Abstract
Millions of people were infected with the coronavirus disease 2019 (COVID‐19) all over the world. Data on clinical symptoms of pediatric inpatients with COVID‐19 infection were unclear. The aim of study was to investigate the clinical features of pediatric inpatients with severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection. PubMed, EMBASE, and the Cochrane Library were searched to seek for studies providing details on pediatric inpatients with SARS‐CoV‐2 infection which were published from 1st January to 21st April 2020. Studies with more than five pediatric inpatients were included in our meta‐analysis.This study was registered in the PROSPERO database (CRD42020183550). As the results shown, fever (46%) and cough (42%) were the main clinical characters of pediatric inpatients with SARS‐CoV‐2 infection and the other clinical characters, such as diarrhea, vomiting, nasal congestion, and fatigue account for 10% in pediatric inpatients. The proportion of asymptomatic cases was 0.42 (95% confidence interval [CI]: 0.27‐0.59) and severe cases was 0.03 (95% CI: 0.01‐0.06). For the laboratory result, leukopenia (21%) and lymphocytosis (22%) were the mainly indicators for pediatric inpatients, followed by high aspartate aminotransferase (19%), lymphopenia (16%), high alanine aminotransferase (15%), high C‐reactive protein (17%), leukocytosis (13%), high D‐dimer (12%) and high creatine kinase‐MB (5%). Regard to chest imaging features, unilateral and bilateral accounts for 22% in pediatric inpatients, respectively. In conclusion, compared with adult inpatients with SARS‐CoV‐2 infection, the pediatric inpatients had mild clinical characters, lab test indicators, and chest imaging features. More clinical studies focus on the pediatric patients with SARS‐CoV‐2 infection in other countries should be conducted.
Keywords: children, clinical features, coronavirus, COVID‐19, SARS‐CoV‐2 infection
Highlights
The clinical features of pediatric inpatients with SARS‐CoV‐2 infection were investigated
Fever and cough were the main clinical characters of pediatric inpatients with SARS‐CoV‐2 infection.
The pediatric inpatients had mild clinical characters, lab test indicators, and chest imaging features compared to the adult inpatients with SARS‐CoV‐2 infection.
1. INTRODUCTION
In December 2019, a new coronavirus pneumonia outbreak in Wuhan city, Hubei Province and rapidly spread across China, and the disease break out in the most countries or regions subsequently. 1 , 2 The World Health Organization has named the novel coronavirus as coronavirus disease 2019 (COVID‐19) and declared COVID‐19 as a pandemic for global health emergency. 1 Generally, the COVID‐19 is less severe and less fatal than the severe acute respiratory syndrome (SARS), furthermore, the elderly SARS‐coronavirus 2 (SARS‐CoV‐2) infection patients are prone to develop more severe symptoms and need more emergent medical resources. 3 , 4
Children are more susceptible to the pneumonia than adults, which may cause the fatal results. Previous studies demonstrated that children were less infected by Middle East respiratory syndrome (MERS) and SARS due to the strict transmission route of MERS and the short‐term epidemic of SARS. In addition, almost all the children were at their home during the festival holiday when the COVID‐19 outbreak, which could protected them from the exposure to the COVID‐19. Except low exposure, lower susceptibility for SARS‐CoV‐2 infection of children might due to the lower detectable rate as the mild and atypical presentations of the infection in the children. 5 Therefore, the amount of pediatric inpatients with SARS‐CoV‐2 infection were less than the adult inpatients with SARS‐CoV‐2 infection. 6 , 7
Since the breakout of COVID‐19, abundant studies have been reported that focus on the demographics, clinical characters, lab indicators, and computed tomography (CT) imaging features of the adult inpatients with SARS‐CoV‐2 infection, 3 , 8 and these characters have been pooled and summarized in several meta‐analyses. 8 , 9 , 10 But owing to the limited pediatric cases with SARS‐CoV‐2 infection, only two systematic reviews with simple analysis that focused on pediatric COVID‐19 were reported. 11 , 12 Therefore, the accurate description of the clinical characteristics of pediatric COVID‐19 are needed urgently to guide the clinical diagnosis and treatment for the children that potential infected with SARS‐CoV‐2. As far as we know, this is the first meta‐analysis that investigated the demographics, clinical characters, lab indicators, and CT imaging features of the pediatric inpatients with SARS‐CoV‐2 infection comprehensively.
