Abstract
Objectives.
To describe the effect of monopolar electrocautery (EC) settings on surgical plume particulate concentration during pediatric tonsillectomy.
Study Design.
Cross-sectional study.
Setting.
Tertiary medical center.
Subjects and Methods.
During total tonsillectomy exclusively performed with EC, air was sampled with a surgeon-worn portable particle counter. The airborne mean and maximum particle concentrations were compared for tonsillectomy performed with EC at 12 W vs 20 W, with smoke evacuation system (SES) and no smoke evacuation (NS).
Results.
A total of 36 children were included in this analysis: 9 cases with EC at 12 W and SES (12SES), 9 cases with EC at 20 W and SES (20SES), 9 cases with EC at 12 W without SES (12NS), and 9 cases with EC at 20 W without SES (20NS). Mean particle number concentration in the breathing zone during tonsillectomy was 1661 particles/cm3 for 12SES, 5515 particles/cm3 for 20SES, 8208 particles/cm3 for 12NS, and 78,506 particles/cm3 for 20NS. There was a statistically significant difference in the particle number concentrations among the 4 groups. The correlation between the particle number concentration and EC time was either moderate (for 12SES) or negative (for remaining groups).
Conclusion.
Airborne particle concentrations during tonsillectomy are over 9.5 times higher when EC is set at 20 W vs 12 W with NS, which is mitigated to 3.3 times with SES. Applying lower EC settings with SES during pediatric tonsillectomy significantly reduces surgical plume exposure for patients, surgeons, and operating room personnel, which is a well-known occupational health hazard.
Keywords: electrocautery, pediatric otolaryngology, surgical plume, tonsillectomy
Tonsillectomy remains the second most common surgical procedure in the United States, with a national analysis in 2017 estimating 289,000 ambulatory cases were performed in children <15 years of age.1 Over time, indications for tonsillectomy have shifted toward obstructive etiologies and away from infectious pathologies in younger children.2 Several surgical techniques (“hot” [coblation, electrocautery, harmonic scalpel, and radiofrequency] and “cold” [stainless steel]) exist for tonsillectomy with an overall aim to improve patient safety, clinical efficacy, and operative efficiency. These goals are achieved by reducing operative time, intraoperative blood loss, postoperative complications, and surgical cost.3 An American Society of Pediatric Otolaryngology survey performed by Walner and colleagues4 revealed a dramatic shift in instrument choice for tonsillectomy toward monopolar electrocautery (EC); 57.0% and 41.3% of pediatric otolaryngologists exclusively use EC for total tonsillectomy and adenoidectomy, respectively. This trend likely reflects the importance placed by surgeons on procedural speed and precision as well as the availability of user-friendly devices for tonsillectomy.
With this significant change in surgical instrumentation for tonsillectomy, notable concerns exist regarding the potentially harmful by-products produced by powered surgical device technology, chiefly EC. Briefly, surgical plume is created when EC heats target tissue to a boiling point, leading to membrane rupture and dispersal of cellular contents as fine particulates.5 The resultant product is composed of 95% water and 5% particulate matter, which is composed of chemicals, blood products, tissue particles, viruses, and bacteria.6 Particulate matter size is dictated by device, with electrosurgical units creating particles roughly 0.07 μm in size. Liberated particulate size is an important concept to understand; overall, inhaled particulates ≥5 μm are deposited in various regions of the respiratory system, including nasal passages, nasopharynx, trachea, and bronchial bifurcations, while particulates <2 μm deposit into the respiratory bronchioles and lung alveoli.7 Traditional surgical masks capture particles >5 μm but offer little protection against particles produced by EC, which liberate by-products <1 μm in size. The chemical composition of surgical plume is a combination of hydrocarbons, phenols, nitriles, and fatty acids.8 Specifically, carbon monoxide, acrylonitrile, and hydrogen cyanide within surgical plume receive the most attention given their known harmful effects. The estimated mutagenic effect of surgical plume condensate from 1 g of cauterized tissue is equivalent to 6 unfiltered cigarettes9; these by-products have been shown to induce dose-dependent acute and chronic inflammatory changes within the respiratory tract and include alveolar congestion, bronchiolitis, emphysematous changes, and interstitial pneumonia.10 Furthermore, although EC is potentially less hazardous than laser technology with regard to disease transmission, human papillomavirus virions have been shown to be present in surgical plume with intact infectivity.11 Thus, surgical plume has been strongly demonstrated to be cytotoxic, genotoxic, and mutagenic.8 Key factors that appear to affect the amount and content of surgical plume include procedure type, surgical technique, target tissue pathology, type of energy imparted, device power levels, and degree of cut, coagulation, or ablation performed.12 To address these vocational risks, previous work by Lee and colleagues13 established SES as an effective technique to significantly reduce the risk of surgical plume exposure, and recommended routine SES utilization in the operating room.
