Abstract
Introduction
Ankle sprains are one of the most common athletic injuries. If a patient fails to improve through conservative management, surgery is an option to restore ankle stability. The purpose of this study was to analyze and assess the variability across different rehabilitation protocols for patients undergoing either lateral ankle ligament repair, reconstruction, and suture tape augmentation.
Methods
Using a web-based search for published rehabilitation protocols after lateral ankle ligament repair, reconstruction, and suture tape augmentation, a total of 26 protocols were found. Inclusion criteria were protocols for post-operative care after an ankle ligament surgery (repair, reconstruction, or suture tape augmentation). Protocols for multi-ligament surgeries and non-operative care were excluded. A scoring rubric was created to analyze different inclusion, exclusion, and timing of protocols such as weight-bearing, range of motion (ROM), immobilization with brace, single leg exercises, return to running, and return to sport (RTS). Protocols inclusion of different recommendations was recorded along with the time frame that activities were suggested in each protocol.
Results
Twenty-six protocols were analyzed. There was variability across rehabilitation protocols for lateral ankle ligament operative patients especially in the type of immobilizing brace, time to partial and full weigh bearing, time to plantar flexion, dorsiflexion, eversion and inversion movements of the ankle, and return to single leg exercise and running. For repair and reconstruction, none of these categories had greater than 60% agreement between protocols. All (12/12) repair, internal brace, and unspecified protocols and 86% (12/14) of reconstruction protocols recommended no ROM immediately postoperatively. Eighty-six percent (6/7) of repair and 78% (11/14) of reconstruction protocols recommended no weight-bearing immediately after surgery, making post-operative ROM and weight-bearing status the most consistent aspects across protocols. Five protocols allowed post-operative weight-bearing in a cast to keep ROM restricted. Sixty-six percent (2/3) of suture tape augmentation protocols allowed full weight-bearing immediately post-operatively. Suture tape augmentation protocols generally allowed rehabilitation to occur on a quicker time-line with full weight-bearing by week 4–6 in 100% (3/3) of protocols and full ROM by week 8–10 in 66% (2/3) protocols. RTS was consistent in repair protocols (100% at week 12–16) but varied more in reconstruction.
Conclusion
There is significant variability in the post-operative protocols after surgery for ankle instability. ROM was highly variable across protocols and did not always match-up with supporting literature for early mobilization of the ankle. Return to sport was most likely to correlate between protocols and the literature. Weight-bearing was consistent between most protocols but requires further research to determine the best practice. Overall, the variability between programs demonstrated the need for standardization of rehabilitation protocols.
Keywords: ankle joints, reconstructive surgical procedure, rehabilitation, immobilization, return to sport
INTRODUCTION
Ankle sprains are one of the most common athletic injuries making up approximately 20–40% of sports related injuries in the United States.1 While many recover through non-operative rehabilitation techniques such as initial immobilization with bracing and casting and strengthening exercises.2 Conservative treatment also consists of physical therapy to work on proprioception and strength deficits that patient may have had leading to instability. However, some patients will continue to experience functional instability and recurrent sprains after conservative management.3 Thus, if functional or mechanical instability remains, surgery should be considered, although patients should attempt conservative, non-operative treatment for instability for at least three months before considering surgery.1,4
There are multiple different operative options to restore the stability of the lateral ankle ligaments. The first line treatment is generally a direct anatomic repair procedure which is the use of native ligament remnants of the anterior talofibular ligament and, if needed, the calcaneofibular ligament.3,4 Overall, there is a very high success rate associated with this surgery. In studies looking at long term success rates of ligament repair, greater than 90% of patients had successful outcomes and mean functional ankle scores were reported to be above 90% in all studies.4–10 Anatomic reconstruction is another operative option for chronic ankle instability, using either allografts or autografted ligaments to repair the unstable lateral ankle. Reconstruction with both allografts and autografts has been shown to have good to excellent short-term outcomes, but autografts have the disadvantage of donor site morbidity.4 A suture tape augmentation procedure is a version of ligament repair using suture tape to reinforce ligament strength and acts as a secondary stabilizer for the ankle.11 This procedure provides the extra stability to the ankle with the advantages of anatomic ligament repair and without the donor site morbidity.12 The outcomes of these surgeries depend on the ligament quality and patient characteristics, and specific indications for one surgery over another is an area of ongoing research.1,4
A few ankle rehabilitation recommendations have been researched but not put together in a standardized protocol. Pearce et al.13 reviewed rehabilitation of the ankle and concluded that there was a lack of studies comparing rehabilitation protocols which lead largely only to use of level 5 evidence when it comes to rehabilitation of these injuries. No specific rehabilitation guidelines for these ankle instability surgeries has been established in the United States. The purpose of this paper was to determine the variability between protocols after lateral ligament repair, reconstruction, and suture tape augmentation surgeries used to treat ankle instability and to evaluate the need for standardization in rehab protocols.
METHODS
All publicly available rehabilitation protocols from U.S. orthopedic academic programs were collected by a systematic search using the FREIDA (Fellowship and Residency Electronic Interactive Database) list of all academic programs. The availability of a protocol for lateral ankle repair from an institution was screened by a Google search for “[Program Name] lateral ankle repair rehab protocol”. Similarly, protocols for lateral ankle reconstructions were found by “[Program Name] lateral ankle reconstruction rehab protocol”. Suture tape augmentation protocols were found both by “[Program Name] Lateral Ankle Suture Tape Augmentation rehab protocol” and by “[Program Name] Internal brace rehab protocol”. Private practice protocols also were included, which were found either during the academic protocol search or through a general Google search for “lateral ankle repair rehab protocol”, “lateral ankle reconstruction protocol”, “suture tape augmentation ankle rehab protocol”, and “ankle internal brace rehab protocol”.
The search was done in June 2019. Because this was a review of publicly published protocols, an Institutional Review Board (IRB) approval was not needed. Protocols were included if they were rehabilitation protocols for post-operative care of the unstable ankle that were meant for the physical rehabilitation of the ankle. Non-operative protocols were excluded from this study. Two duplicates were found, and one protocol was excluded due to being primarily over operative wound care and not ankle rehabilitation. Protocols that included both repair and reconstruction were placed in the reconstruction group. Each protocol included was assessed for inclusion, exclusion, and variability in timing of range of motion (ROM), weight-bearing, bracing, single leg exercises, return to running, RTS, and functional testing. More specifically for ROM, plantar flexion (PF), dorsiflexion (DF), and eversion and inversion times were recorded.
