Abstract
BACKGROUND/OBJECTIVES
To determine the associations of nursing home registered nurse (RN) staffing, overall quality of care, and concentration of Medicaid or racial and ethnic minority residents with 2019 coronavirus disease (COVID‐19) confirmed cases and deaths by April 16, 2020, among Connecticut nursing home residents.
DESIGN
Cross‐sectional analysis on Connecticut nursing home (n = 215) COVID‐19 report, linked to other nursing home files and county counts of confirmed cases and deaths. Multivariable two‐part models determined the associations of key nursing home characteristics with the likelihood of at least one confirmed case (or death) in the facility, and with the count of cases (deaths) among facilities with at least one confirmed case (death).
SETTING
All Connecticut nursing homes (n = 215).
PARTICIPANTS
None.
INTERVENTION
None.
MEASUREMENTS
Numbers of COVID‐19 confirmed cases and deaths among residents.
RESULTS
The average number of confirmed cases was eight per nursing home (zero in 107 facilities), and the average number of confirmed deaths was 1.7 per nursing home (zero in 131 facilities). Among facilities with at least one confirmed case, every 20‐minute increase in RN staffing (per resident day) was associated with 22% fewer confirmed cases (incidence rate ratio [IRR] = .78; 95% confidence interval [CI] = .68–.89; P < .001); compared with one‐ to three‐star facilities, four‐ or five‐star facilities had 13% fewer confirmed cases (IRR = .87; 95% CI = .78–.97; P < .015), and facilities with high concentration of Medicaid residents (IRR = 1.16; 95% CI = 1.02–1.32; P = .025) or racial/ethnic minority residents (IRR = 1.15; 95% CI = 1.03–1.29; P = .026) had 16% and 15% more confirmed cases, respectively, than their counterparts. Among facilities with at least one death, every 20‐minute increase in RN staffing significantly predicted 26% fewer COVID‐19 deaths (IRR = .74; 95% CI = I .55–1.00; P = .047). Other focused characteristics did not show statistically significant associations with deaths.
CONCLUSION
Nursing homes with higher RN staffing and quality ratings have the potential to better control the spread of the novel coronavirus and reduce deaths. Nursing homes caring predominantly for Medicaid or racial and ethnic minority residents tend to have more confirmed cases.
Keywords: COVID‐19, coronavirus, nursing home, disparities, death
As of April 28, 2020, there were nearly 3 million confirmed cases of coronavirus disease 2019 (COVID‐19) and 202,597 deaths globally, with 960,916 confirmed cases and 49,170 deaths in the United States. 1 Residents of long‐term care (LTC) facilities were shown to be highly vulnerable to respiratory disease outbreaks, such as those of influenza or other common human coronaviruses. 2 , 3 Current evidence suggests that COVID‐19 disproportionately affects older adults and persons with chronic health conditions, leading to higher attack rates and more severe adverse outcomes, such as deaths, among them. 4 , 5 , 6 Nursing home residents are characterized by advanced age, more frequent and complex chronic disease patterns, and highly impaired physical, cognitive, and immune system functions that together put them at the greatest risk of severe COVID‐19 infections. 7 , 8 , 9
After the identification of the first confirmed COVID‐19 case in a skilled nursing facility in Seattle, Washington, on February 28, a case investigation conducted by the Public Health–Seattle and King County and the Centers for Disease Control and Prevention (CDC) 7 reported that as of March 18, a total of 167 confirmed COVID‐19 cases affecting nursing home residents, care providers, and visitors were found to be linked epidemiologically to that facility, and that more than one‐half of infected residents were hospitalized and one‐third dead. By April 23, 4,069 LTC facilities in 36 states had been hit by COVID‐19, and more than 10,000 deaths of LTC residents and staff were reported in 23 states. 10
Research is urgently needed to understand COVID‐19 transmissions in LTC facilities and to identify important facility characteristics that may be associated with the spread of the novel coronavirus and case fatality among residents. Strong evidence and broad consensus exist that higher nurse staffing levels in nursing homes, especially higher registered nurse (RN) hours, improve safety of care and resident outcomes. 11 , 12 , 13 , 14 Residents in nursing homes with better quality of care were also shown to have better health outcomes such as reduced risks of pressure ulcers and mortality. 15 , 16 , 17 Moreover, it is widely reported that nursing homes caring for a disproportionately high number of disadvantaged residents, including Medicaid residents and racial or ethnic minority residents, tend to have more limited financial and clinical resources that lead to poorer quality and safety outcomes for their residents. 18 , 19 , 20 , 21 , 22 , 23 However, COVID‐19 is a novel, rapidly evolving pandemic, and evidence regarding COVID‐19–related outcomes and their variation among nursing homes is lacking.
This study describes variations in COVID‐19–confirmed cases and deaths among residents in Connecticut nursing homes through April 16, 2020, and it evaluates their associations with important nursing home characteristics. We test the hypotheses that nursing homes with higher RN staffing level and better overall quality of care have fewer confirmed cases and deaths, whereas facilities in which Medicaid‐paid residents and racial/ethnic minority residents predominate have worse COVID‐19 outcomes.