While multiple investigations have discussed the impact of surgical plume in the medical and surgical subspecialties of dermatology, general surgery, plastic surgery, surgical oncology, and urology,10,14–17 limited information exists regarding exposure to surgical plume in pediatric otolaryngology procedures. Thus, this clinical study aims to evaluate the degree of airborne particulates that otolaryngologists, operating room staff, and surgical patients are exposed to during standard total tonsillectomy in children and assess direct ramifications of adjusting EC settings and selective SES deployment. To our knowledge, this analysis represents the only current report of surgical plume particulate concentrations following pediatric total tonsillectomy in North America.
Materials and Methods
Study Design
Surgical plume generated via an EC surgical device was evaluated during standard total tonsillectomy in children <15 years of age at time of surgery. During total tonsillectomy, 2 protocols were employed. The first group underwent bilateral tonsillectomy with an electrosurgical pencil (Valleylab Electrosurgical Pencil Button Switch; Covidien, Mansfield, Massachusetts) and surgical plume evacuation by a surgical assistant using a Dynarex Sterile Yankauer Suction Handle (Cardinal Health, Waukegan, Illinois) connected to a continuous wall suction unit. The second group underwent standard tonsillectomy with an electrosurgical pencil without surgical plume evacuation. The surgical technique used by the senior author for tonsillectomy was subcapsular dissection, defined as en bloc removal of the palatine tonsil with its capsule. Procedures were performed by the senior author or a junior otolaryngology resident who had already performed at least 50 tonsillectomies. There was no difficulty visualizing the surgical field when suction was not used, likely because surgical times were short and brief intermissions were used. EC time did not include any time when the cautery was off. Hemostasis was achieved with a suction coagulator (Valleylab Suction Coagulator; Covidien). EC settings were adjusted accordingly to either 12 W or 20 W for tonsillectomy and suction coagulator at 20 W for surgical hemostasis. This resulted in a total of 4 patient groups based on EC settings and SES deployment. The number of pediatric tonsillectomies per day ranged from 2 to 4 during the study period. All cases per day were conducted in the same operating room with a turnover time of up to 1.5 hours between cases. For all cases, the same EC unit, setting, and SES method were employed to prevent an additional effect of particulate concentration from prior cases with another EC setting. Other factors, including patient age, operative indication, palatine tonsil size, and total EC time, were not controlled between groups.
Ethics Statement
This study was evaluated by the West Virginia University Institutional Review Board and deemed to be non–human subject research.
Exposure Sampling
During tonsillectomy, a portable measuring device was worn by the operating surgeon (Diffusion Size Classifier miniature DiSCmini v1.0; Matter Aerosol AG, Wohlen, Switzerland) to measure airborne particle particle concentration (particles/cm3), with a measurable size range of 20 nm to 300 nm for every second. The inlet of the device was positioned in the breathing zone, adjacent to but outside of the mask. This was employed in every case during the entire case. The same instrument was used for all sampling. No samples were taken between cases, although prior to sample collection, background concentrations were measured in an empty operating room each day. During electrosurgical pencil utilization, the start and end times of tonsillectomy were recorded for each case. Airborne particle concentrations for tonsillectomy only were compared as adenoidectomy was performed under the same conditions (ie, no difference in SES or EC setting).
