General approach
The current pandemic of a novel coronavirus disease 2019 (COVID‐19) began in December 2019 in Wuhan, China, and has since spread worldwide [1]. Pandemic preparedness has been an ongoing project in Iceland since the severe acute respiratory syndrome (SARS) epidemic in 2003–2004. In mid‐January 2020, the Directorate of Health (DOH) and the Department of Civil Protection and Emergency Management (DCPEM) revised the current pandemic preparedness response plan. The DOH and DCPEM, in close collaboration with the Department of Clinical Microbiology and Internal Medicine Services at Landspitali–The National University Hospital (LUH) and deCODE genetics, initiated a nationwide surveillance program for COVID‐19, including diagnostic testing which began on 31 January. A report describing the extensive screening efforts in Iceland has recently been published [2].
The first case of COVID‐19 in Iceland was diagnosed on 28 February. Immediately, a plan was activated to contact all SARS‐CoV‐2‐positive patients upon diagnosis, trace contacts and initiate isolation and quarantine to minimize spread in the community. The principal objectives were to gain control, prevent unexpected visits to the Emergency Department and to facilitate appropriate care early in the course of illness. In the beginning, an infectious disease specialist contacted all diagnosed patients daily to monitor their symptoms. As the outbreak progressed, additional physicians and nurses were allocated to this service, establishing a comprehensive telehealth program.
In the first two weeks, statistical models projected a dramatic rise in the overall number of COVID‐19 cases and the number of patients requiring hospital admission (Fig. 1). Due to a rapid increase in the number of cases, restrictions on public gatherings and guidance on social distancing were implemented on 16 March and were continued in the ensuing weeks.
Figure 1.
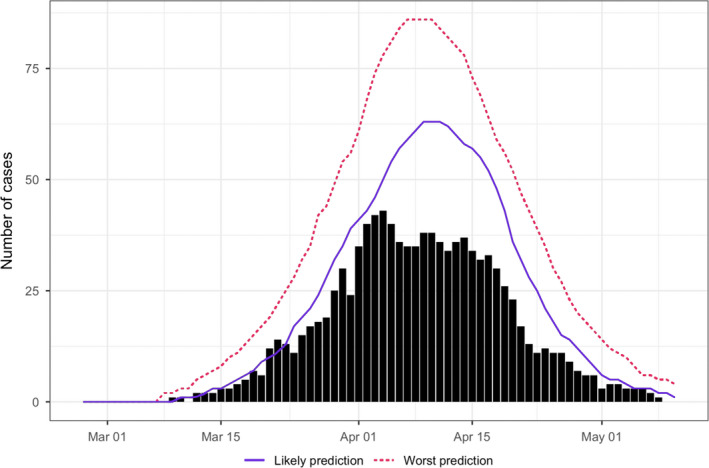
Projected and observed number of patients hospitalized for COVID‐19 [3]. The median number of projected hospitalizations is illustrated as a blue line and upper limit of the 95% prediction interval shown as a red dashed line. The observed hospitalizations are depicted as black bars. [Correction added on 5 October 2020, after first online publication: In Figure 1, the caption has been changed in this current version.]
The COVID‐19 Clinic
As the epidemic grew, a systematic approach to monitoring patients was developed and an outpatient clinic was formally established. The primary goals of the clinic included close monitoring of patients to provide them with instant access to appropriate care, aiming to decrease the risk of unexpected hospitalization, reduce morbidity and increase quality of life.
The COVID‐19 Clinic was divided into two units: a telehealth centre and a specialized urgent care clinic.
The COVID‐19 Telehealth Centre
All SARS‐CoV‐2‐positive patients were captured and entered into a database in the electronic medical record system at LUH. The list of patients was automatically updated in real time when new patients tested positive at the Department of Clinical Microbiology or deCODE genetics.
All patients were enrolled into a telehealth monitoring program through an interview with a physician, who systematically documented past medical history, medication use, social history, lifestyle factors and allergies. A standardized checklist containing 19 symptoms was filled out for each phone call.
Patients were stratified into three risk categories according to age and underlying conditions, which included cardiovascular disease, hypertension, diabetes, chronic lung disease, chronic kidney disease, cancer and systemic inflammatory diseases. The risk categories were as follows: (i) low (age <50 years, no underlying conditions); (ii) intermediate (age 50–70 years without underlying conditions or <50 years with underlying conditions); and (iii) high (age 50–70 years with underlying conditions or >70 years). Clinical severity categories were created based on weighted symptoms that were loosely defined as: (i) green (mild and improving symptoms); yellow (mild dyspnoea, cough or fever for <5 days); or (iii) red (worsening dyspnoea, worsening cough, high or persistent fever for 5 days or longer, or severe fatigue). Risk category and clinical severity score then determined the frequency of contact with telehealth providers. All subsequent follow‐up phone calls were carried out by nurses. During each phone call, the patient was reminded of the importance of maintaining isolation to limit the spread of the disease.
The patients were also given a direct phone number to the telehealth service and instructions to call to report if their condition worsened between scheduled calls or if they had other concerns. During the structured follow‐up interviews, nurses reviewed symptoms, updated the clinical score and provided treatment recommendations. If patients reported worsening symptoms, they were monitored more frequently and contacted by a physician who determined if urgent medical evaluation was needed.
