Abstract
Background
Inappropriate visits to emergency departments (EDs) could represent from 20% to 40% of all visits. Inappropriate use is a burden on healthcare costs and increases the risk of ED overcrowding. The aim of this study was to explore socioeconomic and geographical determinants of inappropriate ED use in France.
Method
The French Emergency Survey was a nationwide cross-sectional survey conducted on June 11 2013, simultaneously in all EDs in France and covered characteristics of patients, EDs and counties. The survey included 48 711 patient questionnaires and 734 ED questionnaires. We focused on adult patients (≥15 years old). The appropriateness of the ED visit was assessed by three measures: caring physician appreciation of appropriateness (numeric scale), caring physician appreciation of whether or not the patient could have been managed by a general practitioner and ED resource utilisation. Descriptive statistics and multilevel logistic regression were used to examine determinants of inappropriate ED use, estimating adjusted ORs and 95% CIs.
Results
Among the 29 407 patients in our sample, depending on the measuring method, 13.5% to 27.4% ED visits were considered inappropriate. Regardless of the measure method used, likelihood of inappropriate use decreased with older age and distance from home to the ED >10 km. Not having a private supplementary health insurance, having universal supplementary health coverage and symptoms being several days old increased the likelihood of inappropriate use. Likelihood of inappropriate use was not associated with county medical density.
Conclusion
Inappropriate ED use appeared associated with socioeconomic vulnerability (such as not having supplementary health coverage or having universal coverage) but not with geographical characteristics. It makes us question the appropriateness of the concept of inappropriate ED use as it does not consider the distress experienced by the patient, and segments of society seem to have few other choices to access healthcare than the ED.
Keywords: emergency department, primary care, healthcare quality improvement, health services research
Introduction
Background
Several studies have underlined significant inequities in primary healthcare in selected Organisation for Economic Co-operation and Development countries.1 In the context of healthcare system evaluation, hospital readmissions2 as well as emergency department (ED) use for non-urgent care3–5 are indicators of suboptimal primary care delivery. Across Europe, different models of out-of-hours primary care exist6 7 and ED use must be considered among other unscheduled care options. Unscheduled care in France includes EDs but also general practitioners (GPs) performing home visits during the day time and out-of-hours or GPs with extended opening hours.8 In 2004, the French Head Office of Research, Studies, Evaluation and Statistics of the Social Affairs Ministry estimated that GPs performing home visits accounted for 5% of unscheduled care, and GPs with extended opening hours represented 11% of unscheduled care.9 However, a high number of avoidable ED visits still represent an issue.
Some have defined the use of ED resources for self-referred patients, with non-urgent conditions, which could have been handled by other services as primary care, pharmacies or telephone advice, as ‘inappropriate’.10–12 These patients use EDs to seek for immediate consultation, diagnostic tests and medication delivery to alleviate non-urgent symptoms.11 However, classifying some ED visits as inappropriate raises the question of what should be considered appropriate or not and the underlying assumptions of these decisions. Several studies have described that the distress experienced by the patient (defined as the lived experience and anxiety of the person seeking help in an ED) might contrast with the discharge diagnosis.13–17 From caregivers’ perspectives, ‘inappropriate’ visits could represent from 20% to 40% of all ED visits,11 18–20 with the different estimates mostly determined by the definition used for appropriateness.11 21
Importance
Although they may appear appropriate from the patient’s perspective, the ‘inappropriate’ ED visits may partly explain the steady increase in annual ED visits in France (13.6 to 21 million in less than 20 years)22 23 and worldwide.24 They have been described as possibly related to overcrowding3 5 25 but with a negligible effect on waiting times for patients with more urgent needs.26 However, they could possibly result in an additional burden on healthcare costs and have negative consequences on staff attitudes toward these patients.27 In 2014, a French administrative report estimated 20% of ED visits as inappropriate, corresponding to an avoidable expenditure of about €500 million.28
Recent studies have reported on substantial social disparities in health29–31 and healthcare access1 32 worldwide. From the patient perspective, the choice to self-refer to an ED (rather than an GP) depends on both individual characteristics (such as socioeconomics and health insurance coverage) and contextual factors, with the availability of primary care services possibly being one of the most important. Having a GP has been described as associated with reduced ED use at any age of life.33–36 Medical density (ratio of GPs to the total population of a given area37) discrepancies might be involved in patient difficulties in obtaining a prompt appointment with a GP.4 Both social disparities in health and territorial healthcare access disparities could be associated cofactors explaining ED use.
Previous studies explored the socioeconomic factors that could be related to ED inappropriate usage,18 38–40 based on a sample of ED patients, but none examined the effect of territorial healthcare access disparities.
Goals of this investigation
The aim of our study was to explore the socioeconomic and territorial factors (ie, territorial healthcare access) associated with inappropriate ED use based on data from a national survey of French EDs. We hypothesised that some indicators of socioeconomic vulnerability and some local territorial features (such as medical density of counties) might be associated with inappropriate ED use.
Methods
Study design and setting
As previously described,41 the French Emergency Survey (FES) was a nationwide cross-sectional survey, with a two-level design, aiming to depict emergency care in France by describing ED organisation and patients. The FES was developed by the French Society of Emergency Medicine and the French Head Office of Research, Studies, Evaluation and Statistics of the Social Affairs Ministry. Data were collected from 734 of the 736 adult and paediatric EDs listed for the French territory. All patients who had visited a French ED during the 24-hour inclusion period (Tuesday, 11 June 2013) were eligible for inclusion. The FES final database included data for 48 711 patients and 734 EDs, corresponding to a response rate of 94%.
Selection of participants
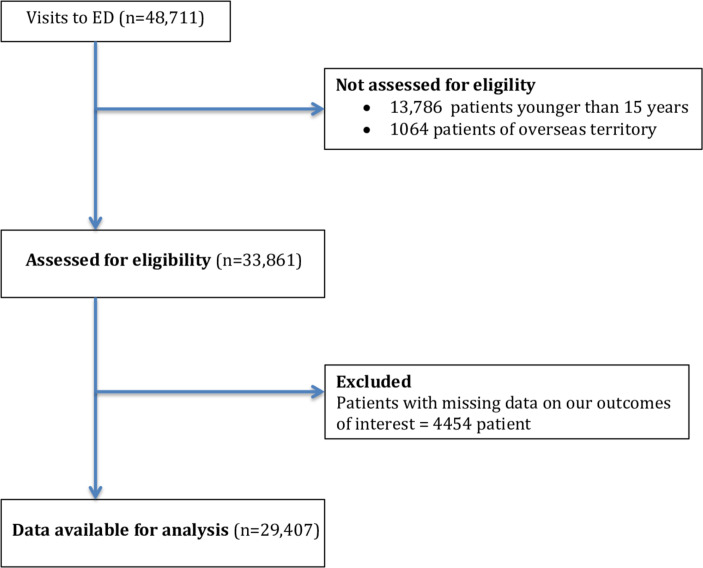
Among the 48 711 patients of the FES, we selected all patients ≥15 years old (the age for care in paediatric EDs versus adult EDs) who had presented to an ED in France (excluding overseas territories). We included all patients except the ones with missing data on all three main measures of ED use appropriateness.
Method of measurement
The methods of this study and the type of data collected were described in a previous publication.41 Briefly, the study took place on 11 June 2013, in all EDs in France. Data were collected from questionnaires concerning the organisation of the participating EDs (completed once by each ED administrator), patient characteristics (sociodemographic, usual use of the healthcare system and prior care procedures undertaken) and care management (completed by the emergency physician (EP) for each patient who presented to any of the surveyed EDs during the study period).
Outcome measures
Measures of ED use appropriateness
To assess the appropriateness of ED visit, we used three different measures.
The first one (Appropriate Use Score Method) was assessed by the caring physician at the end of the ED visit. The physician had to answer the following question: ‘According to you, how appropriate is this ED visit on a scale from 0 to 10 (0, totally not appropriate, to 10, totally appropriate)’. This continuous variable had a normal distribution. According to the literature, 20% to 40% of ED visits are considered inappropriate from EPs’ perspective.18–20 After the analysis of our variable distribution, we found that 20% of the study population had a score <4. We therefore transformed our continuous appropriateness variable to a binary one and considered all visits with a score <4 as inappropriate (corresponding to the 20% of the population with the lowest appropriateness of ED visits, according to the literature previously cited).
The second measure (Possible GP Use Method) was also assessed by the caring physician. The physician had to answer the following question: ‘According to you, could the patient have been managed by a GP the same day or the next day ?’—called « possible GP use » method. These two measures were subjective and based on EP’s judgement at the end of ED visit, as previously described in several studies.18 20 42–51
The last measure (Resource Utilisation Method) referred to ED resource utilisation. This method assesses urgency based on common resources used during the ED visit, including testing, therapeutics and hospital admission. This method assumes that ED visits of higher acuity necessitate greater use of healthcare resource. Resource use method has been used in several studies.52–54 Here, we defined inappropriate ED use as a patient who was discharged after ED visit and did not have any of the following criteria: admitted to the hospital, transferred to another hospital, deceased in the ED, diagnostic tests performed or treatments administered. As explained by Mistry et al,21 current literature suggests that resource utilisation method is the best feasible method for ED urgency assessment, taking into account the limited data.
Measured variables
Sociodemographic variables
The following sociodemographic variables were assessed by the survey: age (classified in 10-year age groups), sex, residence (home/institution/other (hotel, homeless, etc)), level of education (no high-school graduation/high-school graduation and higher), having a GP (yes/no) and employment status (employed/unemployed/inactive). According to the French National Institute for Statistics and Economic Studies definition, inactive work status included any person who was neither employed nor unemployed (students, retired, housewife, disabled). Patients were also asked about their health insurance coverage (none/state medical assistance/public health insurance) and supplementary health insurance coverage (none/private/universal health coverage (CMU-c)). In France, most healthcare costs are covered by the state under a public health insurance scheme. State medical assistance is available to people living in France for more than 3 months but for whom the application for legal residence has not been finalised and offers the same coverage as public health insurance. The copayment expenses must be paid by the patient or by any supplementary health insurance. In France, a large part of the population has private supplementary health insurance to cover reinsurable expenses not covered by public health insurance. Below a certain income threshold, individuals can benefit from a free complementary health insurance called the CMU-c.
ED visit-related variables
The following variables were assessed: presenting problem (medical complaint/traumatic injury), the onset of symptoms (the same day/>24 hours before), time of ED arrival (08:00–20:00/after 20:00) and type of care performed (blood tests/radiology imaging/therapeutic care/specialised advice). Reasons and motivations for ED visits were also recorded during the physician interview. They were then recoded by the physician in one or more modalities proposed in the questionnaire.
Variables related to ED as well as county and medical density
The following variables were included: annual visits for the ED visited (<15 000, 15 000–30 000, 30 000–45 000, >45 000), type of hospital (public academic/public non-academic/non-for-profit private/for-profit private), distance from home to ED (<10/>10 km) and county medical density of outpatient physicians (corresponding to the county number of specialists and GPs per 100 000 inhabitants). This county medical density was classified in three levels (low/medium/high) by the French National Medical Council (available on the French National Medical Council website55). In 2013, low, medium and high levels corresponded to <302, 302–393 and >393 doctors per 100 000 inhabitants, respectively.