METHODS
Data Sources and Variables for Connecticut Nursing Homes
We first obtained data on COVID‐19 laboratory‐confirmed cases and associated deaths in each of Connecticut's nursing homes as of April 16, 2020. These data were collected and regularly updated by the Connecticut Department of Health and Human Services (https://data.ct.gov/Health-and-Human-Services/Nursing-Homes-with-Residents-Positive-for-COVID-19/wyn3-qphu) and were also published in a recent news report. 24 These data were then linked to the Nursing Home Compare (NHC) data files (updated on March 31, 2020), 25 a data system published by the Centers for Medicare & Medicaid Services (CMS) for tracking and reporting nurse staffing, quality of care, findings of state government inspections of nursing home care practices, and other facility characteristics. 16
We obtained the following variables in the NHC files that were potentially associated with resident safety and health outcomes 12 , 13 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 : total number of beds, average daily resident census, ownership status (for profit vs nonprofit or government owned), affiliation with a chain (yes/no), percentage of Medicare residents, percentage of Medicaid residents, average staffing level (hours per resident day) for RNs in 2019, average total nurse staffing level (including RNs, licensed practical nurses, and certified nursing assistants) in 2019, and five‐star ratings for overall quality of care.
The RN and other nurse staffing levels were calculated based on daily resident census and the CMS Payroll‐Based Journal system that allows nursing homes to submit electronically the number of hours that care workers (including agency and contract staff) are paid to work each day. 26 As required by Section 6106 of the Affordable Care Act, the payroll‐based data are submitted quarterly on different types of nursing staff and subject to audit to ensure accuracy. The five‐star ratings aggregate alternative nursing home quality measures into a rating system of one to five stars, with more stars indicating better quality. 27 Specifically, ratings were first developed to summarize three separate domains of “quality”: deficiency citations assigned during annual and complaint inspections; a set of clinical outcomes of residents based on Minimum Data Set (MDS) assessments; and nurse staffing to resident ratios. The overall five‐star ratings were then derived from these domain‐specific ratings using a CMS‐developed algorithm. 27
We used data from the LTCFocUS.org website to obtain two additional variables. These data were created by the Center for Gerontology and Healthcare Research at Brown University by combining multiple sources of resident and nursing home records such as the MDS for all nursing home residents, Medicare enrollment file, and CMS‐maintained facility files. The first variable we obtained was percentage of racial and ethnic minority residents (African Americans, Hispanics, Asians or Pacific Islanders, and American Indians or Alaskan Natives) in the nursing home that was originally defined using the race and ethnicity information in the MDS and Medicare enrollment databases. We also obtained a variable for facility‐level case mix, derived from the resource utilization group classification of all residents in the nursing home; the case‐mix index was calculated by averaging the acuity scores of all residents (approximated by the relative staff time demanded by the resident) in the facility, with higher value indicating higher average acuity.
County COVID‐19 Infections and Demographics
We downloaded data of the numbers of laboratory‐confirmed cases and deaths of COVID‐19 in all counties in the United States, as published by the New York Times (https://github.com/nytimes/covid-19-data). These numbers have been compiled and updated in real time by the Times based on reports from state and local health agencies since the first reported coronavirus case in Snohomish County, Washington, on January 20, 2020. 28 Using these data we calculated, for each of the eight counties in Connecticut, the total number of confirmed COVID‐19 cases as of April 16, 2020 (with and without nursing home confirmed cases). Similarly, we calculated the total number of COVID‐19 deaths in the county, with and without nursing home deaths. Lastly, we used the 2018 Area Healthcare Resource File (https://data.hrsa.gov/topics/health-workforce/ahrf) to obtain information about county population size.
Statistical Analyses
We examined the distributions of nursing home COVID‐19 confirmed cases and deaths, as well as other nursing home characteristics overall, by number of confirmed cases (0, 1–10, and 11–69) and by number of COVID‐19–related deaths (0, 1–5, and 6–15). We also summarized county characteristics and plotted the percentages of COVID‐19 cases and deaths that were attributed to nursing home residents in each county.
Multivariable analyses determined the associations of four independent variables with numbers of confirmed cases and deaths in nursing homes (dependent variables in separate models). The four independent variables were nursing home RN staffing, overall quality of care (measured by overall five‐star ratings and categorized as four‐ or five‐star facilities vs one‐ to three‐star facilities), concentration of Medicaid residents (categorized as facilities in the top quartile group vs other facilities), and concentration of racial and ethnic minority residents (facilities in the top quartile group vs other facilities).