The patients were monitored via the telehealth service for at least 14 days. A discharge phone call was made by a physician when the patient fulfilled two predetermined criteria; 14 days had passed from their first positive test, and they had been symptom‐free for seven days.
By 7 May, 1762 patients had been enrolled into telehealth monitoring. Their median age was 42 years (IQR, 27–54) and 904 (51.3%) were women. A total of 20 919 phone calls were made from 28 February to 7 May, and the median number of calls per patient was 9 (IQR, 7–13). All patients complied with this strategy. Patients (n = 36) who were diagnosed during hospitalization were not enrolled in the telehealth program during their hospital stay. However, patients who were discharged before they had fully recovered were closely monitored following discharge.
Smartphone telehealth application
In order to provide daily monitoring to the growing number of patients, the DCPEM sponsored the creation of a smartphone application that was designed in collaboration with physicians at the COVID‐19 Clinic. The application allowed patients to report symptoms to the telehealth centre via a web portal. Additionally, the application provided patients with important information about COVID‐19 symptoms, treatment measures, exercise and mental health support.
The COVID‐19 Urgent Care Clinic
Patients reporting severe or worsening symptoms were referred for clinical evaluation. In the first weeks of the outbreak, patients were evaluated in the LUH Emergency Department and through house calls carried out by primary care physicians. In order to minimize the risk of viral spread within the hospital and to meet the rising demand for care, a specialized urgent care clinic was opened on 24 March in a separate facility on the hospital campus. It took only several days to refurbish the facility with appropriate isolation rooms. Patients were assessed in a standardized manner which included full physical examination, laboratory testing, 2‐minute walk test with pulse oximetry and imaging as needed. Front line medical staff consisted of doctors in postgraduate training and nurses, who all wore full personal protective equipment, whilst a supervising consultant physician participated in the patient interviews through a video call. Based on this evaluation, a decision whether to admit patients to the hospital was made. No staff member was infected whilst working at the COVID‐19 Clinic.
Patients not requiring hospitalization generally received appropriate supportive treatment. Hydroxychloroquine or azithromycin was administered to selected patients based on an treatment protocol developed by the Division of Infectious Disease. The outpatient clinic served all COVID‐19 patients in the Greater Reykjavik area, and there was close collaboration with healthcare providers in other regions of Iceland.
In total, 101 COVID‐19 patients had been admitted to LUH by 7 May. Ten patients died from the disease. From 24 March to 7 May, 212 patients were seen at the COVID‐19 Clinic in 362 visits, 130 (61.3%) of whom were women. Most patients attended the clinic once but 83 patients attended more frequently. Out of those 212 patients, 47 were admitted to the hospital. All patients who received care in the COVID‐19 Clinic survived.
Conclusions
Although the COVID‐19 pandemic is not yet over, we believe that our systematic approach to the combination of community management and patient care, including societal interventions, screening, isolation, meticulous contact tracing, quarantine, telehealth services, and an outpatient clinic providing urgent care may have resulted in favourable outcomes, highlighted by relatively few hospital admission and lower mortality than was initially projected. Ongoing studies analysing our efforts will be reported in the scientific literature.
Conflict of Interest
The authors have no conflicts of interest to declare.
Author Contribution
Dadi Helgason: Conceptualization (equal); Data curation (supporting); Formal analysis (supporting); Methodology (equal); Writing‐original draft (equal). Elias S Eythorsson: Conceptualization (equal); Data curation (lead); Formal analysis (lead); Methodology (equal); Writing‐original draft (equal). Lovisa B Olafsdottir: Conceptualization (supporting); Methodology (supporting); Writing‐review & editing (supporting). Tomas Agustsson: Conceptualization (supporting); Methodology (supporting); Writing‐review & editing (supporting). Steinunn Ingvarsdottir: Conceptualization (supporting); Methodology (supporting); Writing‐review & editing (supporting). Solveig Sverrisdottir: Conceptualization (supporting); Methodology (supporting); Writing‐review & editing (supporting). Erla D Ragnarsdottir: Conceptualization (supporting); Methodology (supporting); Writing‐review & editing (supporting). Magnus Gottfredsson: Conceptualization (supporting); Methodology (supporting); Writing‐review & editing (supporting). Olafur Gudlaugsson: Conceptualization (supporting); Methodology (supporting); Writing‐review & editing (supporting). Runolfur Palsson: Conceptualization (equal); Methodology (supporting); Supervision (equal); Writing‐review & editing (supporting). Ragnar F Ingvarsson: Conceptualization (equal); Methodology (equal); Supervision (equal); Writing‐original draft (equal).
References
- 1. Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2021; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gudbjartsson DF, Helgason A, Jonsson H et al. Spread of SARS‐CoV‐2 in the Icelandic population. N Engl J Med 2020; 382: 2302–2315. 10.1056/NEJMoa2006100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jonsson BG, Hrafnkelsson B, Aspelund T et al.Spálíkan fyrir fjölda tilfella og álag á heilbrigðis�jónustu [A prediction model for the number of COVID‐19 cases and the corresponding burden on the health care system]. Reykjavik, Iceland: University of Iceland; 2020; Available from: https://covid.hi.is/spa‐30‐april‐2020/. [Google Scholar]


