Abstract
Purpose
Heightened COVID-19 mortality among Black non-Hispanic and Hispanic communities (relative to white non-Hispanic) is well established. This study aims to estimate the relative contributions to fatality disparities in terms of differences in SARS-CoV-2 infections, diagnoses, and disease severity.
Methods
We constructed COVID-19 outcome continua (similar to the HIV care continuum) for white non-Hispanic, Black non-Hispanic, and Hispanic adults in New York State. For each stage in the COVID-19 outcome continua (population, infection experience, diagnosis, hospitalization, fatality), we synthesized the most recent publicly available data. We described each continuum using overall percentages, fatality rates, and relative changes between stages, with comparisons between race and ethnicity using risk ratios.
Results
Estimated per-population COVID-19 fatality rates were 0.03%, 0.18%, and 0.12% for white non-Hispanic, Black non-Hispanic, and Hispanic adults, respectively. The 3.48-fold disparity for Hispanic, relative to white, communities was explained by differences in infection experience, whereas the 5.38-fold disparity for non-Hispanic Black, relative to white, communities was primarily driven by differences in both infection experience and in the need for hospitalization, given infection.
Conclusions
These findings suggest the most impactful stages on which to intervene with programs and policies to build COVID-19 health equity.
Keywords: Coronavirus, Infectious diseases, Epidemiology, Surveillance, Epidemics, Race factors
Introduction
The SARS-CoV-2 pandemic has reached over 2,054,000 diagnosed cases and 114,000 COVID-19 deaths in the United States as of June 13, 2020 [1]. New York State (NYS), especially the New York City (NYC) metropolitan area, has been the geographic area in the United States with the largest cumulative number of diagnosed cases (381,714) and COVID-19 deaths (30,758) as of the same date [1,2].
The racial and ethnic disparities in COVID-19 fatalities have received substantial attention. For example, in a large health system in California, Black patients were hospitalized for COVID-19 at 2.7 times the rate of white patients even after adjustment for sex, age, income, and comorbidities [3]. In a study of COVID-19 racial and ethnic disparities among over 5.8 million U.S. veterans, Black and Hispanic persons were more likely to be tested for COVID-19, and at increased odds of testing positive, although mortality at 30 days did not appear to differ [4]. In a large health care system in Louisiana, 31% of the patients are Black, but comprised 76.9% of the hospitalizations and 70.6% of the COVID-19 deaths [5]. A study of the county-level disparities in the United States found that 22% of the counties were “disproportionately Black” yet accounted for 52% of diagnoses and 58% of deaths related to COVID-19 [6]. Besides empirical observations of racial and ethnic disparities in the COVID-19 pandemic, other recent articles draw lessons from the history of infectious diseases as to why such disparities may exist, and how these lessons may provide a path forward to building health equity [[7], [8], [9]].
The racial and ethnic minority disparities in COVID-19 fatalities in NYS (excluding NYC) are clear and pronounced with the age-adjusted death rates per 100,000 population for Black, Hispanic, Asian American, and white communities being 112, 101, 60, and 28, respectively, as of mid-June 2020 (further information on the impact of SARS-CoV-2 in Native American communities is lacking and much needed) [10,11].
To address racial and ethnic disparities in COVID-19 fatalities, it is crucial to define and compare competing metrics for fatalities, as well as better understand their upstream determinants. First, it is important to separate population fatality rate (COVID-19 deaths divided by population size, PFR), infection fatality rate (deaths divided by estimated number of SARS-CoV-2 infections in the population, IFR), and case fatality rate (deaths divided by estimated number of diagnoses cases in the population, CFR). When stratified by race and ethnicity, PFR, IFR, and CFR potentially portray different lenses through which to view and understand the disparities in COVID-19 deaths. These various fatality rates by race and ethnicity are not currently available in the literature to our knowledge, in part because of limited availability of appropriately stratified data sources, such as population-based seroprevalence studies or case registries.