Primary data analysis
Categorical variables are expressed as number (%). χ2 test was used to compare characteristics between patients with appropriate and inappropriate ED use. To analyse factors associated with inappropriate ED use (considering our three measures: appropriate ED use score, possible GP use method and resource utilisation method), adjusted ORs (aORs) and their 95% CIs were estimated from multilevel logistic regression models,56 57 which allowed us to consider the hierarchical structure of our data. We used multilevel logistic regression to account for the heterogeneity between EDs and to explain the appropriateness of ED use according to both patient and ED characteristics. First, we tested the non-adjusted model (the empty model), considering the cluster effect, but no explanatory variable. The aim of this first step was to confirm the possible intergroup heterogeneity and to justify the multilevel approach. Indeed, the intraclass correlation coefficients obtained in the empty model indicated, respectively, for the three measure methods that 12%, 6%, and 9% of the total variance of inappropriate ED use was explained by the ED level. We also tested the county level but did not find intergroup heterogeneity which justified a third level. Finally, we built the multilevel multivariate logistic regression model, adjusting for both patient and ED characteristics that were statistically significant on χ2 analysis at p<0.20 and included in the models. The nature of complaint was not included in our model because it is integral to whether a visit is appropriate or not (so the outcome would be represented on both sides of the equation). Sensitivity analyses had also been performed with a threshold for the Appropriate Use Score of 3 and 5. All statistical analyses involved using SAS/STAT 2002–2003 (SAS Institute, Cary, North Carolina, USA) and the GLIMMIX procedure. P value of <0.05 was considered statistically significant.
Results
Study participants’ characteristics
Among the 48 711 patients of FES, 29 407 were included in our study. Comparison between study population and patient excluded is available in online supplementary table 1. The study flow chart is shown in figure 1. About 48% (n=13 972) of participants were women and 87% (n=25 597) were living at home (table 1). Most patients (87.5%, n=25 719) had public health insurance, 71.5% (n=21 037) private supplementary health insurance, 7.2% (n=2126) CMU-c and 6.7% (n=1956) no supplementary health insurance (table 1).
Figure 1.
Flow chart. ED, emergency department.
Table 1.
Characteristics of study population
| Appropriateuse score method | PossibleGP use method | Resourceutilisation method | Total | |||||||
| Inappropriate ED use | Appropriate ED use | P value | Inappropriate ED use | Appropriate ED use | P value | Inappropriate ED use | Appropriate ED use | P value | ||
| n=6938 (23.59) | n=22 469 (76.41) | n=8052 (27.38) | n=21 355 (72.62) | n=3968 (13.49) | n=25 439 (86.51) | N=29 407 | ||||
| Patient characteristics | ||||||||||
| Age, years, n (%) | ||||||||||
| 15–24 | 1665 (24.00) | 3627 (16.14) | <0.0001 | 2018 (25.06) | 3275 (15.33) | <0.0001 | 1012 (25.50) | 4280 (16.82) | <0.0001 | 5292 (18.00) |
| 25–34 | 1414 (20.38) | 3615 (16.09) | 1747 (21.70) | 3282 (15.37) | 931 (23.46) | 4098 (16.11) | 5029 (17.10) | |||
| 35–44 | 1120 (16.14) | 3191 (14.20) | 1322 (16.42) | 2989 (14.00) | 703 (17.72) | 3608 (14.18) | 4311 (14.66) | |||
| 45–54 | 929 (13.39) | 2942 (13.09) | 1056 (13.11) | 2815 (13.18) | 583 (14.69) | 3288 (12.93) | 3871 (13.16) | |||
| 55–64 | 704 (10.15) | 2573 (11.45) | 774 (9.61) | 2503 (11.72) | 362 (9.12) | 2915 (11.46) | 3277 (11.14) | |||
| 65–74 | 459 (6,62) | 2002 (8.91) | 479 (5.95) | 1982 (9.28) | 196 (4.94) | 2265 (8.90) | 2461 (8.37) | |||
| 75–84 | 392 (5,65) | 2492 (11.09) | 399 (4.96) | 2485 (11.64) | 126 (3.18) | 2758 (10.84) | 2884 (9.81) | |||
| >85 | 255 (3,68) | 2027 (9.02) | 257 (3.19) | 2025 (9.48) | 55 (1.39) | 2227 (8.75) | 2282 (7.76) | |||
| Sex, n (%) | ||||||||||
| Male | 3447 (49.68) | 11 635 (51.78) | 0.0056 | 3963 (49.22) | 11 119 (52.07) | <0.0001 | 2106 (53.07) | 12 976 (51.01) | 0.0086 | 15 082 (51.29) |
| Female | 3397 (48.96) | 10 575 (47.06) | 3986 (49.50) | 9986 (46.76) | 1804 (45.46) | 12 168 (47.83) | 13 972 (47.51) | |||
| Missing data | 94 (1.35) | 259 (1.15) | 103 (1.28) | 250 (1.17) | 58 (1.46) | 295 (1.16) | 353 (1.20) | |||
| Supplementary health insurance, n (%) | ||||||||||
| None | 590 (8.50) | 1366 (6.08) | <0.0001 | 650 (8.07) | 1306 (6.12) | <0.0001 | 341 (8.59) | 1615 (6.35) | <0.0001 | 1956 (6.65) |
| Universal complementary health coverage | 637 (9.18) | 1489 (6.63) | 755 (9.38) | 1371 (6.42) | 406 (10.23) | 1720 (6.76) | 2126 (7.23) | |||
| Private | 4664 (67.22) | 16 373 (72.87) | 5614 (69.72) | 15 423 (72.22) | 2548 (64.21) | 18 489 (72.68) | 21 037 (71.54) | |||
| Missing data | 1047 (15.09) | 3241 (14.42) | 1033 (12.83) | 3255 (15.24) | 673 (16.96) | 3615 (14.21) | 4288 (14.58) | |||
| Health insurance, n (%) | ||||||||||
| None or state medical assistance | 212 (3.06) | 461 (2.05) | <0.0001 | 229 (2.84) | 444 (2.08) | <0.0001 | 140 (3.53) | 533 (2.10) | <0.0001 | 673 (2.29) |
| Public health insurance | 6021 (86.78) | 19 698 (87.67) | 7161 (88.93) | 18 558 (86.90) | 3365 (84.80) | 22 354 (87.87) | 25 719 (87.46) | |||
| Missing data | 705 (10.16) | 2310 (10.28) | 662 (8.22) | 2353 (11.02) | 463 (11.67) | 2552 (10.03) | 3015 (10.25) | |||
| Employed status, n (%) | ||||||||||
| Employed | 2860 (41.22) | 8429 (37.51) | <0.0001 | 3641 (45.22) | 7648 (35.81) | <0.0001 | 1737 (43.78) | 9552 (37.55) | <0.0001 | 11 289 (38.39) |
| Unemployed | 624 (8.99) | 1438 (6.40) | 695 (8.63) | 1367 (6.40) | 390 (9.83) | 1672 (6.57) | 2062 (7.01) | |||
| Inactive | 2504 (36.09) | 9702 (43.18) | 2762 (34.30) | 9444 (44.22) | 1199 (30.22) | 11 007 (43.27) | 12 206 (41.51) | |||
| Missing data | 950 (13.69) | 2900 (12.91) | 954 (11.85) | 2896 (13.56) | 642 (16.68) | 3208 (12.61) | 3850 (13.09) | |||
| Level of education, n (%) | ||||||||||
| High-school graduation or less | 4436 (63.94) | 13 867 (61.72) | 0.0026 | 5225 (64.89) | 12 078 (61.24) | <0.0001 | 2446 (61.64) | 15 857 (62.33) | 0.4834 | 18 303 (62.24) |
| More than high school graduation | 1048 (15.11) | 3516 (15.65) | 1328 (16.49) | 3236 (15.15) | 641 (16.15) | 3923 (15.42) | 4564 (15.52) | |||
| Missing data | 1454 (20.96) | 5086 (22.64) | 1499 (18.62) | 5041 (23.61) | 881 (22.20) | 5659 (22.25) | 6540 (22.24) | |||
| Residence, n (%) | ||||||||||
| Home | 6100 (87.92) | 19 497 (86.77) | <0.0001 | 7299 (90.65) | 18 298 (85.68) | <0.0001 | 3477 (87.63) | 22 129 (86.95) | <0.0001 | 25 597 (87.04) |
| Institution | 163 (2.35) | 892 (3.97) | 142 (1.76) | 913 (4.28) | 49 (1.23) | 1006 (3.95) | 1055 (3.59) | |||
| Other | 675 (9.73) | 2080 (9.26) | 611 (7.59) | 2144 (10.04) | 442 (11.14) | 2313 (9.09) | 2755 (9.37) | |||
| Having a GP, n (%) | ||||||||||
| Yes | 5930 (85.47) | 19 816 (88.19) | <0.0001 | 7025 (87.25) | 18 721 (87.67) | <0.0001 | 3222 (81.20) | 22 524 (88.54) | <0.0001 | 25 746 (87.55) |
| No | 603 (8.69) | 1334 (5.94) | 665 (8.26) | 1272 (5.96) | 387 (9.75) | 1550 (6.09) | 1937 (6.59) | |||
| Missing data | 405 (5.84) | 1319 (5.87) | 362 (4.50) | 1362 (6.38) | 359 (9.05) | 1365 (5.37) | 1724 (5.86) | |||
| ED visit characteristics | ||||||||||
| Chief complaint of ED visit, n (%) | ||||||||||
| Medical complaint | 4622 (66.62) | 13 107 (58.33) | <0.0001 | 5250 (65.20) | 12 479 (58.44) | <0.0001 | 2702 (68.09) | 15 027 (59.07) | <0.0001 | 17 729 (60.29) |
| Traumatic injury | 1746 (25.16) | 7322 (32.59) | 2335 (29.00) | 6733 (31.53) | 773 (19.48) | 8295 (32.61) | 9068 (30.84) | |||
| Missing data | 570 (8.22) | 2040 (9.08) | 467 (5.80) | 2143 (10.04) | 493 (12.42) | 2117 (8.32) | 2610 (8.88) | |||
| Onset of complaint, n (%) | ||||||||||
| The day of ED visit | 2638 (38.02) | 11 713 (52.13) | <0.0001 | 3577 (44.42) | 10 774 (50.45) | <0.0001 | 1607 (40.50) | 12 744 (50.10) | <0.0001 | 14 351 (48.80) |
| Before the day of ED visit | 3773 (54.38) | 8866 (39.46) | 4058 (50.40) | 8581 (40.18) | 1907 (48.06) | 10 732 (42.19) | 12 639 (42.98) | |||
| Missing data | 527 (7.60) | 1890 (8.41) | 417 (5.18) | 2000 (9.37) | 454 (11.44) | 1963 (7.72) | 2417 (8.22) | |||
| Time of ED arrival, n (%) | ||||||||||
| 08:00–20:00 | 5069 (73.06) | 16 682 (74.24) | 0.0496 | 5731 (71.17) | 16 020 (75.02) | <0.0001 | 2689 (67.77) | 19 062 (74.93) | <0.0001 | 21 751 (73.97) |
| 20:00–08:00 | 1869 (26.94) | 5787 (25.76) | 2321 (28.83) | 5335 (24.98) | 1279 (32.23) | 6377 (25.07) | 7656 (26.03) | |||
| Distance from home to ED, n (%) | ||||||||||
| ≤10 km | 4372 (63.02) | 13 129 (58.43) | <0.0001 | 5102 (63.36) | 12 399 (58.06) | <0.0001 | 2601 (65.55) | 14 900 (58.57) | <0.0001 | 17 501 (59.51) |
| >10 km | 2386 (34.39) | 8740 (38.90) | 2751 (34.17) | 8375 (39.22) | 1267 (31.93) | 9859 (38.76) | 11 126 (37.83) | |||
| Missing data | 180 (2.59) | 600 (2.67) | 199 (2.47) | 581 (2.72) | 100 (2.52) | 680 (2.67) | 780 (2.65) | |||
| Type of resources used, n (%) | ||||||||||
| Radiological imaging | 2052 (29.58) | 12 681 (56.44) | <0.0001 | 2527 (31.38) | 12 206 (57.16) | <0.0001 | ** | ** | 14 733 (50.10) | |
| Blood tests | 1511 (21.78) | 11 328 (50.42) | <0.0001 | 1940 (24.09) | 10 899 (51.04) | <0.0001 | ** | ** | 12 839 (43.66) | |
| Therapeutic care | 1702 (24.53) | 11 254 (50.09) | <0.0001 | 2359 (29.30) | 10 597 (49.62) | <0.0001 | ** | ** | 12 956 (44.06) | |
| Inappropriateness in other measures, n (%) | ||||||||||
| Appropriate use score method | ** | ** | 4800 (59.61) | 2138 (10.01) | 2303 (58.04) | 4625 (18.20) | 6938 (23.59) | |||
| GP possible use method | 4800 (69.18) | 3252 (14.47) | ** | ** | 2463 (62.07) | 5573 (21.93) | 8052 (27.38) | |||
| Resource utilisation method | 2303 (33.19) | 1665 (7.41) | 2463 (30.59) | 1505 (7.05) | ** | ** | 3968 (13.49) | |||
ED, emergency department; GP, general practitioner.
bmjqs-2019-009396supp001.pdf (90.5KB, pdf)
For half of the participants (n=14 351), the symptoms had been present for <24 hours and the chief complaint concerned traumatic injuries for 30.8% (n=9068) (table 1). About 74% (n=21 751) of patients had consulted during the usual hours of outpatient care (08:00–20:00 hours).