Statistical Analysis
After adjusting particle number concentration by subtracting background concentration, statistical analysis was performed to determine the effect of EC setting. One-way analysis of variance (ANOVA) was conducted using SAS software (SAS System Version 9.4; SAS Institute, Cary, North Carolina) to compare particle number concentrations among different smoke evacuation systems and EC settings. Prior to conducting ANOVA, all concentrations were log-transformed due to the failure of normality test using Kolmogorov-Smirnov, and multiple pairwise comparison was used using the Tukey method. A P value of .05 was used to detect a statistical difference between groups. In addition, Pearson correlation coefficients were calculated to determine the relationship between particle number concentration and EC time.
Results
Thirty-six patients undergoing tonsillectomy were assigned to the 4 study groups: 9 cases with EC at 12 W and SES (12SES), 9 cases with EC at 20 W and SES (20SES), 9 cases with EC at 12 W without SES (12NS), and 9 cases with EC at 20 W without SES (20NS). As shown in Table 1, the mean (coefficient of variation) particle number concentration was 1661 (1.2) particles/cm3, 5515 (1.1) particles/cm3, 8208 (0.5) particles/cm3, and 78,506 (1.1) particles/cm3 for 12SES, 20SES, 12NS, and 20NS, respectively. Overall, the NS groups generated considerably higher particle number concentration compared to the SES groups (Figure 1). The particle number concentrations among 4 groups revealed a statistically significant difference (P < .0001); each group was compared pairwise with each of the other groups, and all comparisons showed statistically significant differences (Table 1).
Table 1.
Surgical Case Summary: Particle Number Concentration for Total.
| Smoke Evacuation System | EC Setting, W | No. of Cases | EC Time Range (Mean), min | Particle Number Concentration, Particles/cm3 | Pearson Correlation Coefficientb | P Value from ANOVA Testc | |
|---|---|---|---|---|---|---|---|
| Rangea | Mean (CV) | ||||||
| SES | 12 | 9 | 3.0–7.0 (4.9) | 40–5458 | 1661 (1.2) | 0.313 | <.0001 |
| 20 | 9 | 2.0–5.5 (3.6) | 461–17,657 | 5515 (1.1) | −0.564 | ||
| NS | 12 | 9 | 4.0–11 (8.4) | 4612–15,717 | 8208 (0.5) | −0.075 | |
| 20 | 9 | 1.9–10 (4.5) | 7391–262,107 | 78,506 (1.1) | −0.372 | ||
Abbreviations: ANOVA, analysis of variance; CV, coefficient of variation (standard deviation divided by mean); EC, electrocautery; NS, no smoke evacuation system; SES, smoke evacuation system.
Particle number concentration is the average of each individual case.
Between particle number concentration and electrocautery time for each group.
Comparison of particle number concentrations among the 4 groups.
Figure 1.