2. MATERIALS AND METHODS
2.1. Search strategy and study selection
PubMed, Cochrane Library, and Embase were used to perform the literature search according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses process. The search was concluded until to 21 April 2020, and only English studies were involved in our meta‐analysis. Combination of the following keywords were used in the literature search for the search strategy: 2019 novel coronavirus pneumonia; COVID‐19; coronavirus; SARS‐CoV‐2; Wuhan coronavirus; child; 2019 novel coronavirus pneumonia; pediatric; children.
2.2. Inclusion and exclusion criteria
Inclusive criteria: (a) Research types: observational study and case series; (b) Research subjects: pediatric inpatients with SARS‐CoV‐2 infection, only the pediatric inpatients diagnosed by nucleic acid testing were involved in our meta‐analysis; (c) Data items: including demographical features, clinical characteristics, laboratory indicators, or chest imaging signs. Exclusive criteria: (a) review; (b) studies with less than five children patients; (c) absence of the above case data.
2.3. Data extraction and quality assessment
Information including the first author, publication time, sample size, country, research type were extracted from each study, and the demographical features, clinical characteristics, laboratory indicators, and chest imaging signs in all of the pediatric patients were pooled for the meta‐analysis. The quality of the included studies was assessed independently by two investigators (Xuefeng Ma and Shousheng Liu) according to the Institute of Health Economics scale. 13 The discrepancy was resolved by discussion with all investigators. The district and research period of each study were analyzed to avoid the possible overlap of patients' population from different studies.
2.4. Statistical analysis
Statistical heterogeneity among studies was assessed by Q and I 2 statistics. For the Q statistic, heterogeneity was considered to be present when P < .1 or I 2 > 50%. The fixed‐effect model was used when literature heterogeneity did not exist; otherwise, the random‐effect model was used. The metaphor (version 2.0‐0) and meta (version 4.9‐5) packages of R (version 3.6.1) were used to conduct the statistical analysis. 14
2.5. Study registration
This study was registered as CRD42020183550 in the PROSPERO database (University of York, UK; http://www.crd.york.ac.uk/PROSPERO/).
3. RESULTS
3.1. Literature inclusion and characteristics
A total of 545 potentially relevant studies were identified from the database. After removed the animal studies, reviews, nontopic studies, comments, and irrelevant resources, 84 potentially relevant studies were left for further evaluation. After the full‐text evaluation, 15 studies 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 were included in this systematic review and meta‐analysis (Figure 1). Among these studies, 13 studies 16 , 17 , 19 , 20 , 21 , 22 , 23 , 24 , 27 , 28 , 29 were retrospective studies and two studies 15 , 18 were case report (Table 1).
Figure 1.
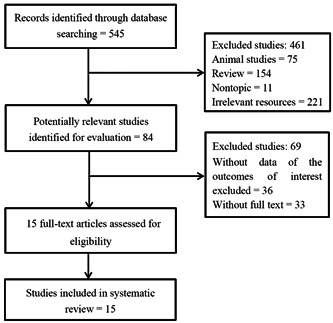
Flow chart of the literature search process
Table 1.
