Abstract
Background:
Medical Assistance in Dying, also known as euthanasia or assisted suicide, is expanding internationally. Canada is the first country to permit Nurse Practitioners to provide euthanasia. These developments highlight the need for nurses to reflect upon the moral and ethical issues that euthanasia presents for nursing practice.
Purpose:
The purpose of this article is to provide a narrative review of the ethical arguments surrounding euthanasia in relationship to nursing practice.
Methods:
Systematic search and narrative review. Nine electronic databases were searched using vocabulary developed from a stage 1 search of Medline and CINAHL. Articles that analysed a focused ethical question related to euthanasia in the context of nursing practice were included. Articles were synthesized to provide an overview of the literature of nursing ethics and euthanasia.
Ethical Considerations:
This review was conducted as per established scientific guidelines. We have tried to be fair and respectful to the authors discussed.
Findings:
Forty-three articles were identified and arranged inductively into four themes: arguments from the nature of nursing; arguments from ethical principles, concepts and theories; arguments for moral consistency; and arguments from the nature of the social good. Key considerations included nursing’s moral ontology, the nurse–patient relationship, potential impact on the profession, ethical principles and theories, moral culpability for acts versus omissions, the role of intention and the nature of the society in which euthanasia would be enacted. In many cases, the same assumptions, values, principles and theories were used to argue both for and against euthanasia.
Discussion:
The review identified a relative paucity of literature in light of the expansion of euthanasia internationally. However, the literature provided a fulsome range of positions for nurses to consider as they reflect on their own participation in euthanasia. Many of the arguments reviewed were not nursing-specific, but rather are relevant across healthcare disciplines. Arguments explicitly grounded within the nature of nursing and nurse–patient relationships warrant further exploration.
Keywords: Euthanasia, ethics, euthanasia, literature review, medical assistance in dying, nursing
Background
Medical assistance in dying
Medical Assistance in Dying was legalized in Canada in 2016 by an amendment to the Criminal Code that removed its prohibition. This legalization, which allows Nurse Practitioners to be both assessors and providers of Medical Assistance in Dying, was the catalyst for the current review. Under the Canadian legislation, two actions to medically aide the dying are permissible: (1) administering a substance to a person at their request that causes their death (commonly referred to as euthanasia) or (2) prescribing or providing a substance to a person at their request so that they may self-administer the substance and in so doing cause their own death (commonly referred to as assisted suicide).1 To date, seven countries around the world offer a type of euthanasia.2 As in Canada, the Netherlands, Belgium, Columbia and some US states have adopted assistance in dying into law. In others (i.e. Switzerland, Luxembourg), medical procedures that aid-in-dying have been decriminalized or are allowable under certain, predetermined circumstances.2
In Canada, the term Medical Assistance in Dying was chosen carefully to reflect Canadian context and values. However, terminology around the world varies to reflect the specific practices in that country. For example, physician-euthanasia is the terminology used in the United States, a term which reflects the limits of a client-administered death. Euthanasia is the term used most commonly in the international context. Specifically, euthanasia is defined as an ‘active and intentional act of putting to death, in a relatively painless way, of persons suffering severely from medical conditions that are incurable, untreatable, or irreversible…at that person’s explicit request’ (para. 1).3 In this article, the term euthanasia will be used to represent euthanasia, medical assistance in dying and assisted suicide or physician-euthanasia.
Euthanasia in relationship to nursing practice
The legalization of euthanasia has presented regulated nurses with a complex array of ethical and moral decisions as they relate to determining one’s level of involvement in this new care option. At one end of the spectrum is full conscientious objection, whereby nurses choose to be relieved of all care for reasons related to preserving moral integrity. At the other end of the spectrum is full involvement in the euthanasia process. In between are levels of involvement in care which may, or may not, be directly related to the actual provision of euthanasia (e.g. ongoing care for persons receiving euthanasia and bereavement support for family).4 Although the right for nurses to conscientiously object is enshrined in Canadian law,1 regulatory policies specify that this act cannot be taken lightly. For example, the regulatory document for nurses in Manitoba suggests that a position of conscientious objection should only be taken based upon long and deeply held values and beliefs.5 Furthermore, nurses have a commitment to proactively inform employers of their conscientious objection, preferably prior to the start of a new employment contract.4 In Canada, health region policies may require nurses to remain involved in euthanasia in non-related care even if they do conscientiously object to euthanasia. This requires nurses to engage in thoughtful and dedicated periods of reflection about their ability to participate, or not, in euthanasia.
Evidence from nurses’ experiences with euthanasia in countries outside of Canada suggests that this can be a rewarding, albeit morally complex, ambiguous and emotionally laden experience.6 A recent publication detailing nurses’ involvement with euthanasia in the first 6 months of its implementation in the Canadian context offered similar findings.7 In light of the moral and ethical complexity of this act, a number of authors have encouraged nurses to engage in discussions around euthanasia.8,9 To do so, nurses require knowledge of the issues they should be considering, time to reflect on the breadth of the issues at hand and a substantive body of literature to draw upon to stimulate reflection. The most recent review of the ethical literature we could locate was published in 2009. This was an arguments-based review of the ethical literature and nurses’ involvement in euthanasia (1987–2007).10 Our article provides a narrative review of the ethical arguments surrounding euthanasia in relationship to nursing practice which includes papers published up to 2018.
Methods
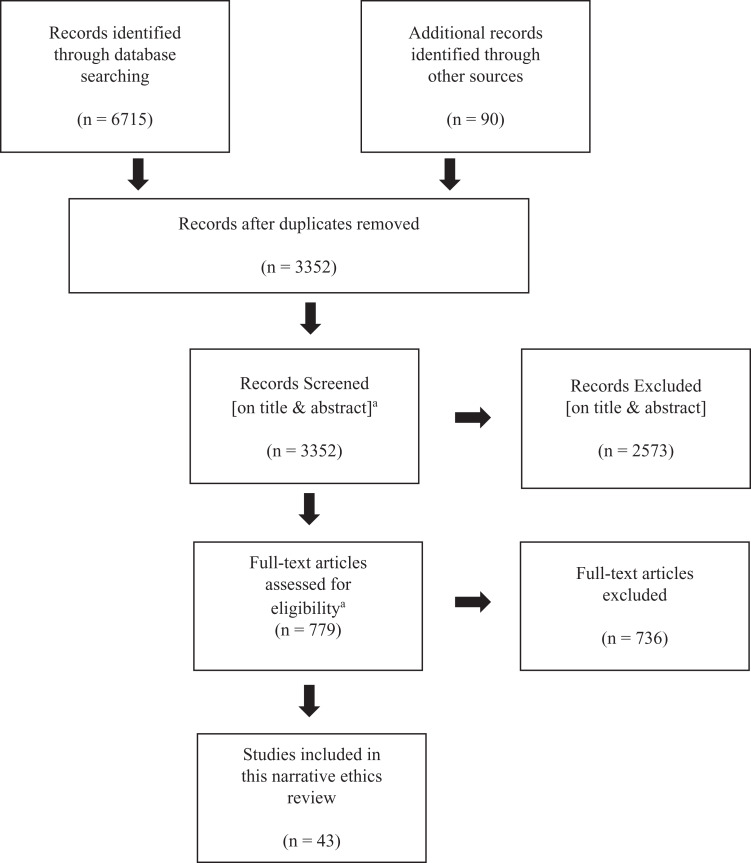
The sources we have drawn on for this article are part of a broader systematic search of the literature focused on the policy, practice and ethical implications of euthanasia for nursing. This broader search was conducted following the principles for systematic reviews developed by the Joanna Briggs Institute.11 Nine electronic databases (Table 1) were searched by an information scientist (R.J.) using strategies developed through consulting team members and previously published reviews on this subject.12,13 Before being finalized, the strategies were refined through a stage 1 search of Medline and CINAHL and peer reviewed using the PRESS Checklist.14 A copy of the final strategy used in Medline is available in the supplementary material. A total of 6715 articles were retrieved and loaded into EPPI-Reviewer where duplicates were identified and removed leaving 3352 unique articles for review. To be included in the broader review, articles had to address policy, practice or ethical implication of euthanasia for nursing. No date restrictions were set. Non-English language articles were excluded, although a count of the non-English language articles was kept to evaluate the degree of bias inherent in the review (see Figure 1 for a PRISMA flow diagram).
