Abstract
Background: Predictors of men’s health behaviors and interest in workplace health promotion are not well known. The aim of this study was to describe men’s interest in workplace health promotion and associated health behaviors. Method: Male employees (N = 781) at six workplaces in British Columbia, Canada, were invited to complete a survey of their health behaviors, demographics, and interest in health promotion prior to implementation of a workplace health program. Findings: A total of 227 male employees (Mage = 43.6 years; SD = 12.1) completed the survey (response rate = 29%). Regarding health behaviors, 62.1% reported 150 weekly minutes of moderate-to-vigorous physical activity (MVPA), 29.3% consumed 5+ servings of fruit/vegetables per day, 56.8% reported 7+ hours sleep/night, 14.4% smoked, and 81.3% consumed alcohol. Men spent 50% of their workday sitting, and higher body mass index (BMI), higher income, and greater hours worked were related to greater hours sitting. Age was inversely related to MVPA. Alcohol consumption was lower among men who were older, had higher income, and worked fewer hours. Most men were interested in being physically active (85%), managing stress (85%), eating healthy (89%), and cancer screening (91%). Higher stage of change for physical activity (β = .20, p = .003) and fruit/vegetable consumption (β = .18, p = .027) were related to interest in these activities. Conclusions/Application to Practice: Occupational health providers should consider worker demographics and could support interventions that target individuals with varying levels of health behaviors given the importance of meeting the needs of often sedentary workers.
Keywords: health promotion, men’s health, occupational health, health behavior, gender
Background
Healthy behaviors such as regular physical activity, healthy eating, avoiding smoking, and limiting alcohol consumption are associated with decreased prevalence of chronic disease, cancer, and premature mortality (Kushi et al., 2012; I. M. Lee et al., 2012; Lim et al., 2012). Although men experience high rates of chronic illness in northern parts of Canada (Statistics Canada, 2013), engaging men in health promotion remains a public health challenge (Bottorff et al., 2015; Caperchione et al., 2012; Taylor et al., 2013). The workplace has emerged as a promising setting for engaging men in promoting their health (Robertson et al., 2015), although men represent a low proportion of participants in workplace health promotion programs (Robroek, van Lenthe, van Empelen, & Burdorf, 2009).
Research exploring sex differences has revealed that men are more likely than women to mistakenly believe they are sufficiently active and to underestimate the health risks of being overweight (Vandelanotte, Duncan, Hanley, & Mummery, 2011). Some evidence also suggests that men are less interested in health-related information and education sessions than women (C. Lee & Owens, 2002). In a recent study, men reported a high level of interest in several topic areas, including physical activity, healthy eating, and managing stress (Dale, Hartley-Folz, Blackman, Dobson, & Gotay, 2016). Predictors of men’s interest in health promotion activities at work are poorly understood. More research is needed to examine associations between sociodemographic factors and health behaviors among men as well as men’s level of interest in workplace health promotion programs. The objectives of this study were to (a) determine what sociodemographic factors were related to men’s health behaviors, (b) describe men’s interest in workplace health promotion activities, and (c) explore whether an association existed between men’s health behaviors and interest in workplace health promotion activities. Having more information about men’s interest in health promotion and their associated health behaviors could allow occupational health practitioners to better support workplace health promotion activities.
Method
This study included a cross-sectional survey where we collected data from men at six worksites prior to the implementation of a men’s workplace health promotion program called POWERPLAY. The POWERPLAY program has been fully described elsewhere (Caperchione et al., 2015). The study protocol was approved by the University or British Columbia Research Ethics Board (H13-02408) and the Northern Health Research Review Committee (RRC-2014-0015).
Participants were recruited from six male-dominated workplaces located in northern British Columbia, Canada. The workplaces included two transport companies (Sites A and B), a shipping terminal (Site C), a regional municipality (Site D), a chemical manufacturing plant (Site E), and a gold mine (Site F). All participants provided (telephone or online) informed consent prior to completing the survey.
