Editor
The novel severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) is the causative agent of the coronavirus disease 2019 (COVID‐19). The pandemic condition was declared by the WHO on 11 March 2020.
The main clinical symptoms are fever, dry cough and dyspnoea, although new symptoms are emerging, such as diarrhoea, anosmia and ageusia. The virus enters cells, likely including those lining blood vessels, by binding to angiotensin‐converting enzyme 2 (ACE2) receptors on the cell surface. Infection can also promote blood clots, heart attacks and cardiac inflammation. 1
In the literature, some dermatological manifestations have recently been reported, such as erythematous, vesiculous and urticarial rashes. 2 , 3 , 4 However, there are no data about nail signs occurring during COVID 19.
A 60‐year‐old otherwise healthy woman presented with a history of fever (>38°C) and cough.
Seven days after the onset of these symptoms the patient referred dyspnoea, associated with anosmia and ageusia. Although chest X‐ray examination was normal, chest CT revealed ground‐glass opacity, leading to a diagnosis of bilateral interstitial pneumonia. A positive RT‐PCR nasopharyngeal swab confirmed SARS‐CoV‐2 infection.
The patient was hospitalized and underwent oxygen therapy together with administration of several drugs, including hydroxychloroquine, lopinavir/ritonavir, ceftriaxone and heparin. Complete remission of respiratory symptoms, associated with negative nasopharyngeal swab was seen 10 days after the treatment was started.
Two weeks after symptoms onset, a distally convex half‐moon‐shaped red band surrounding the distal margin of the lunula appeared on all fingernails (Fig. 1). The patient denied any associated symptoms, and no other skin manifestations were observed. Her dermatological medical history was unremarkable. After one month of follow‐up, the bands are still present and wider (Fig. 2).
Figure 1.

Distally convex half‐moon‐shaped red bands surrounding the distal margin of the lunula.
Figure 2.
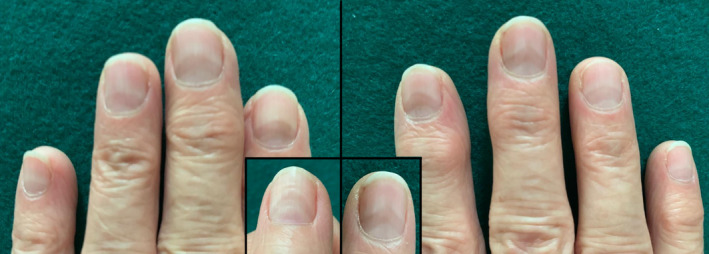
The half‐moon‐shaped red bands are still present after 1 month of follow‐up on all fingernails and appear wider.
Polydactylous erythronychia differential diagnosis includes lichen planus, Darier’s disease and the more rare primary amyloidosis and graft‐versus‐host disease. In all these conditions, however, erythronychia is arranged in longitudinal lines, 5 while in our case erythronychia has an half‐moon shape margining the lunula.
Transversal red bands of the nail were reported for the first time by Lindsley 6 in four patients affected by Kawasaki disease. Unlike our case, however, in those patients the bands were localized in the distal part of the nail bed, in the so‐called nail isthmus.
The pathogenesis of the half‐moon‐shaped transversal red bands seen in our patient after SARS‐CoV‐2 infection is unknown. A localized microvascular injury secondary to inflammatory immune response and a procoagulant state 7 might play a central role. Due to the localization, we hypothesized a damage of the capillary network of the distal subungual arcade.
To the best of our knowledge, this is the first case of nail involvement. This sign is peculiar and has not been previously described even in dermatological or systemic diseases. Further studies are needed to validate our finding and to assess whether red half‐moon nail could represent a pathognomic sign of COVID19.
Conflict of interest
Dr. Neri, Dr. Guglielmo, Dr. Virdi, Dr. Gaspari, Dr. Starace and Dr. Piraccini have nothing to disclose.
Funding source
None.
References
- 1. Wadman M, Couzin‐Frankel J, Kaiser J, Matacic C. A rampage through the body. Science 2020; 368: 356–360. [DOI] [PubMed] [Google Scholar]
- 2. Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol 2020; 34: e212–e213. [DOI] [PubMed] [Google Scholar]
- 3. Marzano AV, Genovese G, Fabbrocini G et al. Varicella‐like exanthem as a specific COVID‐19‐associated skin manifestation: multicenter case series of 22 patients. J Am Acad Dermatol 2020; 83: 280–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Henry D, Ackerman M, Sancelme E et al. Urticarial eruption in COVID‐19 infection. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jellinek NJ. Longitudinal erythronychia: suggestions for evaluation and management. J Am Acad Dermatol 2011; 64:167.e1–167.e11. [DOI] [PubMed] [Google Scholar]
- 6. Lindsley CB. Nail‐bed lines in Kawasaki disease. Am J Dis Child 1992; 146: 659–660. [DOI] [PubMed] [Google Scholar]
- 7. Magro C, Mulvey JJ, Berlin D et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID‐19 infection: a report of five cases. Transl Res 2020; 220: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Acknowledgement
The patient in this manuscript has given written informed consent to the publication of her case details.