Reasons and motivations for ED visits
The three most common motivations for the ED visit were because the patient had an accident (29.2%, n=8591), based on a doctor’s advice (27.3%, n=8027) or because the patient felt that their problem needed to be dealt with promptly (26.9%, n=7919) (table 2). Almost 9% (n=2568) of patients reported being anxious and not knowing where to consult. About 7% (n=2087) and 5% (n=1429) of patients reported having consulted an ED because it was faster than obtaining an appointment with their GP or because their GP was not available.
Table 2.
Reasons and motivations for ED visits
| Appropriateuse score method | PossibleGP use method | Resourceutilisation method | Total | |||||||
| Inappropriate ED use | Appropriate ED use | P value | Inappropriate ED use | Appropriate ED use | P value | Inappropriate ED use | Appropriate ED use | P value | ||
| Because the patient was a victim of an accident | 1575 (22.70) | 7016 (31.23) | <0.0001 | 2149 (26.69) | 6442 (30.17) | <0.0001 | 858 (21.62) | 7733 (30.40 | <0.0001 | 8591 (29.21) |
| On doctor’s advice | 1476 (21.27) | 6551 (29.16) | <0.0001 | 1472 (18.28) | 6555 (30.70) | <0.0001 | 672 (16.94) | 7355 (28.91) | <0.0001 | 8027 (27.30) |
| Because the patient needed the problem to be fixed quickly | 2069 (29.82) | 5850 (26.04) | <0.0001 | 2609 (32.40) | 5310 (24.87) | <0.0001 | 1262 (31.80) | 6657 (26.17) | <0.0001 | 7919 (26.93) |
| Because patient could have blood tests or radiology imaging | 1528 (22.02) | 4803 (21.38) | 0.2514 | 1818 (22.58) | 4513 (21.13) | 0.0072 | 658 (16.58) | 5673 (22.30) | <0.0001 | 6331 (21.53) |
| Because of ED proximity | 1580 (22.77) | 4685 (20.85) | 0.0006 | 2042 (25.36) | 4223 (19.78) | <0.0001 | 978 (24.65) | 5287 (20.78) | <0.0001 | 6265 (21.30) |
| Because the patient thought the problem was serious | 1465 (21.12) | 4328 (19.26) | 0.0007 | 1888 (23.45) | 3905 (18.29) | <0.0001 | 806 (20.31) | 4987 (19.60) | 0.2965 | 5793 (19.70) |
| Because firefighters or emergency responders bring the patient to ED | 500 (7.21) | 3544 (15.77) | <0.0001 | 624 (7.75) | 3420 (16.01) | <0.0001 | 259 (6.53) | 3785 (14.88) | <0.0001 | 4044 (13.75) |
| Because it was possible to see a specialist physician | 788 (11.36) | 2355 (10.48) | 0.0388 | 769 (9.55) | 2374 (11.12) | 0.0001 | 421 (10.61) | 2722 (10.70) | 0.8641 | 3143 (10.69) |
| Because the patient was anxious and did not know where to consult | 912 (13.14) | 1656 (7.37) | <0.0001 | 1066 (13.24) | 1502 (7.03) | <0.0001 | 532 (13.41) | 2036 (8.00) | <0.0001 | 2568 (8.73) |
| Because the patient thought it was faster to wait in the ED than obtain an appointment | 793 (11.43) | 1294 (5.76) | <0.0001 | 923 (11.46) | 1164 (5.45) | <0.0001 | 420 (10.58) | 1667 (6.55) | <0.0001 | 2087 (7.10) |
| Because the patient thought he would be hospitalised | 225 (3.24) | 1234 (5.49) | <0.0001 | 254 (3.15) | 1205 (5.64) | <0.0001 | 94 (2.37) | 1365 (5.37) | <0.0001 | 1459 (4.96) |
| Because the GP was not available | 466 (6.72) | 963 (4.29) | <0.0001 | 643 (7.99) | 786 (3.68) | <0.0001 | 277 (6.98) | 1152 (4.53) | <0.0001 | 1429 (4.86) |
| Because the patient had already consulted but the problem was not better | 451 (6.50) | 931 (4.14) | <0.0001 | 470 (5.84) | 912 (4.27) | <0.0001 | 245 (6.17) | 1137 (4.47) | <0.0001 | 1382 (4.70) |
| Because the patient needed biological or radiological examinations and could not have an appointment | 405 (5.84) | 905 (4.03) | <0.0001 | 478 (5.94) | 832 (3.90) | <0.0001 | 242 (6.10) | 1068 (4.20) | <0.0001 | 1310 (4.45) |
| Because the patient tried self-care but it did not work | 453 (6.53) | 798 (3.55) | <0.0001 | 564 (7.00) | 687 (3.22) | <0.0001 | 264 (6.65) | 987 (3.88) | <0.0001 | 1251 (4.25) |
| Because it is possible to be seen by a doctor beyond the working hours | 222 (3.20) | 441 (1.96) | <0.0001 | 267 (3.32) | 396 (1.85) | <0.0001 | 138 (3.48) | 525 (2.06) | <0.0001 | 663 (2.25) |
| Because there was no GP available | 242 (3.49) | 385 (1.71) | <0.0001 | 308 (3.83) | 319 (1.49) | <0.0001 | 158 (3.98) | 469 (1.84) | <0.0001 | 627 (2.13) |
| Because the patient did not have to pay for care | 256 (3.69) | 339 (1.51) | <0.0001 | 275 (3.42) | 320 (1.50) | <0.0001 | 145 (3.65) | 450 (1.77) | <0.0001 | 595 (2.02) |
| Because there was no GP doing home visits | 82 (1.18) | 247 (1.10) | 0.5674 | 120 (1.49) | 209 (0.98) | 0.0002 | 46 (1.16) | 283 (1.11) | 0.7943 | 329 (1.12) |
| Because the patient could not stay at home | 14 (0.20) | 58 (0.26) | 0.4065 | 13 (0.16) | 59 (0.28) | 0.0756 | 5 (0.13) | 67 (0.26) | 0.1034 | 72 (0.24) |
ED, emergency department; GP, general practitioner.
Characteristics of EDs and counties
More than 80% of patients (80.7%; n=23 738) consulted an ED in a public hospital (academic and non-academic; table 3). About half (47%; n=13 811) sought care in an ED with <30 000 visits per year and about 26% (n=7570) in an ED with >45 000 visits per year. For 59.5% of patients (n=17 501), the distance from home to the ED was ≤10 km (table 1). County medical density was considered high and low for 51.7% (n=15 916) and 38.8% (n=11 695) of patients, respectively.
Table 3.
Characteristics of EDs
| % | n | |
| Type of hospital visited | ||
| Public academic | 12.56 | 80 |
| Public non-academic | 65.31 | 416 |
| Not-for-profit private | 6.59 | 42 |
| For-profit private hospitals | 15.54 | 99 |
| Annual visits of ED visited | ||
| ≤15 000 | 26.06 | 166 |
| 15 000–30 000 | 41.92 | 267 |
| 30 000–45 000 | 19.15 | 122 |
| >45 000 | 12.87 | 82 |
| County medical density | ||
| Low | 42.54 | 271 |
| Intermediate to high | 57.46 | 366 |
ED, emergency department.
Appropriateness of ED use
Among the 29 407 patients, respectively, 23.6% (n=6938), 27.4% (n=8052) and 13.5% (n=3968) were considered to have inappropriate ED use considering the appropriateness score, possible GP use and resource utilisation. Overall, 1812 patients (6.16%) were considered inappropriate according to all method measures. Lack of availability of the GP, anxiety about knowing where to consult and the possibility of seeing a doctor after working hours and not paying for care were reported significantly more often by patients with inappropriate versus appropriate use, regardless of the measure method used (p<0.0001) (table 2).
Multilevel logistic regression model
Regardless of the measure method used, likelihood of inappropriate use decreased with age and distance from home to the ED >10 km (table 4). It also increased with female sex, patient’s probability of not having reported a private supplementary health insurance, having universal supplementary health coverage and presenting symptoms several days old. Likelihood of inappropriate ED use did not seem associated with county medical density. Living in institution was associated with lower likelihood of inappropriate use considering possible GP use and resource utilisation but not appropriateness score. Having a GP was associated with lower likelihood of inappropriate use considering possible GP use but not with the appropriateness score and resource utilisation. Sensitivity analyses are available in online supplementary table 2. Results for a threshold of 5 are similar to the reference threshold of 4. Results for the threshold of 3 are quite similar to the reference threshold except for having a GP and number of annual visits for the ED visited.
Table 4.