RESULTS
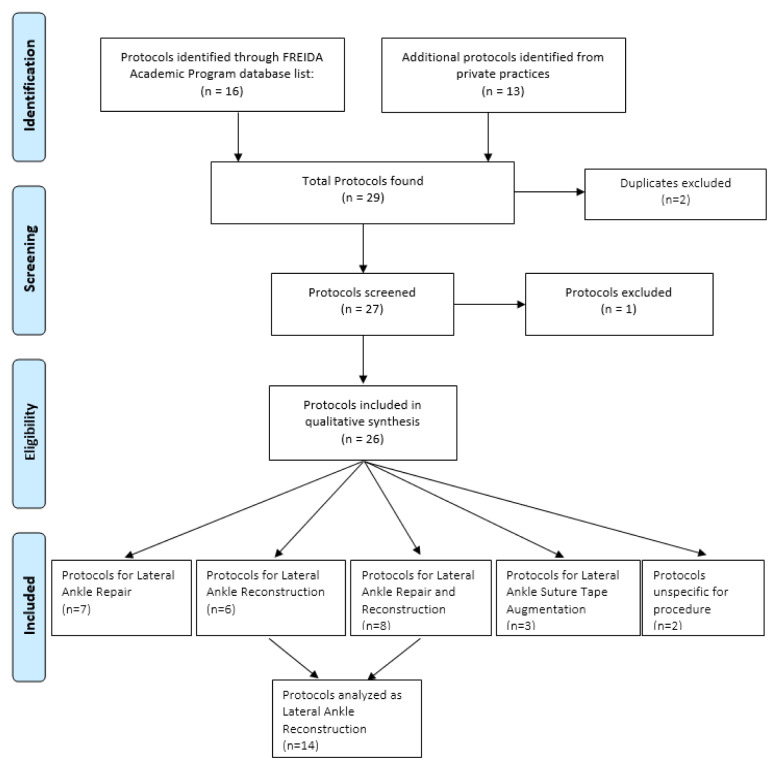
Twenty-six total protocols were found. Thirteen were from U.S. academic programs. A flow chart of the protocol selection process is shown in Figure 1. One of these programs had two published lateral ankle protocols for both repair/reconstruction and suture tape augmentation, both protocols were used in their respective categories. The other 13 protocols were from private practice clinics. Seven total protocols were for lateral ankle ligament repair. Fourteen protocols either specifically were for lateral ankle reconstruction or included it as part of their protocol (6 protocols for reconstruction only and 8 protocols including both repair and reconstruction, which were included with reconstruction results). Three protocols were found for suture tape augmentation/internal brace. Two protocols did not specify which lateral ankle procedure they were meant to follow, but did specify that it was meant for post-operative care. A table of protocols used in this study can be found in Table 1.
Figure 1.
Protocols were screened and selected through the FREIDA residency list database. Additional records were found from private practice organizations.
Table 1.
Different protocol institutions and which surgical category the protocol fell under.
| U.S. academic institution | Private practice | |
|---|---|---|
| Repair | Brigham and Women’s Connecticut Children’s |
Toronto Western American Health Network Southern California Orthopedic Institute The Stone Clinic Sanford Orthopedic Sports Medicine |
| Reconstruction | Loma Linda | Minnesota Orthopedic Sports Medicine Institute SOS med BC Foot & Ankle Clinic Mountain Orthopedics Dr. Anand Vora |
| Repair and reconstruction | NYU Ohio State University UW Health Sports Rehabilitation UNC University of Kansas William Beaumont Army Medical |
Brian Waterman M.D. Orthopedic Surgery Chesapeake Orthopedic & Sports Medicine Center |
| Suture tape augmentation | University of Kansas | Minnesota Orthopedic Sports Medicine Institute Twin Cities Orthopedics |
| Unspecified | NC State Sports Medicine Tripler Army Medical Center |
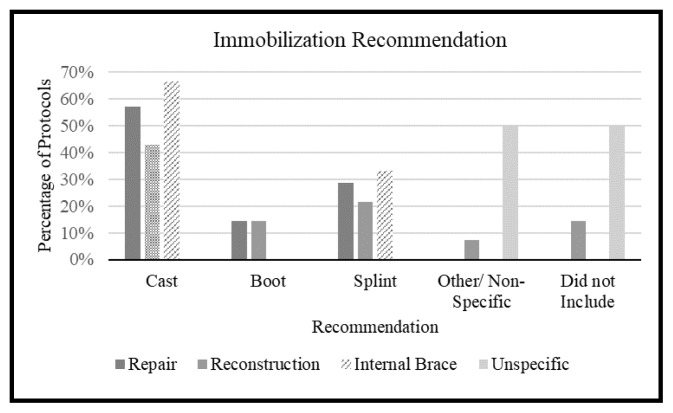
Immobilization
A total of 88.5% (23/26) of protocols mentioned immobilization by bracing the ankle after operating (Figure 2). A total of 42.8% (3/7) of repair protocols, 42.8% (6/14) of the reconstruction protocols, and 66% (2/3) of the suture tape augmentation protocols used a cast. Of the unspecified protocols, 50% (1/2) used an unspecific brace and 50% (1/2) did not mention bracing.
Figure 2.
Postoperative bracing recommendations were included in 23 of 26 protocols.
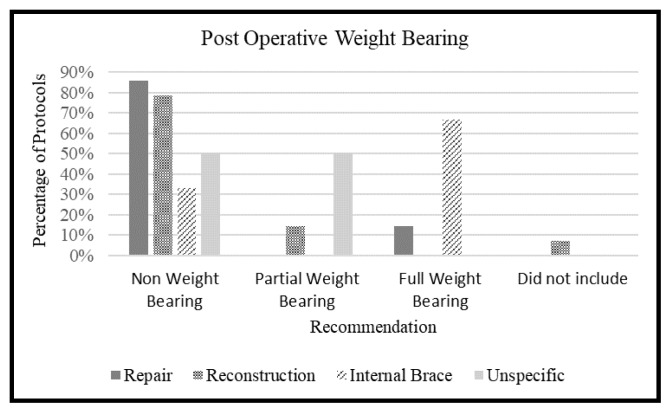
Weight-bearing Recommendations
A total of 96.1% (25/26) of protocols included a weight-bearing status after surgery (Figure 3). A total of 85.7% (6/7) of repair protocols and 78.6% (11/14) of reconstruction protocols recommended no weight-bearing after surgery. Sixty-six percent (2/3) of internal brace protocols allowed full weight-bearing. In the unspecified protocols, 50% (1/2) recommended no weight-bearing and 50% (1/2) partial weight-bearing.