We fit separate two‐part models at the nursing home level to account for the fact that a relatively large number of nursing homes had zero confirmed cases and deaths. 29 The first part of the models was a generalized linear model with a logit link function and assuming binomial distribution that estimated the likelihood of a nursing home having at least one confirmed case (or death). The second part is a count model assuming a Poisson distribution that estimated the number of cases (or deaths) conditional on at least one confirmed case (or death) that was found in the nursing home as of April 16, 2020. Both parts of the model controlled for the same nursing home covariates (Table 1) as well as two county covariates: total number of confirmed cases (or deaths) in the county other than nursing home cases (deaths) and county population size. After model estimation, we obtained the predicted counts of confirmed cases and deaths for all nursing homes and plotted each predicted count against the independent variables.
Table 1.
Characteristics of Connecticut Nursing Homes by Confirmed COVID‐19 Cases or Deaths Among Nursing Home Residents as of April 16, 2020
| Characteristic | Total confirmed cases, N | Total deaths, N | All | ||||
|---|---|---|---|---|---|---|---|
| 0 | 1–10 | 11–69 | 0 | 1–5 | 6–15 | ||
| Nursing homes, N | 107 | 45 | 63 | 131 | 61 | 23 | 215 |
| Mean (IQR) or N (%) | |||||||
| Confirmed cases | 0 | 5.2 (3–8) | 23.5 (13–30) | .9 (0–0) | 14.5 (8–19) | 30.9 (20–40) | 8.0 (0–12) |
| Confirmed deaths | 0 | .9 (0–1) | 5.3 (2–8) | 0 | 2.5 (1–4) | 9.6 (8–12) | 1.7 (0–2) |
| Nurse staffing, hours per resident day | |||||||
| RN | .8 (.6–.9) | .6 (.5–.7) | .6 (.4–.7) | .8 (.5–.9) | .6 (.5–.7) | .5 (.4–.7) | .7 (.5–.8) |
| Total (RNs + LPNs + CNAs) | 3.8 (3.4–4.2) | 3.6 (3.3–3.8) | 3.6 (3.2–3.7) | 3.8 (3.3–4.2) | 3.6 (3.2–3.8) | 3.5 (3.2–3.6) | 3.7 (3.3–4.0) |
| Overall 5‐star rating | 3.6 (2–5) | 3.2 (2–4) | 3.1 (2–4) | 3.5 (2–5) | 3.1 (2–4) | 3.3 (2–4) | 3.4 (2–4) |
| 4‐ or 5‐star facilities, % | 67 (62.6) | 20 (45.5) | 27 (42.9) | 75 (57.7) | 28 (45.9) | 11 (47.8) | 114 (53.3) |
| Residents paid by Medicaid, % | 61.4 (55.4–75.6) | 65.7 (60.7–76.1) | 70.2 (60.1–81.6) | 62.2 (56.0–75.6) | 68.6 (61.7–81.6) | 70.0 (63.5–79.3) | 64.9 (58.3–78.1) |
| Racial or ethnic minority residents, % | 12.0 (1.9–17.2) | 16.2 (6.0–22.8) | 19.3 (3.2–32.3) | 12.9 (2.3–18.4) | 18.9 (4.8–28.4) | 16.6 (2.2–27.3) | 15.0 (2.7–21.7) |
| Beds, n | 98.7 (60–120) | 127.0 (93–150) | 150.0 (120–161) | 103.3 (60–126) | 140.0 (114–155) | 158.0 (120–180) | 120.0 (76–148) |
| Average daily resident census | 85.0 (51.5–108.4) | 108.6 (83.7–129.6) | 131.3 (100.1–143.3) | 88.7 (56.4–111.4) | 120.4 (96.8–136.8) | 143.1 (108.6–156.4) | 103.6 (70.1–123.8) |
| For‐profit ownership, N (%) | 83 (77.6) | 40 (88.9) | 56 (88.9) | 105 (80.2) | 54 (88.5) | 20 (87.0) | 179 (83.3) |
| Chain affiliation, N (%) | 47 (43.9) | 26 (59.1) | 37 (58.7) | 60 (46.2) | 39 (63.9) | 11 (47.8) | 110 (51.4) |
| Case‐mix acuity | 1.1 (1.0–1.2) | 1.1 (1.0–1.2) | 1.1 (1.1–1.2) | 1.1 (1.0–1.2) | 1.1 (1.1–1.2) | 1.1 (1.1–1.2) | 1.1 (1.0–1.2) |
| Residents paid by Medicare, % | 15.3 (8.8–17.6) | 15.0 (9.2–17.8) | 13.9 (8.8–17.9) | 15.4 (9.3–17.6) | 14.3 (8.4–17.5) | 13.0 (9.4–18.2) | 14.8 (8.8–17.6) |
Abbreviations: CNA, certified nursing assistant; IQR, interquartile range; LPN, licensed practical nurse; RN, registered nurse.