Multilevel logistic regression model of determinants of inappropriate use of EDs
| Appropriate use score method | Possible GP use method | Resource utilisation method | |||||||
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | ||||
| Patient characteristics | |||||||||
| Age, years | |||||||||
| 15–24 | Ref | Ref | Ref | ||||||
| 25–34 | 0.799 | 0.716 | 0.891 | 0.810 | 0.732 | 0.895 | 0.872 | 0.767 | 0.990 |
| 35–44 | 0.721 | 0.642 | 0.809 | 0.708 | 0.636 | 0.787 | 0.755 | 0.658 | 0.865 |
| 45–54 | 0.640 | 0.568 | 0.722 | 0.595 | 0.533 | 0.665 | 0.710 | 0.616 | 0.817 |
| 55–64 | 0.556 | 0.490 | 0.631 | 0.485 | 0.431 | 0.546 | 0.509 | 0.434 | 0.598 |
| 65–74 | 0.475 | 0.406 | 0.555 | 0.413 | 0.356 | 0.478 | 0.401 | 0.325 | 0.495 |
| 75–84 | 0.344 | 0.292 | 0.406 | 0.296 | 0.253 | 0.347 | 0.240 | 0.188 | 0.307 |
| >85 | 0.242 | 0.196 | 0.300 | 0.237 | 0.194 | 0.288 | 0.136 | 0.094 | 0.199 |
| Sex | |||||||||
| Male | Ref | Ref | Ref | ||||||
| Female | 1.242 | 1.160 | 1.331 | 1.270 | 1.192 | 1.354 | 1.133 | 1.040 | 1.233 |
| Supplementary health insurance | |||||||||
| Private | Ref | Ref | Ref | ||||||
| Universal complementary health coverage | 1.150 | 1.014 | 1.305 | 1.190 | 1.058 | 1.338 | 1.331 | 1.150 | 1.541 |
| None | 1.342 | 1.170 | 1.539 | 1.160 | 1.018 | 1.322 | 1.268 | 1.075 | 1.497 |
| Health insurance | |||||||||
| Public health insurance | Ref | Ref | Ref | ||||||
| None or state medical assistance | 1.192 | 0.932 | 1.525 | 1.142 | 0.905 | 1.441 | 1.241 | 0.943 | 1.632 |
| Employment status | |||||||||
| Employed | Ref | Ref | Ref | ||||||
| Unemployed | 1.044 | 0.921 | 1.184 | 0.899 | 0.798 | 1.012 | 0.964 | 0.831 | 1.120 |
| Inactive | 0.956 | 0.865 | 1.056 | 0.875 | 0.798 | 0.961 | 0.906 | 0.804 | 1.022 |
| Level of education | |||||||||
| High-school graduation or less | Ref | Ref | Ref | ||||||
| More than high-school graduation | 0.889 | 0.813 | 0.972 | 0.919 | 0.847 | 0.997 | 0.943 | 0.847 | 1.050 |
| Residence | |||||||||
| Home | Ref | Ref | Ref | ||||||
| Institution | 0.798 | 0.613 | 1.038 | 0.629 | 0.483 | 0.820 | 0.661 | 0.445 | 0.982 |
| Other | 0.858 | 0.647 | 1.138 | 0.705 | 0.535 | 0.928 | 0.744 | 0.523 | 1.058 |
| Having a GP | |||||||||
| No | Ref | Ref | Ref | ||||||
| Yes | 0.902 | 0.784 | 1.038 | 0.859 | 0.755 | 0.978 | 0.926 | 0.786 | 1.091 |
| ED visit characteristics | |||||||||
| Onset of complaint | |||||||||
| The day of ED visit | Ref | Ref | Ref | ||||||
| Before the day of ED visit | 2.094 | 1.951 | 2.248 | 1.535 | 1.439 | 1.638 | 1.499 | 1.374 | 1.635 |
| Time of ED arrival | |||||||||
| 08:00–20:00 | Ref | Ref | Ref | ||||||
| 20:00–08:00 | 1.083 | 0.999 | 1.175 | 1.170 | 1.086 | 1.260 | 1.358 | 1.234 | 1.494 |
| Distance from home to ED | |||||||||
| ≤10 km | Ref | Ref | Ref | ||||||
| >10 km | 0.886 | 0.822 | 0.955 | 0.850 | 0.794 | 0.911 | 0.831 | 0.758 | 0.912 |
| ED characteristics | |||||||||
| Type of hospital visited | |||||||||
| Public academic | Ref | Ref | Ref | ||||||
| Public non-academic | 1.253 | 0.998 | 1.573 | 1.198 | 1.011 | 1.421 | 1.025 | 0.824 | 1.275 |
| Not-for-profit private | 0.953 | 0.681 | 1.334 | 0.844 | 0.655 | 1.089 | 0.880 | 0.635 | 1.219 |
| For-profit private | 0.659 | 0.498 | 0.872 | 0.722 | 0.585 | 0.892 | 0.871 | 0.665 | 1.141 |
| Annual visits for the ED visited | |||||||||
| ≤15 000 | Ref | Ref | Ref | ||||||
| 15 000–30 000 | 1.234 | 1.020 | 1.493 | 1.008 | 0.869 | 1.169 | 0.826 | 0.683 | 1.001 |
| 30 000–45 000 | 1.187 | 0.954 | 1.478 | 1.042 | 0.881 | 1.232 | 0.783 | 0.630 | 0.973 |
| >45 000 | 1.329 | 1.044 | 1.692 | 1.033 | 0.859 | 1.241 | 0.958 | 0.758 | 1.212 |
| County medical density | |||||||||
| Low | Ref | Ref | Ref | ||||||
| Intermediate to high | 1.010 | 0.873 | 1.170 | 0.983 | 0.879 | 1.099 | 1.002 | 0.868 | 1.158 |
Significant results are in light colour (versus non-significant in dark colour).
aOR, adjusted OR; ED, emergency department; GP, general practitioner; Ref, reference.
Discussion
In this study, we have investigated the socioeconomic and demographic factors associated with inappropriate ED use by including data from all EDs on a national scale and by using different types of measures of ED appropriateness use. Our results confirmed one of our two hypotheses as we found an association between inappropriate use of ED and some indicators of socioeconomic vulnerability but not with the county medical density. In our multilevel model, age, sex, supplementary health insurance coverage, onset of complaint and distance from home to ED remained significant, independent of the method used to define inappropriate use of the ED. Some results were consistent with previous studies. Young age,18–20 female sex11 19 20 58 59 and symptoms several days old18 52 were previously found associated with a higher likelihood of inappropriate ED use. Some studies have underlined the association between poor or no supplementary health coverage and social health inequalities in both care access29–31 and frequency of ED visits.24 29–31
Patients >65 years corresponded to 25.9% of ED patients versus 17.6% in the general population in 2013 and those >75 years corresponded to 17.6% versus 9% in the general population.60
Our results help in understanding the impact of supplementary health coverage on ED use. Whatever the method of ED appropriateness measure used, we found increased likelihood of inappropriate ED associated with not having supplementary health coverage or having CMU-c. Supplementary health coverage is directly linked to the level of reimbursement (and copayment expenses) and has been identified as one of the financial reasons for not seeking care.61 In our study population, 7.2% and 71.5% reported CMU-c or a private health insurance coverage as compared with 6.8% and 89% in the general population.62 Moreover, 2% of patients reported visiting an ED because they think they did not have to pay for their care, and this percentage was significantly higher for patients with inappropriate use (regardless of the measure method used). In France, healthcare is first paid by the patient, who is then reimbursed in part by the public health insurance. The reinsurable copayments are then covered by the supplementary health insurance coverage, when the patient has coverage. In some cases (some chronic illness and pregnancy in particular), care is directly paid by the public health insurance, called ‘third-party payment’. A reform to the generalisation of third-party payment to the entire population, as in most Europe countries, has been discussed but has not been implemented.63 64 We assume that the generalisation of the third-party payment could positively affect both health behaviour and ED use.
All these results probably reflect two major considerations: first, delay in seeking care and treatment—relative to financial and social difficulties in care access—may explain part of the overall increased use of EDs.38 39 65–69 Second, not seeking healthcare for financial reasons may contribute to distress experienced by the patient. Distress has been described as related to physiological health, spiritual health or social support, and patients’ discharge diagnoses might be trivial in the context of their stories.13 This distress experienced by the patient may induce a displacement of non-urgent consultations from primary care to the ED.
A part of our work was to analyse the possible links between individual and environmental characteristics with inappropriate ED use. However, contrary to our hypothesis, in the multilevel logistic regression model, likelihood of inappropriate ED use was not associated with county medical density, whatever the measure method used. The heterogeneity of medical density in the same county might explain the lack of significant results. This explanation seems even more likely because it agrees with results from our empty models. As explained in the Methods section, we did not find intergroup heterogeneity at the county level which justified the use of a third level in our models. The impact of medical density might not be at the county level but rather at a smaller geographical one. In the last decade, several studies have investigated indicators of access to care, territorial distribution of physicians and medical ‘deserts’.70–72 These indicators tend to take into account both the proximity and availability of doctors, as well as local demand for care, and have been described as more efficient than traditional indicators of medical density.72 Completing our analysis with data from these indicators of patients’ local district might be revealing. However, for reasons of statistical confidentiality, the local district of each patient was not available.
About 7% and 5% of patients reported having consulted at an ED because it was faster than obtaining an appointment or because their GP was not available. This percentage was about twice as high with inappropriate versus appropriate ED use (regardless of the measure method used). And for about 30% and 20% of patients with inappropriate ED use according to EP judgement (appropriateness score and possible GP use methods), ED visits included EP consult as well as radiological examinations or blood tests. Only 1812 (6.16%) patients were considered inappropriate according to all three measures (more when focusing on only inappropriate use score and possible GP use). Considering all barriers to outpatient care access previously discussed and leading to an ED visit (not able to pay out-of-pocket expenses and difficulties in obtaining appointments), the concept of inappropriate ED use itself may not be appropriate because of no other choice than visiting an ED. First, our results show that individualising how patients would be considered as ‘inappropriate’ from any point of view is difficult. Also, to the extent that the doctors seem to have difficulty defining what is appropriate or not, how could we expect patients to? Here, our work focused on EP’s point of view and resource utilisation but did not consider the patient’s view of urgency either at the time of arrival nor at the end of the ED visit. Thus, as previously discussed, defining and measuring the appropriateness of ED use is difficult and is highly depending on whether we considered patient’s or healthcare provider’s/system’s perspectives. Some ED visits might be considered as inappropriate from the EP’s perspective but would be appropriate considering the patient’s point of view either because they felt that their condition was urgent or because of no other alternative for healthcare access.
Additional primary care appointments during out-of-hours might be a way to reduce ED attendance, as it was suggested by the results of a large study in the Greater Manchester Area.73 However, other studies have found that extending opening hours in the evenings and at weekends in the UK were only modestly associated with patient satisfaction74 and that its association with the use of emergency hospital services was small or inconsistent.75 Urgent care centres (UCCs) have also been implemented in the USA and UK and were intended to reduce rates of ED visits and short-stay emergency admissions to hospital. However, more research is needed to examine the effect of the introduction of the UCCs on the frequency of ED attendance and emergency admissions to hospital, especially when the UCC is not colocated with the ED.76
In our study, almost 10% of patients reported being anxious and not knowing where to consult, significantly higher among patients with inappropriate versus appropriate ED use (regardless of the measure method used). Even though there are other options for unscheduled care (including out-of-hours time), it appears here that some patients could have self-referred to the ED because of lack of knowledge about the offer of unscheduled care or because of system deficiency (insufficient availability of out-of-hours consultation). Even with a more efficient system of out-of-hours consultations or UCCs, we do not know whether this anxiety (or urgency felt) did not lead the patient to the ED anyway. All these results suggest that educating the public about unscheduled care offer as well as public policies (whose goal would be to develop and promote alternatives to ED) could be enhanced.77
Limitations
Our study has several limitations. The first limitation is related to the missing data, including on our outcomes of interest, which led to the exclusion of some patients and therefore risk of attrition bias. The second limitation is that one of our method to measure appropriateness, the appropriateness score, was based on the subjective assessment of the caring physician (based on a numeric scale) at the end of the ED visit, which may lead to a possible measurement bias. However, the authors have preferred to split the outcome of interest into two categories, which allowed us to identify 20% of patients with the least appropriate use of ED among all patients. After comparison with possible GP consult and resource utilisation, the results from our multilevel regression model for the appropriateness score are consistent with the other measures. It suggests that even if the assessment of appropriateness by the caring physician is subjective, it was associated with the resource use and so, the fact that the patient could have been managed by a GP. As explained earlier in the discussion, measuring the appropriateness of ED use remains difficult and strongly depends on the chosen perspective, as well as the method used. Here, the data from the survey did not allow us to consider the patient’s perspective.
Conclusion
Our results suggest that inappropriate ED use was more likely among individuals presenting some indicators of socioeconomic vulnerability (eg, not having supplementary health coverage or having universal health coverage for people with lower income), but we did not find an association with the county medical density. Our results make us question the appropriateness of the concept of inappropriate ED use because it does not consider the distress experienced by the patient, and segments of society seem to have few other choices to access healthcare than the ED (lack of healthcare coverage and/or lack of physician availability).
Acknowledgments
We thank all the members of the French Society of Emergency Medicine, the members of the French Society of Emergency Medicine Collaborators group and most particulary all the members of the French Society of Emergency Medicine Evaluation and Quality Committee for their help: Dr Sandra Bernard, Dr Jean Marie Bonnec, Dr Vincent Bounes, Dr Bahram Chaybany, Dr Romain Dufau, Dr Sybille Goddet, Dr Alban Guibert, Dr Romain Hellmann, Dr Mohamed Hachelaf, Dr Jean Yves Lardeur, Dr Philippe Leveau, Dr Claire Mauriat, Dr Pascale Nelh, Dr Carole Paquier, Dr Catherine Pradeau, Dr François Revaux, Dr Patrice Serre, Dr Jean Pierre Tourtier, Dr Gilles Viudes.