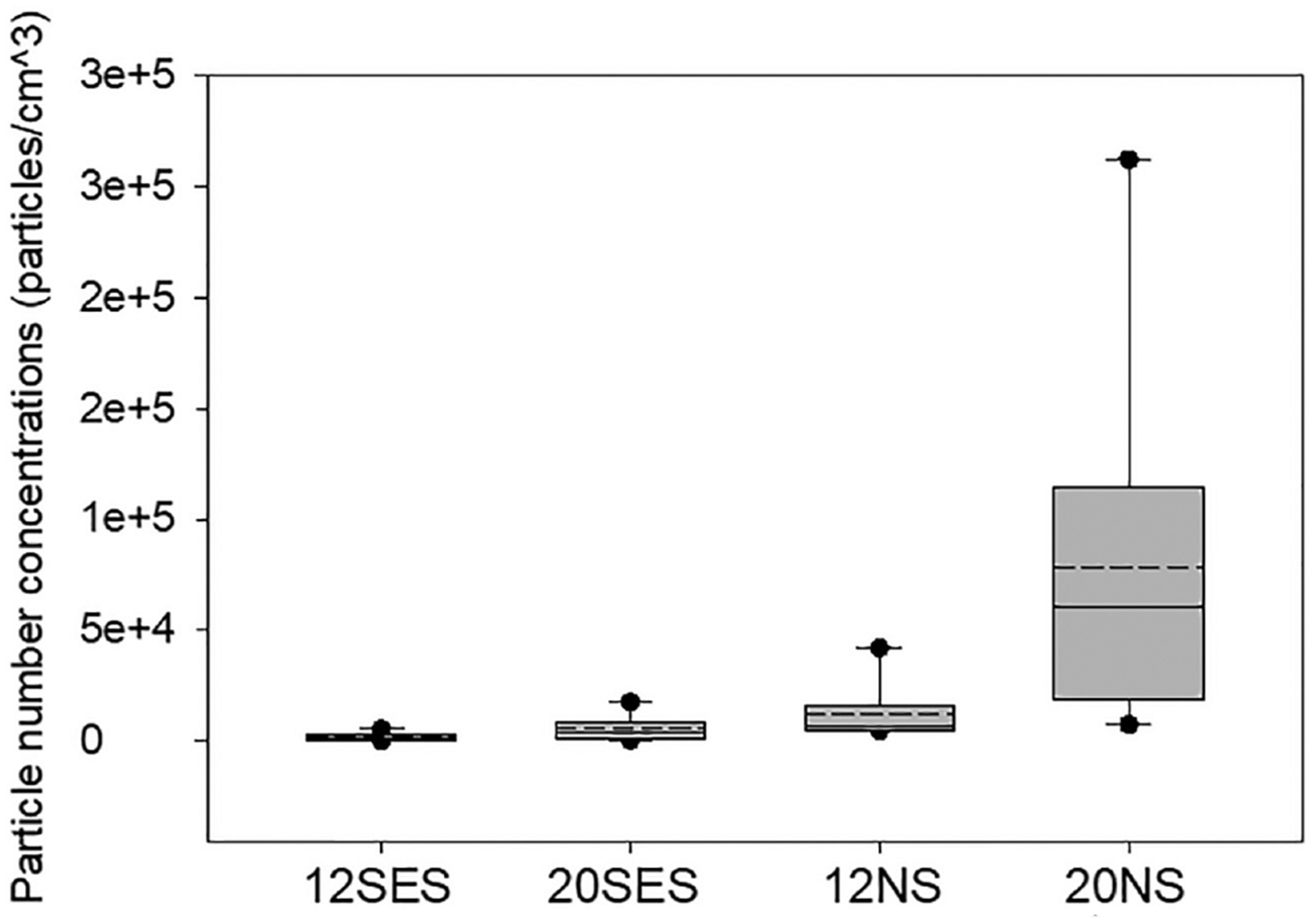
Particle number concentration (particles/cm3) in the breathing zone. Each box plot represents the 10th, 25th, 50th, 75th, and 90th percentiles. Solid circles indicate 5th (lower) and 95th (upper) percentiles. Dashed line defines mean.
The average duration of EC was similar for 12SES, 20SES, and 20NS, whereas 12NS was found to have a longer EC time than the other groups. However, no strong positive correlation between particle number concentration and EC time was observed for each group (Table 1); only 12SES showed a moderate correlation (Pearson correlation coefficient = 0.313), while others showed negative correlations.
Figure 2 depicts the maximum particle concentration of individual cases, which reveals 20NS generated noticeably higher particle concentration compared to other groups for total tonsillectomy. The maximum particle concentrations ranged from 823 to 216,195 particles/cm3 for 12SES, from 1875 to 425,198 particles/cm3 for 20SES, from 86,940 to 799,796 particles/cm3 for 12NS, and from 124,026 to 4,942,961 particles/cm3 for 20NS.
