Abstract
Objective:
Women with schizophrenia appear to be diagnosed with breast cancer at later stages of the disease compared to the general population. To study this disparity, this report reviews and quantifies the differences in rates of screening mammography for women with schizophrenia and other psychotic disorders compared to the general population.
Methods:
A systematic literature search was conducted in PubMed, Embase, Web of Science and PsycInfo databases. Each database was searched from inception to September 14, 2018. The search strategy included search terms for breast cancer, mammography, schizophrenia and psychosis. Two reviewers independently screened and evaluated eligible studies. The main outcome measure was rate of screening mammography for women with schizophrenia and psychotic disorders versus rate in comparable population without these diagnoses. Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines were used for abstracting data and the Newcastle-Ottawa Scale was used for assessing data quality. A random effects model meta-analysis was performed.
Results:
From a total of 304 abstracts reviewed, 11 studies met the inclusion criteria, representing 25,447 women with diagnoses of schizophrenia or psychosis across 4 countries. The meta-analysis showed a pooled odds ratio of 0.50 (95% CI 0.38–0.64, P<0.001), indicating that women with schizophrenia are less likely to receive screening mammography. In subgroup analysis, this association was not significantly affected by quality of the study.
Conclusions:
Women with schizophrenia and other psychotic disorders are about half as likely to receive screening mammography as the general population. Further research is needed to determine causes of this disparity.
BACKGROUND
Individuals with serious mental illness, such as schizophrenia and bipolar disorder, die, on average, 15–20 years earlier than the general population, and the mortality gap is widening.(1–3) The leading causes of death are cardiovascular disease and cancer, suggesting that access to timely and appropriate preventive services for this population could help reduce premature deaths. An improved understanding of issues concerning early cancer detection is one important step in identifying potential causes of early mortality in individuals with serious mental illness.
Breast cancer is of particular interest, as the five-year survival rate for people with breast cancer is nearly 90% due to substantial efforts to increase awareness and screening among American women.(4) Although there is debate in the field regarding screening mammography recommendations,(5–8) the current United States Preventive Services Task Force (USPSTF) guidelines recommend biennial screening mammography for women aged 50 to 74 years.(9) Unfortunately, evidence suggests that women with serious mental illness may not receive these preventative services in a timely and appropriate way.(10) Recent work has found that breast cancer is identified at later stages, characterized by larger tumor sizes, more lymph node involvement and higher grade tumors, in women with serious mental illness when compared to women without these disorders.(11)
In 2014, Mitchell and colleagues conducted a meta-analysis examining breast cancer screening among women with distress or any mental illness, finding that screening mammography rates were lower in women with mental illness.(12) Upon further stratification by diagnosis, they found that women they defined as having “serious mental illness” were almost 50% less likely to receive mammography compared to women without mental illness. However, this study grouped together multiple diagnoses under the category of serious mental illness, which may mask some of the diversity and variation of presentation. For example, while serious mental illness is defined by the National Institutes for Mental Health as psychiatric disorders leading to severe functional impairment, the nature of symptoms and impairment in different psychiatric disorders can vary widely between schizophrenia, bipolar disorder and major depressive disorder. Notably, the type of mental illness appears to affect breast cancer screening rates in some studies.(13, 14)
Because of this limitation, we chose to focus on women with diagnoses of schizophrenia and other psychotic disorders (e.g. schizoaffective disorder) due to robust evidence that this group is more likely to have severe functional impairment and may face additional challenges in accessing care due to cognitive impairment related to psychiatric symptoms.(13) In addition, some studies have found that women diagnosed with schizophrenia face greater stigma,(15) are less likely to attend primary care visits (16, 17) and may have more difficulty with unfamiliar providers.(18) These contributing factors could make access to the health care system, health education and arranging mammography screening particularly burdensome to these individuals.
This paper aims to summarize the literature to-date on screening mammography rates and focus on disparities in care for women with schizophrenia and other psychotic disorders. To our knowledge, this is the first systematic review to distinguish screening mammography rates for this specific population, quantifying the degree of disparity in a meta-analysis.