RESULTS
In all 215 Connecticut nursing homes (Table 1) and by April 16, 2020, the average number of confirmed cases was 8 per nursing home (interquartile range [IQR] = 0–12), but the number ranged from zero for about half of all nursing homes (n = 107) to as high as 69 in one nursing home. The number of confirmed deaths was 1.7 per nursing home on average (IQR = 0–2), ranging from zero for 131 nursing homes to 15 in two nursing homes. Nursing homes with fewer confirmed cases tended to have a higher RN staffing level (.8 hours per resident day for facilities with zero cases and .6 hours per resident day for facilities with 1–10 and 11–69 cases), lower five‐star ratings, and higher concentrations of Medicaid and racial/ethnic minority residents. Similar trends were found for confirmed deaths. Nursing homes with more confirmed cases or deaths were also more likely to be large for‐profit facilities affiliated with a chain and having a higher resident census.
Table 2 shows that by April 16, the cumulative number of confirmed cases was 3.0 per 1,000 population in Connecticut but ranged from .7 to 7.2 over the eight counties; the cumulative number of COVID‐19 deaths was .2 per 1,000 population with a range of .01 to .4 over counties. The number of confirmed cases of Connecticut nursing home residents was 5.2 per 100 nursing home beds (range = 0–8.9 over counties), and the number of COVID‐19 deaths was 1.2 per 100 nursing home beds (range = 0–2.6 over counties). The proportion of confirmed cases who were nursing home residents in Connecticut was 11.2% (ranging from 0% to 19.5% over counties), but the corresponding proportion for deaths was 38.7% in the state with a range from 0% to 50% over counties (Supplementary Figure S1).
Table 2.
Characteristics of Counties (n = 8) in Connecticut
| Characteristic | Mean (range) |
|---|---|
| Confirmed cases | 1,918.8 (87–6,816) |
| COVID‐19 deaths | 121.1 (1–406) |
| Population size × 1,000 | 446.6 (117.0–943.8) |
| Cases per 1,000 population | 3.0 (.7–7.2) |
| Deaths per 1,000 population | .2 (.01–.4) |
| Confirmed cases of nursing home residents | 214.1 (0–516) |
| COVID‐19 deaths of nursing home residents | 46.9 (0–142) |
| Total number of nursing home beds | 3,213 (678–7,689) |
| Confirmed cases of nursing home residents per 100 beds | 5.2 (0–8.9) |
| COVID‐19 deaths of nursing home residents per 100 beds | 1.2 (0–2.6) |
Multivariable analyses showed that RN staffing, five‐star ratings, and concentrations of Medicaid and racial/ethnic minority residents in the nursing home were not statistically significantly associated with the likelihood of having one or more confirmed cases in the facility, after controlling for facility and county covariates (Table 3). However, among facilities with at least one case, these facility characteristics were significantly associated with the count of cases. Every 20 minutes (per resident day) increase in RN staffing was associated with a 22% reduction in confirmed cases (incidence rate ratio [IRR] = .78; 95% confidence interval [CI] = .68–.89; P < .001). Compared with one‐ to three‐star facilities, four‐ or five‐star facilities showed 13% fewer confirmed cases (IRR = .87; 95% CI = .78–.97; P < .015). Nursing homes with a high concentration of Medicaid residents (IRR = 1.16; 95% CI = 1.02–1.32; P = .025) or racial/ethnic minority residents (IRR = 1.15; 95% CI = 1.03–1.29; P = .026) had 16% and 15% fewer confirmed cases, respectively, compared with their counterparts.
Table 3.
Associations of Nursing Home Registered Nurse Staffing, Quality of Care, and Concentrations of Medicaid and Racial/Ethnic Minority Residents with COVID‐19 Confirmed Cases and Deaths Among Nursing Home Residents a
| Two‐part model for confirmed cases | |||
| Part 1: Likelihood of ≥1 case, all facilities | β coefficient | OR (95% CI) | P value |
| RN staffing, every 20 min per resident d | −.21 | .81 (.41–1.60) | .540 |
| 4‐ or 5‐star ratings vs otherwise | −.29 | .75 (.37–1.51) | .416 |
| NHs concentrated by Medicaid residents b | .41 | 1.50 (.60–3.74) | .384 |
| NHs concentrated by racial/ethnic minority residents c | −.03 | .97 (.42–2.23) | .941 |
| Part 2: Count of cases in facilities with ≥1 case | β coefficient | IRR (95% CI) | P value |
| RN staffing, every 20 min per resident‐day | −.25 | .78 (.68–.89) | <.001 |
| 4‐ or 5‐star ratings, vs otherwise | −.14 | .87 (.78–.97) | .015 |
| NHs concentrated by Medicaid residents b | .15 | 1.16 (1.02–1.32) | .025 |
| NHs concentrated by racial/ethnic minority residents c | .14 | 1.15 (1.03–1.29) | .026 |
| Two‐part model for confirmed deaths | |||
| Part 1: Likelihood of ≥1 death (all facilities) | β coefficient | OR (95% CI) | P value |
| RN staffing, every 20 min per resident d | −.47 | .62 (.29–1.35) | .229 |
| 4‐ or 5‐ star ratings, vs otherwise | .25 | 1.29 (.61–2.72) | .507 |
| NHs concentrated by Medicaid residents b | .81 | 2.24 (.88–5.67) | .090 |
| NHs concentrated by racial/ethnic minority residents c | .07 | 1.08 (.46–2.53) | .866 |
| Part 2: Count of deaths in facilities with ≥1 death | β coefficient | IRR (95% CI) | P value |
| RN staffing, every 20 min per resident d | −.30 | .74 (.55–1.00) | .047 |
| 4‐ or 5 star ratings, vs otherwise | −.02 | .98 (.77–1.25) | .898 |
| NHs concentrated by Medicaid residents b | −.10 | .91 (.70–1.18) | .459 |
| NHs concentrated by racial/ethnic minority residents c | −.11 | .89 (.70–1.15) | .377 |
Abbreviations: CI, confidence interval; IRR, incidence rate ratio; NH, nursing home; OR, odds ratio; RN, registered nurse.
