Abstract
Background
Our objective was to quantify trends in emergency medical services (EMS) incidents as the effects of the COVID‐19 pandemic spread across the United States and to determine if there was an increase in EMS‐attended deaths.
Methods
We conducted a 3‐year comparative retrospective cohort analysis of data from the National EMS Information System. Data were included if care was provided between the 40th and 21st weeks of the next year and compared over 3 years. We included incidents identified through 9‐1‐1 where patient contact was made. The total number of EMS incidents per week was used as the denominator to calculate the rate of patient deaths and possible injury. We assessed for temporal and seasonal trends.
Results
Starting in the 10th week of 2020 there was a decrease in the number of EMS activations in the United States compared to the prior weeks and the same time period in previous years. The number of activations between week 10 and week 16 decreased by 140,292 or 26.1%. The portion of EMS activations reporting a patient disposition of death nearly doubled between the 11th and 15th weeks of 2020 (1.49%–2.77% of all activations). The number of EMS activations documenting a possible injury decreased from 18.43% to 15.27% between weeks 10 and 13.
Conclusion
We found that early in the COVID‐19 outbreak there was a significant decrease in the number of EMS responses across the United States. Simultaneously the rate of EMS‐attended death doubled, while the rate of injuries decreased.
The effects of the coronavirus disease 2019 (COVID‐19) pandemic on different aspects of the U.S. healthcare system are evolving and emerging in the literature. These effects are presumed to be directly or indirectly related to COVID‐19, including massive efforts to slow the spread of the disease. Specifically, efforts were made to decrease how rapidly the virus infected the population to avoid placing too high a burden on the health care system, which could have resulted in an inability to meet the demand for care. This message was explained in the popular media as an effort to “flatten the curve.”
As communities began to implement social distancing interventions including “stay‐at‐home” orders and messaging the concept that we had to work together to reduce the spread of the virus to decrease the burden on the health care system, certain social patterns began to emerge. Patient visits to emergency departments (EDs) began dramatically trending downward. 1 The National Syndromic Surveillance Program found that from the 11th week of 2020 (March 9–15) to the 14th week (March 30–April 5) ED visits dropped from just over 2.5 million to 1.2 million. 2 Even in the region that includes New York, New Jersey, and Puerto Rico, ED visits went from 223,489 to 144,249 during that same time period. 2 Simultaneously, in New York, there were three deaths attributed to COVID‐19 in week 11 and 3,194 in week 14, while in New Jersey the number of deaths was 2 in week 11 and 756 in week 14 (data on Puerto Rico were not available). 3 Anecdotally, emergency physicians and other emergency care providers reported fewer patient visits, but higher patient acuity in the United States. 4 These reports were supported in other countries where they too saw a drop in ED visits. 5 , 6 , 7
Very limited information is available on the effect of the pandemic on the emergency medical services (EMS) system. In particular, it is unknown if there has been a similar decrease in patient encounters for prehospital care providers. Anecdotal reports suggest that EMS was responding to increasing numbers of out‐of‐hospital cardiac arrest cases in areas hard hit by the COVID‐19 outbreak. 8 This suggestion is concerning and corroborates reports of declining ED visits, since it may be a sign of the detrimental effects of citizens with emergent conditions not seeking timely emergency care and/or possibly a direct effect of COVID‐19 infection. If confirmed, such a finding could be the result of the virus going undetected in such situations, as some communities have reported that medical examiners have limited access to testing for COVID‐19 in deceased patients. 9 If communities are not testing deceased patients, we may not know the full scope of the effect that the virus is having on our communities. The objective of this paper was to quantify the trends in national EMS incidents as the effects of the pandemic spread across the United States, using absolute numbers of EMS activations, activation rates, and types of EMS incidents. We also sought to determine if there was an increase in the number of EMS attended on‐scene deaths, as has been reported in the popular media. 10
Methods
We conducted a 3‐year comparative retrospective cohort analysis of data submitted to the National Emergency Medical Services Information System (NEMSIS) database. NEMSIS populates a National EMS registry including standardized patient care records (PCRs) submitted by upwards of 10,000 EMS agencies across 47 states and territories in near real time. Transmission of data to the national EMS registry is automated in most systems so that once a PCR is completed, the record populates the associated state and national registries automatically. This project was designated as being exempt from institutional review board review at the State University of New York at Buffalo in Buffalo, NY.