Figure 2.
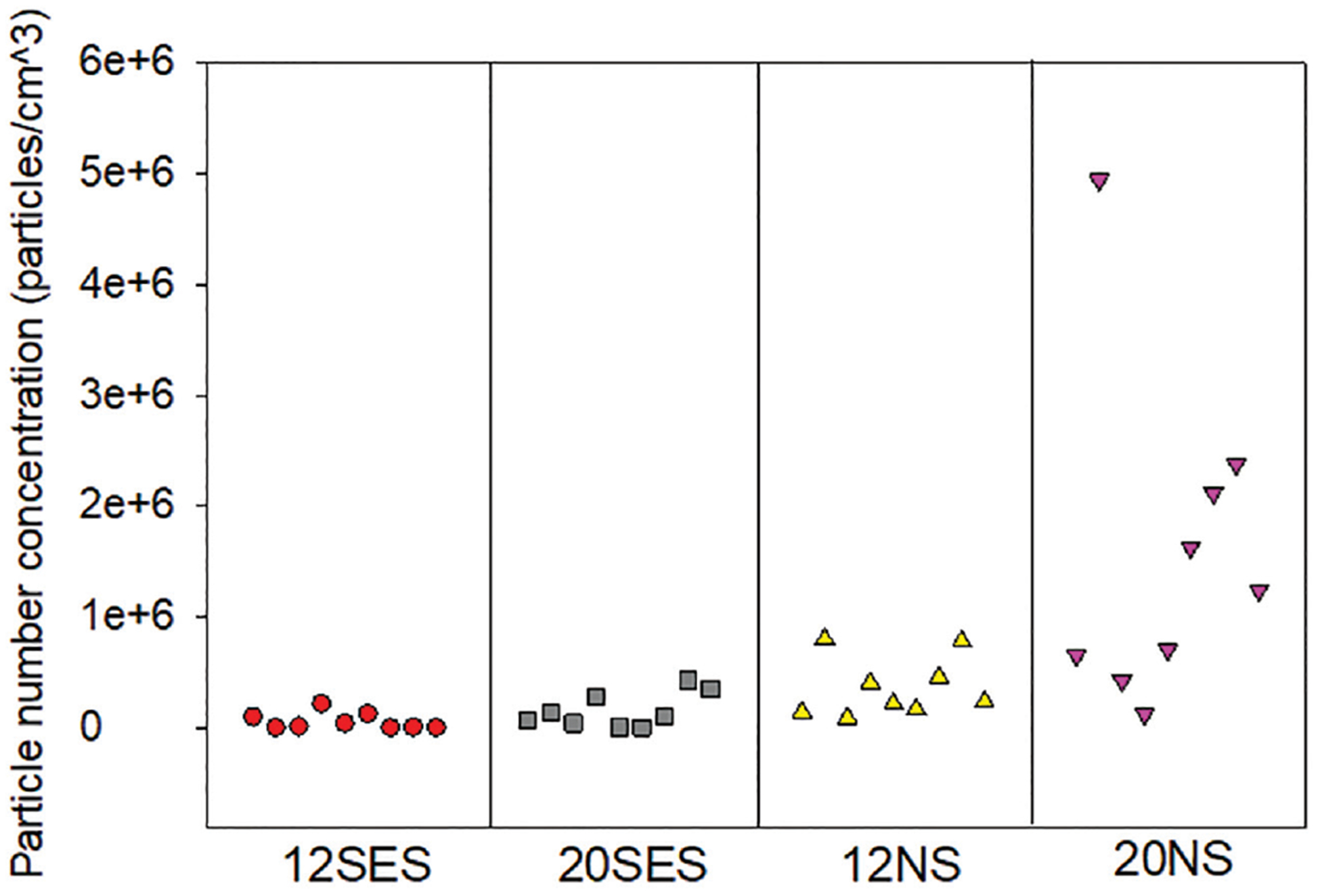
Maximum particle concentration (particles/cm3) during total tonsillectomy, by surgical case.