Two part models for confirmed cases and deaths separately that controlled for the nursing home covariates in Table 1, county total number of confirmed cases less nursing home cases (or county total number of deaths less nursing home deaths), and county population size.
Defined as NHs in the top quartile group for percentage of Medicaid residents (i.e., ≥78.1%) versus all other NHs in Connecticut.
Defined as nursing homes in the top quartile group for percentage of racial and ethnic minority residents (i.e., ≥21.7%) versus all other nursing homes in Connecticut.
Figure 1A shows the predicted number of confirmed cases combining estimates from both parts of the two‐part model and demonstrates strong negative association between RN staffing and predicted count (P = .001 based on a joint test on estimates of the two parts). Supplementary Figure S2, panel A, similarly shows the predicted number of confirmed cases from the two‐part model and demonstrates more confirmed cases in lower star nursing homes and nursing homes with higher concentrations of sociodemographically disadvantaged residents.
Figure 1.
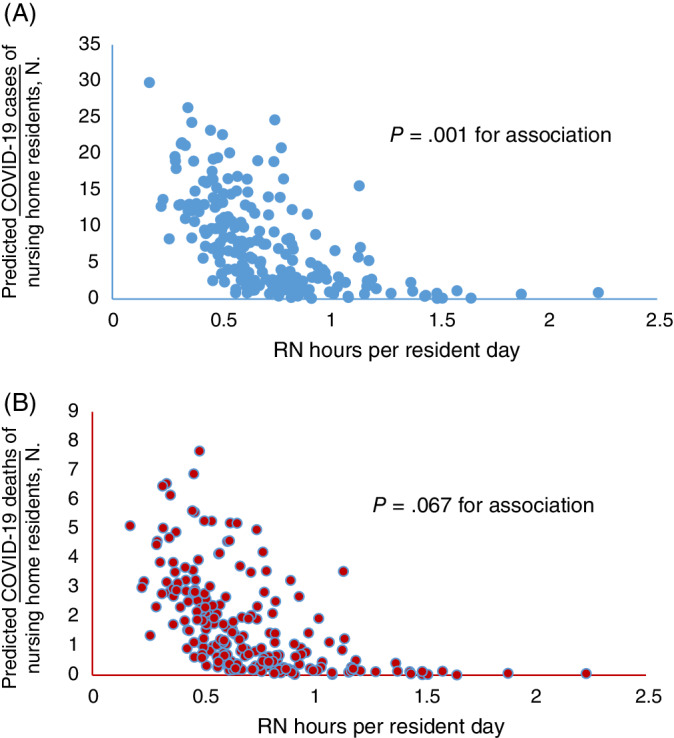
Predicted numbers of COVID‐19 (A) confirmed cases and (B) deaths among Connecticut nursing home residents (as of April 16, 2020) versus registered nurse (RN) staffing hours (P values are for the independent associations of RN staffing with predicted counts that were derived from the joint tests of the two‐part regression models).
Table 3 also shows that these key nursing home characteristics were not significantly associated with the likelihood of one or more COVID‐19 deaths in a nursing home. However, among facilities with at least one death, every 20‐minute increase in RN staffing of the nursing home significantly predicted a 26% reduction in COVID‐19 deaths (IRR = .74; 95% CI = .55–1.00; P = .047). Furthermore, RN staffing level was negatively associated with the overall predicted number of deaths (P = .067 in a joint test of the two‐part model; Figure 1B). Supplementary Figure S2 shows the tendencies of higher predicted numbers of deaths in lower star nursing homes and nursing homes with a higher concentration of sociodemographically disadvantaged residents, although group differences were not statistically significant.
DISCUSSION
By April 16, 2020, COVID‐19 cases had occurred among residents in 50% and deaths in 40% of Connecticut nursing homes. The numbers of confirmed cases and deaths vary substantially over nursing homes, and higher RN staffing is strongly associated with fewer cases and deaths. Nursing homes with lower quality ratings and caring predominantly for Medicaid or racial and ethnic minority residents tend to have more confirmed cases in multivariable analyses. However, current data do not support the hypothesis that these nursing homes have excessively high numbers of confirmed deaths.