METHODS
Protocol and Registration
This systematic review was conducted with reference to the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement, using a protocol registered at the PROSPERO International Prospective Register of Systematic Reviews database (https://www.crd.york.ac.uk/prospero/).(19)
Eligibility Criteria and Study Selection
Studies were eligible if they included women with a diagnosis of schizophrenia or related psychotic disorder such as schizoaffective disorder, as defined by meeting diagnostic criteria of DSM-5 (295.xx) and ICD-10 (F20.x, F25.x) or other valid measures as have been previously described.(20) We did not aim to analyze studies that report screening mammography rates for women with distress, delirium, dementia, developmental disorders, eating disorders, nonpsychotic mood disorders or substance use disorders. Studies had to meet the following inclusion criteria: 1) report on the primary outcome measure of screening mammography; 2) compare screening mammography rates to a control population of women meeting recommended breast cancer screening guideline criteria; and 3) provide sufficient data to calculate relative risk or odds ratios. Of note, because breast cancer screening guidelines have changed over time, the article authors were expected to use screening guidelines that were applicable during the specific time frame of each study.(9) Studies in any language were included. Rates of diagnosis of breast cancer and treatment were not reviewed in this paper.
Search and Information Sources
With a research librarian who specializes in systematic reviews, one author (A.H.) conducted a search of the PubMed, Embase, Web of Science and PsycInfo electronic databases using relevant keywords in the title, abstract and subject descriptors. Databases were searched from their start date to September 14, 2018. An iterative process was used to determine the search terms, which were breast cancer, breast neoplasm, mammogram, mammography combined with screening or routine and schizophrenia, schizophrenic, psychotic, psychosis, severe mental illness. Titles and abstracts were then independently reviewed to determine if they met inclusion criteria by two authors (A.H. and K.W.). Two authors (A.H. and K.W.) also manually reviewed reference lists and bibliographies of the included articles for additional relevant studies. Any disagreements were arbitrated by a third author (C.M.).
Data Extraction
Data were extracted independently by two authors (A.H. and K.W.) using a predetermined spreadsheet. Categories extracted were: country/location, setting, type of study, population, time period, sample size, data collection method, covariates, main outcome measures, and results, including adjustment for factors and statistical analysis. For any missing data or clarification, we attempted to contact authors directly up to three times.
Data Analysis
Quality was assessed using the Newcastle Ottawa Scale, independently rated by two authors (A.H. and K.W.).(21) Quality ratings could range from 0–8, with points given for representativeness of population and control, ascertainment of data, reported outcome, comparability, assessment of outcome, sufficient length of study and adequacy of follow up period. Studies receiving 7–8 points were considered “high” quality, 5–6 points “medium” quality, and 4 points or lower “low quality.”
The primary outcome of interest was rate of screening mammography for women with schizophrenia and psychotic disorders compared to rates in the general eligible population. We compared screening mammography rates for women with the specified diagnoses to the general population using odds ratios, including adjusted risk estimates when these were available. We calculated odds ratios (ORs) from the raw number of cases and controls when no such risk estimate was reported. All analyses were conducted on the log scale using a random effects model. The meta-analyses results were graphically displayed in a forest plot. Statistical heterogeneity was assessed with the I2 and Cochrane’s Q statistic. Publication bias assessment was done using a funnel plot with Begg’s and Egger’s tests.(22) We also performed subgroup analyses of the low and medium quality studies and reported these findings in addition to the primary study findings. All analyses were performed using Stata 15.1 (StataCorp LP, College Station, TX, USA).
RESULTS
Identification and Description of Studies
Of the 408 abstracts reviewed, 104 were duplicates and another 229 were excluded based on title and abstract. In total, 75 articles were retrieved and assessed for eligibility and 11 met the inclusion criteria (Literature Search Flow Diagram in online supplement).(14, 18, 23–31) Common reasons for exclusion were that the study was not comparative or participants with diagnoses of schizophrenia or psychosis could not be extracted separately from others with severe mental illness. The final 11 studies included in this review are summarized in a table (see online supplement). Of these, 7 were considered high quality, 3 medium quality and 1 low quality. The studies were conducted in a range of settings (inpatient and outpatient, community clinic, multisite research centers, privately and publicly insured populations) and included data from 446,475 control participants and 25,447 women with diagnoses of schizophrenia or other psychotic disorders. Seven studies were conducted in the US, two in the United Kingdom, one in Denmark and one in Canada. Data were collected using nationwide registries, administrative claims databases from insurers and individual surveys. Three studies used survey responses linked with databases.