Patient care record data were included for study if patient care was provided by EMS providers between the 40th week of 2017 (October 2‐8) and the 21st week of 2020 (May 18–24, 2020). The 40th week in a year was chosen as the study initiation period to preempt the beginning of the traditional flu season for any given year. For this study, time period 1 included PCRs from the 40th week of 2017 through the 21st week of 2018. Time period 2 included PCRs from the 40th week of 2018 through the 21st week of 2019. Time period 3 includes PCRs submitted from the 40th week of 2019 through the 21st week of 2020. These three study time periods allowed us to evaluate trends over time and to compare those trends to prior years to control for normal seasonal variation.
We analyzed all national EMS data that were available in the National EMS Database repository on June 3, 2020. Data were abstracted from the NEMSIS system at the NEMSIS Technical Assistance Center. EMS responses were included if the request for aid originated through the area's emergency system (i.e., 9‐1‐1) and patient contact was documented. Patient transfers from one facility to another and nonemergent requests for private transport were excluded from the analysis.
The total number of EMS incidents per week were determined for each of the study time periods. We then used this number as the denominator to determine the rate (i.e., percentage) of specific EMS activation types per week. Documentation of patient deaths was based on a NEMSIS patient disposition variable (i.e., eDisposition.12 [Incident/Patient Disposition]) by combining patients who were identified as dead for whom resuscitation was either attempted or not and transportation was provided to a hospital or not. We included EMS responses for which a possible injury was documented as a concurrent comparison group, which is a common reason for EMS activations 11 and, hypothetically, should substantiate our approach, by demonstrating an opposite effect, due to stay‐at‐home orders. Potential injury incidents were identified using the NEMSIS element eSituation.02 (Possible Injury).
Data Analysis
We analyzed data using descriptive statistics. In the National EMS Database repository, PCRs are provided by all EMS units responding to a request for service. Thus, if multiple units are dispatched to the same event, more than one PCR will be submitted to the national repository. We focused on week‐to‐week comparisons for a defined period over several years to assess temporal and seasonal trends. Confidence bands around weekly rates are not provided, since the large number of EMS activations associated with these analyses made them nearly indistinguishable from the reported value.
Results
The overall study time frame included 37,550,949 9‐1‐1–initiated EMS activations resulting in patient contact. Time period 1 includes 8,621,423 EMS activations. Time period 2 includes 13,387,829 EMS activations. Time period 3 includes 15,541,697 EMS activations. Figure 1 illustrates that starting in the 10th week of 2020 (March 2–8) there was a precipitous decrease in the number of 9‐1‐1–initiated EMS activations in the United States compared to the prior weeks and the same time period in previous years. The weekly call volume decreased by 140,292 activations or (26.1%), comparing week 10 of 2020 to week 16.
Figure 1.
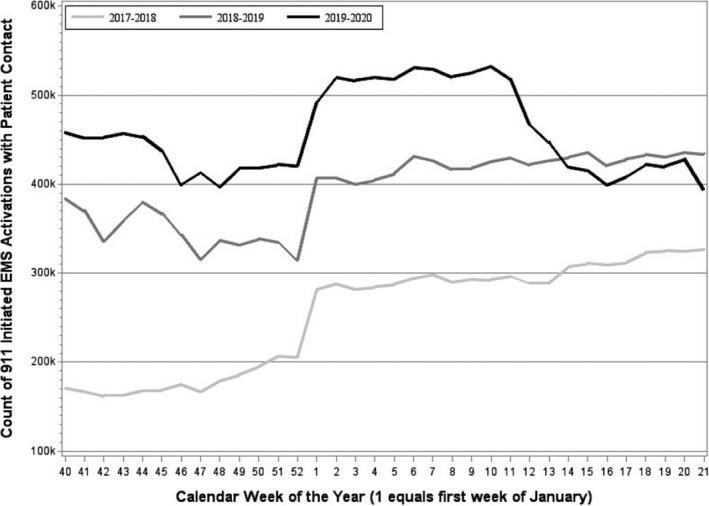
Comparison of the weekly number of 9‐1‐1–initiated EMS activations with patient contact from 2017 to 2020. The number of states submitting to the national EMS repository increased over the study period (2017, 32 states; 2018, 40 states; 2019, 44 states). The District of Columbia submitted PCRs in each time period. States enrolling in the National EMS repository commonly begin submitting PCRs at the beginning of the calendar year. No state stopped submitting PCRs once enrolled. PCR = patient care record.