Second, to better understand the sources of racial and ethnic disparities in the various COVID-19 fatality rate metrics, we construct a continuum analogous to the well-known “care continuum” in the HIV literature which traces the fraction of the population diagnosed as living with HIV, the percentage of diagnosed persons accessing HIV-related medical care, and the fraction of persons who experience HIV viral suppression [[12], [13], [14]]. For COVID-19, such a continuum might trace the following steps, which are key, routinely reported health quantities and events: (a) population size; (b) infection experience with SARS-CoV-2; (c) diagnosis; (d) hospitalization; and (e) fatality. By constructing such a continuum for COVID-19 and stratifying by race and ethnicity, one can better determine if the racial and ethnic disparities seen in fatality metrics are also seen at other steps, and importantly at which steps and to what degree. These insights can inform policy decisions as to how best to intervene to reduce disparities and promote health equity related to COVID-19.
In the present article, we estimate the NYS COVID-19 outcomes continuum by race and ethnicity. An important challenge to address in the construction of a COVID-19 continuum is the establishment of an analytic framework for synthesizing data sources that allows valid and meaningful movement from one step to the next in the continuum, as opposed to simply identifying individual, not comparable sources in estimating each step [14]. Using recently available population-based data sources, we propose such an analytic framework.
Methods
Continuum construction
The COVID-19 outcomes continuum for adults 18 years or older was conceptualized and estimated in five distinct steps: population, infection experience (cumulative incidence), diagnosis, hospitalization, and fatality. We used both publicly available and peer-reviewed data sources (Table 1 ) to estimate the absolute number and relative racial and ethnic distribution of individuals within these steps. We estimated the continuum for the cohort of adults in the period defined for a statewide seroprevalence study in NYS, which estimated cumulative incidence of SARS-CoV-2 by race and ethnicity through approximately March 29 [16]. Calculations were performed for the four racial and ethnic groupings of white non-Hispanic, Black non-Hispanic, Hispanic, and “all other races and ethnicities combined” so as to address the entire adult population; however, we present detailed results on the first 3 because of greater data robustness, completeness, and interpretability. Importantly, we note that for Asian, Native Hawaiian and other Pacific Islander, American Indian, Alaska Native, multiracial, multiethnic, and other communities, the completeness of the available data and the size of each specific community prohibited construction of separate continua, and we identify these as key data gaps to urgently address in the future.
Table 1.
Data sources used to construct the COVID-19 outcomes continuum for New York State
| Data source | Population represented | Areas of New York represented | Race/ethnicity available | Date information | Continuum steps used in | |
|---|---|---|---|---|---|---|
| A | CDC National Center for Health Statistics Bridged Race File, Vintage 2018 [15] | Adults 18 years or older | Statewide, by region | Yes | 2018 | Population |
| B | New York State Department of Health antibody seroprevalence study [16] | Noninstitutionalized adults aged 18+ years | Statewide, by region | Yes (infection experience, but not diagnosis) | Conducted April 19–28, reflecting infections through approx. March 29th. Includes total diagnoses through April 9 | Infection experience, Diagnosis |
| C | New York City Department of Health and Mental Hygiene COVID-19 data report [17] | Individuals diagnosed with COVID-19 | New York City (NYC) | Yes | All diagnoses through April 9th, 2020 | Diagnosis |
| D | Retrospective cohort study of hospitalized New York COVID-19 patients [18] | Random sample of individuals hospitalized with laboratory-confirmed COVID-19 in 25 hospitals | New York Metropolitan Area (NYC, Nassau, Suffolk, and Westchester Counties) | Yes | Admissions between March 15th and 28th, 2020 | Hospitalization, fatality |
| E | Online archive of officially reported New York State COVID-19 hospitalizations and deaths [19] | All individuals reported hospitalized and died with COVID-19 | Statewide | No | As of April 9th (hospitalization) and April 17th (fatality) | Hospitalization, fatality |
Population
The continuum is estimated here for all adults including institutionalized persons (i.e., including incarcerated persons and nursing home residents; Table 1, source A) who are disproportionally affected by COVID-19 while making up a small portion (1.3%) of the general adult population. This population is represented in all data sources utilized here, other than the seroprevalence study [15].
Infection experience
The probabilities of a history of SARS-Cov-2 infection by race–ethnicity observed in the NYS seroprevalence study (Table 1, source B) were applied to the adult population estimates [16].
Diagnosis
Information on the race and ethnicity of COVID-19 diagnoses is not publicly available statewide, but is reported for residents of NYC, with 41% completeness (source C) [17]. Completeness of 41% is not ideal, but it is the best available public information to the best of our knowledge. We thus first estimated the full diagnosis distribution in NYC by applying the race and ethnicity distribution for complete cases to the total number of diagnosed cases in NYC as of April 9th (source B, reflecting 4 days to symptom onset plus 9 to diagnosis). Next, for each racial and ethnic group, the percentage diagnosed within NYC was estimated by dividing the diagnosed case counts by the number of individuals who experienced SARS-CoV-2 infection (“infection experienced”), as previously carried out for age and sex stratifications [16].