Meta-Analysis
The random effects meta-analysis yielded a pooled OR of 0.50 (95% CI 0.38–0.64, P<0.001), reflecting that women with schizophrenia and other psychotic disorders are about half as likely to receive screening mammography as the general population (Figure 1). The I2 (96.4%) statistic indicated a high level of heterogeneity. Based on visual inspection, the funnel plot was symmetrical and neither the Begg (P=0.24) nor Egger bias test (P = 0.88) demonstrated evidence of publication bias.
Figure 1.
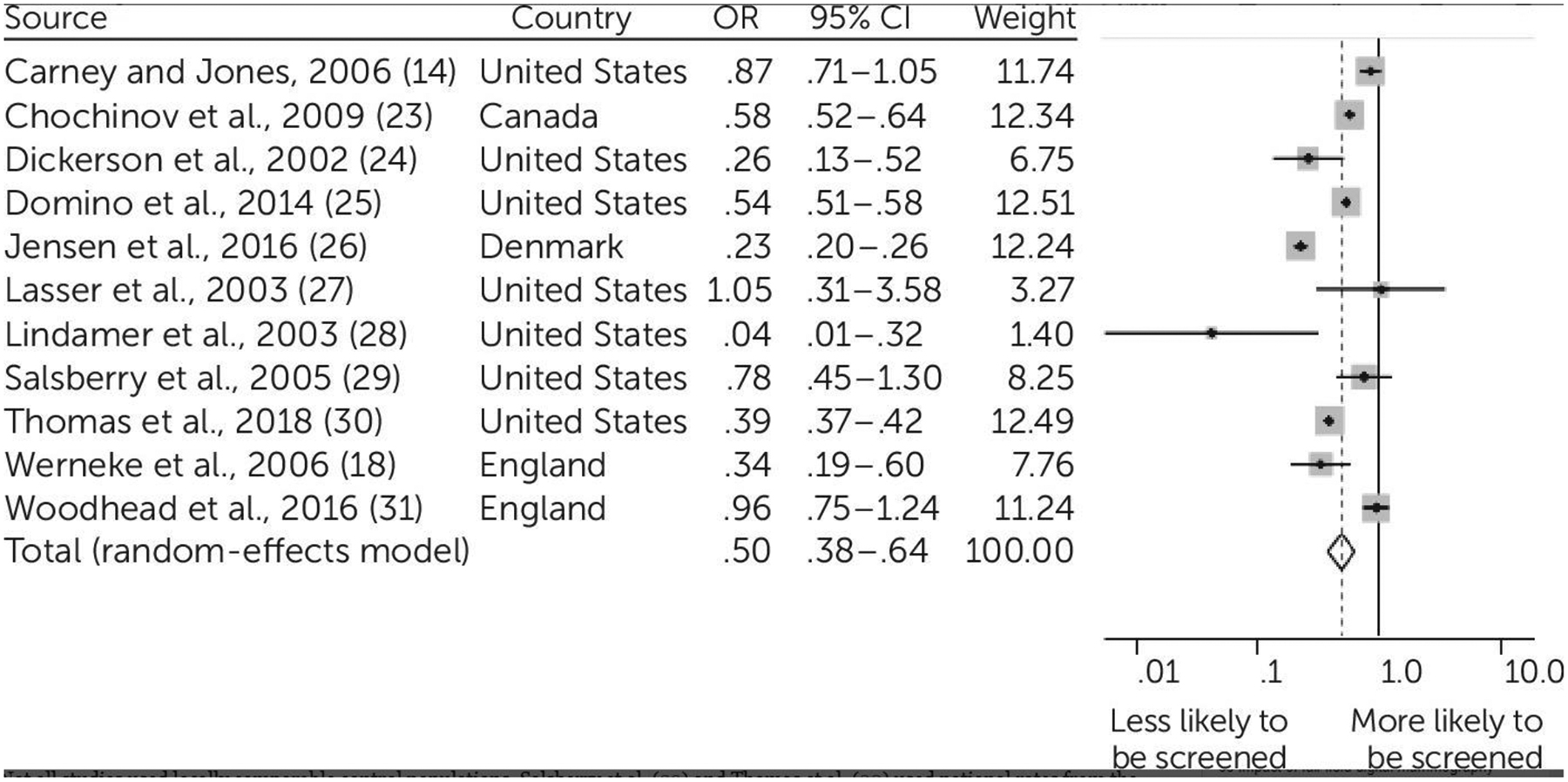
Pooled odds ratios comparing screening mammography rates for women with schizophrenia to general population
Not all studies used locally comparable control populations. Salsberry et al.(29) and Thomas et al.(30) reference national rates from the National Health Interview Survey from the time of study, while Domino’s(25) comparison population was individuals with other chronic medical conditions. In subgroup analyses that examine low and medium quality studies, overall findings did not change significantly (for the low/medium quality subgroup: OR=0.48, 95% CI 0.36–0.65, P<0.001; for the remaining high quality studies: OR=0.51, 95% CI 0.31–0.85, P=0.009).