The characteristics of the included literatures
| Study | Year | Country | No. patients | Sex (male) | Research type | Quality |
|---|---|---|---|---|---|---|
| Cai et al 15 | 2020 | China | 10 | 4 | Case series | 5 |
| Sun et al 23 | 2020 | China | 8 | 6 | Observational study | 6 |
| Zheng et al 28 | 2020 | China | 25 | 14 | Observational study | 6 |
| Qiu et al 21 | 2020 | China | 36 | 23 | Observational study | 5 |
| Zhu et al 29 | 2020 | China | 10 | 8 | Observational study | 6 |
| Feng et al 17 | 2020 | China | 15 | 5 | Observational study | 5 |
| Su et al 22 | 2020 | China | 9 | 3 | Observational study | 6 |
| Yang et al 27 | 2020 | China | 7 | 4 | Observational study | 6 |
| Wang et al 25 | 2020 | China | 31 | NA | Observational study | 6 |
| Du et al 16 | 2020 | China | 14 | 6 | Observational study | 6 |
| Li et al 18 | 2020 | China | 5 | 4 | Case Series | 4 |
| Xia et al 26 | 2020 | China | 20 | 13 | Observational study | 5 |
| Su et al 22 | 2020 | China | 171 | 104 | Observational study | 5 |
| Ma et al 20 | 2020 | China | 115 | 73 | Observational study | 5 |
| Tan et al 24 | 2020 | China | 10 | 3 | Observational study | 6 |
Abbreviation: NA, not available.
3.2. Demographical and clinical characteristics
The demographical and clinical characteristics were analyzed according to the included studies. As the results shown, the ratio of male to female was 1.64 (95% confidence interval [CI]: 0.95‐2.83) in pediatric inpatients with SARS‐CoV‐2 infection with the heterogeneity of 62% (P < .01) (Table 2). The proportion of most common clinical characters were 0.42 (95% CI: 0.29‐0.57) of cough, 0.46 (95% CI: 0.36‐0.56) of fever in pediatric inpatients with SARS‐CoV‐2 infection with heterogeneity of 72% and 67%, respectively. And the proportion of diarrhea was 0.10 (95% CI: 0.07‐0.14), vomiting was 0.08 (95% CI: 0.05‐0.11), nasal congestion was 0.12 (95% CI: 0.06‐0.23), fatigue was 0.08 (95%CI: 0.05‐0.12), respectively (Table 2) (Figure 2). Furthermore, the proportion of asymptomatic cases was 0.42 (95% CI: 0.27‐0.59) and severe cases was 0.03 (95% CI: 0.01‐0.06) (Figure S1 and S2).
Table 2.
Meta‐analysis results of demographical and clinical characters
| Variable | N | Estimate | 95% CI | I 2 (%) | P |
|---|---|---|---|---|---|
| Sex (male) | 455 | 1.64 | (0.95‐2.83) | 62 | <.01 |
| Cough | 299 | 0.42 | (0.29‐0.57) | 72 | .04 |
| Fever | 464 | 0.46 | (0.36‐0.56) | 67 | <.01 |
| Diarrhea | 265 | 0.10 | (0.07‐0.14) | 0 | .31 |
| Vomiting | 284 | 0.08 | (0.05‐0.11) | 46 | .05 |
| Nasal congestion | 24 | 0.12 | (0.06‐0.23) | 58 | <.01 |
| Fatigue | 230 | 0.08 | (0.05‐0.12) | 0 | .89 |
Abbreviation: CI, confidence interval.
Figure 2.
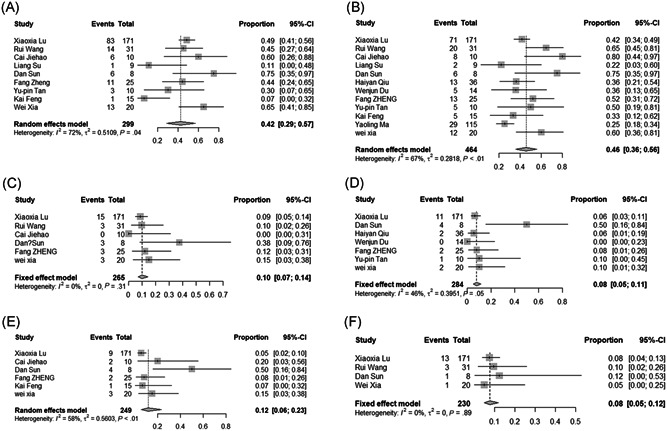
The forest plots of the incidence of clinical features. A, Cough; B, Fever; C, Diarrhea; D, Vomiting; E, Nasal congestion; F, Fatigue. CI, confidence interval
3.3. Laboratory test indicators
The laboratory test indicators were analyzed in this study. As the results shown, the incidence of leukocytosis was 0.13 (95% CI: 0.05‐0.29), leukopenia was 0.21 (95% CI: 0.12‐0.34), high CRP was 0.17 (95% CI: 0.07‐0.37), lymphocytosis was 0.22 (95% CI: 0.11‐0.38), lymphopenia was 0.16 (95% CI: 0.07‐0.32), high alanine aminotransferase was 0.15 (95% CI: 0.05‐0.38), high aspartate aminotransferase (AST) was 0.19 (95% CI: 0.10‐0.33), high D‐dimer was 0.12 (95% CI: 0.05‐0.25), and high creatine kinase‐MB (CK‐MB) was 0.05 (95% CI: 0.01‐0.32) (Table 3) (Figure S3‐11).