We next applied this distribution to the rest of NYS (ROS) by multiplying the within-group diagnosis rates in NYC by the total number of infections by each group in the ROS, thus accounting for differences in racial/ethnic composition of adults in the ROS compared with NYC. As the overall percentage diagnosed was previously found significantly higher in the ROS compared with NYC (12.9% vs. 7.1%), diagnoses were next equally scaled across racial/ethnic groups to match the total overall number of diagnoses in the ROS through April 9th (source B). The sum within-group diagnoses for NYC and the ROS diagnoses then yielded the statewide estimates.
Hospitalization
The racial/ethnic distribution among hospitalizations was calculated from a random sample of medical records from the patients admitted to hospitals in metropolitan NYC counties, which represented 88% of diagnosed COVID-19 patients in NYS from March 15 to 30 (source D) [18]. These proportions were multiplied by the cumulative number of individuals hospitalized for COVID-19 in NYS as of April 9th (42,852) (source E), reflecting that 85% of hospitalized patients were diagnosed concurrent with admission during this time period, then multiplied by the percentage of hospitalized individuals 18 years or older (98.3%) from the sample study, to yield the total number of hospitalized adults (42,124) for each racial and ethnic group [19].
Fatality
Although racial and ethnic data on fatalities are available publicly from both NYC and the ROS, they differ in completeness and methodology, and are likely underestimates due to missingness in race and ethnicity collection. Therefore, we estimated in-hospital fatality by multiplying, for each racial/ethnic group, the probability of in-hospital death observed in the hospital sample study by the estimated number of persons hospitalized (source D). These total deaths were finally scaled to allow the resulting estimated total in-hospital deaths (8,580) to match the total officially reported number of COVID-19 fatalities in NYS (12,822) as of April 17th, which were then multiplied by the percentage of fatalities attributed to adults 18 years or older (99.94%), to yield the total number of adult fatalities (12,814) by race and ethnicity (source E).
Assessment of outcomes and disparities
After estimation of adults at each step of the continuum, we computed the percentage at each step per population. In addition to overall fatality per population (“PFR”), we estimated race-specific infection fatality rates (per infection-experienced individuals, “IFR”) and case-fatality rates (per diagnosed persons, “CFR”). We also present additional conditional percentages to assess where along the continuum racial/ethnic disparities emerge: severity (hospitalization, among those infected) and fatalities to hospitalizations (total fatalities, per person hospitalized). Disparities in these quantities were summarized using risk ratios.
Results
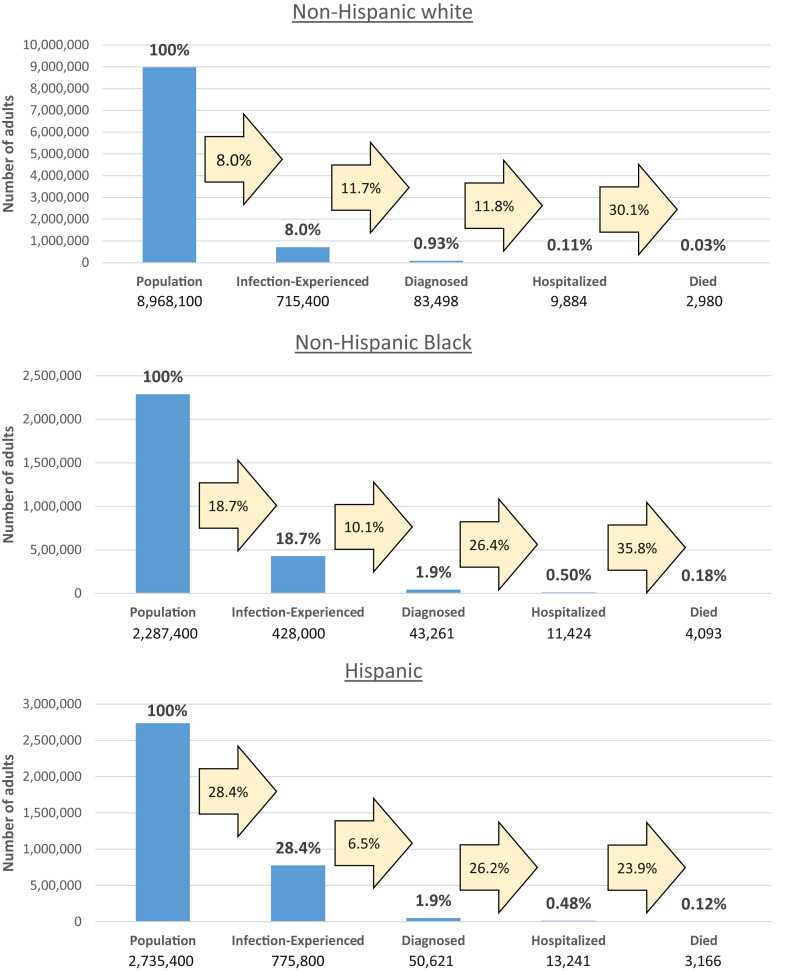