Connecticut is among the earliest states to publicly report COVID‐19 cases and deaths in its nursing homes, and Connecticut's report is granular enough to allow for evaluation of variations over facilities. In an effort to fill the information gap for nursing home residents, their families, and policymakers, CMS released guidance on April 19, 2020, requiring nursing homes to report COVID‐19 cases directly to the CDC and to notify residents and their representatives appropriately of conditions at the facilities. 30 Although the federally reported data are not yet available, a study by the Kaiser Family Foundation 10 documented that by April 23, 36 states were reporting some level of data about coronavirus cases and deaths in LTC facilities. The Kaiser study further reported that the LTC facility shares of total COVID‐19 cases and deaths were 11% and 27%, respectively, but varied substantially over states. Our study found that in Connecticut, the nursing home shares of total confirmed cases and deaths are 11% and 39%, respectively, with large variations across counties. Such variations are likely due to multiple factors such as differences in population characteristics, case mix of nursing home residents, and the number of coronavirus tests being performed.
RNs lead almost all aspects of care delivery in nursing homes including the assessment, treatment, and management of resident conditions, and the supervision of other nursing staff (licensed practical nurses and certified nursing assistants). In most nursing homes, RNs are the linchpin for the assessment and provision of medical care including early identification of and response to emergencies and life‐threatening situations. Previous literature on hospital care has demonstrated that increased RN staffing levels are key to the ability of hospitals to respond to outbreaks of emerging infections. 31 Our findings of the strong negative associations between RN staffing and counts of COVID‐19 cases and deaths in nursing homes are consistent with these prior findings, and they highlight the critical role of RNs in dealing with COVID‐19 outbreaks in nursing homes.
In addition to RN and other nurse staffing levels, the CMS five‐star ratings incorporate two other components for nursing home quality of care: deficiency citations and risk‐adjusted quality measures. Deficiency citations represent state surveyors’ evaluations of quality and safety problems in nursing homes, covering a comprehensive list of federal and state standards in clinical and personal care; and quality measures include 15 risk‐adjusted measures of care processes and health outcomes for both long‐stay and short‐stay residents. Our results suggest that nursing homes in better compliance with these multifaceted care standards and performing better in resident‐oriented quality measures are more able to contain the spread of coronavirus among their residents, although their abilities to prevent COVID‐19–related deaths were not found superior compared with other nursing homes.
Disparities in quality of care have long been documented in nursing homes, with consistent evidence showing that facilities caring for disproportionately higher numbers of Medicaid and racial/ethnic minority residents tend to be located in communities of lower socioeconomic status, be financially strained, and have worse resident outcomes. 18 , 19 , 20 , 32 , 33 Thus our finding of the higher cumulative incidences of COVID‐19 infection in these facilities is likely a new manifestation of these long‐standing disparities. In addition, early data suggested less social distancing in lower income neighborhoods, 34 possibly due to the lack of job security and other disadvantages, and a higher COVID‐19 contraction rate among racial minorities. 35 These may also contribute to the disparities in COVID‐19 contractions in nursing homes.
CMS recently released a series of guidelines, focusing on visitor restrictions, infection control policies, and plans on cohorting residents, to combat the surge of COVID‐19 infections and deaths in LTC facilities. Starting in early March, CMS also refocused the on‐site nursing home inspections on compliance with infection control standards. 36 Findings of this study may inform these current and future efforts to better control the epidemic in nursing homes and other LTC facilities. For example, although the CMS refocused inspections initially targeted nursing homes in areas hit earliest by the COVID‐19 pandemic or with known infection control deficiencies, our results suggest that going forward, CMS and state nursing home inspectors may target more broadly those facilities with lower RN staffing levels and lower quality ratings, where transmission of the novel coronavirus is more rapid and deaths are more common. Also, current federal regulations require nursing homes to have an RN on duty at least 8 hours a day and 7 days a week. Although this staffing requirement may be hard to raise nationally, nursing homes able to increase their RN hours should consider doing so for more effective control of COVID‐19 outbreaks.
Furthermore, in the face of the COVID‐19 pandemic, nursing homes caring for more sociodemographically disadvantaged residents may be more likely than other facilities to experience severe shortages of staff, personal protective equipment (PPE), and medical equipment, as well as other issues such as poor testing capacity, delayed diagnosis, lack of access to medical treatment, and high risk of cross‐infection among residents and staff. Thus national and local efforts to bolster healthcare capacity in nursing homes should target these facilities; other supports to mitigate coronavirus transmission in LTC facilities, such as staff training for proper use of PPE, may also target these highly strained facilities.
This study has several limitations. First, our analyses focused on Connecticut nursing homes, and results should be generalized to other states with caution. However, in the current absence of national COVID‐19 data for nursing homes, findings in this study provide timely evidence to inform policies and practices. Second, the observational study design allows for estimation of associations only that may be biased by unmeasured confounders such as number of tests done in the nursing home (likely limited due to insufficient testing capacity in the state) and actual infection control and prevention practices in individual facilities. Finally, the lack of significance in the associations of nursing home star ratings and concentrations of disadvantaged residents with predicted COVID‐19 deaths may reflect insufficient power in multivariable analyses.