Table 1.
List of electronic databases searched (31 August 2017).
| Database | Results |
|---|---|
| Medline | 1987 |
| Embase | 2352 |
| Database of Abstracts of Review and Effects (DARE) | 1 |
| Ageline | 138 |
| PsychINFO | 438 |
| CINAHL | 1555 |
| Social Services Abstracts | 47 |
| Sociological Abstracts | 77 |
| ProQuest Dissertations and Theses Global (Search conducted 5 September 2017) | 120 |
| Total | 6715 |
Figure 1.
PRISMA flow diagram for broader systematic search of the literature.
aScreening of the ethics literature was conducted at the same time as the broader review (which included a focus on the policy, practice and ethical implications of euthanasia for nursing).
This article focuses on the sub-set of literature that discussed the ethical implications of euthanasia for nursing. To be eligible for this review of the ethical literature, the article had to (1) answer a focused ethical inquiry in relation to euthanasia and (2) make explicit application to nursing practice. For example, if an author simply provided an overview of some of the ethical issues related to euthanasia, it was excluded. On the contrary, if an author provided a robust analysis of the ethical implications of euthanasia in relation to nursing, even if the author did not argue to a particular conclusion, it was included. To ensure the reliability of the screening in accordance with these criteria, articles were screened by two investigators after establishing an inter-rater reliability rating of 90%.
Articles were then analysed using the process of narrative review. Narrative reviews seek to map complex bodies of literature for the purposes of conveying not only the depth and breadth of a field of study, but also the ‘reasons why it has been studied in a particular way, the interpretations that have been made with respect to what we know about it, and the nature of the knowledge base that informs or might inform clinical practice’ (p. 3).15 Unlike argument-based reviews designed to ask and answer focussed ethical questions based upon the quality of the arguments,16 the goal of a narrative review is to provide a map of the scholarly work, alongside interpretation and critique.15 As such, our focus in this review was on better understanding how nursing ethical discourse has chosen to approach the subject of euthanasia by surveying the arguments put forward rather than by directly answering the question of whether euthanasia is an ethical good in the context of nursing practice.
Forty articles focusing on ethical issues related to euthanasia in the context of nursing practice were identified and formed the basis of this narrative review. An additional three articles were identified through backward and forward searching and through the process of hand searching tables of contents of relevant journals (e.g. Nursing Ethics). A data extraction table (see supplementary material) was created that included authors, date, country, definition of euthanasia used and the focused ethical question addressed. The next step of this narrative review was to do a critical analysis of these articles to determine the current knowledge around nursing ethics and euthanasia. These articles were thematically categorized based upon the nature of the questions and the arguments used to address those questions. This process took the form of a qualitative inductive analysis. To begin, questions and arguments contained within the included articles were extracted by two investigators (M.G. and B.P.). Extracted data were then placed on an analysis map to look for commonalities within and between the ethical questions and arguments. Once the data were grouped within categories that shared common features, descriptors were assigned to the groupings to construct the thematic categories. Articles that contained ethical questions and arguments that overlapped categories were assigned to multiple themes.
Findings
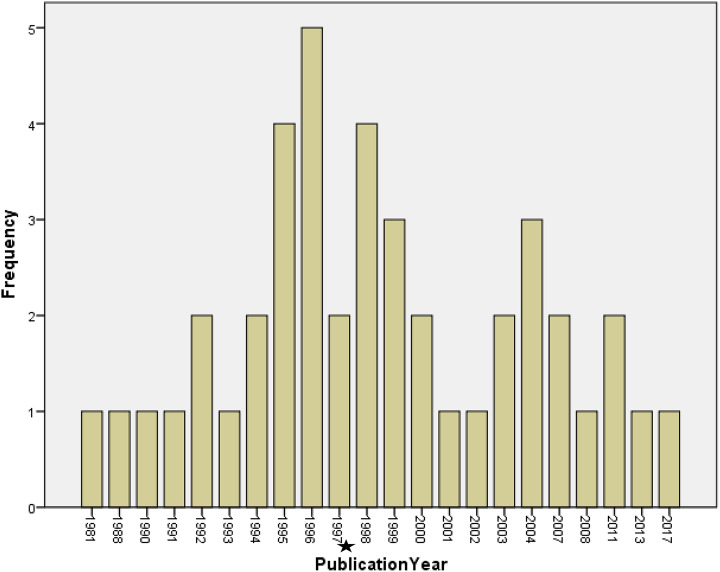
Of the 43 articles identified, the majority originated from the United States (see Table 2) and were published between 1995 and 1998 (see Figure 2). Relatively few articles were published within the last decade. The findings will be presented using the four thematic categories developed as a result of the analysis: the nature of nursing; ethical principles, concepts and theories; moral consistency; and the nature of the social good. Here, in keeping with the intent of narrative review methodology, we provide an overview of the kinds of arguments that were raised within the body of literature in relation to each thematic category.15
Table 2.
Countries of studies’ origins (N = 43).
| Country | Number of studies, n (%) |
|---|---|
| United States | 24 (56%) |
| United Kingdom | 12 (28%) |
| Australia | 3 (7%) |
| Canada | 3 (7%) |
| New Zealand | 1 (2%) |
Figure 2.
Frequency of publications (by year).
aIncrease in publications between the years of 1995 and 1999 may be attributed, in part, to the legalization of assisted suicide in Oregon, USA (Death with Dignity Act, 1997).