In the population of adult New York residents, through late March 2020, 8.0% of white non-Hispanic, 18.7% of Black non-Hispanic, and 28.4% of Hispanic adults were estimated to have experienced infection with SARS-CoV-2 (Fig. 1 ). Compared with white non-Hispanic adults, racial/ethnic minority populations had disproportionately higher per-population likelihoods of COVID-19 diagnosis (0.93% white non-Hispanic, 1.89% Black non-Hispanic, 1.85% Hispanic), hospitalization (0.11% white non-Hispanic, 0.50% Black non-Hispanic, 0.48% Hispanic), and death (0.03% white non-Hispanic, 0.18% Black non-Hispanic, 0.12% Hispanic).
Fig. 1.
Estimated COVID-19 outcomes continuum for adults infected with SARS-CoV-2 through March 29, by race and ethnicity, New York Statea,b. a. The bars represent total individuals at each step (with percentages among the total population). The arrows represent the portion estimated to proceed to the next step. b. Estimates are rounded after calculations conducted at greater precision.
Next, the analyses indicate that among individuals with infection experience, diagnosis rates varied by race and ethnicity: 11.7% of infection-experienced white non-Hispanic adults were diagnosed compared with 10.1% of Black non-Hispanic adults and 6.5% of Hispanic adults (Fig. 1). Levels of hospitalization among persons diagnosed were about two-fold higher Black non-Hispanic and Hispanic adults compared with white non-Hispanic adults, with hospitalizations also relatively elevated among persons who were infected (Table 2 ).
Table 2.
Fatality rates and additional measures, by race and ethnicity∗
| Outcome | White, non-Hispanic |
Black, non-Hispanic |
Hispanic |
||
|---|---|---|---|---|---|
| % | % | Ratio versus white, non-Hispanic | % | Ratio versus white, non-Hispanic | |
| Fatality rates | |||||
| Crude fatality rate (deaths, per population) | 0.03% | 0.18% | 5.38 | 0.12% | 3.48 |
| Infection fatality rate (deaths, per person infected) | 0.42% | 0.96% | 2.30 | 0.41% | 0.98 |
| Case fatality rate (deaths, per diagnosed case) | 3.57% | 9.46% | 2.65 | 6.25% | 1.75 |
| Additional conditional measures | |||||
| Infection risk (infection, per population) | 7.98% | 18.71% | 2.35 | 28.36% | 3.56 |
| Severity (hospitalization, per person infected) | 1.38% | 2.67% | 1.93 | 1.71% | 1.24 |
| Fatalities to hospitalizations (total fatalities, per person hospitalized). | 30.15% | 35.83% | 1.19 | 23.91% | 0.79 |
Estimates are rounded after calculations conducted at greater precision.
Fatality rates and rate ratios comparing racial and ethnic minorities with white adults are shown in Table 2. The population fatality rate ratios illustrate that per population, Black non-Hispanic and Hispanic adults were, respectively, 5.38 and 3.48 times as likely to die of COVID-19 as were white non-Hispanic adults. Conditioning among those who were infected, the IFR for Black non-Hispanic adults remained 2.30-fold that of white non-Hispanic, whereas no disparity remained for Hispanic versus white non-Hispanic adults (IFR ratio = 0.98). Among those diagnosed, the relative CFR was 2.65 for Black non-Hispanic versus white non-Hispanic adults, and 1.75 for Hispanic versus white non-Hispanic adults.