Table 3.
Meta‐analysis results of the laboratory tests
| Variable | N | Estimate | 95% CI | I 2 (%) | P |
|---|---|---|---|---|---|
| Leukocytosis | 198 | 0.13 | (0.05‐0.29) | 68 | <.01 |
| Leukopenia | 217 | 0.21 | (0.12‐0.34) | 66 | .02 |
| High CRP | 86 | 0.17 | (0.07‐0.37) | 58 | .03 |
| Lymphocytosis | 166 | 0.22 | (0.11‐0.38) | 57 | .03 |
| Lymphopenia | 398 | 0.16 | (0.07‐0.32) | 86 | .01 |
| High ALT | 137 | 0.15 | (0.05‐0.38) | 64 | .01 |
| High AST | 47 | 0.19 | (0.10‐0.33) | 0 | .37 |
| High D‐dimer | 43 | 0.12 | (0.05‐0.25) | 0 | .45 |
| High CK‐MB | 123 | 0.05 | (0.01‐0.32) | 73 | <.01 |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CI, confidence interval; CK‐MB, creatine kinase‐MB; CRP, C‐reactive protein.
3.4. Chest imaging features
For the chest CT features, the pneumonia characteristic was mainly bilateral and unilateral with the incidence of 22% (95% CI: 0.12‐0.33) and 22% (95% CI: 0.06‐0.44), respectively. The most common features on chest computed tomography were ground‐glass with the incidence of 39% (95% CI: 0.25‐0.53) (Table 4) (Figure 3).
Table 4.
Meta‐analysis results of chest imaging
| Variable | N | Estimate | 95% CI | I 2 (%) | P |
|---|---|---|---|---|---|
| Unilateral | 72 | 0.22 | (0.12‐0.33) | 0 | .72 |
| Bilateral | 288 | 0.22 | (0.06‐0.44) | 83 | .01 |
| Ground‐glass | 254 | 0.39 | (0.25‐0.53) | 60 | .02 |
Abbreviation: CI, confidence interval.
Figure 3.