Nature of nursing
Twenty-three articles provided ethical arguments for and against euthanasia based upon the nature of nursing. Of these 23 articles, 14 focused exclusively on a nursing standpoint and nine discussed the nursing standpoint alongside other arguments (e.g. principle-based, societal consequences). Eleven articles did not take a position in relation to euthanasia, nine argued against and three argued for. Three assumptions about the nature of nursing were used to position arguments related to euthanasia: the nature of nursing’s moral ontology; nurses’ unique relational space with patients; and the consequence of euthanasia on nurses’ personhood and nursing as a profession.
The first set of assumptions concerned the nature of nursing’s moral ontology. As Mathes17 asked, ‘is there something intrinsic to the nursing role that makes it ethically impermissible for a nurse to aid a patient in committing suicide even if the suicide itself were ethically acceptable?’ (p. 262). For example, in arguing against euthanasia, Ferrell and Rivera (citing Coyle)18 appealed to nursing’s tacit values of alleviating suffering, preserving dignity, addressing meaningfulness, guarding sanctity of life and acting with compassion.19 Compassion was commonly cited as a foundational and enduring nursing value that could be used to argue both for and against euthanasia.20–22 This ontological morality of nursing was further described as altruistic beneficence in which the nurse’s goal is to work on behalf of the good of their patients and to avoid doing harm; again an argument that could be used to support positions both for and against euthanasia.20,23 These values were accompanied by moral goals of practice that included improving patient quality of life;19,22 healing;17,22,24–26 and preserving, protecting and respecting life.24,27,28 Those against euthanasia argued that euthanasia, as the act of killing, is a violation of this ontological morality and so nurses should not take part. In taking part, nursing as a discipline would be perceived as killers rather than healers resulting in the erosion of public trust.20,27,29,30
However, in defence of euthanasia, White31 argued that this ontological morality is subject to interpretation. She stated that there is justified harm in the context of nursing practice, that nursing’s social trust might include euthanasia if the public sees it to be in its best interest and that euthanasia could be viewed as relieving pain and suffering. As such, White argued that, although there may be an ontological morality, how that morality works itself out in practice is subject to interpretation. This argument was revealed in the way that authors used common concepts, such as compassion, to argue for different end points.
Likewise, Newham32 argued against an ‘internal morality’ (p. 109) of nursing on the basis that there is no agreed upon outcome or ‘end of nursing’ (p. 115). Without a definitive end of nursing, it is impossible to have an internal morality robust enough to address challenging ethical problems. Rather, he suggested that any claim to an internal morality is most useful as a ‘heuristic for people entering the profession of nursing’ (p. 115). Ultimately, he argued that the ‘moral agent is and must be one person’ (p. 115).
Others questioned whether the moral ontology of nursing remains stable or should respond to social change. For example, in arguing against euthanasia, McCabe25 suggested that nurses must resist a social contract in which nursing becomes nothing more than a profession which adheres to patient wishes in the guise of autonomy. Without explicitly arguing a position in regard to euthanasia, Thiele and Dunsford26 argued that nursing’s ontology needs to be fluid in response to a changing world.
A second set of assumptions that had implications for nurses’ ethical relationship to euthanasia was the nature of the nurse–patient relationship. Several authors opposing euthanasia argued that nurses have a unique relationship with patients because of the intense and continuing nature of their interaction. This relationship was characterized as genuine, caring, founded on mutual respect and inclusive of family as the unit of care.19 Exemplary relationships are characterized by nurses’ abilities to see patients as persons, by the ability to generate meaning for both patients and nurses,33 and by a duty of promise-keeping or faithfulness.34 Without coming to a position, Wurzbach discussed the implications of nurses being the ones who ‘stay with patients’35 during the dying process. Furthermore, nurses are viewed as ‘chief witnesses’19 in that they can understand the context within which patients make medical decisions19,36 and so can advocate on behalf of their patients to the larger team.19,36 However, this unique relationship was seen to have unique challenges in the context of euthanasia. Young,37 citing Jameton,38 described this as the ‘nurse in the middle’ (p. 12) phenomenon whereby nurses have a responsibility for care that does not match their power to influence decisions about care. In the context of euthanasia, she acknowledged the paradox that although nurses do not order medication for symptom management, they are in the position of delivering and titrating that medication to alleviate suffering. A nurse in the middle may be the ‘chief witness’19 to suffering without the means to relieve that suffering. As such, euthanasia may have unique moral implications for nurses. The acknowledgement of this special relationship between nurses and patients was used to argue both for30,36 and against19,33 euthanasia.
The third assumption in this body of literature was the potential impact that engaging in euthanasia could have on the nursing profession and on nurses’ personhood. In her argument for euthanasia, Young37 suggested that a nurse’s integrity is an essential part of professional practice. As such, nurses must do the difficult work of examining ‘competing demands carefully and making decisions that are congruent with their personal beliefs and within professional guidelines’ (p. 12). Beyond that, she argued that professional integrity must support patient self-determination and hence, requests for euthanasia. In contrast, Zimbelman and McCabe39 argued that professionalism means much more than simply supporting autonomy through state-enacted legislation. Arguing against euthanasia, Zimbelman suggested that nursing is a social institution whose ‘power, status, [and] role’ (p. 164) in society must transcend both individual interests of its practitioners and private choices of patients.40 Without arguing a position in relation to euthanasia, other authors suggested that euthanasia may have consequences that could exacerbate the sense of failure and loss that nurses often feel after a patient death,41 or harm nurses if their values and beliefs are challenged or ignored,21 which in turn, can affect the nature of the nurse–patient relationship.
Ethical principles, concepts and theories
Eighteen articles drew upon ethical principles, concepts and theories to provide arguments for or against the ethical permissibility of euthanasia in the context of nursing practice. The majority of articles grounded ethical arguments and discussions in one or more of the four main tenets of biomedical ethics: autonomy, beneficence, nonmaleficence and justice.42 Four authors argued in support of euthanasia, six were in opposition and the remaining eight authors took no position. Articles that provided a descriptive overview will be addressed first, followed by articles that argued using principle-based ethics and finally, articles that drew upon ethical theories, such as consequentialism, virtue ethics, relational ethics and care ethics.