Figure 3.
Post-operative weight-bearing recommendations were included in 25 of the 26 total protocols.
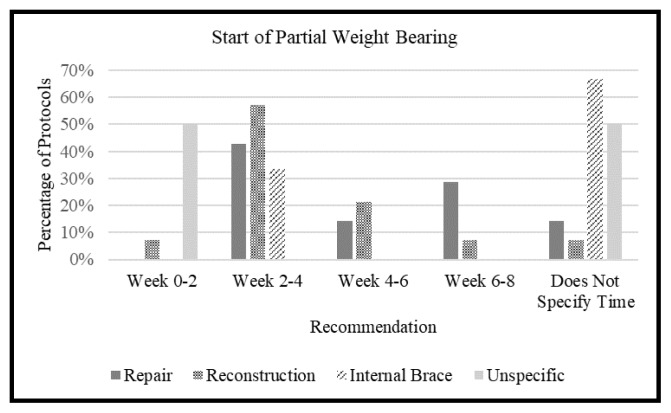
A total of 80.7% (21/26) of protocols included a recommendation for partial weight-bearing (Figure 4). A total of 42.8% (3/7) repair protocols and 57% (8/14) reconstruction protocols recommended week 2 to 4. Sixty-six percent (2/3) of the suture tape augmentation protocols did not specify time until partial weight-bearing. Of the unspecified protocols, 50% (1/2) said week 0 to 2 and 50% (1/2) did not specify.
Figure 4.
Time of returning to partial weight-bearing were included in 21 of 26 protocols.
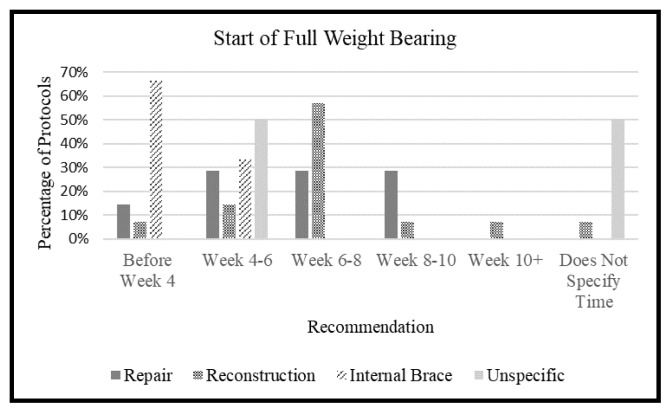
A total of 92.3% (24/26) of protocols included a goal time for full weight-bearing (Figure 5). There was not a majority recommendation in protocols for repair, 28.6% (2/7) said week 4 to 6, 28.6% (2/7) said week 6 to 8, and 28.6% (2/7) said week 8 to 10. A total of 57.1% (8/14) of reconstruction protocols said week 6 to 8. Sixty-six percent (2/3) of the suture tape augmentation protocols said before week 4. Of the unspecified protocols, 50% (1/2) said week 4–6 and 50% (1/2) did not specify.
Figure 5.
Time of returning to full weight-bearing status were included in 24 of 26 protocols.
Range of Motion (ROM)
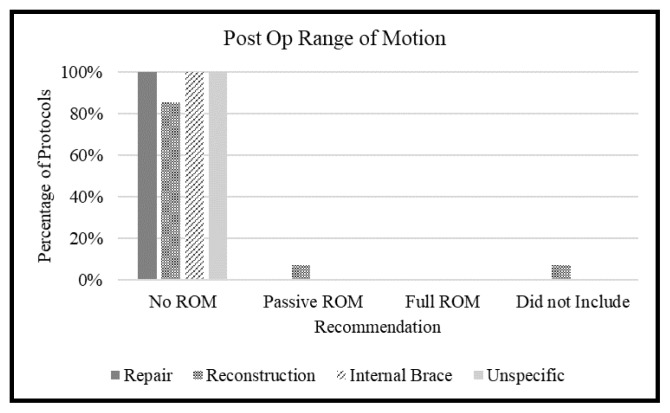
A total of 96.1% (25/26) of protocols specified ROM after surgery (Figure 6). All (7/7) repair protocols, 85.7% (12/14) of reconstruction protocols, all (3/3) suture tape augmentation protocols, and all (2/2) of the unspecific protocols allowed no ROM.
Figure 6.
Postoperative Range of Motion guidelines were included in 25 of the 26 protocols.
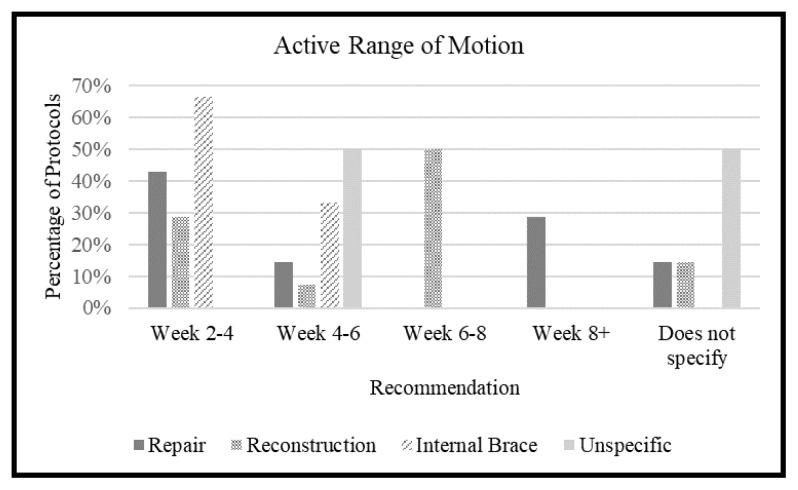
Passive ROM (PROM) was only specifically included in 5 out of the 26 protocols, therefore, no graph was included. PROM recommendations ranged from week 0 to week 4. Active ROM (AROM) was included in 22 out of the 26 protocols (84.6%; Figure 7). A total of 42.8% (3/7) of the repair protocols and 66% (2/3) of the suture augmentation protocols included AROM at week 2 to 4. Half (7/14) of the reconstruction protocols allowed AROM at week 6 to 8. A total of 66% (2/3) of the suture tape augmentation protocols included AROM at week 2 to 4. Of the unspecified protocols, 50% (1/2) included AROM at week 4 to 6 while the other 50% (1/2) did not specify.