The portion of EMS activations reporting a patient disposition of death at the scene remained fairly consistent until the 11th week of 2020 (March 9–15), at which point the proportion of scene deaths nearly doubled, increasing from 1.49% to 2.77% among all EMS activations with patient contact by week 15 (Figure 2). Examining the raw numbers of EMS‐attended scene deaths reported in 2020, the number increases from 6,294 in week 11 to 8,942 in week 15. Conversely, the proportion of patients attended by EMS for which a potential injury is reported demonstrates an opposing trend for EMS activations, falling from 18.43% in week 10 of 2020 to 15.27% in week 13, with the actual number of EMS activations trending downward for this 3‐week period from 98,487 to 66,593 (Figure 3).
Figure 2.
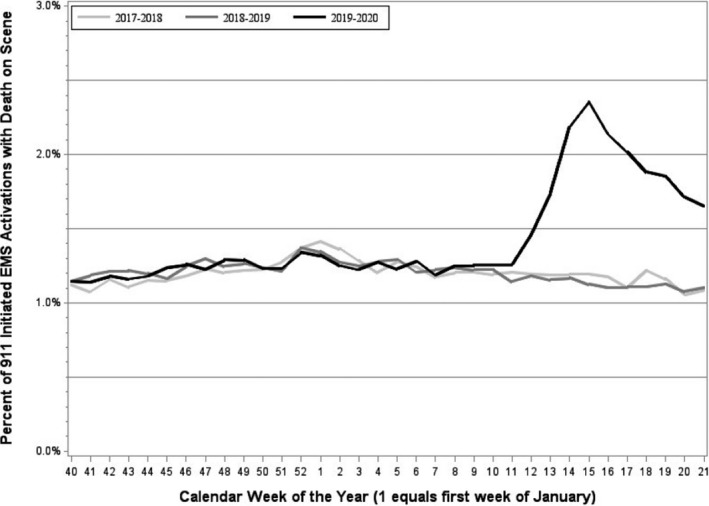
The percentage of 9‐1‐1–initiated EMS activations with patient.
Figure 3.
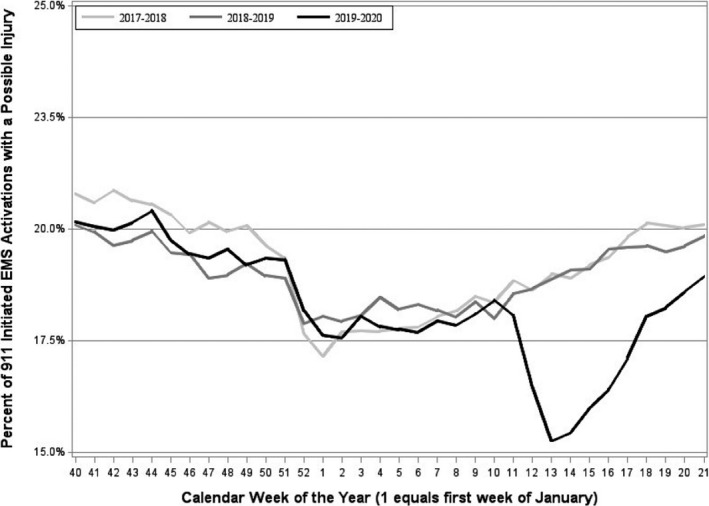
The percentage of 9‐1‐1–initiated EMS activations with patient contact that document a possible injury.
Discussion
In this study, we found that EMS activations initiated through the emergency response system and resulting in a patient contact declined rapidly since COVID‐19 cases were first identified in the United States and social distancing measures were enacted. Further, there has been an increase in the percentage of EMS‐attended scene deaths compared to prior weeks during similar time periods in previous years. This is in contrast to EMS activations reporting potential injuries, which decreased during the time frame representing the COVID‐19 infection. These findings have both public health and economic implications for the U.S. emergency response system.