Four articles addressed focused ethical questions by providing a descriptive landscape of the ethical principles, concepts and theories that are being discussed in the existing literature on euthanasia in the context of nursing practice.43–46 Interestingly, the majority of arguments raised within this body of literature presented what Snelling47 would call ‘intuitive arguments’; opinions related to ‘feelings’, such as mercy, ‘understanding that sometimes death is preferable to life’ (p. 352), respecting autonomy, and, conversely, ‘the feeling that it is wrong to kill’ (p. 352). All four articles incorporated – to varying degrees – Beauchamp and Childress’42 principles for biomedical ethics into their respective discussions on euthanasia from a nursing perspective. In two of the four articles, the main tenets of biomedical ethics were presented in a way that elucidated the tension and malleability that exists within and between the principles.43,46 For instance, Benedict et al.43 highlighted the tension that exists between respecting an individual’s autonomous decision to request euthanasia and upholding one’s professional duty to prevent harm. Other ethical issues raised included arguments related to ethical concepts, such as the sanctity of life, quality of life, suffering, pain management and the ‘slippery slope’.i,44,45
Nine articles drew upon principles of biomedical ethics to construct arguments for and against the justification of euthanasia in the context of nursing practice. Most often, arguments in favour of euthanasia were grounded in rights-based language; for example, the ‘right to die’, the ‘right to self-determination’,48 or the ‘right to die with dignity’.49 A number of authors argued that upholding an individual’s right to die fosters human flourishing and in turn, facilitates a dignified and autonomous death.21,48,50,51 These arguments can be summarized by the perspective that respect for persons requires respect for individuals’ autonomous decision-making.21 Such arguments are predicated on the belief that individuals’ ‘own’ their death, just as they have ‘owned’ their life.21,50,51 For instance, Farsides51 argued that requests for euthanasia are not an indication of failure of healthcare professionals’ abilities to provide care, but rather an expression of autonomy or the right of an individual to make a ‘choice that they consider consistent with the person that they are and the life that they have led’ (p. 104). However, despite a firm commitment to upholding patient autonomy, a number of authors acknowledged and indeed emphasized, that the principle of autonomy ought not to be considered in isolation, such that it is seen without any limits.21,50 For example, Begley,50 as well as Kopala and Kennedy,21 emphasized that, in upholding a patient’s autonomous decision to participate in euthanasia, the autonomy of the healthcare provider who is involved in caring for that patient must also be respected. As Begley50 stated, ‘…consenting adults should not be prevented from availing themselves of beneficent voluntary active euthanasia if another consenting [emphasis added] adult (a medical doctor) is available and capable of carrying out their wishes’ (p. 224). This perspective takes into consideration that the involvement of at least one other person is required should an individual seek to end his or her life through euthanasia.52
Conversely, a number of authors provided arguments in opposition to euthanasia, using the principle of autonomy to highlight their view that other biomedical principles, such as nonmaleficence and beneficence,21,53,54 can outweigh an individual’s claim to self-determination. For instance, in an argument against the absolutism of autonomy, and in particular, against obligations to always fulfil autonomous requests, Friend53 argued,
[i]ndividual autonomy is not a supreme ethical doctrine and does not deserve to be weighted more heavily than the physician’s duty to ‘above all do no harm’. Although respect for patient self-determination is important, especially when deciding to withhold and withdraw life-sustaining treatments, it does not mandate a right that others help them end their lives. (p. 115)
As reflected in the passage above, arguments against the absolutism of autonomy were often grounded in the assumption that individuals exist, and indeed, thrive, within a constellation of relationships.21,53,55 Following this line of reasoning, an individual’s decision to pursue an euthanasia significantly affects those around them and, as such, ‘…cannot be a purely private decision’ (p. 23).21
Kopala and Kennedy,21 Kowalski,29 and King and Jordan-Welch54 put forth arguments which refuted the claim that requests for euthanasia are part of a truly autonomous and rational decision-making process. For example, instead of seeing requests for euthanasia as extensions of a patient’s right to self-determination, King and Jordan-Welch argued that an individual’s true autonomy is upheld when nurses help patients to find meaning in life even in times of suffering and when nurses explore questions such as ‘why is the patient asking for assistance in dying?’ (p. 52).54
Five articles drew upon ethical theories to discuss euthanasia in the context of nursing practice. Two authors raised consequentialist arguments.47,56 Snelling47 discussed the contradictory nature of absolute deontological positions (i.e. referring to the law in the United Kingdom), which claim that consideration of consequences cannot justify killing in the form of euthanasia because it is always morally wrong to kill an innocent life. In particular, he contended that the credibility of the prohibition against euthanasia depends on distinguishing it from other legally and morally sanctioned end-of-life care practices (i.e. omissions, refusal of extraordinary measures or letting die). These distinctions depend on consequentialist considerations so it is inconsistent to claim that the prohibition on euthanasia cannot consider consequences. Snelling47 argued that just as increased doses of opioids (at levels that are potentially life-shortening) can be morally and legally acceptable under certain conditions, so might be an injection of potassium chloride (i.e. a lethal injection). In each circumstance, the consequences have been weighed, a thoughtful decision to shorten the individual’s life has been reached, and in the end ‘the consequences are the same’ (p. 356).47 In contrast, Praskwiecz55 focused on the sub-category of assisted suicide, which she defines as requiring ‘both patient request and patient action’ (p. 37), to contrast to some forms of euthanasia. She55 contended that some moral justification for assisted suicide might be provided by act utilitarianism – a consequentialist theory whereby the consequences of an action are weighed in the context of a particular situation. Praskwiecz55 argued that, because the consequences of legalized assisted suicide are difficult to fully understand and predict, rule utilitarian analysis cannot determine whether legalization would lead to ‘maximum balance of good over evil’ (p. 38)54,55 and, thus is ethically unjustified from a rule utilitarian perspective. Praskwiecz55 further argued that assisted suicide could not be justified by Kantian or natural law theories, and concluded that nurses should focus on other approaches to improving end-of-life care.
From another ethical perspective, Begley57 suggested that, in comparison to a strictly principled approach to analysis, a virtue ethics approach to analysing euthanasia widens the field of moral appraisal. Indeed, she argued that in virtue terms, euthanasia facilitates ‘eudaimonia (living well, flourishing) because dying is a life event, and not dying well frustrates the goal of flourishing and well-being for both client and professional’ (p. 441).57 In a different, albeit not entirely unrelated argument, Rich and Butts58 suggested that coherence in ethical positions opposing and supporting euthanasia can be achieved through an ethic of care. In opposition to a more legalistic approach inherent in absolutist principles, an ethic of care invites nurses and other healthcare providers to consider ‘where boundaries lie in the imposition of one’s morality on others’ (p. 275)58 when we ‘care’ for another person. For instance, if the act of caring involves ‘feeling with’ the other (Noddings,59 as cited in Rich and Butts),58 euthanasia can be ethically justified if the actions of the individual requesting aid in dying are rational and do not infringe on the rights of others.58 Finally, in an application of the four core elements of relational ethics – mutual respect, engagement, environment and embodiment – Thiele and Dunsford26 argued not about the ethical or moral permissibility of euthanasia, but rather, how relational ethics can provide nurses and nurse leaders with a framework for thinking through the moral complexity that has accompanied the legalization of euthanasia in Canada.24
Moral consistency
Seven articles examined the ethical permissibility of euthanasia from the perspective of moral consistency across acts. Such arguments sought to elucidate the moral difference, if any, between one practice and another related practice. Five authors sought to clarify the moral distinction between a ‘passive’ and ‘active’ euthanasia through an examination of the role of causation, and more specifically, the philosophic differences between ‘killing’ and ‘letting die’,41,47 and in some cases, using the acts and omissions doctrine.47,52,60,61 In addition, a number of authors examined the role of intention – either in isolation or alongside other arguments.47,52,56,61 From the standpoint of consistency (i.e. if one type of euthanasia is ethically justified, then why isn’t the other), five of the seven authors argued in support of euthanasia, one author argued against and another author did not take a position on the topic.