Figure 7.
Active ROM recommendations were included in 22 of 26 protocols.
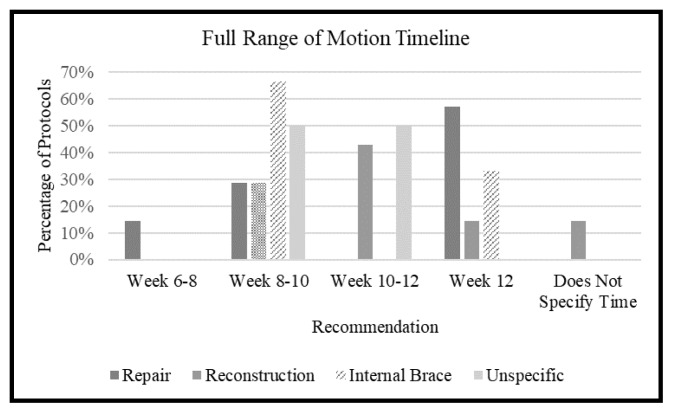
A total of 92.3% (24/26) of protocols included a full ROM time-line (Figure 8). A total of 57.1% of the repair protocols said week 12+, 42.8% (6/14) of the reconstruction protocols said week 10 to 12, and 66% (2/3) of the suture tape augmentation protocols said week 8 to 10. For the unspecific protocols, 50% (1/2) said week 8 to 10 and 50% (1/2) said week 10–12.
Figure 8.
Full ROM recommendations were included in 24 of 26 protocols.
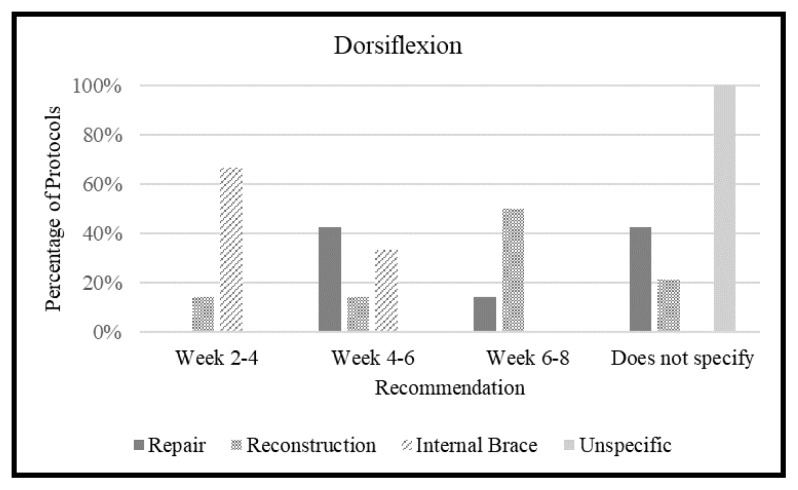
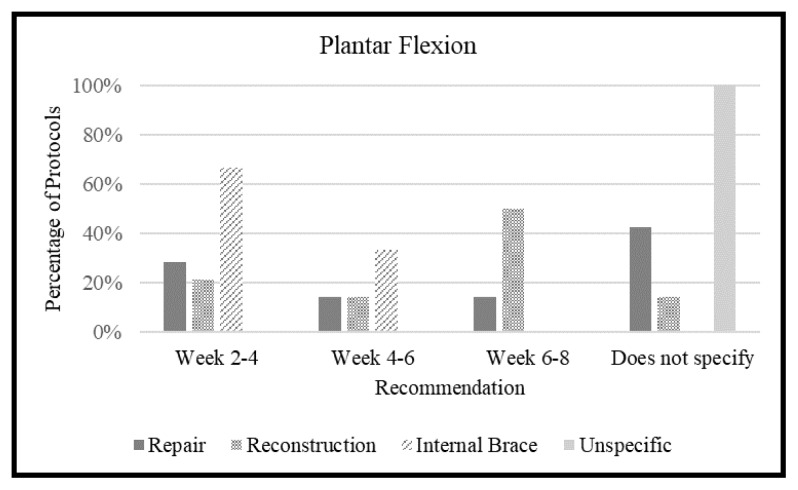
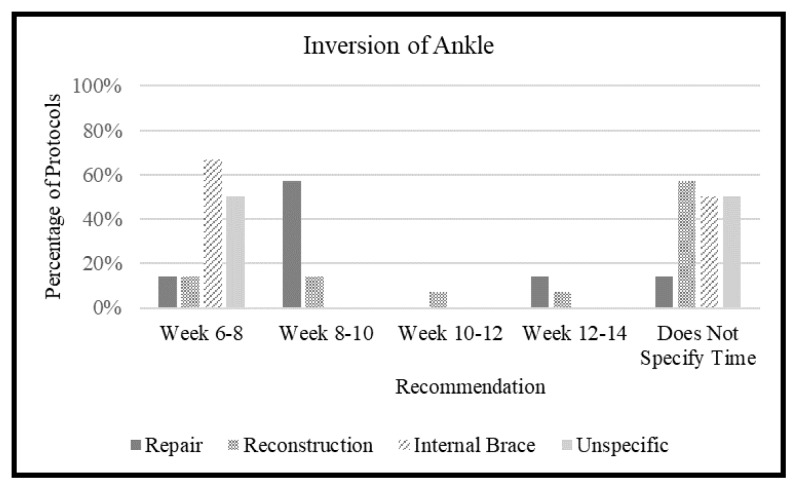
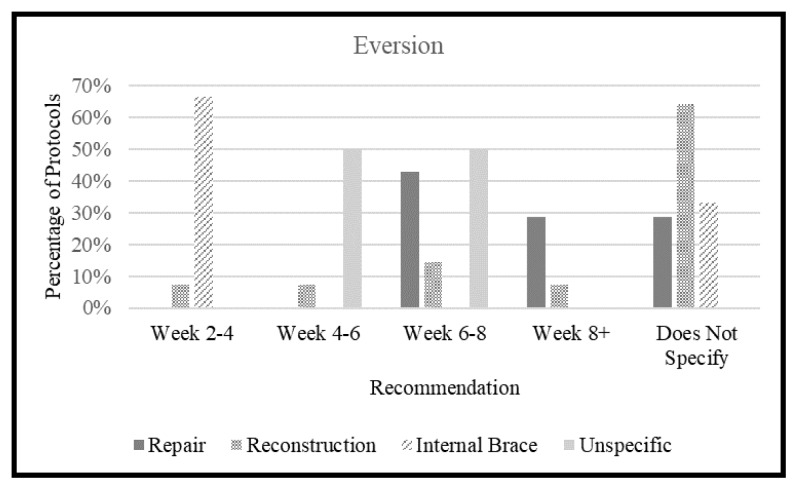
Various aspects of ROM were more specifically looked at, including dorsiflexion, plantar flexion, inversion, and eversion. The results are shown below and in Figures 9, 10, 11, and 12.