Footnotes
Twitter: @yordayou
French Society of Emergency Medicine Collaborators group: We woud like all members of the Frenche Society of Emergency Medicine who helped filling the questionnaire on the day of the survey: Abalea L, MD (Brest), Abdelhadi M, MD (Chalautre la Petite), Achouri A, MD (Libourne), Adi O, MD (St Jean d’Angely), Agbessi A, MD (Boulogne Billancourt), Ahmed M, MD (Koungou), Ait Ali M, MD (Amboise), Ait Idir T, MD (Arnas), Ait Oual A, MD (St Amand Montrond), Akendegue J, MD (Bourgoin Jallieu), Al Bourgol S, MD (Ambilly), Al Tabchi A, MD (Belmont-sur-Vair), Alarcon P, MD (Maubeuge), Alayrangues G, MD (St Barthelemy—Antilles), Alazia M, MD (Marseille), Alazia ML, MD (Marseille), Albert J, MD (Cabestany), Alexander R, MD (Appilly), Allix V, MD (Le Mans), Amama H, MD (Auxerre), Amellal F, MD (Narbonne), Amiens E, MD (Issoire), Amrane A, MD (Le Blanc Mesnil), Ancelin P, MD (Mont de Marsan), Andre A, MD (Pontarlier), Andritsakis O, MD (L’Union), Andronikof M, MD (Clamart), Anfart E, MD (Biarritz), Arabeyre G, MD (Melun), Arnault F, MD (Vannes), Ascofare IC, MD (Amilly), Asdrubal J, MD (Macon), Auroy V, MD (Pontivy), Bah T, MD (Bordeaux), Bailly B, MD (Chaumont), Ballestrazzi V, MD (Armentieres), Ballouz M, MD (Provins), Bandaly F, MD (Vierzon), Banihachemi JJ, MD (Echirolles), Bar C, MD (Brignoles), Barriere P, MD (Nantes), Bartou C, MD (Villeneuve-sur-Lot), Bassil J, MD (Laval), Battaglini P, MD (Aubagne), Baudot V, MD (Le Pont de Beauvoisin), Baugnon D, MD (Verdun), Baure JJ, MD (Rochetaillee), Beaujean F, MD (Tulle), Bedioui A, MD (Almont les Junies), Begnis R, MD (Champagnole), Belabbas H, MD (Ales), Belkhodja H, MD (Compiegne), Bello M, MD (Royan), Benabbas S, MD (Amecourt), Benadda A, MD (Perigueux), Benaissa A, MD (Arnas), Bengrina M, MD (Remiremont), Benmouffok A, MD (L’Aigle), Benmoulai A, MD (Les Adjots), Bennour A, MD (Lille), Benoit D, MD (Baratier), Bergeron C, MD (Villeneuve St Georges), Bersou M, MD (Moissac), Bertheil S, MD (Dax), Billaud N, MD (Metz), Bissolokele P, MD (Fougueyrolles), Blenet JC, MD (Perpignan), Blondeel D, MD (Paris), Blum O, MD (St Priest), Bonelle P, MD (Autheux), Bongrand C, MD (Nogent-sur-Marne), Borel-Kuhner J, MD (Eaubonne), Borsa-Dorion A, MD (Vandoeuvre les Nancy), Bouayad-Agha K, MD (Strasbourg), Boubakar L, MD (Apt), Boubia T, MD (Cosne Cours-sur-Loire), Bouguellid M, MD (Quimperle), Boularan J, MD (Castres), Boumpoutou R, MD (Pau), Bouquillon J, MD (Lille), Bourgeois S, MD (Avignon), Bousquet A, MD (Saintes), Bouvet P, MD (Agones), Brabander D, MD (L’Aiguillon), Braconnier L, MD (St Quentin), Braud F, MD (Cesson Sevigne), Braun F, MD (Metz), Braun JB, MD (Montbeliard), Braun JB, MD (Belfort), Breant I, MD (Livry-sur-Seine), Brilland R, MD (Tarare), Brochet F, MD (Montlucon), Bronet N, MD (Lille), Brousse B, MD (Louviers), Broustal E, MD (Pointe-à-Pitre), Brouste Y, MD (Fort de France), Bulle S, MD (Decines Charpieu), Bultez B, MD (Sisteron), Burckel S, MD (Digne les Bains), Burin B, MD (Nantes), Busseuil C, MD (Montelimar), Cabirol L, MD (Lunel), Campagne J, MD (Guilherand Granges), Canivet I, MD (Fort de France), Capelle P, MD (Nimes), Carbajal R, MD (Paris), Cardona J, MD (Poitiers), Carolet C, MD (Reims), Carpentier F, MD (Grenoble), Carret V, MD (La Seyne-sur-Mer), Carret V, MD (Toulon), Castera F, MD (St Girons), Caucat C, MD (Le Chesnay), Caumon L, MD (Aurillac), Cauvy-Martin S, MD (Bagnols-sur-Ceze), Cavalli P, MD (Roanne), Cayarcy C, MD (Beaumont), Cayrel P, MD (Rodez), Chabaille E, MD (Compiegne), Chabot P, MD (Sedan), Chace A, MD (Villeneuve St Georges), Chaillan D, MD (Sarlat la Caneda), Chaillet O, MD (Thiers), Chakouri A, MD (Aubenas), Chamouilli JM, MD (Toulon), Champly F, MD (Cordon), Champvillard J, MD (Jonzac), Chantepie C, MD (La Ferte Bernard), Charestan P, MD (Aulnay-sous-Bois), Charles JY, MD (Autun), Charlier F, MD (Auberville la Campagne), Charpente F, MD (Montpellier), Charpentier E, MD (Clermont), Charpentier S, MD (Toulouse), Charroin D, MD (St Priest en Jarez), Chasle V, MD (Rennes), Chatoui F, MD (Montpellier), Chehab F, MD (Peronne), Chekroun A, MD (Blois), Cherhabil N, MD (Aire-sur-l’Adour), Cheron G, MD (Paris), Chery N, MD (Pont-à-Mousson), Chevallot N, MD (Romilly-sur-Seine), Chhuy F, MD (Stains), Chonion F, MD (Avallon), Choquet C, MD (Paris), Chretien C, MD (Charleville Mezieres), Claret M, MD (Agnin), Claudet I, MD (Toulouse), Claussner F, MD (Forbach), Cochet-Monier B, MD (Montmorency), Cohen D, MD (Reims), Cointin M, MD (Avignon), Cojocaru B, MD (Colombes), Cojocaru R, MD (Strasbourg), Colin B, MD (Carpentras), Colin-Gorski AM, MD (Argenteuil), Colombani G, MD (Buisson), Combes L, MD (Longjumeau), Comoz H, MD (Rouen), Compagnon F, MD (Coulommiers), Conduche C, MD (Neuilly-sur-Seine), Conte M, MD (Mende), Corege D, MD (Chalon-sur-Saone), Coste V, MD (Montauban), Costes P, MD (Creil), Couillard C, MD (Fontenay le Comte), Couleru G, MD (Pau), Courtot F, MD (Menton), Crepieux O, MD (St Lo), Crocheton N, MD (Champigny-sur-Marne), Crouan JL, MD (St Gregoire), Cueille N, MD (St Junien), Curac S, MD (Clichy), D’andigne E, MD (Villenave d’Ornon), Dabas JP, MD (Arthies), Dalmon F, MD (Chambery), Daoud P, MD (Montreuil), Daoudi M, MD (Beauvain), Darviot E, MD (Angers), De Albasini F, MD (Albiez le Jeune), De Bastard L, MD (Versailles), De Bouguelmouna H, MD (Lormont), De Cagny B, MD (Amiens), De Letter A, MD (Meaux), De Pontual L, MD (Bondy), De Talance M, MD (Epinal), De Touchard P, MD (Langon), Debas O, MD (Ambleon), Debuc E, MD (Paris), Dechaume JL, MD (St Avold), Decroix A, MD (Oyonnax), Degrange P, MD (Rillieux la Pape), Delaire L, MD (Angouleme), Delannoy X, MD (Montmorillon), Delefosse F, MD (Dreux), Delgado G, MD (Hyeres), Delporto S, MD (Quincy-sous-Senart), Demiere E, MD (Nemours), Demil H, MD (Saverne), Depil-Duval A, MD (Evreux), Dequin PF, MD (Chambray les Tours), Der Sahakian G, MD (Grillon), Descamps L, MD (Calmels Et le Viala), Deschamps P, MD (Ennery), Deshayes JL, MD (Le Mans), Desmettre T, MD (Besancon), Devienne J, MD (Arras), Deville F, MD (Limoges), Devos F, MD (Lievin), Deweerdt E, MD (St Gaudens), Dhaou H, MD (Aubergenville), Dheu C, MD (Colmar), Diallo D, MD (Brunelles), Diani A, MD (Acy Romance), Dianteill S, MD (Yerres), Dieckmann K, MD (Blois), Dinant L, MD (Porto Vecchio), Dizabo F, MD (Juvisy-sur-Orge), Dolhem P, MD (St Quentin), Donati JF, MD (Marseille), Douart-Leger C, MD (Neufchateau), Draou B, MD (St Claude), Dubart A, MD (Bethune), Dubouix F, MD (Toulouse), Duche M, MD (Auxerre), Ducreux B, MD (Arnas), Dugas L, MD (Campistrous), Duncan G, MD (Boulogne-sur-Mer), Dupeyron R, MD (Pont l’Abbe), Duplain C, MD (St Chamond), Dupuis E, MD (La Trinite en Martinique), Eckart P, MD (Caen), Ehlinger P, MD (Altkirch), El Andaloussi M, MD (Aubigny), El Arabi J, MD (Cognac), El Cadi T, MD (Vesoul), El Dalati S, MD (Le Blanc), El Idreissi T, MD (Aix en Diois), El Kohen R, MD (Lille), El-Bez M, MD (Evry), Elczar S, MD (Basse Terre), Elias O, MD (Gonesse), Epain D, MD (Lagny-sur-Marne), Escat F, MD (Muret), Escudier V, MD (Balesmes-sur-Marne), Eskandanian A, MD (Bourg en Bresse), Esturoune G, MD (St Jean de Luz), Eyer D, MD (Strasbourg), Faour A, MD (Bernay), Faranpour F, MD (Niort), Faure I, MD (Bordeaux), Favier P, MD (Hazebrouck), Favre-Mercuret C, MD (Apremont), Ferracci S, MD (Pointe-à-Pitre), Ferrand C, MD (Paimpol), Fiani N, MD (Chateau Thierry), Figuere P, MD (Marignane), Flodrops H, MD (St Pierre de la Réunion), Fontaine JP, MD (Paris), Foskett P, MD (Beziers), Fossay C, MD (Fontainebleau), Foucault J, MD (Flers), Fradin P, MD (La Roche-sur-Yon), Francini V, MD (Mantes la Jolie), Freys M, MD (Dijon), Frigui L, MD (Joigny), Fringant MJ, MD (Toul), Froger E, MD (Romans-sur-Isere), Fuzet A, MD (Agnat), Gaffinel C, MD (Etampes), Gaid M, MD (Montlucon), Galvez A, MD (Caen), Ganansia O, MD (Paris), Garitaine P, MD (Gassin), Garnier N, MD (Chassagny), Garraud P, MD (Gueret), Gaspari T, MD (Granville), Gauclere V, MD (Annonay), Gaudin B, MD (Vernon), Gelee C, MD (Lannion), Gelly JM, MD (Salon de Provence), Georges N, MD (Guingamp), Georget F, MD (Amilly), Gerardin D, MD (Beduer), Ghemari T, MD (Bagnolet), Gibey S, MD (Dole), Gilavert PJ, MD (Gien), Giraud I, MD (Montpellier), Glastre C, MD (Pringy), Gnansounou M, MD (Maubeuge), Godescence C, MD (Roubaix), Goix L, MD (Livry-sur-Seine), Gottwalles Y, MD (Colmar), Goulmy M, MD (Bar le Duc), Gouraud F, MD (Meaux), Gov C, MD (Ade), Govindoorazoo S, MD (Montlucon), Graille JP, MD (Aubagne), Griffet J, MD (Grenoble), Grizon-Samit V, MD (Perigueux), Guenot I, MD (Decize), Guenoun L, MD (La Ciotat), Guet L, MD (Trappes), Gueugniaud PY, MD (Lyon), Guibellino P, MD (Marseille), Guyet S, MD (Fontaine la Mallet), Guyon-Veuillet R, MD (Vitry le Francois), Haas