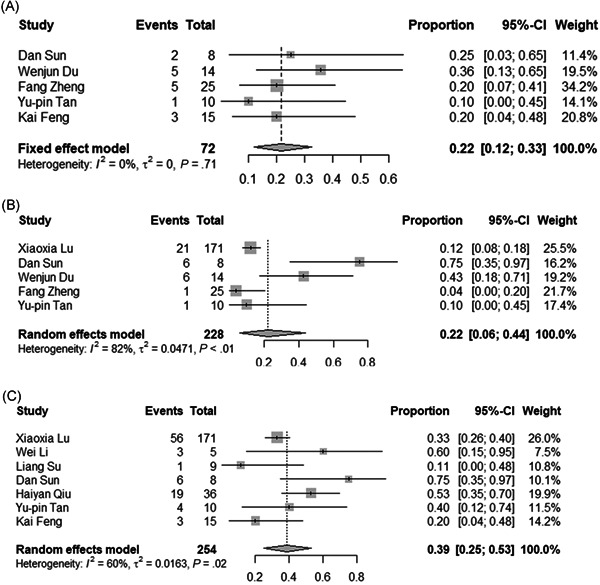
The forest plots of the incidence of imaging features. A, Unilateral; B, bilateral; C, ground‐glass. CI, confidence interval
4. DISCUSSION
Understanding the clinical characteristics of SARS‐CoV‐2 infection inpatients is benefit to the clinical diagnosis and treatment of COVID‐19. At the current studies, the clinical features of pediatric patients with SARS‐CoV‐2 infection were remains unclear. This meta‐analysis investigated this issues, and the results demonstrated that fever (46%) and cough (42%) were the main clinical characters of pediatric inpatients with SARS‐CoV‐2 infection and the other clinical characters, such as diarrhea, vomiting, nasal congestion, and fatigue account for approximately 10% in the pediatric inpatients. For the laboratory results, leukopenia (21%), and lymphocytosis (22%) were the mainly indicators for pediatric inpatients, followed by high AST (19%), high CRP (17%), lymphopenia (16%), high ALT (15%), leukocytosis (13%), high D‐dimer (12%), and high CK‐MB (5%). Regard to chest imaging features, unilateral and bilateral accounts for 22% in pediatric inpatients, respectively. Compared with adult inpatients with SARS‐CoV‐2 infection, 8 , 9 the pediatric inpatients had mild clinical characters, lab test indicators, and chest imaging features.
The reasons why pediatric inpatients are milder than the adult inpatients were still unknown. Recently, a systematic review reported that smoking could promote the progression of COVID‐19, and the smoking patients tend to suffer from the adverse outcomes of COVID‐19. 30 The absence of smoking in children may be one of the reasons for the mild clinical manifestation. What's more, other factors during life might also affect the disease degree of COVID‐19, and this suppose should be investigated in the further clinical studies. Recently, an updated expert consensus statement demonstrated lots of recommendation for the diagnosis, treatment, and prevention of COVID‐19 in children. 31 Furthermore, compared with adult patients, the number of pediatric patients was lower with milder symptoms and better prognosis, 31 which is consistent with the outcome of our meta‐analysis. Different from the expert consensus on 29 January 2020 which was clearly based on findings from adults, some recent studies on pediatric patients with SARS‐CoV‐2 infection play an essential role in update consensus. 15 , 23 , 26 , 29 In this update expert consensus, diagnosis and treatment criteria have been optimized, and early identification of severe and critical patients is emphasized. A case report from Singapore demonstrated that the asymptomatic infant with SARS‐CoV‐2 infection can excrete the virus, which indicated that the infant patients may act as a pivotal part in human‐to‐human transmission. 32 Another study that conducted by Tan et al 24 reported that persistent intestinal excretion of virus is another characteristic among children. Furthermore, Su et al 22 also found that five discharged children were admitted again owing to the positive result of their stool in SARS‐CoV‐2 nucleic acid polymerase chain reaction (PCR).
Several studies reported the fractures of infants and newborns with SARS‐CoV‐2 infection. Zhang et al showed that of four infections in newborn babies whose age range was 30 hours to 17 days old, all the mothers of them were infected with SARS‐CoV‐2, 3 displayed symptoms before delivery and one after delivery, but none of the babies had any severe complications. 33 In addition, the study on nine pregnant women with SARS‐CoV‐2 infection suggested that there is no obvious evidence of intrauterine infection caused by vertical transmission from mother to child. 34 In a word, newborn babies are easy to be infected by SARS‐CoV‐2. compared with adults, the clinical features in newborn babies were milder and prognosis was less severe. Intrauterine vertical transmission is possible but obvious evidence is still lacking.
As for the diagnosis of pediatric patients, all of them were confirmed SARS‐CoV‐2 infection by reverse transcription‐PCR of samples that were taken from upper nasopharyngeal swabs. In addition, rectal swabs were used to identify viral shedding through gastrointestinal tract in parts of studies. 22 At present, the therapeutic methods for pediatric patients were still limited. For the pediatric patients with mild clinical characters, antibiotics and symptomatic treatment were used. For the severe pediatric patients, parts of them were transferred to the pediatric intensive care unit, and several critical cases were given invasive mechanical ventilation and corticosteroids and immunoglobulin. As most of the pediatric inpatients had mild clinical characters, more diagnosis and treatment strategy for those pediatric patients with milder presentation should be developed.