Figure 9.
Time when dorsiflexion of the ankle was allowed after surgery were included in 18 of the 26 protocols.
Figure 10.
Time when plantar flexion was allowed after surgery were included in 19 of the 26 protocols.
Figure 11.
Time when inversion of the ankle was allowed after surgery were included in 13 of 26 protocols.
Figure 12.
Time when eversion was allowed after surgery were included in 14 of the 26 protocols.
A total of 69.2% (18/26) of protocols included dorsiflexion (DF; Figure 9). A total of 42.8% (3/7) of the repair protocols allowed DF at week 4 to 6. Half (7/14) of the reconstruction protocols allowed DF at week 6 to 8. Sixty-six percent (2/3) of the suture tape augmentation protocols allowed DF at week 2 to 4. Neither of the unspecified protocols included DF.
A total of 73% (19/26) of protocols included plantar flexion (PF; Figure 10). For the repair protocols, 42.8% (3/7) did not specify, 50% (7/14) of the reconstruction protocols allowed PF week 6 to 8, and 66% (2/3) of the suture tape augmentation protocols included PF at week 2 to 4. Both unspecific protocols did not include PF.
A total of 50% (13/26) of protocols included recommendations about inversion of the ankle (Figure 11). A total of 57.1% (4/7) of the repair protocols said week 8 to 10, 57% (8/14) of the reconstruction protocols did not specify, and 66% (2/3) of the suture tape augmentation protocols allowed inversion by week 8. Half (1/2) of the unspecified protocols said week 6 to 8 while the other protocol (50%, 1/2) did not specify.
A total of 53.8% (14/26) of protocols included eversion of the ankle (Figure 12). A total of 42.8% (3/7) of repair protocols included eversion at week 6 to 8, 64% (9/14) of reconstruction protocols did not include eversion, and 66% (2/3) of the suture tape augmentation protocols included eversion at week 2 to 4. One unspecified protocol (50%, 1/2) included eversion at week 4 to 6 while the other (50%, 1/2) included eversion at week 6 to 8.
Exercise Recommendations
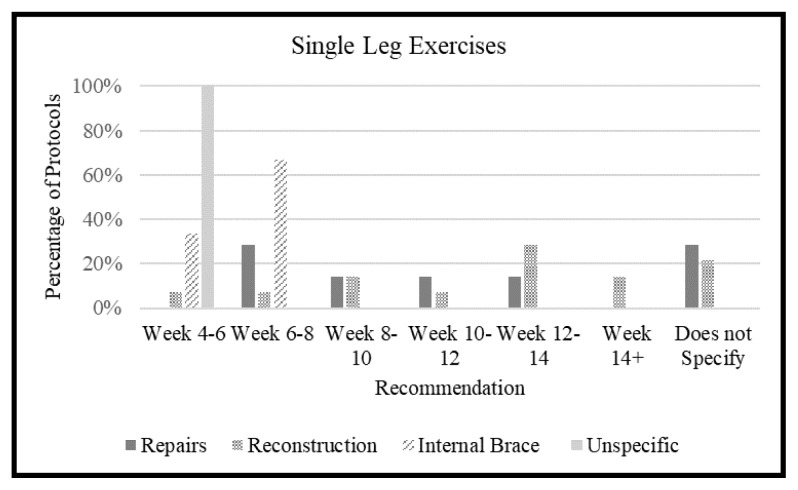
A total of 80.7% (21/26) of protocols included single leg exercises (Figure 13). A total of 28.5% (2/7) of the repair protocols said week 6 to 8 and 28.5% (2/7) did not specify. A total of 28.5% (4/14) of the reconstruction protocols said week 12 to 14 and 66% (2/3) of suture tape augmentation protocols said week 6 to 8. All (2/2) unspecified protocols said week 4 to 6.
Figure 13.
Time recommendation for single leg exercises to begin were included in 21 of 26 protocols.
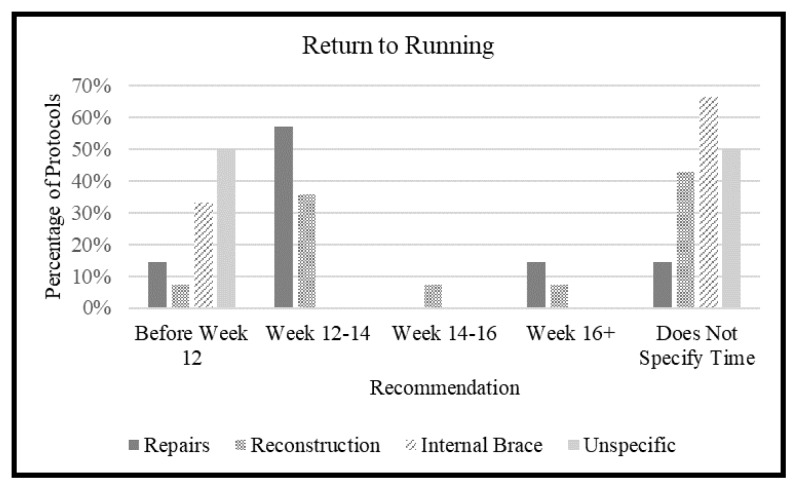
A total of 57.6% (15/26) of protocols included recommendations over returning to running (Figure 14). A total of 57% (4/7) of the repair protocols said week 12 to 14, 35.7% (5/14) of the reconstruction protocols said week 12 to 14, and 42.8% (6/14) did not specify. A total of 33% (1/3) of the suture tape augmentation protocols said before week 12 while the other 66% (2/3) did not specify. Half (1/2) of the unspecified protocols said before week 12 while the other half (1/2) did not specify.
Figure 14.
Time goals for beginning returning to running and running progressions were included in 15 of 26 protocols.
