Editor,
First cases of pneumonia with unknown cause were reported in Wuhan, China, in December 2019. 1 The new pathogen, called SARS‐CoV‐2, has rapidly spread reaching the level of a pandemic disease.
The worldwide diffusion of coronavirus disease 2019 (COVID‐19) is characterized by various clinical presentations and different related complications. This disease exacerbates in some patients and causes pulmonary oedema, multiple organ failure and acute respiratory distress syndrome.
Controlling the airways often requires mechanical invasive ventilation, and in cases of severe acute respiratory distress syndrome, prone positioning of the patient can reduce mortality when applied for at least 12 h daily. 2 , 3 In addition to the effectiveness of this treatment method, caretaking aspects and the side effects of this position should be also considered. Patients that undergo ventilation with ventilator in prone position face risks such as accidental removal of the tracheal tube, limited access to the venous route, bending or pulling of the catheters and chest tube, pressure wound, bruising around the mouth due to the presence of the tracheal tube, oedema around the eyes and facial oedema, gastroesophageal reflux, hyper‐salivation and skin injuries. 4 , 5
We report a 78‐year‐old male patient, hospitalized for COVID‐19 bilateral pneumonia at our hospital. After initial treatment with lopinavir/ritonavir, hydroxychloroquine, ceftriaxone and azithromycin, respiratory worsening to acute respiratory distress syndrome happened and the patient was transferred to the intensive care unit. Ventilation was applied in prone position for thirteen sessions of twenty hours each and treatment with tocilizumab and alpha interferon was added. Symmetric chest pressure ulcers developed in three days since the mechanical ventilation in prone position began (Fig. 1). Ulcers were treated with serial sharp debridement on the bed of the patient, followed by chemical debridement and hydrocolloid dressing with great response (Fig. 2). Two weeks after the skin lesions’ improvement, the patient clinical condition worsened due to bacterial coinfection, so that, ventilation in prone position was needed again and ulcers returned. At the time of this submission, the patient is still hospitalized.
Figure 1.

Symmetric chest pressure ulcers before treatment.
Figure 2.
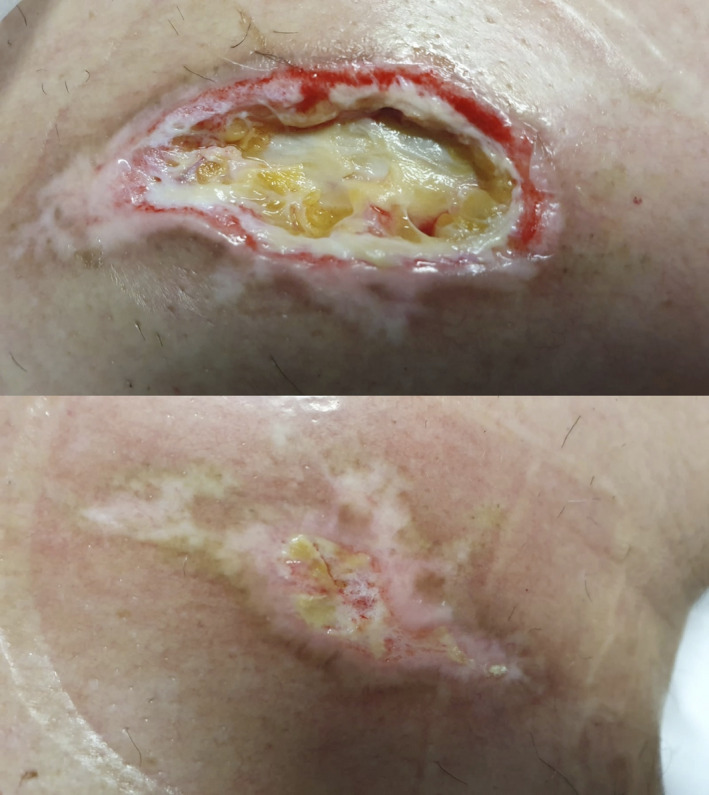
Chest pressure ulcers after treatment.
Pressure ulcers preventive measures should be implemented, as suggested in the literature. A thin silicone foam dressing can represent a valid precaution approach. The position of patients placed in prone position should be changed every 2 h and sides should be switched. Adequate local cleaning and debridement stimulate wound healing and reduce the risk of infection. Optimized nutrition is also necessary. 6
A description of the cutaneous manifestations associated with COVID‐19 has been provided lately. 7 We now present a skin consequence of this disease that may help clinicians to prevent, recognize and treat it.
The patients in this manuscript have given written informed consent to the publication of their case details.
All authors have contributed, read and approved the paper.
Conflict of interest
None.
Funding sources
None.
References
- 1. Phelan AL, Katz R, Gostin LO. The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA 2020; 323: 709. [DOI] [PubMed] [Google Scholar]
- 2. Munshi L, Del Sorbo L, Adhikari NKJ et al. Prone position for acute respiratory distress syndrome. a systematic review and meta‐analysis. Ann Am Thorac Soc 2017; 14(Supplement_4): S280–S288. [DOI] [PubMed] [Google Scholar]
- 3. Ghelichkhani P, Esmaeili M. Prone position in management of COVID‐19 patients; a commentary. Arch Acad Emerg Med 2020; 8: e48. [PMC free article] [PubMed] [Google Scholar]
- 4. Zingarelli EM, Ghiglione M, Pesce M, Orejuela I, Scarrone S, Panizza R. Facial pressure ulcers in a COVID‐19 50‐year‐old female intubated patient. Indian J Plast Surg 2020; 53: 144–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McCormick J, Blackwood B. Nursing the ARDS patient in the prone position: the experience of qualified ICU nurses. Intensive Crit Care Nurs 2001; 17: 331–340. [DOI] [PubMed] [Google Scholar]
- 6. Mervis JS, Phillips TJ. Pressure ulcers: Prevention and management. J Am Acad Dermatol 2019; 81: 893–902. [DOI] [PubMed] [Google Scholar]
- 7. Galván Casas C, Català A, Carretero Hernández G et al. Classification of the cutaneous manifestations of COVID‐19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol 2020. [Epub ahead of print]. 10.1111/bjd.19163 [DOI] [PMC free article] [PubMed] [Google Scholar]
Acknowledgements
Mariana Campayo Paños.