Discussion
Surgical Plume Particulates
To date, the nature of ultra-fine particles generated in surgical plume remains largely unexplored. At the time of EC activation, a cloud of ultra-fine particles may be observed, after which particulate volume falls to a lower background level.18 Establishing liberated particle quantity and size is important since traditional surgical masks are known to provide ineffective protection against fine or ultra-fine particles.19 At this time, only a handful of studies have previously examined particle size from EC. Compared to laser technology and ultrasonic tissue ablation, EC produces surgical plume with the smallest particulate size.8 Bruske-Hohlfeld and colleagues18 examined particles collected during 5 different types of general surgery procedures (adhesion lysis with tumor removal, biliodigestive anastomosis, hemihepatectomy, laparoscopic appendectomy, and mesh hernia repair). Particle size for these operations ranged from 10 nm to 1 μm with a short period of very high exposure to ultra-fine particles (>100,000 particles/cm3) for surgeons and surgical assistants. When specifically evaluating general surgery procedures similar to tonsillectomy in terms of duration, adhesion lysis with tumor removal (operative time, 73 minutes) resulted in a mean particle concentration of 3320 particles/cm3, whereas laparoscopic appendectomy (operative time, 88 minutes) with filter system deployment reduced mean and peak particle concentrations drastically to 74 particles/cm3 and 379 particles/cm3, respectively. In this study, mean particle concentration in the breathing zone during total tonsillectomy was 1661 particles/cm3 for 12SES, 5515 particles/cm3 for 20SES, 8208 particles/cm3 for 12NS, and 78,506 particles/cm3 for 20NS. Airborne particle concentrations were over 9.5 times higher when EC was set at 20 W vs 12 W during total tonsillectomy, which was mitigated to 3.3 times with SES. In addition, these findings reveal that the particle number concentration was not positively correlated with the duration of EC. It is important to note that laparoscopic surgery occurs in a closed abdominal cavity, with lower reported mean particle concentrations compared to open procedures occurring in the oral cavity and oropharynx. Further clinical studies are necessary to determine if ongoing exposure to EC particles, especially in the oropharynx, leads to adverse respiratory events.
Smoke Evacuation Systems
A SES is essentially a vacuum pump with 1 or more filters removing particles from surgical plume. The most important factor in surgical plume capture is the vortex, which requires both high flow and intake velocity to draw air into the device nozzle through the hose and evacuator where captured material passes through an air filter. High-efficiency particulate air filters are essential in surgical plume evacuation since they have a 99.97% efficiency in capturing particles of >0.3 μm in size.20 Two studies have previously examined surgical plume evacuation techniques and found SES deployment leads to a reduction in surgical plume concentration or volume. Pillinger and colleagues21 conducted a randomized controlled clinical trial (n = 30) in 2003 to investigate the amount of surgical plume reaching the surgeon’s mask during thyroidectomy or parathyroidectomy. In their study, EC was set to 30 W for both groups, the SES was placed at the level of the EC pencil, and released particles were measured at the level of the operator’s mask. The mean amount of surgical plume released was 0.137 mg/m3 without SES and 0.012 mg/m3 with SES (P < .001). The maximum amount of surgical plume detected was 2.411 mg/m3 without SES and 0.255 mg/m3 with SES, respectively (P < .001). There was not a significant difference in terms of incision time to division of anterior cervical strap musculature, background particles, and endocrine gland weight between groups.21 In addition, Bruske-Hohlfeld et al18 described that in the presence of a very efficient SES, the increment and decrement of ultra-fine particles occur within a matter of seconds, which is critical in mitigating total exposure to potentially toxic agents. The present study also showed a significant difference when particle number concentrations were compared with and without SES; the particle number concentration was 4.9 times and 14.2 times higher without SES compared to those with SES for EC setting at 12 W and 20 W, respectively.