5. STRENGTH AND LIMITATION
This meta‐analysis investigated the clinical, laboratory, and chest CT features of prediatric inpatients with SARS‐CoV‐2 infection comprehensively with relatively large sample size and relatively high study quality. The results of this study were more detailed accurate. However, this meta‐analysis has the following limitations. First, all of the samples are coming from china, so the race‐specific factors may bring a bias of the results. However, we analyzed the district of each study and found that subjects of most studies were from different provinces or districts. For the studies which were conducted at the same provinces of districts, the research period was also different. Therefore, the overlap of patients' population from different studies could be ignored. Second, lots of result were based on the random‐effect model analysis,which might reduce the strength of evidence; Third, studies with non‐English written were excluded from this study, which may influences the accuracy of the results. Fourth, all the included subjects in this study were inpatients, but it's may not necessary hospitalized for all the prediatric COVID‐19 cases as the symptoms in most patients were mild. Whether the prediatric COVID‐19 cases require hospitalization should be decided based on their clinical symptoms.
6. CONCLUSION
Compared with the adult patients with SARS‐CoV‐2 infection, the pediatric patients had mild clinical characters, lab test indicators, and chest imaging features. More clinical studies focus on the pediatric patients with SARS‐CoV‐2 infection in other countries should be conducted to investigate the more detailed characteristics of pediatric patients with SARS‐CoV‐2 infection.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Study concept and design: XYN. Study collection: MXF, LSS, CLZ, ZLK, and ZJ. Acquisition and analysis of data: MXF, LSS, CLZ, and ZLK. The drafting and writing of the manuscript: MXF and LSS. The revision of the manuscript: XYN.
Supporting information
Supporting information
ACKNOWLEDGMENT
This project was supported by the National Natural Science Foundation of China (grant no. 31770837).
Ma X, Liu S, Chen L, Zhuang L, Zhang J, Xin Y. The clinical characteristics of pediatric inpatients with SARS‐CoV‐2 infection: A meta‐analysis and systematic review. J Med Virol. 2021;93:234–240. 10.1002/jmv.26208
Xuefeng Ma and Shousheng Liu contributed equally to this work.
REFERENCES
- 1. Guan WJ, Ni ZY, Hu Y, Liang, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Malik YS, Sircar S, Bhat S, et al. Emerging novel coronavirus (2019‐nCoV)‐current scenario, evolutionary perspective based on genome analysis and recent developments. Vet Q. 2020;40(1):68‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Al‐Tawfiq JA, Kattan RF, Memish ZA. Middle East respiratory syndrome coronavirus disease is rare in children: an update from Saudi Arabia. World J Clin Pediatr. 2016;5(4):391‐396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Xu Y, Li X, Zhu B, et al. Characteristics of pediatric SARS‐CoV‐2 infection and potential evidence for persistent fecal viral shedding. Nature Med. 2020;26(4):502‐505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li AM, Ng PC. Severe acute respiratory syndrome (SARS) in neonates and children. Arch Dis Child Fetal Neonatal Ed. 2005;90(6):F461‐F465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chan KW, Wong VT, Tang SCW. COVID‐19: An update on the epidemiological, clinical, preventive and therapeutic evidence and guidelines of integrative Chinese‐western medicine for the management of 2019 novel coronavirus disease. Am J Chin Med. 2020;48(3):737‐762. [DOI] [PubMed] [Google Scholar]
- 8. Cao Y, Liu X, Xiong L, Cai K. Imaging and clinical features of patients with 2019 novel coronavirus SARS‐CoV‐2: a systematic review and meta‐analysis. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li LQ, Huang T, Wang YQ, et al. COVID‐19 patients' clinical characteristics, discharge rate, and fatality rate of meta‐analysis. J Med Virol. 2020;92:577‐583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rodriguez‐Morales AJ, Cardona‐Ospina JA, Gutiérrez‐Ocampo E, et al. Clinical, laboratory and imaging features of COVID‐19: a systematic review and meta‐analysis. Travel Med Infect Dis. 2020;34:101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chang TH, Wu JL, Chang LY. Clinical characteristics and diagnostic challenges of pediatric COVID‐19: a systematic review and meta‐analysis. J Formosan Med Assoc. 2020;119(5):982‐989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ludvigsson JF. Systematic review of COVID‐19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088‐1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Quality appraisal of case series studies checklist . Institute of Health Economics 2014.