These divergent fatality disparities are explained by different trajectories along the continuum. Among Black non-Hispanic adults, disparities are evident at all continuum steps; the 5.38 overall fatality ratio compared with white non-Hispanic adults is the product of risk ratios of 2.35 for infection, 1.93 for severity (hospitalization given infection), and 1.19 for fatalities to hospitalizations. Among Hispanic adults, compared with white non-Hispanic adults, the risk ratio was 3.56 for infection, whereas the product of the latter two ratios of 1.24 for severity, and 0.79 for fatalities to hospitalizations, yields the estimated 0.98 relative risk for death given infection summarized by the IFR.
Discussion
Examination of the racial and ethnic continua for SARS-CoV-2 in NYS shows that the disparities in fatalities in Hispanic communities relative to non-Hispanic white populations appear to be due in large part to differences earlier on in infections. For non-Hispanic Black communities relative to white, disparities in mortality appear to be due to both differences in infections and in hospitalization rates and equally so at approximately 2-fold disparity each. This provides important signals about which stages on the continuum might be most useful to enhance service delivery and to focus policy interventions and further research. For instance, to address racial and ethnic differences in cumulative infection in Hispanic and Black communities, one might consider addressing “upstream” factors that are directly related to exposure to SARS-CoV-2 such as housing and food insecurity, high housing density, more front-line service occupations that made sheltering at home more difficult, and heightened reliance on public transportation, in addition to root causes of these conditions such as systemic income inequality, racism, and discrimination [[7], [8], [9],20]. To address differences in hospitalizations for Black communities, one might further consider disparities in underlying health conditions, such as diabetes, coronary disease, and chronic lung disease, which appear to be predisposing to poor clinical outcomes in COVID-19 (the root societal causes of those underlying health conditions must also be addressed, of course) [[7], [8], [9],20].
We also provide the first state-level estimates of the percentage of infections diagnosed by race and ethnicity, showing lower diagnosis levels among Black and particularly Hispanic adults, relative to white non-Hispanic adults. Lower levels of diagnosis may be related to diminished access to routine health care and/or specialized testing for SARS-CoV-2 due to a variety of factors including transportation, health insurance access, and other key social determinants of health [[7], [8], [9]]. We note that the lesser percentage of infections diagnosed among Hispanic adults also serves to inflate apparent disparities in estimates of hospitalization among those diagnosed and the CFR relative to white adults—once hospitalization and fatality are evaluated over a denominator of infection experience, the disparities become more muted. An important resulting epidemiologic lesson is that measures of hospitalization and fatality that condition on diagnosis may be ill-suited for understanding of disparities.
Furthermore, we note that the methodology used here to establish comparable measures across stages of the continuum and across racial and ethnic groups appears to triangulate well with other known data sources; for instance, the high per-population disparities in fatality by race and ethnicity closely track with what has been observed on the state and NYC fatality dashboards [10,17].
There are several limitations in the current analysis, and they include the following. First, a number of the metrics measured or estimated here are subject to sources of random and systematic error. Given that there is no clear a priori estimate of the scope and direction of the latter bias because we are in the earlier days of the pandemic, we do not include further sensitivity analyses here in this first exposition of the continuum, but rather present the most detailed, empirically based information for each stage. However, we note that continued validation of the continuum parameter estimates will be important in the months and years ahead as further data are gathered relevant to each stage in the continua. For instance, it is not yet clear whether there are differences by race and ethnicity in terms of percentage of persons living with SARS-CoV-2 who are asymptomatic or presymptomatic; as lessons are learned in the future in this regard, potential refinements to the continua can be made.
A second limitation is that our estimated continuum does not include as separate categories Asian, other Pacific Islander, Native American, Alaskan Native, and multiracial, multiethnic communities, and this is a clear limitation of currently available data; given the population size of some of these racial and ethnic communities, it will be necessary to construct future applied studies and surveillance activities dedicated to the oversampling needed to make meaningful continua estimates by each population.
Third, although we estimate in detail the continuum for NYS, it will be useful to see the development of the continuum in other jurisdictions, and until that is accomplished, we are careful not to generalize our findings beyond New York, although the methodology used here could be productively used in other locales. Fourth, although we have taken care to establish the continuum at a given, well-specified moment in time, the COVID-19 pandemic is evolving quickly, and it will be important to repeat this analysis at multiple, future times to better understand the dynamic trajectories of racial and ethnic disparities.