DISCUSSION
Women with schizophrenia and other psychotic disorders were about half as likely to be screened for breast cancer as the general population. To our knowledge, this is the first meta-analysis to focus specifically on screening mammography rates for women with psychotic disorders. This study extends findings from previous reviews to highlight a disparity across 4 countries, in privately and publicly insured populations, at academic research centers and community clinics, and in inpatient and outpatient populations. Our review includes nearly double the number of publications as a previous review on screening mammography for women with mental illness,(12) enabling us to evaluate breast cancer screening provision for over 25,000 women with diagnoses of schizophrenia and other psychotic disorders.
There are a number of limitations of our study. First, all studies came from Western countries, primarily the United States, so findings may not be generalizable to other countries. However, four countries were included, reflecting screening rates in a Nordic country, Canadian and UK national health systems as well as private and public systems in the US. Second, criteria for screening mammography vary across countries as well as time, with the USPSTF altering its recommendations in 2009 to routinely screen only women 50–75 years of age. However, the changes in guidelines would not be expected to affect disparities in screening in our analyses, as the comparisons are between women with and without schizophrenia were receiving care under the same guidelines at that period. Third, there was considerable heterogeneity between studies. One reason for this may be that we could not determine severity of illness based on diagnosis. This is important since Carney et al. suggest that severity of mental illness, not specific diagnosis, may be the more important factor in accessing preventive care services. Fourth, it is possible that other factors drive low screening mammography rates such as socioeconomic status, race/ethnicity, or access to primary care, though we used adjusted odds ratios when possible, and multiple studies attempted to control for demographic factors and co-morbidities. Despite these limitations, we found a strong summary result that women with schizophrenia and other psychotic disorders receive screening mammography at lower rates than the general population, which is consistent with prior studies showing lower rates of preventive health services for individuals with serious mental illness.(32–34)
While Lasser et al.(27) was the one study that found higher rates of screening mammography in women with psychosis compared to a control population, it was the smallest of the included studies, with only 12 women with psychosis diagnoses. It is possible that there was selection bias in the participants in this study, such that they were more engaged in health care services than other patients with similar diagnoses.
Lower screening rates could explain why women with schizophrenia and other serious mental illnesses are found to have more advanced breast cancer at time of diagnosis.(11) In addition, poor screening is concerning given a recent literature review finding that women with schizophrenia have higher incidence of breast cancer and higher mortality rates due to breast cancer compared to the general population.(35, 36) It is important to note that these studies of cancer incidence and mortality have considerable heterogeneity, however, and it can be difficult to account for socioeconomic confounding factors.
Some barriers to adequate screening may apply to populations with and without mental illness. Having a regular primary care provider appears to promote preventive care such as cancer screening in the general population, and utilization of primary care services increases screening mammography rates among women with serious mental illness.(37, 38) Other studies of mammography utilization in the general population find lower probability of screening mammography receipt in areas of poverty and ethnic segregation.(39) Other barriers to cancer screening in the general population include lack of test awareness, fear, poor communication and limited financial resources.(40, 41)
However, individuals with serious mental illness may also face additional challenges to accessing appropriate cancer screening. In a survey of participants with psychiatric disorders at a community-based wellness center, the main barrier to mammography screening was identified as physicians not suggesting cancer screening to patients and failure to communicate the importance of screening, rather than access to a primary care provider or to the screening procedure itself.(42) With time constraints, primary care providers and psychiatrists may not prioritize cancer screening for patients with serious mental illness-rather, they may focus on metabolic disorder monitoring, which is increasingly recognized as being a side effect of psychotropic medications and a driver of early morbidity in this population.(43) The increased focus on addressing psychiatric symptoms may lead to deferring routine preventive screening discussion for future visits, but the future discussion never occurs. Some providers might defer screening because they believe individuals with serious mental illness will have difficulties following through with treatment such as radiation and chemotherapy.(17)
Given that patients with serious mental illness may need more in-depth communication and guidance to follow up with cancer screening procedures, such as mammography and colonoscopy, creative models are needed for emphasizing the importance of preventive care for individuals with serious mental illness. As an inverse of the collaborative care model, a care manager, social worker or nurse may be able to play a critical role in connecting these patients with necessary cancer screening services in specialty mental health settings.(44, 45) Based on the latest Cochrane review, no evidence-based interventions have been identified yet for increasing cancer screening rates for people with severe mental illness.(46) New strategies are being trialed to link the population with serious mental illness and diagnosed cancer to services, with support from mental health and oncology providers, but the initial screening remains a barrier to timely and appropriate treatment.(47)
Prior studies have found disparities in breast cancer screening rates based on race/ethnicity and income, with minority and low-income women less likely to receive screening per guidelines. Our finding that women with schizophrenia and psychosis are about half as likely to be screened supports the argument that the population with severe mental illness should be designated as a health disparity population, with special funding to target disparities in care.(48, 49) Future studies are needed to determine whether there are further differences in mammography screening rates among women who have schizophrenia based on race or ethnicity.