Room Ventilation
The performance of room ventilation systems has been widely studied to highlight suitability and assess effects on parameters related to airborne contaminant control (adopted filtration stages, air humidity, air pressurization, air temperature, airflow pattern, airflow rate, frequency of door opening, and number of surgical personnel).22 Several techniques have been described for surgical plume evacuation via room ventilation: vertical or horizontal unidirectional airflow as well as upward displacement or mixing systems. In a clinical work by Romano and colleagues22 evaluating surgical plume evacuation during liver resection at the level of the surgeon, a hybrid operating room equipped with an upward displacement airflow ventilation system had ultra-fine particle concentrations 13 times higher than an operating room with a unidirectional downward airflow ventilation system. Thus, the unidirectional downward airflow system, with its large airflow volume and well-defined airflow pattern, evacuates surgical plume in critical areas quickly and efficiently with a short recovery time compared to upward displacement airflow ventilation systems. How this might apply to tonsillectomy is unknown.
Limitations
Limitations of this study include the small sample size and the variation in time taken for each tonsillectomy. Indication for surgery was not considered in this study; there is the possibility that chronically infected tonsils may be different with regard to the procedure or emitted surgical plume. Pediatric tonsillectomy is a very short surgery taking place in a confined space, so generalizability to other head and neck procedures may be limited.
Understanding the potential risks of surgical plume exposure remains a top priority to optimize the health and safety of surgeons, operating room staff, and patients in hospitals nationwide. Reflecting the growing body of evidence on the potential hazards of surgical plume, strong leadership in the implementation of practice guidelines and education modules for operating room staff is necessary to address these concerns.23
Conclusions
Surgeons, operating room staff, and patients should be aware of the harmful risks associated with surgical plume. Risks from direct exposure are cumulative in nature and greatest for operating room personnel closest to the point of electrosurgical smoke production. Systematic steps should be taken to reduce exposure to aerosolized toxic compounds generated during procedures requiring powered instrumentation; lower EC settings and SES deployment appear to effectively minimize the extent of potentially hazardous agents released during pediatric total tonsillectomy. Future research efforts are necessary to investigate the long-term impact of surgical plume exposure among operating room personnel and delineate a link, if one exists, between electrosurgical smoke and adverse health outcomes.
Acknowledgments
Funding source: National Institute for Occupational Safety and Health (927ZLEN). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC). Mention of any corporation or product does not constitute an endorsement by CDC/NIOSH.
Footnotes
Competing interests: None.
Sponsorships: None.
References
- 1.Hall MJ, Schwartzman A, Zhang J, Liu X. Ambulatory surgery data from hospitals and ambulatory surgery centers: United States, 2010. Natl Health Stat Report. 2017;(102):1–15. [PubMed] [Google Scholar]
- 2.Patel HH, Straight CE, Lehman EB, Car MM. Indications for tonsillectomy: a 10 year retrospective review. Int J Pediatr Otorhinolaryngol. 2014;78(12):2151–2155. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell RB, Archer SM, Ishman SL, et al. Clinical practice guideline: tonsillectomy in children (update)—executive summary. Otolaryngol Head Neck Surg. 2019;160(2):187–205. [DOI] [PubMed] [Google Scholar]