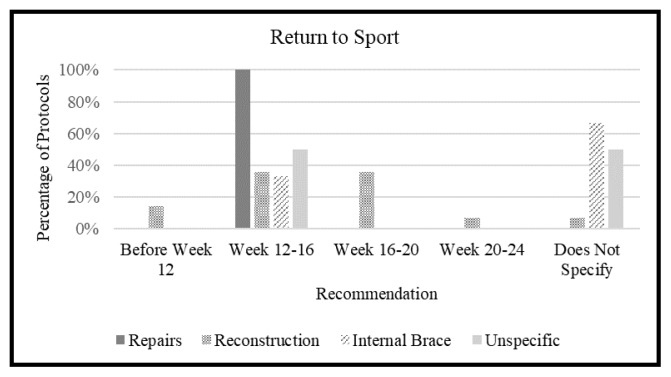
Return to Sport (RTS)
A total of 84.6% (22/24) of protocols included a RTS recommendation (Figure 15). Of the repair protocols, all (7/7) recommended week 12 to 16. For the reconstruction protocols, 35.7% (5/14) said week 12 to 16 and 35.7% (5/14) said week 16 to 20. For the suture tape augmentation protocols, 33% (1/3) said week 12 to 16 and 66% (2/3) did not specify. Fifty percent (1/2) of the unspecified protocols said week 12 to 16 and 50% (1/2) did not specify.
Figure 15.
RTS time recommended by protocols were included in 22 of the 26 protocols.
DISCUSSION
The results of this study indicated that there is considerable variability across different rehabilitation protocols for lateral ankle ligament operative patients especially with regards to immobilizing brace, time of partial and full weigh bearing, time to different ROM movements of the ankle, and return to single leg exercise and running. For repair and reconstruction, none of these categories had greater than 60% agreement of a time between protocols. The most consistent aspects of protocols were the postoperative restricted ROM and non-weight-bearing status. RTS was consistent in repair protocols but varied more in reconstruction. The variation in protocols shows a lack of standardization of care in rehabilitation procedures. Even though rehabilitation is an important part of the treatment process, there was no agreed upon protocol across different institutions on what should be done during the rehab phase.
The majority of protocols recommended no ROM14–36 and no weight-bearing14–18,20,23,24,26–37 immediately post-operatively. However, one reconstruction protocol37 allowed passive ROM immediately post-operatively, and five protocols allowed full weight-bearing immediately after surgery while immobilized.19,21,22,25,26 The majority of protocols used casts to immobilize post-operatively in all three types of surgery.14–16,20–22,25,26,29,32,33,36,38 Of the five that allowed weight-bearing right after surgery, four protocols21,22,26,38 used casts to immobilize and one protocol did not specify.19 Reconstruction protocols generally allowed partial weight-bearing earlier than repairs with 64% partial weight-bearing by week 4 in reconstruction but only 42.8% by week 4 after repair, but the majority for both procedures returned to full weight-bearing status by week 8.
In the current literature, not many studies have looked at immediate weight-bearing after surgery; however, those that have did not find any increase in wound complications.7,39 Although, there is little objective evidence to support whether early weight-bearing is beneficial to the patient.13 Karlson et al.40 found that most authors recommended 6 weeks of immobilization and weight-bearing after 2 to 3 weeks. A study by Pearce et al.13 outlined the European Ankle Instability groups guidelines for rehabilitation, which included immobilization for 6 weeks, early rehabilitation from 6 to 10 weeks, and late rehabilitation from 8 to 12 weeks postoperatively.
Immediately after surgery, the ankle was immobilized in the majority for all types of protocols, and although the types of immobilization varied across protocols most did specify the use of either a cast, boot, or splint to keep the ankle restricted. There was a wide range of variability between protocols in timing of AROM. Most studies recommend 6 weeks of immobilization,16,20,24,28,29,31–33,36 and previous studies have shown the benefits of early mobilization as early as 4 weeks after surgery.13,40,41 Thus, Karlsson et al.40 reported no difference in functional or stability outcomes between early mobilization and normal mobilization, and illustrated beneficial values in earlier RTS and better muscle strength. Early mobilization was defined as movement in an air cast after only 7 to 10 days in plaster casts, while normal mobilization was defined as a plaster cast for 6 weeks. Similarly, Pearce et al.13 outlined the conflict between immobilizing and protecting the joint versus avoiding stiffness and the complications of immobilization. Their recommendation was a 10 to 14-day immobilization phase.13 Of DF, PF, eversion, and inversion, inversion was restricted for the longest time in protocols that included these. This is likely because inversion provides the greatest stress to the lateral ankle fixation and inversion force is the original mechanism of injury for the patients suffering from ankle sprains.
For repair protocols, RTS was one of the most consistent aspects with all protocols RTS level training being around 12 to 16 weeks, which matches up with recommendations in the literature.13,42,43 Although slightly more variable, reconstruction protocols mostly recommended RTS between 12 to 20 weeks, which matches relatively well with the literature.28,31,35,38,44 However, in the literature there is also variability in RTS time. Pearce et al.13 outlined RTS as occurring between 12 weeks and 4 months postoperatively. Lee et al.42 found a mean time of return to personal training in 1.9 months, team training in 2.9 months, and competitive play in 3.9 months. White et al.43 reported a median return to training to be 63 days and RTS in 77 days. In addition, they also made the distinction that these return times were dependent on distinguishing athletes with isolated injuries versus athletes who sustained associated injuries such as osteochondral lesions, injuries to the deltoid ligament, and the distal tibiofibular syndesmosis, which significantly prolonged RTS. Results from studies such as the two previously mentioned, set a framework on which patients could expect to return to daily activities and movements postoperatively, but did not create a standard protocol to follow.
In terms of single leg exercises and return to running, Pearce et al.13 described single leg movements and running as part of the late rehabilitation phase the precedes RTS and included single leg hops as a possible functional test for RTS. It makes sense that protocols allow patients to return to these activities earlier on in rehabilitation than the RTS date as these activities should prepare a patient for the functional demands of RTS. However, strict cut-offs and guidelines for different types of sports were not always discussed in the rehabilitation protocols analyzed in this study, leaving some ambiguity to what RTS functionally meant for the patient.
In areas where suture tape augmentation protocols included recommendations, generally they were earlier in rehabilitation than repair and reconstruction protocols.17,21,22 This included weightbearing immediately postoperatively, all aspects of ROM (DF, PF, eversion, and inversion) during earlier weeks than other protocols, and single leg and running earlier than other protocols (when included). There were no significant differences between repair and reconstruction protocols in terms of the timing of rehabilitation measures.
Although there were some general trends in rehabilitation protocols for lateral ankle repairs, there is high variability in postoperative recommendations. Standardization of rehabilitation would benefit patient outcomes and education. Ultimately, future studies that compare different rehabilitation regimens are necessary to determine the best approach to rehabilitation.