CONCLUSION
Given the high prevalence of breast cancer and promising prognosis if detected early, screening mammography is a key first step in improving diagnosis and treatment for people living with schizophrenia. This review quantifies the inequity in breast cancer screening, and highlights the need for novel strategies to promote screening mammography for women with schizophrenia.
Supplementary Material
HIGHLIGHTS.
This systematic review and meta-analysis examined differences in rates of breast cancer screening for women diagnosed with schizophrenia compared to the general population.
Women diagnosed with schizophrenia were about half as likely to receive breast cancer screening according to guidelines compared to the general population.
There was considerable heterogeneity across studies, but a strong summary result of lower rates of screening mammography for women with schizophrenia.
Further work is needed to understand underlying causes of this disparity, and to develop interventions to promote breast cancer screening for this vulnerable population.
Acknowledgements:
Thanks to I. Elain Allen, Evans Whitaker, Nicholas A. Riano for assistance and guidance on literature search and data analysis.
Funding: Dr. Hwong receives funding from R25 MH060482. This publication was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number UL1 TR001872. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Contributor Information
Alison Hwong, University of California, San Francisco; Department of Psychiatry; UCSF Weill Institute for Neurosciences.
Kara Wang, University of California, San Francisco School of Medicine.
Stephen Bent, University of California, San Francisco; Department of Medicine.
Christina Mangurian, University of California, San Francisco; Department of Psychiatry; UCSF Weill Institute for Neurosciences.
REFERENCES
- 1.Saha S, Chant D, and McGrath J, A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry, 2007. 64(10): p. 1123–31. [DOI] [PubMed] [Google Scholar]
- 2.Olfson M, et al. , Premature mortality among adults with schizophrenia in the United States. JAMA psychiatry, 2015. 72(12): p. 1172–1181. [DOI] [PubMed] [Google Scholar]
- 3.(NIMH), N.I.o.M.H. Serious Mental Illness (SMI) among U.S. Adults 2015. March 4, 2016]; Available from: http://www.nimh.nih.gov/health/statistics/prevalence/serious-mental-illness-smi-among-us-adults.shtml.
- 4.Prevention, C.f.D.C.a. Cancer Survival in the United States. 2017. December 7, 2017 October 1, 2018]; Available from: https://www.cdc.gov/cancer/dcpc/research/articles/concord-2-supplement.htm.
- 5.Bleyer A and Welch HG, Effect of three decades of screening mammography on breast-cancer incidence. New England Journal of Medicine, 2012. 367(21): p. 1998–2005. [DOI] [PubMed] [Google Scholar]
- 6.Bleyer A, Screening mammography: update and review of publications since our report in the New England Journal of Medicine on the magnitude of the problem in the United States. Academic radiology, 2015. 22(8): p. 949–960. [DOI] [PubMed] [Google Scholar]
- 7.Mandelblatt J, To screen or not to screen older women for breast cancer: a new twist on an old question or will we ever invest in getting the answers? 2007, American Society of Clinical Oncology. [DOI] [PubMed] [Google Scholar]
- 8.Lash TL, et al. , Mammography surveillance and mortality in older breast cancer survivors. Journal of Clinical Oncology, 2007. 25(21): p. 3001–3006. [DOI] [PubMed] [Google Scholar]
- 9.US Preventive Services Task Force. Breast Cancer: Screening. 2016; Available from: https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening1.