From a public health perspective, these findings suggest that individuals are not accessing the emergency medical system with the same frequency as experienced prior to the spread of COVID‐19. While some of our findings could be explained by the lifestyle changes related to stay‐at‐home orders, such as driving less and participating in less risky recreational activities (i.e., fewer injuries), the decrease in EMS activations is likely not entirely explained by societal changes implemented in response to COVID‐19. It is possible that changes in social perceptions (i.e., fear of infection) may explain our observed increase in the frequency of scene deaths attended by EMS. Recent publications have documented a decrease in the number of patients presenting to hospitals for acute coronary syndromes during the initial months of the pandemic in the United States, Spain, and Australia. 12 , 13 , 14 , 15 Further, over a third of patients who delayed presenting for care of their myocardial infarction cited fear of COVID‐19 or not wanting to burden the hospital as a reason for their delay. 15 This phenomenon appears to be affecting EDs and EMS systems in the United States, which could be a positive consequence if people whose medical needs do not require those services are seeking other avenues for care. However, our finding of a doubling in the rate of EMS attended deaths suggests that people who are experiencing medical emergencies are not accessing timely care. This conclusion is supported by a publication from Portugal that found an excess number of deaths that were not entirely explained by the reported fatalities due to COVID‐19. 16 As well as in Italy where they too saw an increase in cardiac arrests. 17
Changes in EMS call volume and case mix can have significant negative effects on EMS providers, especially if patient needs become more significant and urgent. More severely ill patients require EMS professionals to provide more technically complex care and increased exposure to high‐stress situations related to patients not seeking early care for treatable conditions. These cases place additional stress and anxiety on EMS professionals, potentially resulting in long‐term negative consequences to the health, well‐being, and longevity of these important frontline responders. 18
It is also important to consider the economic implications of changing EMS volumes. EMS agencies must schedule units so that there is always additional capacity to respond to the next call. That is, if all EMS units are responding to individual patients at the same time there will be no capacity in the system for the next emergency. However, if too many units are idle then the community's cost of maintaining the EMS system becomes too high to sustain the service since many agencies only earn revenue when they treat and transport patients. Most EMS agencies are required to have a certain number of units in service to meet contractual obligations or due to geographic factors related to response time requirements across the service area. A drop in call volume will result in agency costs that are likely flat, while agency revenues significantly decline, leading to EMS budgetary shortfalls that will be difficult to recover from. The ability of EMS to quickly and efficiently respond to future emergencies could be jeopardized.
While our reported findings may adjust over time, it will be important to consider how public health messaging regarding the potential burden on health care systems and fears about contracting a novel virus may affect community member's decision to access care. In future outbreaks and other public health emergencies, it will be important to balance the need for people to seek and receive needed care with the requirement for communities to implement practices (such as social distancing) that are meant to address and contain an emerging threat.
Limitations
This study is limited by the expansion of states participating in NEMSIS during the time frame that was studied. During the study period, the number of states contributing data to the NEMSIS expanded from 32 to 44. States enrolling in the National EMS Database repository commonly begin submitting PCRs at the beginning of the calendar year (Figure 1). No states began submissions to the National EMS Database repository during the COVID‐19 pandemic. With that expansion, the expectation is that the number of EMS activations per week would increase from year to year. Instead, we found fewer activations from week 10 through week 17 of 2020, during the period of COVID‐19 community spread compared to the weeks preceding it and the same weeks in the prior time periods. Another potential limitation is that the analysis is based on EMS unit activations rather than individual patients. In some cases, multiple records may have been completed for the same patient. However, this limitation applies to all years of PCRs submitted to NEMSIS and can therefore be considered consistent across the three time periods. It is unknown what affect the pandemic may have had on the number of units responding to a scene. We could expect to see the practice of multiple responding units potentially decrease for responses during the pandemic to limit the number of responders and reduce exposure, as was recommended by the American Heart Association during week 15 of 2020. 19 This would result in an opposite effect than that observed, but this assumption cannot be evaluated with the available data so there also may have been an increase in the number of units responding to each patient.
In some areas of the U.S. EMS data are submitted to NEMSIS with a defined lag period to promote data validity. This analysis was done in the 23rd week of 2020. It is possible that some data were not yet submitted, which may affect the activation rates reported for scene deaths and patients with potential injuries. However, the use of a rate (or proportion) should minimize the impact of this potential bias. There is no obvious reason why EMS responders would systematically withhold (or accelerate) the submission of specific types of EMS activations.
Conclusion
We found that early in the COVID‐19 outbreak there was a significant decrease in the number of emergency medical services responses across the United States. Simultaneously the rate of emergency medical services–attended scene death doubled, while the rate of emergency medical service activations related to patient injury decreased.
The authors recognize the analytical support provided by Mengtao Dia and Chris Hoffman and thank all participating EMS clinicians, EMS agencies, and state EMS offices who provided data to the NEMSIS National Database and delivered patient care during this very difficult time in U.S. history.
Academic Emergency Medicine 2020;27:693–699.
This project was supported by a contract with the National Highway Traffic Safety Administration, Office of Emergency Medical Services (DTNH‐22‐15‐C‐00030). This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $2,799,974 with 0% financed with nongovernmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by, HRSA, HHS, or the U.S. Government.
The authors have no potential conflict of interest to disclose.
Author contributions: EBL—study concept and design, interpretation of the data, drafting of the manuscript, and acquisition of funding; CDN—study concept and design, interpretation of the data, and critical revision of the manuscript for important intellectual content; and NCM—study concept and design, acquisition of the data, analysis and interpretation of the data, critical revision of the manuscript for important intellectual content, and acquisition of funding.