Several articles sought to elucidate the moral difference between ‘killing’ versus ‘letting die’47,62,41 or, as Dines60 refers to it, ‘killing’ versus ‘going along with nature’. Such arguments often centred on the ambiguous nature of what ‘letting die’ or ‘going along with nature’ entailed, and in particular, how it is morally distinct from an act that also causes death, albeit in a more direct way. For instance, Dines60 argued that the moral distinction between causing death and ‘going along with nature’ is not a ‘water tight barometer of moral acceptability’ (p. 914), and that if it were, then many attempts to redress suffering (i.e. pain and symptom management) would be immoral as a result of their unnatural interference with the dying, or indeed living, process. Kuhse62 argued to a similar position; however, she arrived at more of a direct conclusion,
you may refuse treatment and then ‘nature’ will look after the rest – you will be dead in a few hours, a few days, or at the very latest in a few weeks, [this] is an approach unfit for a humane and rational society. It imposes on those patients a mode of dying that they find unacceptable, much unnecessary suffering, and all that for no good reason. (p. 12)
Several authors situated the ‘killing’ versus ‘letting die’ argument within the acts and omissions doctrine.63 Central to this doctrine is the belief that sometimes we are morally less responsible for our omissions – our failures to take action – than we are for our actions.64 Central to this debate is the question of if you consider an action and do not act, is that then an omission or an action? Four authors examined the validity of the ethical and moral arguments inherent in the acts and omissions doctrine.47,52,60,61 For instance, through the evaluation of three different approaches to one case-based scenario, Begley50 questioned whether there is a morally significant difference between an act and an omission. She argued, much to the same conclusion as Dines60 and Moody,61 that if the initial and end states of the patient are the same (i.e. they are dying (initial); they are dead (end)) and that the actions or inactions of the healthcare provider are what rendered the patient into that end state, then what is the morally significant difference between an act and an omission? The argument here is that because the beginning and end states are the same, and the healthcare provider is the agent involved in the intervening performance, then the healthcare provider is the ethically responsible agent. Begley,50 Dines,60 and Moody61 all argued that the acts and omissions doctrine does little to clarify a moral distinction between an act and an omission, thereby failing to distinguish a morally significant difference between passive euthanasia and active euthanasia on the sole basis of causation. This conclusion was later echoed by Snelling,47 who, like Moody,61 argued that in practice it may also be difficult to differentiate between acts and omissions. For instance, Snelling47 illustrated how the removal of a feeding tube can be regarded as both a case of passive euthanasia (i.e. withdrawing care; ‘letting die’) and a case of active euthanasia (i.e. ‘killing’). This would lend further support to the need for moral consistency across practices for, as Moody61 pointed out,
it is apparent that omissions can be just as effective as actions in terms of bringing about change…(t)he fact that one response was passive and the other active seems to have little bearing on the moral assessment of the situation. (p. 913)
Indeed, should a moral distinction exist, additional factors, such as the role of intention, must be taken into consideration.
Four authors examined the role of direct versus indirect intention, and more specifically, the doctrine of double effect.47,52,56,61 The doctrine of double effect seeks to describe the circumstances in which harmful actions (or omissions) are permitted ‘in the overall pursuit of good’ (p. 355).47 However, in order to satisfy these requirements – so as to justify the ‘two effects of one act (or omission)’ (p. 870)52 – the following conditions must be met:
1. The action itself must not be intrinsically bad; 2. The good effect must not be a direct consequence of the bad effect; 3. The good effect must be ‘directly intended’; the bad effect only ‘indirectly intended’, or ‘tolerated’; 4. The good effect must be equal to or greater than the bad effect. (p. 85)65
This would be exemplified by the nurse who provides large doses of opioids to manage pain, but through that act unintentionally hastens death. In the context of this body of literature, Goodman56 argued that the intent to kill inherent in euthanasia is not only what makes it a morally unacceptable choice but also what makes it morally distinct from actions sanctioned under the doctrine of double effect. However, Begley,50 Moody,61 and Snelling,47 argued that the morally significant difference between direct and indirect intention is not easily identifiable if both acts lead to death. In defence of moral congruence, Snelling47 suggested that the doctrine of double effect ‘allows us to deflect moral criticism and legal redress by arguing that we did not intend the death’ (p. 355), thus encouraging a particular type of hypocrisy. The argument that there is no morally significant distinction between direct and indirect intention or causation is a rejection of the doctrine of double effect as a valid ethical principle.
Nature of the social good
Six articles raised ethical questions in relation to the possible impact that the legalization of euthanasia might have on society more broadly. By ‘social good’, we are referring to what is perhaps more commonly known as ‘the common good’: ‘those facilities – whether material, cultural or institutional – that the members of a community provide to all members in order to fulfill a relational obligation they all have to care for certain interests that they have in common’ (para. 1).66 Four of the six articles argued against euthanasia based upon the nature of the social good, while two articles did not take a position on the topic.
Articles in this theme focused on questions such as ‘does assisted suicide harm society?’ (p. 22).21 Central to many of these arguments was an exploration of the existing social context upon which euthanasia would be layered. For instance, authors examined how existing social fragilities, such as vulnerable populations,21,27,46,67 fragmented healthcare teams,67 threats of cost containment,18,21,27,67 poor public understanding of euthanasia,67 and perceptions of burden at the end-of-life,21,27,67 would be affected should euthanasia be legalized. A number of articles examined the intersection of such concerns. For instance, Ericksen et al.67 argued that in an era of cost containment, euthanasia policies put vulnerable groups, such as the disabled, women, older people and the impoverished, at an ever-heightened risk for exploitation and harm. The authors stated, ‘there is a very real danger that patients and their family members will opt for euthanasia because of inadequate resources for care rather than because of well-informed, autonomous decision-making’ (p. 32).67 This concern for resources was echoed by Goodman56 who situated her argument within the good of palliative care. She questioned the rightness of alleviating suffering through euthanasia when many patients and families do not have access to high-quality palliative care or understand its goal of improving quality of life. Throughout these articles, there was a recognition of the complexity of interacting factors that would ultimately influence the goodness of euthanasia in a social context.
Discussion
In this narrative review, we have analysed the ethical arguments surrounding euthanasia in relationship to nursing practice based upon the nature of nursing; ethical principles, concepts and theories; moral consistency; and the nature of the social good. In the literature reviewed, arguments based within the first three categories were used to argue both for and against euthanasia. The latter category of the nature of the social good contained only arguments against or reflecting no opinion towards euthanasia.