- 10.Hwong AR and Mangurian C, Improving Breast Cancer Screening and Care for Women With Severe Mental Illness. Journal of Clinical Oncology, 2017: p. JCO.2017.76.0462. [DOI] [PubMed] [Google Scholar]
- 11.Iglay K, et al. , Diagnosis and treatment delays among elderly breast cancer patients with pre-existing mental illness. Breast Cancer Research and Treatment, 2017: p. 1–9. [DOI] [PubMed] [Google Scholar]
- 12.Mitchell AJ, P. I, Yadegarfar M, Pepereke S, Mugadza V, Stubbs B, Breast cancer screening in women with mental illness: comparative meta-analysis of mammography uptake. Br J Psychiatry, 2014. 205(6): p. 428–435. [DOI] [PubMed] [Google Scholar]
- 13.Aggarwal A, Pandurangi A, and Smith W, Disparities in breast and cervical cancer screening in women with mental illness: a systematic literature review. American journal of preventive medicine, 2013. 44(4): p. 392–398. [DOI] [PubMed] [Google Scholar]
- 14.Carney CP and Jones LE, The influence of type and severity of mental illness on receipt of screening mammography. Journal of general internal medicine, 2006. 21(10): p. 1097–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henderson C, E.-L. S, Thornicroft G, Mental illness stigma, help seeking, and public health. Am J Public Health, 2013. 103(5): p. 777–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garcia Maria E., et al. , Nonpsychiatric Outpatient Care for Adults With Serious Mental Illness in California: Who Is Being Left Behind? Psychiatric Services, 2017. 68(7): p. 689–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mangurian C, et al. , A Doctor is in the house: Stakeholder focus groups about expanded scope of practice of community psychiatrists. Community Ment Health J, 2017: p. 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Werneke U, H. O, Maryon-Davis A, Wessley S, Donnan S, McPherson K, Uptake of screening for breast cancer in patients with mental health problems. J Epidemiol Community Health, 2006. 60(7): p. 600–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D, L. A, Tetzlaff J, Altman DG, The PRISMA Group, Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine, 2009. 6(7): p. e100097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mangurian C, S. D, Newcomer JW, Vittinghoff E, Essock S, Zhu Z, et al. , Comorbid diabetes and severe mental illness: outcomes in an integrated health care delivery system. JGIM, 2019: p. forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Institute, T.O.H.R., Newcastle-Ottawa Quality Assessment Scale.
- 22.Egger M, S. G, Altman DG, Systematic Reviews in Health Care: Meta-Analysis in Context. 2nd. ed 2001, London: BMJ Publishing Group. [Google Scholar]
- 23.Chochinov HM, M. P, Prior HJ, Fransoo R, Burland E, Does a diagnosis of schizophrenia reduce rates of mammography screening? A Manitoba population-based study. Schizophr Res, 2009. 113: p. 95–100. [DOI] [PubMed] [Google Scholar]
- 24.Dickerson FB, P. A, Origoni AE, Health behaviors and health status of older women with schizophrenia. Psych Services, 2002. 5f3: p. 882–884. [DOI] [PubMed] [Google Scholar]
- 25.Domino ME, B. C, Lichstein JC, Farley JF, Morrissey JP, Ellis AR, et al. , Heterogeneity in the quality of care for patients with multiple chronic conditions by psychiatric comorbidity. Med Care, 2014. 52(Suppl 3): p. S101–109. [DOI] [PubMed] [Google Scholar]
- 26.Jensen LF, P. A, Bech BH, Andersen B, Vedsted P, Psychiatric morbidity and non-participation in breast cancer screening. Breast, 2016. 25: p. 38–44. [DOI] [PubMed] [Google Scholar]
- 27.Lasser KE, Z. H, Miller E, Becker AE, Hermann RC, Bor DH, Do women who screen positive for mental disorders in primary care have lower mammography rates? Gen Hosp Psychiatry, 2003. 25(3): p. 214–216. [DOI] [PubMed] [Google Scholar]
- 28.Lindamer LA, et al. , A comparison of gynecological variables and service use among older women with and without schizophrenia. Psychiatric Services, 2003. [DOI] [PubMed] [Google Scholar]
- 29.Salsberry PJ, Chipps E, and Kennedy C, Use of general medical services among Medicaid patients with severe and persistent mental illness. Psychiatric Services, 2005. [DOI] [PubMed] [Google Scholar]
- 30.Thomas M, et al. , Mammography Among Women With Severe Mental Illness: Exploring Disparities Through a Large Retrospective Cohort Study. Psychiatric Services, 2017: p. appi. ps. 201600170. [DOI] [PubMed] [Google Scholar]