H, MD (Nice), Haesevoets M, MD (Albertville), Hallouche D, MD (Argentan), Hamelin V, MD (Chenove), Hammel JL, MD (Tarbes), Hamza L, MD (Bobigny), Harchaoui S, MD (Lisieux), Harisolofo-Tafika J, MD (Crest), Hascoet JM, MD (Nancy), Hassam J, MD (Bastia), Hauet P, MD (Nantes), Hellio R, MD (Orsay), Henry R, MD (Alencon), Hernandez G, MD (Moulins), Herno E, MD (Redon), Herve T, MD (Pont Audemer), Hilal M, MD (Vendome), Ho Ba Tho JJ, MD (Massy), Houareau C, MD (Bourg St Maurice), Hourdin N, MD (Chateaubriant), Huet F, MD (Dijon), Humbert K, MD (Dieval), Hyrien JP, MD (Clamart), Idir C, MD (Bergerac), Immoune Y, MD (Troyes), Issa-Brunet L, MD (Mulhouse), Jacob F, MD (Millau), Jacob X, MD (Pierre Benite), Jacques-Antoine Y, MD (St Benoit de la Réunion), Jacquet V, MD (Orange), Jammes D, MD (Frejus), Janssen P, MD (Beauzelle), Javaud N, MD (Bondy), Javouhey E, MD (Bron), Jean P, MD (Marseille), Jedrecy C, MD (Dourdan), Job E, MD (Meudon), Joly LM, MD (Rouen), Joly M, MD (St Denis), Jomin E, MD (Orthez), Joseph-Louisia J, MD (St Martin—Antilles), Jourdain De Muizon J, MD (Loudun), Jouve JL, MD (Marseille), Kadi L, MD (Armes), Kadi M, MD (Ancenis), Kahn JP, MD (Airon Notre Dame), Kannass M, MD (Nevers), Kareh R, MD (Ermont), Kayemba Kay’s S, MD (Dreux), Kefif F, MD (Courchelettes), Kezza C, MD (St Laurent du Maroni), Kfoury M, MD (Abbeville), Khalaf L, MD (Any Martin Rieux), Khelaf M, MD (Creteil), Khodr Z, MD (St Omer), Kone-Pau I, MD (Le Kremlin Bicetre), Kops L, MD (Mulhouse), Kosayyer M, MD (Sarreguemines), Kozisek S, MD (Flers), Kristic S, MD (Paris), Labes P, MD (Bayonne), Labidi M, MD (Bayeux), Lablanche C, MD (Lyon), Lacampagne F, MD (Bourges), Lacrampe B, MD (Douai), Ladent JM, MD (Bruay la Buissiere), Lafforgue E, MD (Tarbes), Lafleur F, MD (Gonesse), Lagarde S, MD (Cagnes-sur-Mer), Lahlou H, MD (Vitry-sur-Seine), Laichour C, MD (Maisons Laffitte), Laisney N, MD (St Lo), Lamalle D, MD (Arches), Lamont P, MD (Agen), Lamrani C, MD (Beaulieu les Loches), Lanastre B, MD (Briancon), Langlais A, MD (Besancon), Lansade P, MD (Calvi), Lansari M, MD (Verneuil-sur-Avre), Lardeur JY, MD (Poitiers), Larroque D, MD (Toulouse), Lavagna L, MD (Montreuil), Lazaro L, MD (Bayonne), Lazim A, MD (Les Brunels), Lazzarotto D, MD (St Vallier), Le Dreff P, MD (Marseille), Le Gal C, MD (Les Sables d’Olonne), Le Gall C, MD (Argenteuil), Le Guen T, MD (Cayenne), Le Renard A, MD (Brix), Le Sire F, MD (Fontaine la Mallet), Lebars Y, MD (Burlats), Lecoules N, MD (Toulouse), Leflon L, MD (Epernay), Legagneur M, MD (Forbach), Legalloudec E, MD (Beauvais), Lehot H, MD (Metz), Lejri N, MD (Haguenau), Leloup P, MD (Saumur), Lepine T, MD (Abzac), Lepori M, MD (Soissons), Leroux L, MD (Pessac), Leroy C, MD (Colombes), Lesage P, MD (Chambery), Lestavel P, MD (Henin Beaumont), Leveau P, MD (Bressuire), Levraut J, MD (Nice), Levy M, MD (Evreux), Lher E, MD (Brest), Libong L, MD (Conflans-sur-Anille), Lignel M, MD (Mayenne), Lionel B, MD (Montauban), Louis F, MD (Grasse), Loup P, MD (Toulouse), Loyer A, MD (Alleuze), Lubrano O, MD (St Denis de la Réunion), Lucas F, MD (Escaufourt), Luhata J, MD (Denain), Luigi S, MD (Martigues), Lutz C, MD (St Julien en Genevois), Mado P, MD (Firminy), Magd S, MD (Nice), Mahai A, MD (Sarcelles), Maignal R, MD (Albi), Maillet L, MD (Castelnau de Guers), Maisonneuve A, MD (Valenciennes), Maitre O, MD (Orleans), Mangin Y, MD (Beziers), Mansour V, MD (Lisieux), Mansouri A, MD (Osny), Manya J, MD (Perpignan), Marchand D, MD (Fougeres), Marguet C, MD (Rouen), Marianne PJ, MD (St Pierre de la Réunion), Marin-Braun F, MD (Strasbourg), Marinthe B, MD (St Dizier), Mariotti JC, MD (Cherbourg Octeville), Marot Y, MD (Tours), Marquet JL, MD (Cellule), Martel E, MD (Evreux), Martelli V, MD (Ajaccio), Martin D, MD (La Chapelle du Noyer), Martin O, MD (Nancy), Martin-Delgado M, MD (Macon), Martin-Laval A, MD (Marseille), Martinet A, MD (Bethune), Martinez M, MD (Montbrison), Masmoudi R, MD (Paris), Massol V, MD (Dieppe), Matas O, MD (Vienne), Mathieu E, MD (Suresnes), Maugard T, MD (Cherbourg Octeville), Mauger C, MD (Gaillon-sur-Montcient), Mazet B, MD (Angers), Megarni S, MD (La Roche-sur-Yon), Mehrsa K, MD (Le Chesnay), Mehu G, MD (Quimper), Mekerri H, MD (Pithiviers), Menot E, MD (Laon), Mercier JC, MD (Paris), Meress N, MD (Clermont Ferrand), Merlaud C, MD (Royan), Merle F, MD (Cannes), Mescam M, MD (Douarnenez), Meyer F, MD (Lyon), Meyer G, MD (Senlis), Meyran S, MD (Lyon), Mezard P, MD (Aulnay-sous-Bois), Mier L, MD (Laval), Milleret MJ, MD (Sens), Mimouni M, MD (Auxerre), Mingasson P, MD (Manosque), Minguet JM, MD (Draguignan), Minodier P, MD (Marseille), Miramont JP, MD (Albi), Mitamona J, MD (Marmande), Mittler B, MD (St Louis), Mokdadi K, MD (Lyon), Monnet C, MD (Charigny), Monnet M, MD (Aix les Bains), Monroche G, MD (Angers), Montesinos C, MD (Bagneres de Bigorre), Montesquieu F, MD (La Bastide l’Eveque), Mora M, MD (Narbonne), Morel C, MD (Echirolles), Morignot D, MD (Grenoble), Mory O, MD (St Priest en Jarez), Mougel C, MD (St Die Des Vosges), Mougin K, MD (St Denis de la Réunion), Mouriesse D, MD (Bourg en Bresse), Mourou H, MD (Carcassonne), Mourtada MV, MD (Avranches), Moussouni H, MD (Tourcoing), Mouthemy G, MD (Laon), Mselati JC, MD (Orsay), Muller D, MD (Mably), Muller S, MD (Rambouillet), Mzoughi M, MD (Niort), Nace L, MD (Nancy), Nahani A, MD (Gray), Nampont A, MD (Autoire), Nancel-Penard S, MD (Ambleville), Nasr F, MD (St Quentin), Navarro A, MD (Istres), Neuilly C, MD (Tremblay en France), Niederhoffer C, MD (Mulhouse), Nigoghossian P, MD (Arles), Niziolek C, MD (Briey), Obert L, MD (Besancon), Ohayon Y, MD (Barbey), Ollivier F, MD (Dinan), Ourvois P, MD (Calais), Pacchioni F, MD (Gap), Paget P, MD (Amberieu en Bugey), Pailler-Pradeau C, MD (Selestat), Pamart P, MD (Cambrai), Pantaleo V, MD (St Laurent du Var), Papaix-Puech M, MD (Kourou), Paquirimo¤dine R, MD (Thiais), Paradi T, MD (Auch), Pasgrimaud L, MD (La Trinite en Martinique), Patella F, MD (Baie Mahault), Patin MN, MD (St Cloud), Pellerin S, MD (Sens), Pereyre M, MD (Bayonne), Peribois G, MD (Thonon les Bains), Perreaux F, MD (Clamart), Persillon C, MD (Oloron Ste Marie), Peure C, MD (Montfermeil), Phlippoteau C, MD (Creteil), Picaud S, MD (Villeurbanne), Pignon P, MD (Lens), Pillet P, MD (Bordeaux), Pinel P, MD (Sete), Plaisance P, MD (Paris), Plas M, MD (La Teste de Buch), Pochet F, MD (Wattrelos), Pohlmann E, MD (Foix), Poirel C, MD (Le Chalard), Poirier P, MD (Chateau Gontier), Pons I, MD (Aubagne), Poquet G, MD (Favieres), Porche M, MD (Arpajon), Portecop P, MD (Grand Bourg), Potinet-Pagliaroli V, MD (Lyon), Poujol B, MD (Cholet), Pouyanne I, MD (Pau), Prigent G, MD (Voiron), Principe A, MD (Morlaix), Pugnière JP, MD (Ollioules), Quilliec C, MD (Antony), Rajaonarivony JP, MD (Chauny), Rakaa A, MD (Venissieux), Rama S, MD (Campome), Rambaud O, MD (Challans), Ranai R, MD (La Rochelle), Raphael M, MD (Le Kremlin Bicetre), Ray P, MD (Paris), Razafindranazy L, MD (Soissons), Renard A, MD (Marseille), Renaud G, MD (Lons le Saunier), Renize J, MD (Brive la Gaillarde), Revue E, MD (Barjouville), Ricarhibon A, MD (Beaumont-sur-Oise), Richard P, MD (Nimes), Rigo C, MD (Montpellier), Rimet Y, MD (Aix en Provence), Riollot JC, MD (Caen), Riou B, MD (Paris), Risler JP, MD (Aisey-sur-Seine), Riviere C, MD (Ares), Roche JM, MD (Reims), Roland-Billecart D, MD (La Chapelle Montligeon), Romeo B, MD (Amiens), Rosa D, MD (Luneville), Roseau P, MD (Ambert), Rothe MR, MD (St Brieuc), Rouby D, MD (Ussel), Rougetet C, MD (Annemasse), Roupie E, MD (Caen), Sadat K, MD (Nanterre), Saf M, MD (Arpajon), Sanza E, MD (St Georges de Didonne), Sarda H, MD (Ennery), Sattonnet P, MD (Thionville), Sava E, MD (Clermont Ferrand), Savary D, MD (Pringy), Sawalha S, MD (Thann), Schinkel D, MD (Metz), Schlegel J, MD (Haguenau), Schneider JM, MD (Thionville), Schneider M, MD (Sarrebourg), Schol C, MD (Seclin), Schuster M, MD (Guebwiller), Schweig T, MD (Chinon), Scouarnec C, MD (Pessac), Seaume H, MD (Longjumeau), Sebton D, MD (Beauvais), Seguin P, MD (Rennes), Semhoun M, MD (Aunay-sur-Odon), Senee D, MD (Bloye), Sentias C, MD (Coutances), Siagni S, MD (Anglade), Sidhoum A, MD (Strasbourg), Sidialy S, MD (Grande Synthe), Simon N, MD (Poissy), Simon-Libchaber E, MD (Corbeil Essonnes), Smaiti N, MD (Lille), Soliveau G, MD (Le Puy en Velay), Soulat L, MD (Chateauroux), Souquiere L, MD (Brest), Soussan V, MD (Boulogne Billancourt), Soussi M, MD (Cognet), Storme D, MD (Vichy), Strozyk L, MD (Bois Guillaume), Subtil F, MD (St Cyr-sur-Loire), Suffys I, MD (Romorantin Lanthenay), Tabyaoui S, MD (Montceau les Mines), Tahir A, MD (Limoges), Tailhan R, MD (Boujan-sur-Libron), Taki B, MD (Fecamp), Taleb Benbiab Djaouad M, MD (Les Aires), Tandonnet P, MD (Poitiers), Tap R, MD (Rochefort), Taquet