Several limitations characterize this review. In that this was a review of published papers that asked and answered a focussed ethical question, there was no attempt to formally evaluate the overall robustness of this body of literature, although papers without a focussed ethical question were excluded from the review from the outset. Furthermore, only English language literature was reviewed. Another limitation of this review stems from our decision to not differentiate in the analysis between articles that addressed physician-assisted suicide from those that addressed euthanasia. One could argue that the ethical issues surrounding a clinician-administered death (euthanasia) might be quite different than a client-administered death (assisted suicide). To aid the reader in deciding whether this is relevant, we have included relevant definitions in the data extraction table. Interestingly, we were unable to locate any articles originating from the Netherlands, Belgium or Luxembourg. This may have been related to our search strategy that included only articles that had an explicit nursing focus.
Finally, we found a relative paucity of literature that addressed the ethical issues surrounding euthanasia in the context of nursing practice, a disproportionate number of articles published from the United States, and a surprising paucity of recent publications. These findings could be related to the perception that nursing has been viewed as having a limited role in euthanasia and, hence, the idea that debating the moral permissibility of the act is outside of the concern of nurses. However, evidence of the importance of the nursing role, particularly in dealing with those preliminary requests for euthanasia, has been well documented in the literature.7,68–71 The disproportionate ethical debate generated out of the United States may also be related to the American Nurses Association’s definitive stance against euthanasia.72 It is understandable that this definitive stance would have generated substantial ethical debate, considering client-administered euthanasia has been legal in a number of states for many years and is currently under consideration for legalization in others. The somewhat dated nature of many of these articles may not necessarily reflect current debates, particularly as it relates to the social good, which is largely context dependent.
The apparent lack of ethical debate from a Canadian perspective is more intriguing. Public advocacy in favour of euthanasia had been developing within Canada for many years prior to the 2016 legalization of euthanasia. However, early Canadian literature focusing on euthanasia was largely physician-centric and thus, nurses may not have been alerted to the implications for nursing practice. Therefore, nurses may not have fully considered the practical, ethical and philosophic implications of their role in this new practice. More recently, however, it was widely anticipated that Nurse Practitioners would play a key role, not only in assessing for eligibility but also in providing the means for clients to pursue an euthanasia. This unique role for Canadian nurses will likely generate more debate in the upcoming years.
Our goal in this article was to synthesize literature that specifically focused on the discipline of nursing in relation to euthanasia. This naturally leads to the question of how much of this literature is delineating ethical and moral issues that would be considered unique to nursing. Arguments based upon ethical principles, concepts and theories; moral consistency; and the nature of the social good are likely to be relevant across practice-related healthcare disciplines. Furthermore, the arguments put forward in relation to euthanasia are ones that apply to many healthcare situations encountered by nurses. But what about those arguments based upon the nature of nursing? One might argue that assumptions about nursing’s moral ontology could be applied to any discipline that might hold similar values (e.g. compassion, dignity). Likewise, arguments related to the impact that engaging in euthanasia could have on nursing and nurses could be applied just as well to medicine. However, the nature of the nurse–patient relationship may raise unique issues. For instance, nurses bear the responsibility of being the care providers who are closest to patients, witnessing the day-to-day experiences, and at times, suffering, of their patients. Yet, they often hold little power to influence the care decisions that shape these experiences. Particularly in the context of euthanasia, where suffering is a key concern, this places nurses in a unique social location. As such, we can expect that ethical and moral concerns of special interest to the discipline may arise. Further study of these concerns is important.
In conclusion, despite the relatively small volume of nursing-specific literature identified, the breadth of perspectives in argumentation was impressive. Disciplinary philosophical arguments, ethical principles, concepts and theories, as well as social justice arguments were all used to explore the ethical and moral implications of euthanasia for nursing. Likewise, the relative balance between supportive, opposed and no opinion provided diverse viewpoints upon which nurses can reflect. Taken together, this literature provides a fulsome range of positions for nurses to consider as they reflect on their role, both as individuals and as a discipline, in relation to euthanasia. While not neglecting traditional biomedical ethics, these articles challenged nurses to look beyond biomedical ethics to other questions relevant to the discipline of nursing. Is there something about the relationship between nurses and their patients that influences the moral acceptability of euthanasia? How does nursing’s location in an institutional and social hierarchy, and the social privilege accorded to nursing in our society, influence nurses’ considerations of social good beyond autonomy? From an individual perspective, does these articles support nurses to become morally consistent in our end-of-life nursing practices? In a related paper, we discuss some of the factors for nurses to consider as they engage with questions about their participation in euthanasia, factors such as their intuitional responses, the relational impacts of their decisions and their moral coherence with similar end-of-life decisions.73 Wrestling with questions such as these will provide important intellectual substance for nursing’s ongoing dialogue around its particular relationship with euthanasia. Articles identified within this review provide a range of arguments from a variety of perspectives for nurses to consider as the development of euthanasia continues to unfold within the international context.
Supplemental material
Supplemental Material, NEJ845127_SUPPLEMENTAL_MATERIAL_CLN for Nursing and euthanasia: A narrative review of the nursing ethics literature by Barbara Pesut, Madeleine Greig, Sally Thorne, Janet Storch, Michael Burgess, Carol Tishelman, Kenneth Chambaere and Robert Janke in Nursing Ethics
Note
‘Slippery slope arguments, which are regularly invoked in a variety of practical ethics contexts, make the claim that if some specific kind of action (such as euthanasia) is permitted, then society will be inexorably led (“down the slippery slope”) to permitting other actions that are morally wrong’ (Benatar, 2011, p. 206).
Footnotes
Authors’ note: Carol Tishelman is also affiliated with the Centre for Rural Medicine, Storuman Sweden and Stockholm Health Care Services, Stockholm Sweden.
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project is supported by a Canadian Institutes for Health Research Project Grant PJT-376065. Barbara Pesut is supported, in part, through the Canada Research Chairs Program.
ORCID iD: Barbara Pesut  https://orcid.org/0000-0002-1063-7190
https://orcid.org/0000-0002-1063-7190
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Sally Thorne, The University of British Columbia, Canada.
Janet Storch, University of Victoria, Canada.
Michael Burgess, University of British Columbia, Canada.
Carol Tishelman, Karolinska Institutet, Sweden.
Kenneth Chambaere, Vrije Universiteit Brussel; Belgium Ghent University, Belgium.
Robert Janke, University of British Columbia, Canada.