Limitations
This study was limited by the lack of published protocols and the small sample size to analyze. However, this small number is also an important indication of the lack of publishing of protocols from programs. Many programs probably have protocols that they distribute or discuss with patients, but they are not accessible which leaves a wide range of variability unknown. There was such a wide range in recommendations across protocols that it is difficult to consolidate many common themes between protocols. Although many of them mention similar broad topics, within those categories the dates and specific exercises were often completely different from one protocol to the next. This meant that creating a framework of rehabilitation timeline and exercises included was impossible to do by just analyzing the existing published protocols.
CONCLUSION
There is significant variability in the postoperative protocols after surgery for ankle instability. ROM was highly variable across protocols and did not always match up with supporting literature for early mobilization of the ankle. Return to sport was most likely to correlate between protocols and the literature. Weight-bearing was consistent between most protocols but requires further research to determine the best practice. Overall, the variability between programs demonstrated the need for standardization of rehabilitation protocols.
REFERENCES
- 1.Shakked RJ, Karnovsky S, Drakos MC. Operative treatment of lateral ligament instability. Curr Rev Musculoskelet Med. 2017;10(1):113–121. doi: 10.1007/s12178-017-9391-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buerer Y, Winkler M, Burn A, Chopra S, Crevoisier X. Evaluation of a modified Broström-Gould procedure for treatment of chronic lateral ankle instability: A retrospective study with critical analysis of outcome scoring. Foot Ankle Surg. 2013;19(1):36–41. doi: 10.1016/j.fas.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Colville MR. Surgical treatment of the unstable ankle. J Am Acad Orthop Surg. 1998;6(6):368–377. doi: 10.5435/00124635-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Yasui Y, Shimozono Y, Kennedy JG. Surgical procedures for chronic lateral ankle instability. J Am Acad Orthop Surg. 2018;26(7):223–230. doi: 10.5435/JAAOS-D-16-00623. [DOI] [PubMed] [Google Scholar]
- 5.Agoropoulos Z, Papachristou G, Efstathopoulos N, Kokoroghiannis C. Late results of surgical repair in recent ruptures of the lateral ligament of the ankle. Injury. 1997;28(8):531–534. doi: 10.1016/s0020-1383(97)00065-x. [DOI] [PubMed] [Google Scholar]
- 6.Bell SJ, Mologne TS, Sitler DF, Cox JS. Twenty-six-year results after Broström procedure for chronic lateral ankle instability. Am J Sports Med. 2006;34(6):975–978. doi: 10.1177/0363546505282616. [DOI] [PubMed] [Google Scholar]
- 7.Petrera M, Dwyer T, Theodoropoulos JS, Ogilvie-Hrris DJ. Short- to medium-term outcomes after a modified Broström repair for lateral ankle instability with immediate postoperative weightbearing. Am J Sports Med. 2014;42(7):1542–1548. doi: 10.1177/0363546514530668. [DOI] [PubMed] [Google Scholar]
- 8.Russo A, Giacché P, Marcantoni E, Arrighi A, Molfetta L. Treatment of chronic lateral ankle instability using the Broström-Gould procedure in athletes: Long-term results. Joints. 2016;4(2):94–97. doi: 10.11138/jts/2016.4.2.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li X, Killie H, Guerrero P, Busconi BD. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: Functional outcomes after the modified Broström repair using suture anchors. Am J Sports Med. 2009;37(3):488–494. doi: 10.1177/0363546508327541. [DOI] [PubMed] [Google Scholar]
- 10.Guelfi M, Zamperetti M, Pantalone A, Usuelli, Salini V, Oliva XM. Open and arthroscopic lateral ligament repair for treatment of chronic ankle instability: A systematic review. Foot Ankle Surg. 2018;24(1):11–18. doi: 10.1016/j.fas.2016.05.315. [DOI] [PubMed] [Google Scholar]
- 11.Yoo JS, Yang EA. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016;17(4):353–360. doi: 10.1007/s10195-016-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cho BK, Park KJ, Park JK, SooHoo NF. Outcomes of the modified Broström procedure augmented with suture-tape for ankle instability in patients with generalized ligamentous laxity. Foot Ankle Int. 2017;38(4):405–411. doi: 10.1177/1071100716683348. [DOI] [PubMed] [Google Scholar]
- 13.Pearce CJ, Tourné Y, Zellers J, et al. Rehabilitation after anatomical ankle ligament repair or reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1130–1139. doi: 10.1007/s00167-016-4051-z. [DOI] [PubMed] [Google Scholar]
- 14.Southern California Orthopedic Institute. Status Post Brostrom Procedure Ankle Rehabilitation Protocol. Jan 10, 2011. https://www.michaelbahkmd.com/pdf/modified-brostrom-procedure-rehabilitationprotocol.pdf.
- 15.The Stone Clinic. Brostom Procedure Rehab Protocol. 2019. https://www.stoneclinic.com/brostrom-procedure-rehab.
- 16.Cheesapeaker Orthopaedic & Sports Medicine Center. Physical Therapy Section. Ankle Reconstruction/Modified Bröstrom Repair/Peroneal Tendon Repair. 2016. http://www.chesapeakeortho.com/files/cosmc/forms/Brostrom.pdf.
- 17.The University of Kansas Health System. Lateral Ankle Reconstruction/ Brostrom with Reconstruction/Internal Brace Postoperative Protocol. Nov, 2017. https://www.kansashealthsystem.com/-/media/Files/PDF/Ortho-Sports-Med/Ankle-Reconstruction-Brostrom-Internal-Brace.pdf.
- 18.The University of Kansas Health System. Lateral Ankle Reconstruction/ Brostrom with Reconstruction/Syndesmotic Repair Postoperative Protocol. Nov, 2017. https://www.kansashealthsystem.com/-/media/Files/PDF/Ortho-Sports-Med/AnkleReconstructionBrostromSyndesmotic.pdf.
- 19.Tripler Army Medical Center. Ankle Surgery Rehabilitation Guidelines. 2005. https://www.tamc.amedd.army.mil/offices/musculoskeletal/anklefoot_guidelines/ankle_foot.htm.
- 20.UW Health Sports Rehabilitation. Rehabilitation Guidelines for Lateral Ankle Reconstruction. 2014. https://www.uwhealth.org/files/uwhealth/docs/sportsmed/SM-39916_Lateral_AnkleProtocol.pdf.