Fifth, the continuum offered here provides a framework for further COVID-19 surveillance activities; indeed, a comprehensive, timely COVID-19 surveillance system could be crafted around this continuum, and the resultant data and analyses used as a dashboard to monitor progress in the pandemic both in terms of health outcomes and social justice.
We also note the limitations to the construction of each step of the continuum from the currently available data sources, and maturation of the available data over time for each continuum step will be important. For example, our approach applied a general population cumulative incidence estimate to the entire population, including institutionalized persons, who are included in the diagnosis, hospital, and fatality outcomes. Given documented excess burden in institutional settings such as nursing homes, this likely underestimates our estimate of infection-experienced adults, but it is the only feasible option absent more comprehensive prevalence data on these populations, who make up 1.3% of the adult population [21].
Another limitation related to data availability is that current publicly available data on the racial and ethnic composition of diagnoses are limited to partially complete data on NYC, which contains about 43% of the state's population [15]. Enhancements for routine collection and reporting of race and ethnicity from diagnostic testing are needed. Indeed, the sparseness of racial and ethnic data for COVID-19 diagnoses has been a source of major discussion in the public domain, notably including a recent federal mandate that all jurisdictions must collect and report race and ethnicity for diagnoses by August 1, 2020 [22]. Although data to characterize the distribution of this missingness, and assess the direction of potential bias, are currently not available, we have attempted to use the available information in the best way feasible; we have drawn on principles of risk factor redistribution from HIV surveillance by proportionally applying known information to those with unknown data in NYC and also to the rest of NYS, after first adjusting for the higher levels of diagnosis in the rest of the state. A major purpose of this article is to lay out a framework for illuminating disparities using the best available data, and also for highlighting priority areas for future data refinement toward the end of increasing health equity; this is such a priority area.
A similar call can be made for more complete racial and ethnic information for hospitalizations. Here we used a hospitalized sample reflecting 88% of NYS COVID-19 cases located in metropolitan NY, a region with proportionally more nonwhite persons than the ROS. Were data on the racial/ethnic composition of the remaining 12% ROS hospitalizations available, they may more reflect white-patient hospitalizations. We also note that hospitalization totals may not be fully deduplicated for multiple admissions and transfers, thus possibly inflating the hospitalized estimates, although it is unknown if this is differential by race and ethnicity. Finally, in scaling in-hospital to all fatalities, we assumed nonhospital fatalities followed the same relative patterns as in-hospital fatalities by race and ethnicity.
We note that our findings are not age-adjusted, thus providing an overall view of outcomes for and disparities between racial and ethnic groups, which may be further explained by differences in risk factors. One such important factor is age, which is associated with COVID-19 severity [3,18]. Although the lack of age distribution data within racial and ethnic groupings precludes control in this analysis, we note that per Census data 25%, 17%, and 13% of white non-Hispanic, Black non-Hispanic, and Hispanic adults, respectively, in New York are aged more than 65 years. Given that we observed racial and ethnic disparities in most continuum outcomes, despite the white non-Hispanic population being older, this suggests that the overall disparities documented might increase if we additionally controlled for age.
Our conceptualization of the continuum is not intended to be final, but rather illustrative of current key outcomes that are vital to describing the epidemic; stages may be added or modified as epidemiological and clinical understanding evolves. Furthermore, the continuum provides a framework for organizing many data sets in a way that is coherent, program and policy relevant, and can be constantly updated as new data become available. We assert that this continuum should be a “living document” much as the HIV care continuum described previously is continually updated with new clinical understanding, data, and analytic approaches. Indeed a series of such analyses should be performed over time so that the continua are better understood by the dynamic and evolving intersections of race and ethnicity with gender, age, geography, comorbid conditions, and key social factors.
Despite these limitations, the COVID-19 continuum stratified by race and ethnicity, even in this early form, provides important insights as to what factors underlie the already widely recognized health disparities in COVID-19 deaths, and suggest possible points of intervention to begin to better build health equity in the era of the COVID-19 pandemic.
Footnotes
Author contribution: D.R.H.: Writing – original draft, Writing – review & editing, Formal analysis. M.A.B.: Writing – original draft, Writing – review & editing, Formal analysis. J.M.T.: Writing – review & editing. D.S.B.: Writing – review & editing. E.S.R.: Methodology, Writing – original draft, Writing – review & editing, Formal analysis.