References
- 1. Supreme Court of Canada. An act to amend the criminal code and to make related amendments to other acts (medical assistance in dying), 2016, https://laws-lois.justice.gc.ca/eng/annualstatutes/2016_3/fulltext.html
- 2. Dalhousie University, Health Law Institute. End-of-life law & policy in Canada, http://eol.law.dal.ca/?page_id=236 (2018, accessed 10 September 2018). [Google Scholar]
- 3. Cohen J, Chambaere K. Euthanasia. Access Science, 2018, https://doi org/10.1036/1097-8542.246850
- 4. Canadian Nurses Association. National nursing framework on medical assistance in dying in Canada, 2017, https://www.cna-aiic.ca/∼/media/cna/page-content/pdf-en/cna-national-nursing-framework-on-maid.pdf
- 5. College of Licensed Practical Nurses of Manitoba, College of Registered Nurses of Manitoba and The College of Registered Psychiatric Nurses of Manitoba. Medical assistance in dying: guidelines for Manitoba nurses, 2018, https://www.crnm.mb.ca/uploads/ck/files/MAID%20guideline%20FINAL.pdf
- 6. De Bal N, Gastmans C, Dierckx de Casterle B. Nurses’ involvement in the care of patients requesting euthanasia: a review of the literature. Int J Nurs Stud 2008; 45: 626–644. [DOI] [PubMed] [Google Scholar]
- 7. Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum 2018; 53(4): 511–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Storch JL. Planned assisted suicide. Nurs Ethics 2011; 18(6): 753–755. [DOI] [PubMed] [Google Scholar]
- 9. Scanlon C. Assisted suicide: how should nurses respond? In: ICN 21st quadrennial congress, Vancouver, BC, Canada, 15–20 June 1997 Geneva: ICN. [Google Scholar]
- 10. Quaghebeur T, Dierckx de Casterle B, Gastmans C. Nursing and euthanasia: a review of argument-based ethics literature. Nurs Ethics 2011; 18: 735–755. [DOI] [PubMed] [Google Scholar]
- 11. The Joanna Briggs Institute. Joanna Briggs Institute reviewers’ manual: 2014 edition, 2014, http://joannabriggs.org/assets/docs/sumari/reviewersmanual-2014.pdf
- 12. Rietjens JA, Deschepper R, Pasman R, et al. Medical end-of-life decisions: does its use differ in vulnerable patient groups? A systematic review and meta-analysis. Soc Sci Med 2012; 74(8): 1282–1287. [DOI] [PubMed] [Google Scholar]
- 13. Steck N, Egger M, Maeseen M, et al. Euthanasia and assisted suicide in selected European countries and US states: systematic literature review. Med Care 2013; 51: 938–944. [DOI] [PubMed] [Google Scholar]
- 14. McGowan J, Sampson M, Salzwedel DM, et al. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 2016; 75: 40–46. [DOI] [PubMed] [Google Scholar]
- 15. Greenhalgh T, Thorne S, Malterud K. Time to challenge the spurious hierarchy of systematic over narrative reviews. Eur J Clin Invest 2018; 48(6): e12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McCullough L, Coverdale J, Chervenak FA. Constructing a systematic review for argument-based clinical ethics literature: the example of concealed medications. J Med Philos 2007; 32(1): 65–76. [DOI] [PubMed] [Google Scholar]
- 17. Mathes MM. Assisted suicide and nursing ethics. Medsurg Nurs 2004; 13(4): 261–264. [PubMed] [Google Scholar]
- 18. Coyle N. The assisted death and physician-assisted suicide debate: issues for nursing. Oncol Nurs Forum 1992; 19: 41–46. [PubMed] [Google Scholar]
- 19. Ferrell BR, Rivera LM. Nursing perspectives on assisted suicided and euthanasia. J Pain Palliat Care Pharmacother 1995; 3: 55–66. [Google Scholar]
- 20. Ogden R. AIDS, euthanasia and nursing. Nurs Stand 1996; 10: 49–51. [DOI] [PubMed] [Google Scholar]
- 21. Kopala B, Kennedy SL. Requests for assisted suicide: a nursing issue. Nurs Ethics 1998; 5(1): 16–26. [DOI] [PubMed] [Google Scholar]
- 22. Salmon B. On arguing from ethical principles to practical conclusions: nurses and assisted death. N Z Nurs J 1981; 74: 15–17. [PubMed] [Google Scholar]
- 23. Hawkey M. Doctors, nurses and physician-assisted suicide. J Nurs Manag 1997; 5(5): 259–261. [PubMed] [Google Scholar]
- 24. Tuten M. A death with dignity in Oregon. Oncol Nurs Forum 2001; 28: 58–65. [PubMed] [Google Scholar]
- 25. McCabe H. Nursing involvement in euthanasia: a ‘nursing-as-healing-praxis’ approach. Nurs Philos 2007; 8: 176–186. [DOI] [PubMed] [Google Scholar]
- 26. Thiele T, Dunsford J. Nurses leaders’ role in medical assistance in dying: a relational ethics approach. Nurs Ethics 2019; 26(4): 993–999. [DOI] [PubMed] [Google Scholar]
- 27. Kowalski SD. Assisted suicide: where do nurses draw the line? Nurs Health Care 1993; 14(2): 70–76. [PubMed] [Google Scholar]
- 28. Sullivan M. Ethics of assisted suicide and assisted death. Nurs Manag 1999; 30: 31–33. [PubMed] [Google Scholar]
- 29. Kowalski SD. Assisted suicide: is there a future? Ethical and nursing considerations. Crit Care Nurs Q 1996; 19(1): 45–54. [DOI] [PubMed] [Google Scholar]
- 30. Young MG, Ogden RD. The role of nurses in AIDS care regarding voluntary euthanasia and assisted suicide: a call for further dialogue. J Adv Nurs 2000; 31: 513–519. [DOI] [PubMed] [Google Scholar]
- 31. White BC. Assisted suicide and nursing: possibly compatible? J Prof Nurs 1999; 15(3): 151–159. [DOI] [PubMed] [Google Scholar]
- 32. Newham RA. An internal morality of nursing: what it can and cannot do. Nurs Philos 2014; 14: 109–116. [DOI] [PubMed] [Google Scholar]
- 33. Davis AJ. Selected issues in nursing ethics: clinical, philosophical, political. Bioethics Forum 1994; 10(1): 10–14. [PubMed] [Google Scholar]
- 34. Simpson R. Nursing ethics and assisted death. Complex questions surround the issue of the ‘right to die’. It helps to know the principles involved. Can Nurse 1992; 88: 36–38. [PubMed] [Google Scholar]
- 35. Wurzbach ME. Nursing perspectives on practitioner-assisted suicide. Nurs Outlook 2000; 48(3): 116–120. [DOI] [PubMed] [Google Scholar]
- 36. Ellis P. Euthanasia: the way to a peaceful end? Prof Nurs 1991; 7: 157–160. [PubMed] [Google Scholar]
