Abstract
OBJECTIVES
To illustrate dissemination and asymptomatic transmission of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) during a skilled nursing facility (SNF) outbreak.
DESIGN
Case report.
SETTING AND PARTICIPANTS
Residents of a 150‐bed SNF.
MEASUREMENTS
Heat maps generated by the SNF's infection prevention team to track staff and resident symptoms and SARS‐CoV‐2 test results to identify infection patterns.
RESULTS
The SNF experienced a severe outbreak of SARS‐CoV‐2 early in the pandemic. The initial cluster of residents with symptoms and the first confirmed case occurred on the SNF's dementia care unit. The insufficient availability and prolonged turnaround time of testing for both residents and staff at the outset of the outbreak prevented timely and accurate identification and cohorting of cases. Despite extensive other infection control measures being in place, SARS‐CoV‐2 disseminated widely through the facility within 3 weeks of the first confirmed case, resulting in significant morbidity and mortality.
CONCLUSION
Early, rapid, universal SARS‐CoV‐2 testing of both SNF residents and staff at the outset of an outbreak and then repeatedly thereafter is critical to mitigate viral transmission. This will become even more important as states relax stay‐at‐home orders and SNF staff intermingle with communities that are increasingly mobile. Increased testing will inevitably result in more staff testing positive and having to self‐quarantine at home, meaning that states must partner with SNFs and other long‐term care providers to coordinate and support strategic staffing reserves that can supplement current frontline staff. J Am Geriatr Soc 68:2174–2178, 2020.
Keywords: COVID‐19, skilled nursing facility, SARS‐CoV‐2, nursing home, infection control
Long‐term care residents are particularly vulnerable to coronavirus disease 2019 (COVID‐19) caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), accounting for around half of total deaths during the pandemic both in the United States and internationally. 1 , 2 In this brief report, we present the case of a skilled nursing facility (SNF) outbreak using heat maps generated by the facility to track infection patterns over time. The experience of this SNF clearly illustrates the speed and extent to which SARS‐CoV‐2 can disseminate through a facility, despite the implementation of broad infection control measures, when widespread testing is unavailable to identify asymptomatic resident and staff cases.
CASE STUDY
Facility A is a 150‐bed SNF that specializes in long‐term care for medically frail cognitively impaired individuals, with 99% of residents carrying a dementia diagnosis. It is a single‐story building with four units, housing a secured dementia care unit. Before the start of the pandemic, most residents had advance directives in place; roughly 85% had Do Not Resuscitate orders, and approximately one‐third had Do Not Hospitalize orders.
In early March, nurses began conducting daily assessments to screen all residents for COVID‐19 symptoms. The infection prevention team prepared a dated line listing to track symptomatic residents and staff. On March 5, the facility began screening all employees and visitors on entry, turning away anyone who triggered the screen. Staff with symptoms were required to stay home and self‐quarantine for 2 weeks. On March 10, a no visitation policy was implemented. All communal dining and group activities had already ceased by then. On March 11 and 13, a facility‐wide mandatory staff in‐service was held to review respiratory outbreak management, signs and symptoms of COVID‐19, transmission prevention, and the donning and doffing of personal protective equipment. This supplemented other educational materials that had been distributed to staff and displayed around the building since the start of the month.
On March 23, two residents on the dementia care unit (B) triggered the screen for cough and one had a low‐grade fever. Both were placed on contact and droplet isolation precautions, as was the protocol for any residents with new respiratory symptoms or fever. On March 24, a direct care staff member who worked on the dementia care unit called out from work for 2 days with fever and cough. The following day, a second staff member from Unit A, who was a roommate of the first, called out from work for the same symptoms. Both individuals last worked on March 20. Both employees saw their own healthcare providers, but due to the absence of any documented widespread community presence of SARS‐CoV‐2 in the area, neither was initially tested. Facility leadership continued to monitor sick staff callouts closely.
From March 24 to March 25, four other dementia care residents developed similar symptoms. All were negative for influenza. On the morning of March 26, facility leadership notified the local board of health as well as the state department of health to report the outbreak. Facility A received six testing kits from a private laboratory to conduct polymerase chain reaction SARS‐CoV‐2 testing that same day, March 26. Five residents on the dementia care unit (B) and one resident on Unit A who had also developed symptoms were tested. Also, on March 26, Facility A began requiring that all employees wear face masks at all times when in the building. The local board of health and state department of health were updated on March 27.
The first of the six tests returned positive on March 28 for a dementia care unit resident. The senior leadership outbreak management team convened and closed Facility A to admissions. All residents on the dementia care unit were placed on contact and droplet precautions, and the unit's staff began wearing full personal protective equipment, including N95 face masks, gowns, gloves, and eye protection. The March 29 heat map (Figure 1) illustrates the location of that first confirmed case (red circle), as well as the remaining five pending tests (blue circles). At this point, there was a cluster of 16 symptomatic residents on the dementia care unit (B) and an additional two symptomatic residents on the adjacent Unit A. Symptomatic residents who were not tested are represented by green circles.