N, MD (Aulnoy lez Valenciennes), Tatulli T, MD (Ales), Telitel N, MD (Strasbourg), Testaert E, MD (Le Havre), Texier S, MD (Lorient), Thiery P, MD (Fourmies), Thomas L, MD (Brest), Tilhet-Coartet S, MD (Lyon), Tillaux A, MD (Baromesnil), Tisseron B, MD (Orleans), Tisseron M, MD (Beru), Tixier L, MD (St Etienne), Torres A, MD (Carcassonne), Touil M, MD (La Fleche), Trarieux F, MD (Aubervilliers), Treguer J, MD (Landerneau), Troller S, MD (La Rochelle), Tschill C, MD (Chatellerault), Tuil E, MD (Paris), Ursulescu N, MD (Belfort), Vachon I, MD (Chambeon), Valdenaire G, MD (Bordeaux), Vallejo C, MD (Limoges), Vallet B, MD (Beaune), Vannson MO, MD (Remiremont), Vanrenterghem B, MD (Dunkerque), Vansteenkiste N, MD (St Denis), Varin A, MD (Cricqueboeuf), Vauguet E, MD (Caen), Verdeil J, MD (Nice), Verley L, MD (St Malo), Vervel C, MD (Compiegne), Viala T, MD (Aix en Provence), Viallon A, MD (St Priest en Jarez), Viant E, MD (St Mande), Vicente P, MD (Cahors), Vigneron P, MD (Lorient), Vinciguerra D, MD (Toulon), Violet S, MD (Castelnau Le lez), Voisin X, MD (Antibes), Voituret N, MD (Paray le Monial), Volait G, MD (Le Havre), Vrignaud B, MD (Nantes), Vuillermoz F, MD (Anglars Nozac), Wadih S, MD (Ambres), Wahiche M, MD (Privas), Wargon M, MD (Bry-sur-Marne), Wiener P, MD (Vitre), Wingert D, MD (Wissembourg), Wohler A, MD (Agen), Wongeczowski O, MD (Levallois Perret), Wuilmet L, MD (Chalons en Champagne), Ximenes A, MD (Aicirits Camou Suhast), Younsi S, MD (Vire), Yousfi R, MD (St Nazaire), Zamoum D, MD (Mont St Martin), Zamour C, MD (Valence), Zane D, MD (Augan), Zaoui A, MD (Issoudun), Zegar T, MD (Amiens), Zerga M, MD (Chevreville), Ziade E, MD (Le Creusot), Zimmermann S, MD (Assainvillers), Zix AM, MD (Saverne), Zunino FM, MD (Aix en Provence).
Contributors: DN and YY were involved in the study data analysis, interpretation of results and drafting the manuscript. CEK and GR were involved in the study data analysis and interpretation of results. AV and JS were involved in the study conception, data analysis and interpretation of results. All the authors critically revised the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data may be obtained from a third party and are not publicly available.
References
- 1. Devaux M. Income-Related inequalities and inequities in health care services utilisation in 18 selected OECD countries. Eur J Health Econ 2015;16:21–33. 10.1007/s10198-013-0546-4 [DOI] [PubMed] [Google Scholar]
- 2. McKee M, Suhrcke M, Nolte E, et al. . Health systems, health, and wealth: a European perspective. The Lancet 2009;373:349–51. 10.1016/S0140-6736(09)60098-2 [DOI] [PubMed] [Google Scholar]
- 3. Grumbach K, Keane D, Bindman A. Primary care and public emergency department overcrowding. Am J Public Health 1993;83:372–8. 10.2105/AJPH.83.3.372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rust G, Ye J, Baltrus P, et al. . Practical barriers to timely primary care access: impact on adult use of emergency department services. Arch Intern Med 2008;168:1705–10. 10.1001/archinte.168.15.1705 [DOI] [PubMed] [Google Scholar]
- 5. Afilalo J, Marinovich A, Afilalo M, et al. . Nonurgent emergency department patient characteristics and barriers to primary care. Acad Emerg Med 2004;11:1302–10. 10.1197/j.aem.2004.08.032 [DOI] [PubMed] [Google Scholar]
- 6. Grol R, Giesen P, van Uden C. After-Hours care in the United Kingdom, Denmark, and the Netherlands: new models. Health Aff 2006;25:1733–7. 10.1377/hlthaff.25.6.1733 [DOI] [PubMed] [Google Scholar]
- 7. Huibers L, Giesen P, Wensing M, et al. . Out-Of-Hours care in Western countries: assessment of different organizational models. BMC Health Serv Res 2009;9:105 10.1186/1472-6963-9-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baier N, Geissler A, Bech M, et al. . Emergency and urgent care systems in Australia, Denmark, England, France, Germany and the Netherlands - Analyzing organization, payment and reforms. Health Policy 2019;123:1–10. 10.1016/j.healthpol.2018.11.001 [DOI] [PubMed] [Google Scholar]
- 9. Gouyon M. Les recours aux Médecins urgentistes de ville 2006.
- 10. Uscher-Pines L, Pines J, Kellermann A, et al. . Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 11. Carret MLV, Fassa ACG, Domingues MR. Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cad. Saúde Pública 2009;25:7–28. 10.1590/S0102-311X2009000100002 [DOI] [PubMed] [Google Scholar]
- 12. McHale P, Wood S, Hughes K, et al. . Who uses emergency departments inappropriately and when - a national cross-sectional study using a monitoring data system. BMC Med 2013;11:258 10.1186/1741-7015-11-258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gill JM, Riley AW. Nonurgent use of hospital emergency departments: urgency from the patient’s perspective. J Fam Pract 1996;42:491–6. [PubMed] [Google Scholar]
- 14. Koziol-McLain J, Price DW, Weiss B, et al. . Seeking care for nonurgent medical conditions in the emergency department: through the eyes of the patient. Journal of Emergency Nursing 2000;26:554–63. 10.1067/men.2000.110904 [DOI] [PubMed] [Google Scholar]
- 15. Agarwal S, Banerjee J, Baker R, et al. . Potentially avoidable emergency department attendance: interview study of patients' reasons for attendance. Emerg Med J 2012;29:e3 10.1136/emermed-2011-200585 [DOI] [PubMed] [Google Scholar]
- 16. Togher FJ, O'Cathain A, Phung V-H, et al. . Reassurance as a key outcome valued by emergency ambulance service users: a qualitative interview study. Health Expect 2015;18:2951–61. 10.1111/hex.12279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Martin A, Martin C, Martin PB, et al. . 'Inappropriate' attendance at an accident and emergency department by adults registered in local general practices: how is it related to their use of primary care? J Health Serv Res Policy 2002;7:160–5. 10.1258/135581902760082463 [DOI] [PubMed] [Google Scholar]
- 18. Barbadoro P, Di Tondo E, Menditto VG, et al. . Emergency department non-urgent visits and hospital readmissions are associated with different socio-economic variables in Italy. PLoS One 2015;10:e0127823 10.1371/journal.pone.0127823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Carret MLV, Fassa AG, Kawachi I. Demand for emergency health service: factors associated with inappropriate use. BMC Health Serv Res 2007;7:131 10.1186/1472-6963-7-131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bianco A, Pileggi C, Angelillo IF. Non-Urgent visits to a hospital emergency department in Italy. Public Health 2003;117:250–5. 10.1016/S0033-3506(03)00069-6 [DOI] [PubMed] [Google Scholar]
- 21. Mistry RD, Brousseau DC, Alessandrini EA. Urgency classification methods for emergency department visits: do they measure up? Pediatr Emerg Care 2008;24:870–4. 10.1097/PEC.0b013e31818fa79d [DOI] [PubMed] [Google Scholar]
- 22. Site internet du Ministère de la Santé donnant accès aux données collectées dans le cadre de la Statistique annuelle des établissements de santé [Internet]. [cited 2018 Jul 3]. Available from. Available: https://www.sae-diffusion.sante.gouv.fr/sae-diffusion/accueil.htm
- 23. Bellou A, de Korwin J-D, Bouget J, et al. . Implication of emergency departments in the regulation of public hospitalizations]. Rev Médecine Interne Fondée Par Société Natl Francaise Médecine Interne 2003;24:602–12. [DOI] [PubMed] [Google Scholar]
- 24. Lin MP, Baker O, Richardson LD, et al. . Trends in emergency department visits and admission rates among US acute care hospitals. JAMA Intern Med 2018;178:1708–10. 10.1001/jamainternmed.2018.4725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Howard MS, Davis BA, Anderson C, et al. . Patients' perspective on choosing the emergency department for nonurgent medical care: a qualitative study exploring one reason for overcrowding. J Emerg Nurs 2005;31:429–35. 10.1016/j.jen.2005.06.023 [DOI] [PubMed] [Google Scholar]
- 26. Schull MJ, Kiss A, Szalai J-P. The effect of low-complexity patients on emergency department waiting times. Ann Emerg Med 2007;49:257–64. 10.1016/j.annemergmed.2006.06.027 [DOI] [PubMed] [Google Scholar]
- 27. Sanders J. A review of health professional attitudes and patient perceptions on 'inappropriate' accident and emergency attendances. The implications for current minor injury service provision in England and Wales. J Adv Nurs 2000;31:1097–105. 10.1046/j.1365-2648.2000.01379.x [DOI] [PubMed] [Google Scholar]
- 28. Cour des comptes Les urgences hospitalières : une fréquentation croissante, une articulation avec la médecine de ville repenser [Internet]. Rapport sur l’application des lois de financement de la sécurité sociale pour 2014, 2014. Available: https://www.ccomptes.fr/sites/default/files/EzPublish/rapport_securite_sociale_2014_urgences_hospitalieres.pdf [Accessed 19 Jun 2019].