- 31.Woodhead C, C. R, Ashworth M, Barley E, Stewart RJ, Henderson MJ, Cervical and breast cancer screening uptake among women with serious mental illness: a data linkage study. BMC Cancer, 2016. 16(1): p. 819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Druss BG, et al. , Quality of preventive medical care for patients with mental disorders. Medical care, 2002. 40(2): p. 129–136. [DOI] [PubMed] [Google Scholar]
- 33.Mangurian C, et al. , Low Rates of HIV Testing Among Adults With Severe Mental Illness Receiving Care in Community Mental Health Settings. Psychiatr Serv, 2017. 68(5): p. 443–448. [DOI] [PubMed] [Google Scholar]
- 34.Mangurian C, et al. , Diabetes Screening Among Underserved Adults With Severe Mental Illness Who Take Antipsychotic Medications. JAMA Internal Medicine, 2015. 175(12): p. 1977–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhuo Chuanjun, T. R, Jiang Ronghuan, Lin Xiaodong, Shao Mingjing, Cancer mortality in patients with schizophrenia: systematic review and meta-analysis. Br J Psychiatry, 2017. 211(1): p. 7–13. [DOI] [PubMed] [Google Scholar]
- 36.Zhuo C, P. T, Association of schizophrenia with the risk of breast cancer incidence: a meta-analysis. JAMA Psychiatry, 2018. 75(4): p. 363–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller E, L. K, Becker A, Breast and cervical cancer screening for women with mental illness: patient and provider perspectives on improving linkages between primary care and mental health. Arch Women’s Ment Health, 2007. 10(5): p. 189–197. [DOI] [PubMed] [Google Scholar]
- 38.Starfield B, S. L, Macinko J, Contribution of primary care to health systems and health. Milbank Q, 2005. 83: p. 457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mobeley LR, K. T, Clayton LJ, Evans WD, Mammography facilities are accessible, so why is utilization so low? Cancer Causes Control, 2009. 20(6): p. 1017–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lauver DR, S. L, Kane JH, Henriques JB, Tailored messages, external barriers, and women’s utilization of professional breast cancer screening over time. Cancer, 2003. 97(11): p. 2724–2735. [DOI] [PubMed] [Google Scholar]
- 41.O’Malley MS, E. J, Hawley ST, Schell MJ, Mathews JF, Mitchell J, The association of race/ethnicity, socioeconomic status, and physician recommendation for mammography: who gets the message about breast cancer screening? Am J Public Health, 2001. 91(1): p. 49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rockson LE, S. M, Pratt C, Cancer screening among peer-led community wellness center enrollees. Journal of Psychosocial Nursing and Mental Health Services, 2016. 54(3): p. 36–40. [DOI] [PubMed] [Google Scholar]
- 43.Mangurian C, et al. , Diabetes and Cardiovascular Care Among People with Severe Mental Illness: A Literature Review. Journal of General Internal Medicine, 2016. 31(9): p. 1083–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Katon W, et al. , Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry, 1999. 56(12): p. 1109–15. [DOI] [PubMed] [Google Scholar]
- 45.Mangurian C, et al. , Utilization of the Behavior Change Wheel framework to develop a model to improve cardiometabolic screening for people with severe mental illness. Implementation Science, 2017. 12(1): p. 134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barley EA, B. R, Walters P, Tylee A, Interventions to encourage uptake of cancer screening for people with severe mental illness. Cochrane Database of Systematic Reviews, 2016(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Irwin KE, P. E, Fields LE, Corveleyn AE, Greer JA, Perez GK, et al. , Bridge: Person-centered collaborative care for patients with serious mental illness and cancer. Oncologist, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goldman ML, Spaeth-Rublee B, and Pincus HA, The case for severe mental illness as a disparities category. Psychiatric services, 2018: p. appi. ps. 201700138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bartels SJ, D. P, Why serious mental illness should be designated a health disparity and the paradox of ethnicity. Lancet Psychiatry, 2017. 4(5): p. 351–352. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