- 37. Young A. Professional integrity and assisted suicide: a nursing view. Bioethics Forum 1994; 10(2): 11–13. [PubMed] [Google Scholar]
- 38. Jameton A. The nurse: when roles and rules conflict. Hastings Cent Rep 1977; 7: 22–23. [PubMed] [Google Scholar]
- 39. McCabe H. Nursing involvement in euthanasia: how sound is the philosophical support? Nurs Philos 2007; 8: 167–175. [DOI] [PubMed] [Google Scholar]
- 40. Zimbelman J. Changing the present legal prohibitions on assisted suicide is a bad idea. J Prof Nurs 1999; 15(3): 160–169. [DOI] [PubMed] [Google Scholar]
- 41. Johnson RA, Weiler K. Aid-in-dying: issues and implications for nursing. J Prof Nurs 1990; 6(5): 258–264. [DOI] [PubMed] [Google Scholar]
- 42. Beauchamp TL, Childress JF. 2013. Principles of biomedical ethics. 7th ed London: Oxford University Press. [Google Scholar]
- 43. Benedict S, Pierce AG, Sweeney S. Historical, ethical, and legal aspects of assisted suicide. J Assoc Nurses AIDS Care 1998; 9(2): 34–44. [DOI] [PubMed] [Google Scholar]
- 44. Daly BJ, Berry D, Fitzpatrick JJ, et al. Assisted suicide: implications for nurses and nursing. Nurs Outlook 1997; 45(5): 209–214. [DOI] [PubMed] [Google Scholar]
- 45. Erlen JA. Issues at the end of life. Orthop Nurs 1996; 15: 37–41. [DOI] [PubMed] [Google Scholar]
- 46. Sumodi V. Legalization of physician-assisted suicide: point/counterpoint. Nurs Forum 1995; 30(1): 11–17. [DOI] [PubMed] [Google Scholar]
- 47. Snelling PC. Consequences count: against absolutism at the end of life. J Adv Nurs 2004; 46(4): 350–357. [DOI] [PubMed] [Google Scholar]
- 48. Fontana JS. Rational suicide in the terminally ill. J Nurs Scholarsh 2002; 34: 147–151. [DOI] [PubMed] [Google Scholar]
- 49. Baumrucker SJ, Stolick M, Carter GT, et al. Legal but not always allowed: physician aid in dying. Am J Hosp Palliat Med 2011; 28: 449–454. [DOI] [PubMed] [Google Scholar]
- 50. Begley AM. Beneficent voluntary active euthanasia: a challenge to professionals caring for terminally ill patients. Nurs Ethics 1998; 5: 294–306. [DOI] [PubMed] [Google Scholar]
- 51. Farsides C. Euthanasia: failure or autonomy? Int J Palliat Nurs 1996; 2: 102–105. [DOI] [PubMed] [Google Scholar]
- 52. Begley AM. Acts, omissions, intentions and motives: a philosophical examination of the moral distinction between killing and letting die. J Adv Nurs 1998; 28(4): 865–873. [DOI] [PubMed] [Google Scholar]
- 53. Friend ML. Physician-assisted suicide: death with dignity? J Nurs Law 2011; 14: 110–116. [Google Scholar]
- 54. King P, Jordan-Welch M. Nursing-assisted suicide: not an answer in end-of-life care. Issues Ment Health Nurs 2003; 24: 45–57. [DOI] [PubMed] [Google Scholar]
- 55. Praskwiecz BH. Assisted suicide: right or wrong? Plast Surg Nurs 2000; 20: 37–40. [DOI] [PubMed] [Google Scholar]
- 56. Goodman ML. Is there a place for euthanasia in palliative care? Int J Palliat Nurs 1996; 2: 163–167. [DOI] [PubMed] [Google Scholar]
- 57. Begley AM. Guilty but good: defending voluntary active euthanasia from a virtue perspective. Nurs Ethics 2008; 15: 434–445. [DOI] [PubMed] [Google Scholar]
- 58. Rich KL, Butts JB. Rational suicide: uncertain moral ground. J Adv Nurs 2004; 46(3): 270–278. [DOI] [PubMed] [Google Scholar]
- 59. Noddings N. Caring: a feminine approach to ethics and moral education. Berkeley, CA: University of California Press, 1984. [Google Scholar]
- 60. Dines A. Does the distinction between killing and letting die justify some forms of euthanasia? J Adv Nurs 1995; 21: 911–916. [DOI] [PubMed] [Google Scholar]
- 61. Moody J. Assisted death: a need for reform. Nurs Stand 2003; 17: 40–44. [DOI] [PubMed] [Google Scholar]
- 62. Kuhse H. Sanctity of life and the role of the nurse. Aust Nurses J 1988; 18(2): 10–12. [PubMed] [Google Scholar]
- 63. Glover J. Causing death and saving lives. London: Penguin Books, 1977. [Google Scholar]
- 64. Callahan JC. Acts, omissions, and euthanasia. Public Aff Q 1988; 2: 21–36. [PubMed] [Google Scholar]
- 65. Campbell AV. Moral dilemmas in medicine. 3rd ed London: Churchill Livingstone, 1984. [Google Scholar]
- 66. Hussain W. Stanford encyclopedia of philosophy. The common good, https://plato.stanford.edu/entries/common-good/ (2018, accessed 10 September 2018).
- 67. Ericksen J, Rodney P, Starzomski R. When is it right to die? Can Nurse 1995; 91: 29–33. [PubMed] [Google Scholar]
- 68. Sheridan L. When patients ask to die: the role of nurses in medical assistance in dying. Master of Science in Nursing Thesis, Western University, London, ON, Canada, 2017. [Google Scholar]
- 69. Van de Scheur A, Van der Arend A. The role of nurses in euthanasia: a Dutch study. Nurs Ethics 1998; 5: 498–509. [DOI] [PubMed] [Google Scholar]
- 70. Denier Y, Gastmans C, De Bal N, et al. Communication in nursing care for patients requesting assisted death: a qualitative study. J Clin Nurs 2010; 19: 3372–3380. [DOI] [PubMed] [Google Scholar]
- 71. Denier Y, Dierckx de Casterle B, De Bal N, et al. ‘It’s intense, you know’. Nurses’ experiences in caring for patients requesting euthanasia. Med Healthcare Phil 2000; 13: 41–48. [DOI] [PubMed] [Google Scholar]
- 72. American Nurses Association. Euthanasia, assisted suicide, and aid-in-dying (Position statement for the American Nurses Association). Silver Spring, Moral distress: American Nurses Association, 2013. [Google Scholar]
- 73. Pesut B, Thorne S, Greig M. Shades of grey: conscientious objection in medical assistance in dying. Nurs Inq 2019; 4: e12308. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, NEJ845127_SUPPLEMENTAL_MATERIAL_CLN for Nursing and euthanasia: A narrative review of the nursing ethics literature by Barbara Pesut, Madeleine Greig, Sally Thorne, Janet Storch, Michael Burgess, Carol Tishelman, Kenneth Chambaere and Robert Janke in Nursing Ethics