References
- 1.JHU COVID-19 United States Cases. 2020. https://coronavirus.jhu.edu/us-map
- 2.Rosenberg E.S., Dufort E.M., Blog D.S., Hall E.W., Hoefer D., Backenson B.P. COVID-19 testing, epidemic features, hospital outcomes, and household prevalence, New York State-March 2020. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa549. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Azar K.M.J., Shen Z., Romanelli R.J., Lockhart S.H., Smits K., Robinson S. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood) 2020;39(7):1253–1262. doi: 10.1377/hlthaff.2020.00598. [DOI] [PubMed] [Google Scholar]
- 4.Rentsch C.T., Kidwai-Khan F., Tate J.P., Park L.S., King J.T., Skanderson M. Covid-19 by race and ethnicity: a national cohort study of 6 million United States veterans. medRxiv. 2020 doi: 10.1101/2020.05.12.20099135. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Millett G.A., Jones A.T., Benkeser D., Baral S., Mercer L., Beyrer C. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krishnan L., Ogunwole S.M., Cooper L.A. Historical insights on coronavirus disease 2019 (COVID-19), the 1918 influenza pandemic, and racial disparities: illuminating a path forward. Ann Intern Med. 2020 doi: 10.7326/M20-2223. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pan D., Sze S., Minhas J.S., Bangash M.N., Pareek N., Divall P. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine. 2020;23:100404. doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laurencin C.T., McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7(3):398–402. doi: 10.1007/s40615-020-00756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.New York State Department of Health NYSDOH COVID-19 tracker. 2020. https://covid19tracker.health.ny.gov/views/NYS-COVID19-Tracker/NYSDOHCOVID-19Tracker-DailyTracker?%3Aembed=yes&%3Atoolbar=no&%3Atabs=n
- 11.Akee R. 2020. How COVID-19 is impacting indigenous peoples in the U.S.https://www.pbs.org/newshour/nation/how-covid-19-is-impacting-indigenous-peoples-in-the-u-s [Google Scholar]
- 12.Gardner E.M., McLees M.P., Steiner J.F., Del Rio C., Burman W.J. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall H.I., Frazier E.L., Rhodes P., Holtgrave D.R., Furlow-Parmley C., Tang T. Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Intern Med. 2013;173(14):1337–1344. doi: 10.1001/jamainternmed.2013.6841. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg E.S., Millett G.A., Sullivan P.S., Del Rio C., Curran J.W. Understanding the HIV disparities between black and white men who have sex with men in the USA using the HIV care continuum: a modeling study. Lancet HIV. 2014;1(3):e112–e118. doi: 10.1016/S2352-3018(14)00011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NCHS U.S. census populations with bridged race categories. 2019. https://www.cdc.gov/nchs/nvss/bridged_race.htm
- 16.Rosenberg E.S., Tesoriero J.M., Rosenthal E.M., Chung R., Barranco M.A., Styer L.M. Cumulative incidence and diagnosis of SARS-CoV-2 infection in New York. Ann Epidemiol. 2020 doi: 10.1016/j.annepidem.2020.06.004. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.New York City Department of Health and Mental Hygiene Age-adjusted rates of lab-confirmed COVID-19 non-hospitalized cases, estimated non-fatal hospitalized cases, and total persons known to have died (lab-confirmed and probable) per 100,000 by race/ethnicity group. 2020. https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-deaths-race-ethnicity-05142020-1.pdf
- 18.Rosenberg E.S., Dufort E.M., Udo T., Wilberschied L.A., Kumar J., Tesoriero J. Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State. JAMA. 2020;323(24):2493–2502. doi: 10.1001/jama.2020.8630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Project TCT Our data: New York. 2020. https://covidtracking.com/data/state/new-york
- 20.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020 doi: 10.1001/jama.2020.8598. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McMichael T.M., Clark S., Pogosjans S., Kay M., Lewis J., Baer A. COVID-19 in a long-term care facility - King County, Washington, February 27-March 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):339–342. doi: 10.15585/mmwr.mm6912e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.HHS announces new laboratory data reporting guidance for COVID-19 testing [press release] 2020. https://www.cdc.gov/media/releases/2020/p0604-new-lab-data-reporting.html