- 29. Mackenbach JP, Stirbu I, Roskam A-JR, et al. . Socioeconomic inequalities in health in 22 European countries. N Engl J Med 2008;358:2468–81. 10.1056/NEJMsa0707519 [DOI] [PubMed] [Google Scholar]
- 30. Trannoy A, Tubeuf S, Jusot F, et al. . Inequality of opportunities in health in France: a first pass. Health Econ 2010;19:921–38. 10.1002/hec.1528 [DOI] [PubMed] [Google Scholar]
- 31. Tubeuf S, Jusot F. Social health inequalities among older Europeans: the contribution of social and family background. Eur J Health Econ 2011;12:61–77. 10.1007/s10198-010-0229-3 [DOI] [PubMed] [Google Scholar]
- 32. Jusot F. [Inequalities in access to care and their evolution: A review.]. Rev Dépidémiologie Santé Publique 2013;61:S163–9. [DOI] [PubMed] [Google Scholar]
- 33. Brousseau DC, Hoffmann RG, Nattinger AB, et al. . Quality of primary care and subsequent pediatric emergency department utilization. Pediatrics 2007;119:1131–8. 10.1542/peds.2006-3518 [DOI] [PubMed] [Google Scholar]
- 34. Christakis DA, Wright JA, Koepsell TD, et al. . Is greater continuity of care associated with less emergency department utilization? Pediatrics 1999;103:738–42. 10.1542/peds.103.4.738 [DOI] [PubMed] [Google Scholar]
- 35. Gill JM, Mainous AG, Nsereko M. The effect of continuity of care on emergency department use. Arch Fam Med 2000;9:333–8. 10.1001/archfami.9.4.333 [DOI] [PubMed] [Google Scholar]
- 36. Ionescu-Ittu R, McCusker J, Ciampi A, et al. . Continuity of primary care and emergency department utilization among elderly people. Can Med Assoc J 2007;177:1362–8. 10.1503/cmaj.061615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Définition - Medical density | Insee. Available: https://www.insee.fr/en/metadonnees/definition/c1615 [Accessed 21 Aug 2019].
- 38. Capp R, Rooks SP, Wiler JL, et al. . National study of health insurance type and reasons for emergency department use. J Gen Intern Med 2014;29:621–7. 10.1007/s11606-013-2734-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Khan Y, Glazier RH, Moineddin R, et al. . A population-based study of the association between socioeconomic status and emergency department utilization in Ontario, Canada. Acad Emerg Med 2011;18:836–43. 10.1111/j.1553-2712.2011.01127.x [DOI] [PubMed] [Google Scholar]
- 40. Phelps K, Taylor C, Kimmel S, et al. . Factors associated with emergency department utilization for nonurgent pediatric problems. Arch Fam Med 2000;9:1086–92. 10.1001/archfami.9.10.1086 [DOI] [PubMed] [Google Scholar]
- 41. Naouri D, El Khoury C, Vincent-Cassy C, et al. . The French emergency national survey: a description of emergency departments and patients in France. PLoS One 2018;13:e0198474 10.1371/journal.pone.0198474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Béland F, Lemay A, Boucher M. Patterns of visits to hospital-based emergency rooms. Soc Sci Med 1998;47:165–79. 10.1016/S0277-9536(98)00029-X [DOI] [PubMed] [Google Scholar]
- 43. Billings J, Parikh N, Mijanovich T. Emergency department use in New York City: a substitute for primary care? Issue Brief Commonw Fund 2000;433:1–5. [PubMed] [Google Scholar]
- 44. Dale J, Green J, Reid F, et al. . Primary care in the accident and emergency department: I. prospective identification of patients. BMJ 1995;311:423–6. 10.1136/bmj.311.7002.423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Finn JC, Flicker L, Mackenzie E, et al. . Interface between residential aged care facilities and a teaching hospital emergency department in Western Australia. Med J Aust 2006;184:432–5. 10.5694/j.1326-5377.2006.tb00313.x [DOI] [PubMed] [Google Scholar]
- 46. Gill JM, Reese CL, Diamond JJ. Disagreement among health care professionals about the urgent care needs of emergency department patients. Ann Emerg Med 1996;28:474–9. 10.1016/S0196-0644(96)70108-7 [DOI] [PubMed] [Google Scholar]
- 47. Lee A, Lau FL, Hazlett CB, et al. . Factors associated with non-urgent utilization of accident and emergency services: a case-control study in Hong Kong. Soc Sci Med 2000;51:1075–85. 10.1016/S0277-9536(00)00039-3 [DOI] [PubMed] [Google Scholar]
- 48. Michelen W, Martinez J, Lee A, et al. . Reducing frequent flyer emergency department visits. J Health Care Poor Underserved 2006;17:59–69. 10.1353/hpu.2006.0010 [DOI] [PubMed] [Google Scholar]
- 49. Shah NM, Shah MA, Behbehani J. Predictors of non-urgent utilization of hospital emergency services in Kuwait. Soc Sci Med 1996;42:1313–23. 10.1016/0277-9536(95)00233-2 [DOI] [PubMed] [Google Scholar]
- 50. Stein AT, Harzheim E, Costa M, et al. . The relevance of continuity of care: a solution for the chaos in the emergency services. Fam Pract 2002;19:207–10. 10.1093/fampra/19.2.207 [DOI] [PubMed] [Google Scholar]
- 51. Young GP, Wagner MB, Kellermann AL, et al. . Ambulatory visits to hospital emergency departments. patterns and reasons for use. 24 hours in the ED Study Group. JAMA 1996;276:460–5. 10.1001/jama.276.6.460 [DOI] [PubMed] [Google Scholar]
- 52. Pereira S, Oliveira e Silva A, Quintas M, et al. . Appropriateness of emergency department visits in a Portuguese university hospital. Ann Emerg Med 2001;37:580–6. 10.1067/mem.2001.114306 [DOI] [PubMed] [Google Scholar]
- 53. Sarver JH, Cydulka RK, Baker DW. Usual source of care and nonurgent emergency department use. Acad Emerg Med 2002;9:916–23. 10.1197/aemj.9.9.916 [DOI] [PubMed] [Google Scholar]
- 54. Cunningham PJ, Clancy CM, Cohen JW, et al. . The use of hospital emergency departments for nonurgent health problems: a national perspective. Med Care Res Rev 1995;52:453–74. 10.1177/107755879505200402 [DOI] [PubMed] [Google Scholar]
- 55. Cartographie interactive de la Démographie Médicale. Available: https://demographie.medecin.fr/#s=2016;v=map2;i=demo_med.dens_tte_act;l=fr [Accessed 16 Dec 2018].
- 56. Merlo J, Chaix B, Yang M, et al. . A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health 2005;59:443–9. 10.1136/jech.2004.023473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Weinmayr G, Dreyhaupt J, Jaensch A, et al. . Multilevel regression modelling to investigate variation in disease prevalence across locations. Int J Epidemiol 2017;46:336–47. 10.1093/ije/dyw274 [DOI] [PubMed] [Google Scholar]
- 58. Petersen LA, Burstin HR, O’Neil AC, et al. . Nonurgent emergency department visits: the effect of having a regular doctor. Med Care 1998;36:1249–55. [DOI] [PubMed] [Google Scholar]
- 59. Lang T, Davido A, Diakité B, et al. . Using the hospital emergency department as a regular source of care. Eur J Epidemiol 1997;13:223–8. 10.1023/A:1007372800998 [DOI] [PubMed] [Google Scholar]
- 60. Bilan démographique Insee Première - 1482, 2013. Available: https://www.insee.fr/fr/statistiques/1280956 [Accessed 19 Jun 2019].
- 61. Despres DC. Le renoncement aux soins: des parcours de soins sous contraintes ou une forme d’émancipation? Renoncement Aux Soins, 2011. Available: http://coderpa77.fr/wp-content/uploads/2015/03/DRES_actes_renoncement_soins_2012.pdf#page=69 [Accessed 7 Apr 2016].
- 62. Batto V, Leduc A, Legal R, et al. . La complémentaire santé. Acteurs, bénéficiaires, garanties: édition 2016 2016.
- 63. Inspection Générale des Affaires Sociales Rapport SUR Le tiers payant pour les consultations de médecine de ville, 2013. Available: https://www.argusdelassurance.com/mediatheque/4/4/2/000025244.pdf [Accessed 19 Jun 2019].
- 64. Raginel T, Ruelle Y, Saint-Lary O, et al. . Perspectives SUR Le tiers payant en médecine générale. Exercer 2015;120:166–75. [Google Scholar]
- 65. Baker DW, Stevens CD, Brook RH. Determinants of emergency department use: are race and ethnicity important? Ann Emerg Med 1996;28:677–82. 10.1016/S0196-0644(96)70093-8 [DOI] [PubMed] [Google Scholar]
- 66. Ginde AA, Lowe RA, Wiler JL. Health insurance status change and emergency department use among US adults. Arch Intern Med 2012;172:642–7. 10.1001/archinternmed.2012.34 [DOI] [PubMed] [Google Scholar]
- 67. Pukurdpol P, Wiler JL, Hsia RY, et al. . Association of Medicare and Medicaid insurance with increasing primary care-treatable emergency department visits in the United States. Acad Emerg Med 2014;21:1135–42. 10.1111/acem.12490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Rust G, Baltrus P, Ye J, et al. . Presence of a community health center and uninsured emergency department visit rates in rural counties. J Rural Health 2009;25:8–16. 10.1111/j.1748-0361.2009.00193.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sun BC, Burstin HR, Brennan TA. Predictors and outcomes of frequent emergency department users. Acad Emerg Med 2003;10:320–8. 10.1197/aemj.10.4.320 [DOI] [PubMed] [Google Scholar]
- 70. Radke J, Mu L, Decompositions S. Modeling and mapping service regions to predict access to social programs. Geogr Inf Sci 2000;6:105–12. [Google Scholar]
- 71. Wang F, Luo W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place 2005;11:131–46. 10.1016/j.healthplace.2004.02.003 [DOI] [PubMed] [Google Scholar]
- 72. Vergier N, Chaput H, Lefebvre-Hoang I. Déserts médicaux : comment les définir ? Comment les mesurer ? [Internet]. Les Dossiers de la Drees;, 2017. Available: http://drees.solidarites-sante.gouv.fr/IMG/pdf/dd17.pdf [Accessed 1 Feb 2018].
- 73. Whittaker W, Anselmi L, Kristensen SR, et al. . Associations between extending access to primary care and emergency department visits: a Difference-In-Differences analysis. PLoS Med 2016;13:e1002113 10.1371/journal.pmed.1002113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Cowling TE, Majeed A, Harris MJ. Importance of accessibility and opening hours to overall patient experience of general practice: analysis of repeated cross-sectional data from a national patient survey. Br J Gen Pract 2018;68:e469–77. 10.3399/bjgp18X697673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Cowling TE, Majeed A, Harris MJ. Patient experience of general practice and use of emergency hospital services in England: regression analysis of national cross-sectional time series data. BMJ Qual Saf 2018;27:643–54. 10.1136/bmjqs-2017-007174 [DOI] [PubMed] [Google Scholar]
- 76. Cowling TE, Ramzan F, Ladbrooke T, et al. . Referral outcomes of attendances at general practitioner led urgent care centres in London, England: retrospective analysis of hospital administrative data. Emerg Med J 2016;33:200–7. 10.1136/emermed-2014-204603 [DOI] [PubMed] [Google Scholar]
- 77. Jaffe TA, Kocher KE, Ghaferi AA. Potentially avoidable emergency department use: when policy expects patients to be physicians. Ann Emerg Med 2018;72:256–8. 10.1016/j.annemergmed.2018.05.019 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjqs-2019-009396supp001.pdf (90.5KB, pdf)