- 4.Walner DL, Mularczyk C, Sweis A. Utilization and trends in surgical instrument use in pediatric adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2017;100:8–13. [DOI] [PubMed] [Google Scholar]
- 5.Alp E, Bijl D, Bleichrodt RP, Hansson B, Voss A. Surgical smoke and infection control. J Hosp Infect. 2006;62:1–5. [DOI] [PubMed] [Google Scholar]
- 6.González-Bayón L, González-Moreno S, Ortega-Pérez G. Safety considerations for operating room personnel during hyperthermic intraoperative intraperitoneal chemotherapy per-fusion. Eur J Surg Oncol. 2006;32(6):619–624. [DOI] [PubMed] [Google Scholar]
- 7.Taravella MJ, Viego J, Luiszer F, et al. Respirable particles in the excimer laser plume. J Cataract Refract Surg. 2001;27: 604–607. [DOI] [PubMed] [Google Scholar]
- 8.Barrett WL, Garber SM. Surgical smoke: a review of the literature. Surg Endosc. 2003;17:979–987. [DOI] [PubMed] [Google Scholar]
- 9.Tomita Y, Mihashi S, Nagata K, et al. Mutagenicity of smoke condensates induced by CO2-laser irradiation and electrocauterization. Mutat Res. 1981;89:145–149. [PubMed] [Google Scholar]
- 10.Sawchuck WS, Weber PJ, Lowy DR, Dzubow LM. Infectious papillomavirus in the vapor of warts treated with carbon dioxide laser or electrocoagulation: detection and protection. J Am Acad Dermatol. 1981;21:41–49. [DOI] [PubMed] [Google Scholar]
- 11.Freitag L, Chapman GA, Sielczak M, Ahmed A, Russin D. Laser smoke effect on the bronchial system. Lasers Surg Med. 1987;7:283–288. [DOI] [PubMed] [Google Scholar]
- 12.Gatti J, Bryant CJ, Noone RB, Murphy JB. The mutagenicity of electrocautery smoke. Plastic Reconstr Surg. 1992;89:781–784. [PubMed] [Google Scholar]
- 13.Lee T, Soo JC, Lebouf RF, et al. Surgical smoke control with local exhaust ventilation: experimental study. J Occup Environ Hyg. 2018;15(4):341–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calder JS, Emerson DJ, Murray-Wilson A. Smoke evacuation during surgery. Ann R Coll Surg Engl. 1992;74(5):370. [PMC free article] [PubMed] [Google Scholar]
- 15.Dobrogowski M, Wesołowski W, Kucharska M, Sapota A, Pomorski LS. Chemical composition of surgical smoke formed in the abdominal cavity during laparoscopic cholecystectomy—assessment of the risk to the patient. Int J Occup Med Environ Health. 2014;27(2):314–325. [DOI] [PubMed] [Google Scholar]
- 16.Tseng HS, Liu SP, Uang SN, et al. Cancer risk of incremental exposure to polycyclic aromatic hydrocarbons in electrocautery smoke for mastectomy personnel. World J Surg Oncol. 2014;12:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weston R, Stephenson RN, Kutarski PW, Parr NJ. Chemical composition of gases surgeons are exposed to during endoscopic urological resections. Urology. 2009;74(5):1152–1154. [DOI] [PubMed] [Google Scholar]
- 18.Bruske-Hohlfeld I, Preissler G, Jauch K, et al. Surgical smoke and ultrafine particles. J Occup Med Toxocol. 2008;3:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oberg T, Brosseau LM. Surgical mask filter and fit performance. Am J Infect Control. 2008;36(4):276–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wenig BL, Stenson KM, Wenig BM, Tracey D. Effects of plume produced by the Nd:YAG laser and electrocautery on the respiratory system. Lasers Surg Med. 1993;13(2):242–245. [DOI] [PubMed] [Google Scholar]
- 21.Pillinger SH, Delbridge L, Lewis DR. Randomized clinical trial of suction versus standard clearance of the diathermy plume. Br J Surg. 2003;90(9):1068–1071. [DOI] [PubMed] [Google Scholar]
- 22.Romano F, Gusten J, DeAntonellis S, Joppolo CM. Electrosurgical smoke: ultrafine particle measurements and work environment quality in different operating theatres. Int J Environ Res Public Health. 2017;14(2):E137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.AORN. Guideline summary: surgical smoke safety. AORN. 2017;105(5):498–500. [DOI] [PubMed] [Google Scholar]