- 21.Coetzee JC, Ebeling PB. Ankle Ligament Reconstruction/Internal Brace Rehabilitation Protocol. https://tcomn.com/wp-content/uploads/2014/08/Internal-Brace-Ankle-Ligament-Reconstruction.pdf.
- 22.Coetzee JC, Nilsson L. Ankle Ligament Reconstruction Internal Brace Rehabilitation Protocol. https://tcomn.com/wp-content/uploads/2017/08/JCC_Internal-Brace-Ankle-Ligament-Reconstruction-8.28.2017-1.pdf.
- 23.Dierckman B. Modified Brostrom Procedure Protocol (Ankle) American Health Network. Bone and Spine. n.d. https://www.indyboneandspine.com/therapy-protocols.
- 24.Galland M, Kirby K. Galland/Kirby Ankle Reconstruction/Modified Bröstrom Repair/Peroneal Tendone Repair Post Surgical Rehabilitation Protocol. https://orthonc.com/uploads/pdf/Ankle_Reconsrtuction_Modified_Brostrom_Peroneal_Tendon_Repair_New.pdf.
- 25.Toronto Western Hospital. Ankle Rehabilitation Protocol. http://www.utosm.com/wp-content/uploads/2015/06/ankle-ligament-repair-djoh.pdf.
- 26.Jazrawi LM. Post Operative Instructions: Modified Brostrom Gould Procedure. https://www.newyorkortho.com/pdf/modified-brostromgould-procedure-complete-packet-03feb17.pdf.
- 27.Kipnis J, Squire S. Lateral Ligament Reconstruction-Postoperative Protocol. BC Bone and Ankle Clinic; http://bcfootandankle.com/wp-content/uploads/2013/02/Microsoft-Word-Postop-Lateral-Lig-Recon-Protocol-revised-April-2011.pdf. [Google Scholar]
- 28.Seacoast Orthopedics & Sports Medicine. Lateral Ankle Reconstruction Protocol. Sep 20, 2017. http://www.sosmed.org/wp-content/uploads/2014/03/Lateral-Ankle-Reconstruction.pdf.
- 29.Sanford Health. Modified Brostrom Procedure - Operative Rehabilitation Guideline. Jan 16, 2018. https://www.sanfordhealth.org/-/media/org/files/medical-professionals/resources-and-education/modifiedbrostrom-procedure-rehabilitation-guideline.pdf?la=en&hash=16A0BB50537FF352426C77A7CF99356C4AAE3303.
- 30.NC State Sports Medicine. Broström Procedure Protocol. 2020. https://gopack.com/documents/2015/9/8//2_Brostrom_8_5_2013.pdf?id=11758.
- 31.Murray RP, Steven SB, Stevens DW, et al. Lateral Ankle Ligament Reconstruction Rehabilitation Protocol. Oct, 2016. https://mountainortho.com/wp-content/uploads/2016/10/Lateral-Ankle-Ligament-Reconstruction-Rehabilitation-Protocol.pdf.
- 32.William Beaumont Army Medical Center. Ankle Reconstruction/Modified Brostrom Repair/Peroneal Tendon Repair. Aug, 2008. https://www.wbamc.amedd.army.mil/PatientCare/Documents/PostOpRehabProtocols/Brostrom%20WB08.pdf.
- 33.Brigham and Women’s Hospital. Modified Broström Gould Repair for Chronic Ankle Instability. 2010. https://www.brighamandwomens.org/assets/BWH/patients-and-families/pdfs/ankle-brostrom-gould-repairfor-lateral-ankle-instablility.pdf.
- 34.The Stone Clinic. Broström Repair for Chronic Ankle Instability Post Operative Physical Therapy Protocol. https://www.stoneclinic.com/sites/default/files/uploads/brostromrepair.docx.pdf.
- 35.Vora A. Ankle Reconstruction Rehabilitation Protocol. https://dranandvora.com/rehabilitation-protocol/ankle-reconstruction/
- 36.Waterman B. Ankle Reconstruction/Modified Broström Repair/Peroneal Tendon Repair. 2017. https://brianwatermanmd.com/postop/ankle-reconstruction-modified-brostrom-repair-peroneal-tendon-repair/
- 37.Wexner Medical Center. Chronic Ankle Instability Clinical Practice Guideline. https://wexnermedical.osu.edu/-/media/files/wexnermedical/patient-care/healthcare-services/sports-medicine/education/medicalprofessionals/knee-ankle-and-foot/chronic-ankle-instability-cpg-2019.pdf?la=en&hash=97A3C17853F6072AD5C6C759ED46AE8E4CD546E2.
- 38.Coetzee JC, Nilsson L. Ankle Ligament Reconstruction Rehabilitation Protocol. https://tcomn.com/wp-content/uploads/2020/01/Coetzee_Ankle_Ligament_Reconstruction_2020-01.pdf.
- 39.Miyamoto W, Takao M, Yamada K, Matsushita T. Accelerated versus traditional rehabilitation after anterior talofibular ligament reconstruction for chronic lateral instability of the ankle in athletes. Am J Sports Med. 2014;42(6):1441–1447. doi: 10.1177/0363546514527418. [DOI] [PubMed] [Google Scholar]
- 40.Karlsson J, Lundin O, Lind K, Styf J. Early mobilization versus immobilization after ankle ligament stabilization. Scand J Med Sci Sports. 1999;9(5):299–303. doi: 10.1111/j.1600-0838.1999.tb00250.x. [DOI] [PubMed] [Google Scholar]
- 41.de Vries JS, Krips R, Sierevelt N, Blankevoort L, van Dijk CN. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011;(8):CD004124. doi: 10.1002/14651858.CD004124.pub3. [DOI] [PubMed] [Google Scholar]
- 42.Lee K, Jegal H, Chung H, Park Y. Return to play after modified Broström operation for chronic ankle instability in elite athletes. Clin Orthop Surg. 2019;11(1):126–130. doi: 10.4055/cios.2019.11.1.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.White WJ, McCollum GA, Calder JD. Return to sport following acute lateral ligament repair of the ankle in professional athletes. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1124–1129. doi: 10.1007/s00167-015-3815-1. [DOI] [PubMed] [Google Scholar]
- 44.Godges J, Klingman R. Ankle - Lateral Ligament Reconstruction and Rehabilitation. https://s3-us-west-2.amazonaws.com/scal-assets/scal-pt-residencyfellowship/09FootRegion/30Ankle-LateralLigamentReconstruction.pdf.