Figure 1.
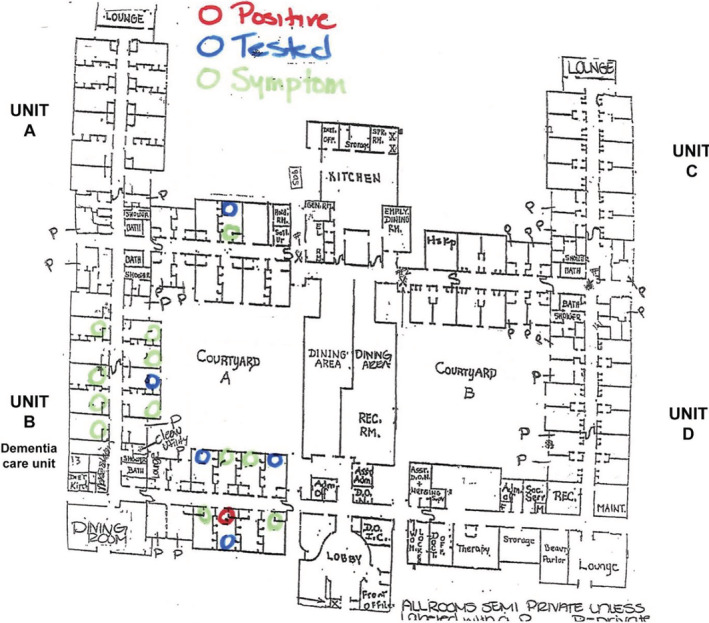
March 29 heat map. (Note: Image has been edited for clarity and deidentification.)
By March 31, a total of 22 residents on the dementia care unit (B) were exhibiting symptoms, and four were confirmed positive (Figure 2). Nine residents in Unit A and one resident on the other side of the building, Unit D, were also symptomatic. Due to still limited testing capacity, screening of asymptomatic individuals was not accepted practice at the time. However, facility leadership obtained three testing kits from a private laboratory and were able to test three asymptomatic residents in different parts of the building (yellow circles) to estimate virus dissemination. The resident spot tested in Unit A had previously had a roommate with symptoms, who was moved to another room. That resident was asymptomatic at time of testing, but developed symptoms shortly after (replaced by a blue circle), and was confirmed positive.
Figure 2.
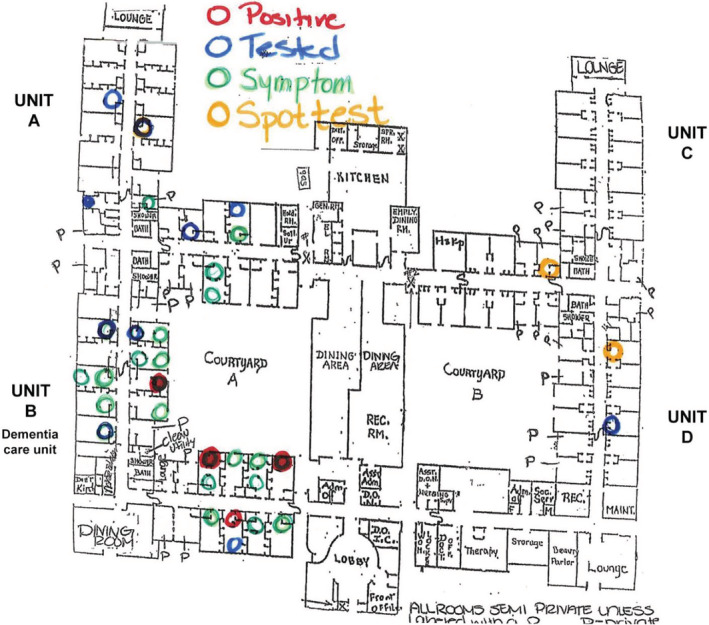
March 31 heat map. (Note: Image has been edited for clarity and deidentification.)
Figure 3 shows the building as of April 17, with deaths now represented as pink circles. Despite broad infection control measures, 3 weeks after the first confirmed case, SARS‐CoV‐2 had disseminated widely, causing many deaths. At that time, neither the state department of health nor the facility was able to support widespread staff testing, but several symptomatic staff were tested independently, and 26 employees were out of work due to confirmed or presumed COVID‐19.
Figure 3.