In conclusion, nursing homes with higher RN staffing and quality ratings have the potential to better control the spread of the novel coronavirus and reduce deaths. Thus inspections of nursing home infection control practices may target facilities with lower RN staffing and star ratings. Compared with other nursing homes, nursing homes caring predominantly for Medicaid or racial and ethnic minority residents tend to have more COVID‐19 confirmed cases. Efforts to help nursing homes combat the COVID‐19 pandemic should prioritize these facilities.
Supporting information
Supplementary Figure S1: Proportions of (A) COVID‐19 confirmed cases and (B) deaths who were nursing home residents by county of Connecticut, as of April 16, 2020.
Supplementary Figure S2: Predicted numbers of (A) COVID‐19 confirmed cases and (B) deaths among Connecticut nursing home residents (as of April 16, 2020) versus nursing home five‐star ratings, high versus low concentration of Medicaid residents, and high versus low racial and ethnic minority residents in the nursing home (P values are for the independent associations of nursing home categories with predicted counts that were derived from the joint tests of the two‐part regression models).
Supplementary Table S1: Full Model Results.
ACKNOWLEDGMENTS
Conflict of Interests
The authors have declared no conflicts of interest for this article.
Author Contributions
Conception and design, acquisition of data, analysis and interpretation of data, drafting of article, critical revision for important intellectual content, and final approval of version to be published: Li, Temkin‐Greener, and Cai. Acquisition of data, analysis and interpretation of data, and final approval of version to be published: Shan.
Sponsor's Role
The research of the authors was funded by the National Institutes of Health (NIH) under Grant No. R01MH117528 and the Agency for Healthcare Research and Quality (AHRQ) under Grant Nos. R01HS026893 and R01HS024923. The views expressed in this article are those of the authors and do not necessarily represent the view of the NIH or the AHRQ. The NIH and the AHRQ had no role in study design, data collection, analyses, or interpretation of results.
REFERENCES
- 1. World Health Organization . Coronavirus disease (COVID‐2019) situation reports. Coronavirus disease 2019 (COVID‐19), 28 April 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed April 29, 2020.
- 2. Lansbury LE, Brown CS, Nguyen‐Van‐Tam JS. Influenza in long‐term care facilities. Influenza Other Respi Viruses. 2017;11(5):356‐366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hand J, Rose EB, Salinas A, et al. Severe respiratory illness outbreak associated with human coronavirus NL63 in a long‐term care facility. Emerg Infect Dis. 2018;24(10):1964‐1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City area. JAMA. 2020;323(20):2052‐2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Myers LC, Parodi SM, Escobar GJ, Liu VX. Characteristics of hospitalized adults with COVID‐19 in an integrated health care system in California. JAMA. 2020;323(21):2195‐2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McMichael TM, Currie DW, Clark S, et al. Epidemiology of Covid‐19 in a long‐term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005‐2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS‐CoV‐2 infections in residents of a long‐term care skilled nursing facility—King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Roxby AC, Greninger AL, Hatfield KM, et al. Detection of SARS‐CoV‐2 among residents and staff members of an independent and assisted living community for older adults—Seattle, Washington, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(14):416‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kaiser Family Foundation (KFF). State reporting of cases and deaths due to COVID‐19 in long‐term care facilities. https://www.kff.org/medicaid/issue‐brief/state‐reporting‐of‐cases‐and‐deaths‐due‐to‐covid‐19‐in‐long‐term‐care‐facilities/?utm_campaign=KFF‐2020‐Medicaid&utm_source=hs_email&utm_medium=email&utm_content=2&_hsenc=p2ANqtz‐_g3x0lLoESTRe6UgazNM0z81iW3Vn2rGNK1CDP4D4ifzyzh3tuGLqWllBYM2IqaJi_T63Qg3862U‐XrCj9e_td7vKMEg&_hsmi=2. Accessed April 23, 2020.