- 14. Vienna ARFfSC . R: a language and environment for statistical computing. R‐Core‐Team.
- 15. Cai J, Xu J, Lin D, et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Du W, Yu J, Wang H, et al. Clinical characteristics of COVID‐19 in children compared with adults in Shandong Province, China. Infection. 2020;48:445‐452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Feng K, Yun YX, Wang XF, et al. Analysis of CT features of 15 children with 2019 novel coronavirus infection. Zhonghua Er Ke Za Zhi. 2020;58:E007. [DOI] [PubMed] [Google Scholar]
- 18. Li W, Cui H, Li K, Fang Y, Li S. Chest computed tomography in children with COVID‐19 respiratory infection. Pediatr Radiol. 2020;50:796‐799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lu X, Zhang L, Du H, et al. SARS‐CoV‐2 infection in children. N Engl J Med. 2020;382(17):1663‐1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ma YL, Xia SY, Wang M, Zhang SM, Du WH, Chen Q. Clinical features of children with SARS‐CoV‐2 infection: an analysis of 115 cases. Zhongguo Dang Dai Er Ke Za Zhi. 2020;22(4):290‐293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID‐19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020;20:689‐696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Su L, Ma X, Yu H, et al. The different clinical characteristics of corona virus disease cases between children and their families in China—the character of children with COVID‐19. Emerg Microbes Infect. 2020;9(1):707‐713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sun D, Li H, Lu XX, et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center's observational study. World J Pediatr. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tan YP, Tan BY, Pan J, Wu J, Zeng SZ, Wei HY. Epidemiologic and clinical characteristics of 10 children with coronavirus disease 2019 in Changsha, China. J Clin Virol. 2020;127:104353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang D, Ju XL, Xie F, et al. Clinical analysis of 31 cases of 2019 novel coronavirus infection in children from six provinces (autonomous region) of northern China. Zhonghua Er Ke Za Zhi. 2020;58(4):E011. [DOI] [PubMed] [Google Scholar]
- 26. Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID‐19 infection: different points from adults. Pediatr Pulmonol. 2020;55(5):1169‐1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yang P, Wang X, Liu P, et al. Clinical characteristics and risk assessment of newborns born to mothers with COVID‐19. J Clin Virol. 2020;127:104356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zheng F, Liao C, Fan QH, et al. Clinical characteristics of children with coronavirus disease 2019 in Hubei, China. Curr Med Sci. 2020;40(2):275‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhu H, Wang L, Fang C, et al. Clinical analysis of 10 neonates born to mothers with 2019‐nCoV pneumonia. Transl Pediatr. 2020;9(1):51‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vardavas CI, Nikitara K. COVID‐19 and smoking: a systematic review of the evidence. Tob Induc Dis. 2020;18:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Carugno J, Di Spiezio Sardo A, Alonso L, et al. COVID‐19 pandemic. Impact on hysteroscopic procedures. A consensus statement from the Global Congress of Hysteroscopy Scientific Committee. J Minim Invasive Gynecol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kam KQ, Yung CF, Cui L, et al. A well infant with coronavirus disease 2019 (COVID‐19) with high viral load. Clin Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhang ZJ, Yu XJ, Fu T, et al. Novel coronavirus infection in newborn babies under 28 days in China. Eur Respir J. 2020;55:2000697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wei M, Yuan J, Liu Y, Fu T, Yu X, Zhang ZJ. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information