References
- 1. Hartnett KP, Kite‐Powell A, DeVies J, et al. Impact of the COVID‐19 Pandemic on Emergency Department Visits – United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Syndromic Surveillance Program (NSSP): Emergency Department Visits Percentage of Visits for COVID‐19‐Like Illness (CLI) or Influenza‐like Illness (ILI) September 29, 2019 – April 4, 2020 Data as of April 9, 2020. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/04102020/nssp-regions.html. Accessed May 7, 2020.
- 3. COVID‐19 Projections. Available at: https://covid19.healthdata.org. Accessed May 7, 2020.
- 4. Rosenbaum L. The untold toll – The pandemic's effects on patients without Covid‐19. N Engl J Med 2020;382:2368–71. [DOI] [PubMed] [Google Scholar]
- 5. Mantica G, Riccardi N, Terrone C, Gratarola A. Non‐COVID‐19 visits to emergency departments during the pandemic: the impact of fear. Public Health 2020;183:40–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet Child Adolesc Health 2020;4:e10–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thornton J. Covid‐19: A&E visits in England Fall by 25% in week after lockdown. BMJ 2020;369:m1401. [DOI] [PubMed] [Google Scholar]
- 8. NYC Cardiac Calls Skyrocket as Coronavirus Fear Grips City. NY Daily News. Available at: https://www.nydailynews.com/coronavirus/ny-coronavirus-cardiac-calls-jump-in-the-city-20200407-tzlxcqaqs5a2flpnlmhsffnyjm-story.html. Accessed May 7, 2020. [Google Scholar]
- 9. Coroners Worry Covid‐19 Test Shortages Could Lead to Uncounted Deaths. Available at: https://www.cnn.com/2020/04/06/health/coronavirus-coroners-uncounted-deaths-invs/index.html. Accessed May 7, 2020.
- 10. Nearly a Third of Americans Have Put Off Healthcare During COVID‐19. Modern Healthcare. Available at: https://www.modernhealthcare.com/patient-care/nearly-third-americans-have-put-healthcare-during-covid-19. Accessed May 7, 2020.
- 11. Mann NC, Kane L, Dai M, Jacobson K. Description of the 2012 NEMSIS public‐release research dataset. Prehospital Emerg Care 2015;19:232–40. [DOI] [PubMed] [Google Scholar]
- 12. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST‐segment elevation cardiac catheterization laboratory activations in the United States during COVID‐19 pandemic. J Am Coll Cardiol 2020;75:2871–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID‐19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020;41:1852–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rodríguez‐Leor O, Cid‐Álvarez B, Ojeda S, et al. Impact of the COVID‐19 pandemic on interventional cardiology activity in Spain. REC: Interventional Cardiol 2020;2:82–9. [Google Scholar]
- 15. Hammad TA, Parikh M, Tashtish N, et al. Impact of COVID‐19 pandemic on ST‐elevation myocardial infarction in a non‐COVID‐19 epicenter. 2020. [early online]. doi: 10.1002/ccd.28997 [DOI] [PMC free article] [PubMed]
- 16. Nogueira PJ, Nobre MA, Nicola PJ, Furtado C, Vaz Carneiro A. Excess mortality estimation during the COVID‐19 pandemic: preliminary data from Portugal. Acta Med Port 2020;33:376–83. [DOI] [PubMed] [Google Scholar]
- 17. Baldi E, Sechi GM, Mare C, et al. Out‐of‐hospital cardiac arrest during the Covid‐19 outbreak in Italy. N Engl J Med 2020. [early online]. doi: 10.1056/NEJMc2010418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Caulkins CG. Psychological trauma: the silent stalker. J Emerg Med Serv 2018; online only. Available at: https://www.jems.com/2018/09/17/psychological-trauma-the-silent-stalker/. Accessed Jun 26, 2020. [Google Scholar]
- 19. Edelson DP, Sasson C, Chan PS, et al. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID‐19: From the Emergency Cardiovascular Care Committee and Get With the Guidelines®‐Resuscitation Adult and Pediatric Task Forces of the American Heart Association in Collaboration With the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, The Society of Critical Care Anesthesiologists, and American Society of Anesthesiologists: Supporting Organizations: American Association of Critical Care Nurses and National EMS Physicians. Circulation 2020. [early online]. doi: 10.1161/CIRCULATIONAHA.120.047463 [DOI] [PMC free article] [PubMed] [Google Scholar]