- 11. Harrington C, Kovner C, Mezey M, et al. Experts recommend minimum nurse staffing standards for nursing facilities in the United States. Gerontologist. 2000;40(1):5‐16. [DOI] [PubMed] [Google Scholar]
- 12. Harrington C, Olney B, Carrillo H, Kang T. Nurse staffing and deficiencies in the largest for‐profit nursing home chains and chains owned by private equity companies. Health Serv Res. 2012;47(1 pt 1):106‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Konetzka RT, Stearns SC, Park J. The staffing‐outcomes relationship in nursing homes. Health Serv Res. 2008;43(3):1025‐1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Harrington C, Choiniere J, Goldmann M, et al. Nursing home staffing standards and staffing levels in six countries. J Nurs Scholarsh. 2014;44(1):88‐98. [DOI] [PubMed] [Google Scholar]
- 15. Temkin‐Greener H, Cai S, Zheng NT, Zhao H, Mukamel DB. Nursing home work environment and the risk of pressure ulcers and incontinence. Health Serv Res. 2012;47(3 pt 1):1179‐1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Li Y, Cen X, Cai X, Temkin‐Greener H. Perceived patient safety culture in nursing homes associated with “Nursing Home Compare” performance indicators. Med Care. 2019;57(8):641‐647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cho E, Kim IS, Lee TW, Kim GS, Lee H, Min D. Effects of registered nurse staffing on quality of care and resident outcomes in nursing homes. Geriatr Nurs. 2020. [DOI] [PubMed] [Google Scholar]
- 18. Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227‐256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li Y, Mukamel DB. Racial disparities in receipt of influenza and pneumococcus vaccinations among US nursing‐home residents. Am J Public Health. 2010;100(suppl 1):S256‐S262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Li Y, Harrington C, Temkin‐Greener H, et al. Deficiencies in care at nursing homes and racial/ethnic disparities across homes fell, 2006–11. Health Aff (Millwood). 2015;34(7):1139‐1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Konetzka RT, Grabowski DC, Perraillon MC, Werner RM. Nursing home 5‐star rating system exacerbates disparities in quality, by payer source. Health Aff (Millwood). 2015;34(5):819‐827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rivera‐Hernandez M, Rahman M, Mor V, Trivedi AN. Racial disparities in readmission rates among patients discharged to skilled nursing facilities. J Am Geriatr Soc. 2019;67(8):1672‐1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Li Y, Yin J, Cai X, Temkin‐Greener J, Mukamel DB. Association of race and sites of care with pressure ulcers in high‐risk nursing home residents. JAMA. 2011;306(2):179‐186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. NBC Connecticut . Coronavirus outbreak: This is where there are confirmed cases of COVID‐19 in CT nursing homes. https://www.nbcconnecticut.com/news/local/this-is-where-there-are-confirmed-cases-of-covid-19-in-ct-nursing-homes/2256775/. Published April 16, 2020. Updated April 16, 2020.
- 25. Centers for Medicare and Medicaid Services . Nursing Home Compare. https://www.medicare.gov/nursinghomecompare/Data/About.html. Accessed April 29, 2020.
- 26. Geng F, Stevenson DG, Grabowski DC. Daily nursing home staffing levels highly variable, often below CMS expectations. Health Aff (Millwood). 2019;38(7):1095‐1100. [DOI] [PubMed] [Google Scholar]
- 27. Centers for Medicare and Medicaid Services . Design for Nursing Home Compare Five‐Star Quality Rating System, Technical Usersʼ Guide. April 2018. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/downloads/usersguide.pdf. Accessed April 29, 2020.
- 28. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929‐936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cameron AC, Trivedi PK. Regression Analysis of Count Data. 2nd ed. Cambridge, UK: Cambridge University Press; 2013. [Google Scholar]
- 30. CMS. Center for Clinical Standards and Quality/Quality, Safety & Oversight Group . Upcoming requirements for notification of confirmed COVID‐19 (or COVID19 persons under investigation) among residents and staff in nursing homes. April 19, 2020. https://www.cms.gov/files/document/qso-20-26-nh.pdf. Accessed April 29, 2020.
- 31. Stone PW, Clarke SP, Cimiotti J, Correa‐de‐Araujo R. Nursesʼ working conditions: implications for infectious disease. Emerg Infect Dis. 2004;10(11):1984‐1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li Y, Glance LG, Yin J, Mukamel DB. Racial disparities in rehospitalization among Medicare patients in skilled nursing facilities. Am J Public Health. 2011;101(5):875‐882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Li Y, Cai XY, Harrington C, et al. Racial and ethnic differences in the prevalence of depressive symptoms among US nursing home residents. J Aging Soc Policy. 2019;31(1):30‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Valentino‐DeVries J, Lu D, Dance G. Location data says it all: staying at home during coronavirus is a luxury. New York Times. April 3, 2020. https://www.nytimes.com/interactive/2020/04/03/us/coronavirus-stay-home-rich-poor.html. Accessed April 29, 2020.
- 35. Yancy CW. COVID‐19 and African Americans. JAMA. 2020;323(19):1891‐1892. 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 36. CMS Center for Clinical Standards and Quality/Quality, Safety & Oversight Group . Suspension of survey activities. March 4, 2020. https://www.cms.gov/files/document/qso-20-12-allpdf.pdf-1. Accessed April 29, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure S1: Proportions of (A) COVID‐19 confirmed cases and (B) deaths who were nursing home residents by county of Connecticut, as of April 16, 2020.
Supplementary Figure S2: Predicted numbers of (A) COVID‐19 confirmed cases and (B) deaths among Connecticut nursing home residents (as of April 16, 2020) versus nursing home five‐star ratings, high versus low concentration of Medicaid residents, and high versus low racial and ethnic minority residents in the nursing home (P values are for the independent associations of nursing home categories with predicted counts that were derived from the joint tests of the two‐part regression models).
Supplementary Table S1: Full Model Results.