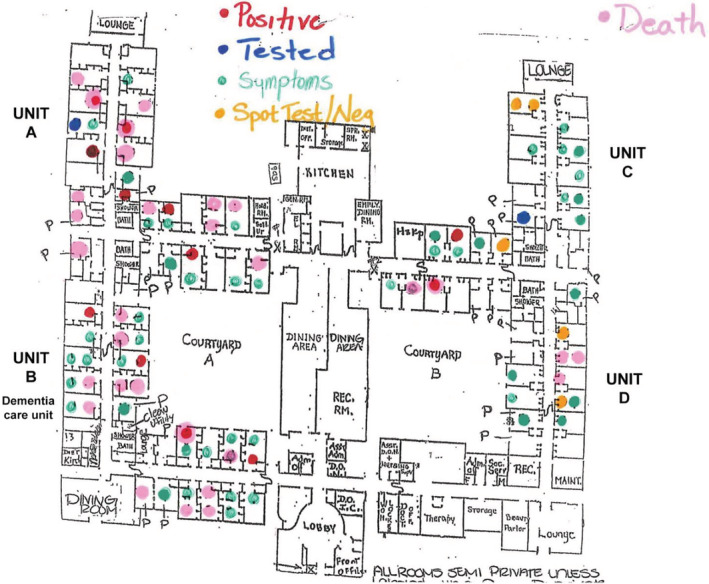
April 17 heat map. (Note: Image has been edited for clarity and deidentification.)
DISCUSSION
Facility A's experience illustrates how undetected asymptomatic SARS‐CoV‐2 transmission led to a severe outbreak with significant morbidity and mortality. Within just 3 weeks of the initial confirmed case, the virus disseminated widely throughout the building despite visitor exclusion, frequent symptom screening of residents and staff, contact and droplet precautions for symptomatic residents, universal masking, aggressive social distancing policies, and other infection control measures being in place. This dementia population was particularly vulnerable, because most residents require extensive close contact with staff for assistance with activities of daily living, including one‐to‐one feedings, personal hygiene, and position changes or transfers. The presumed index cases were two staff members who were asymptomatic when they worked, but later developed symptoms and eventually tested positive.
This underscores the importance of early, rapid, universal SARS‐CoV‐2 testing of both residents and staff at the outset of an outbreak and then repeatedly thereafter to identify cases and cohort residents appropriately. The insufficient availability and prolonged turnaround time of testing at the outset of Facility A's outbreak prevented timely and accurate identification and cohorting of cases, undermining all other infection control efforts. Adequate testing capacity is required to mitigate viral transmission to prevent further clusters and keep residents and staff as safe as possible. As states relax stay‐at‐home orders, repeated testing for SNFs will become even more essential as staff intermingle with communities that are increasingly mobile, increasing their risk of contracting the virus and introducing it into their workplace.
As important as it is to “flatten the curve” at the state level, so too is it essential at the individual SNF level to help administrators protect staff and their families, appropriately use personal protective equipment, and slow the spread of disease within a building. Repeated universal testing is an epidemiological tool to help SNFs prevent and manage outbreaks that can overwhelm already limited resources. Frequent testing will inevitably result in the identification of asymptomatic positive staff who will then have to quarantine at home for 10 to 14 days. It is thus critical that as states ramp up testing capacity and requirements, that they simultaneously partner with SNFs and other long‐term care providers to coordinate and support strategic staffing reserves that can supplement current frontline staff.
ACKNOWLEDGMENTS
Financial Disclosure
This case report was supported by the National Institute on Aging (3P01AG027296‐11S1; principal investigator: Vincent Mor).
Conflict of Interest
Vincent Mor is Chair of the Scientific Advisory Committee at NaviHealth, Inc, former Chair of the Independent Quality Committee at HCR ManorCare, and former Director of PointRight, Inc, where he holds less than 1% equity. The other authors have no conflicts of interest to disclose.
Author Contributions
Study concept and design: C.B., S.F., R.A.F., V.M., and E.M.W. Data acquisition: C.B., S.F., and R.A.F. Data analysis and interpretation: C.B., S.F., R.A.F., V.M., and E.M.W. Manuscript preparation: C.B., S.F., R.A.F., V.M., and E.M.W.
Sponsor's Role
The funding organization had no role in the design, methods, data collection, analysis, or manuscript preparation.
REFERENCES
- 1. Kaiser Family Foundation . State reports of long‐term care facility cases and deaths related to COVID‐19. 2020. https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/. Accessed May 12, 2020.
- 2. Comas‐Herrera A, Zalakaín J, Litwin C, Hsu AT, Lane N, Fernández JL. Mortality associated with COVID‐19 outbreaks in care homes: early international evidence. 2020. https://ltccovid.org/wp-content/uploads/2020/05/Mortality-associated-with-COVID-3-May-final-5.pdf. Accessed May 7, 2020.


