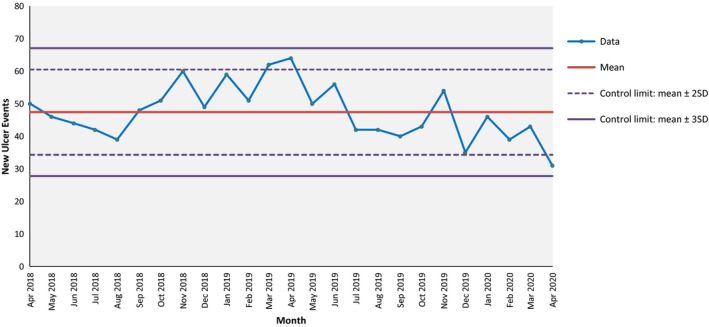
New ulceration events by month.
Our 2019–2020 annual incidence of new ulceration was 3% using latest full‐year NDA data to calculate the potential referral population. This is in line with the expected published incidence from previous series.
Our CCGs have maintained a 100% NDA participation rate and part‐year NDA data show no reduction in the prevalence of diabetes [9]; there have no service changes or local initiatives that may explain this abrupt change.
Taking our mean monthly new ulcer event rate of 48 from April 2018 to March 2020 inclusive, and applying it to the full‐year NDA‐recorded population of people with diabetes in England, one might expect 8227 ulcers per month [8]. If our April 2020 data are compared with this mean and applied to England as a whole, there are 2914 fewer new diabetic foot ulcers compared with the pre‐lockdown mean monthly rate. If we compare April 2018 and 2019 with April 2020, we might have expected to see 57 new ulcers in our service; we saw 31. Extrapolating this to the entire diabetes population of England, there is an unexplained difference of 4456.
We believe the reduction in patients with new diabetic foot ulcer events seen in our service is of immediate interest, is greater than that explained by natural variation, and needs further investigation to determine whether the reduction seen in our area is reflected across the country. It is important to determine whether the apparent reduction in ulceration is due to advised sedentary behaviour or whether there is a large cohort of patients delaying seeking care, with the potential for significant preventable harm. We recognize the limitations of the size of our population and the heterogeneity of the healthcare landscape across England. We wish to alert colleagues and recommend an urgent national review of hospital admission and outpatient diabetic foot clinic data.
Funding sources
None.
Competing interests
None declared.
References
- 1. Clinical Guide for the Management of People with Diabetes During the Coronavirus Pandemic. 19 May 2020, Version 2. Available at https://www.england.nhs.uk/coronavirus/wp‐content/uploads/sites/52/2020/03/speciality‐guide‐diabetes‐19‐march‐v2‐updated.pdf Last accessed 1 May 2020. [Google Scholar]
- 2. Paisey RB, Abbott A, Paisey CF, Walker D. Diabetic foot ulcer incidence and survival with improved diabetic foot services: an 18‐year study. Diabet Med 2019; 36: 1424–1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kerr M, Barron E, Chadwick P, Evans T, Kong WM, Rayman G et al. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med 2019; 36: 995–1002. [DOI] [PubMed] [Google Scholar]
- 4. NHS Digital . National Diabetes Foot Care Audit Fourth Annual Report: England and Wales, 01 April 2015 to 31 March 2018. Available at: https://files.digital.nhs.uk/FC/18ED7F/NDFA%204AR%20‐%20Main%20Report%20v1.1.pdf Last accessed 1 May 2020. [Google Scholar]
- 5. Hoffman M, Kujath P, Flemming A, Proß M, Begum N et al. Survival of diabetes patients with major amputation is comparable to malignant disease. Diab Vasc Diseas Res 2015; 12: 265–271. [DOI] [PubMed] [Google Scholar]
- 6. Diabetes Sample Service Specification, 30 July 2014. Available at https://diabetes‐resources‐production.s3‐eu‐west‐1.amazonaws.com/diabetes‐storage/migration/pdf/FINAL%2520Diabetes%2520Sample%2520Specification%2520V19%252029%2520July.pdf Last accessed 3 May 2020. [Google Scholar]
- 7. COVID‐19 Prioritisation Within Community Health Services, updated 2 April 2020. Available at https://www.england.nhs.uk/coronavirus/publication/covid‐19‐prioritisation‐within‐community‐health‐services‐with‐annex_19‐march‐2020/ Last accessed 2 May 2020. [Google Scholar]
- 8. NHS Digital . National Diabetes Audit Report 1 – Care Processes and Treatment Targets 2018–19 Short Report, 13 December 2019. Available at https://digital.nhs.uk/data‐and‐information/publications/statistical/national‐diabetes‐audit/report‐1‐‐care‐processes‐and‐treatment‐targets‐2018‐19‐short‐report Last accessed 3May 2020. [Google Scholar]
- 9. NHS Digital . National Diabetes Audit – Care Processes and Treatment Targets, January to September 2019, 13 February 2020. Available at https://digital.nhs.uk/data‐and‐information/publications/statistical/national‐diabetes‐audit/care‐processes‐and‐treatment‐targets‐january‐to‐september‐2019 Last accessed 11 May 2020. [Google Scholar]
Acknowledgements
We would like to acknowledge Helen Vaughan and Alistair McInnes for their constructive critique of this commentary. We would also like to acknowledge the hard work and dedication of Helen Dooley and the Diabetes Care for You team of podiatrists who continue to see people with diabetic foot complications face‐to‐face at this difficult time.
Diabet. Med. 37, 1413–1414(2020)