All male employees from each of the study sites were invited to complete a survey prior to implementation of a workplace health promotion program. At four worksites (Sites A, B, C, and D), the survey was administered via a computer-assisted telephone interview (2014). At Site E, a shorter online survey was administered (2016), and at Site F, a shorter paper version of the online survey was used to collect participant responses (2017).
Measures
Demographic data collected from all participants included age, ethnicity, marital status, education, employment, income, and occupation. Self-reported height (in centimeters) and weight (in kilograms) was collected to calculate body mass index (BMI [kg/m2]).
Health behaviors
Weekly physical activity was assessed using the Godin Leisure-Time Exercise Questionnaire (Godin & Shephard, 1985). This measure has demonstrated 1-month test–retest reliability of .62, as well as convergent validity (correlation coefficients) with several indices of physical activity such as body fat percentage (.43), 4-week physical activity history (.36), accelerometer readings (.32), and maximal oxygen consumption (VO2max [.56]; D. R. Jacobs, Ainsworth, Hartman, & Leon, 1993). Participants were given definitions and examples of mild (minimal effort, no perspiration, for example, easy walking), moderate (not exhausting, light perspiration, for example, fast walking), and vigorous (heart beats rapidly, sweating, for example, running) activity, and asked to report the number of times per week, and average length of each session (in minutes) they engaged in each for the past 7 days during their free time. Times per week and average length of each session were multiplied to obtain minutes per week of activity. Total minutes of moderate and vigorous activity per week were summed, and a cutoff of 150 minutes was used to classify participants as meeting or not meeting guidelines for recommended physical activity (Canadian Society for Exercise Physiology, 2011; World Health Organization, 2011). Participants were also asked to report their average daily servings of fruit and vegetables based on a measure described by Ma, Betts, Horacek, Georgiou, and White (2003).
Based on the transtheoretical model of change (Prochaska & DiClemente, 1983), stage of change for physical activity and fruit and vegetable consumption was also included (Ma et al., 2003; Nigg, 2005). In this questionnaire, participants were asked a series of questions pertaining to engaging in “regular physical activity” (defined as at least 150 minutes of moderate activity each week) and “regularly eating 7 or more vegetables and fruit in a day” with different branching options depending on response. Response options categorized participants into one of the five groups: precontemplation (“No, and I don’t intend to within the next 6 months”); contemplation (“No, but I intend to within the next 6 months”); preparation (“No, but I intend to within the next 30 days”); action (“Yes, and I have for less than 6 months”); and maintenance (“Yes, and I have for more than 6 months”). These groupings were used as a scale ranging from 1 (precontemplation) to 5 (maintenance) for both physical activity and fruit/vegetable consumption.
The Occupational Sitting and Physical Activity Questionnaire (Chau, Van Der Ploeg, Dunn, Kurko, & Bauman, 2012) was used to capture hours at work, and time spent sitting, standing, walking, and doing heavy labor while at work. On this questionnaire, participants were asked to provide the number of hours they worked in the past 7 days, as well as the number of days they were at work in the last 7 days. Participants were then asked to describe their typical workday in the past 7 days by providing the percent of time they spent sitting, standing, walking, and doing heavy labor or physically demanding tasks (with instructions to make sure the values add up to 100). Hours worked in the last 7 days were divided by days worked to obtain hours per day. The proportion of time spent sitting, standing, walking, and doing heavy labor was multiplied by hours worked per day to obtain hours spent doing each of these activities per day while at work.
Smoking questions (Worksites A-D) were adapted from a national survey (Ontario Tobacco Research Unit, 2011). Participants were asked to choose one option in response to the question, “Are you a . . . .” Response options included regular smoker (smoke everyday), occasional smoker (smoke once in a while, not everyday), ex-smoker (don’t smoke at all anymore, but used to smoke), or nonsmoker (don’t smoke, and have never smoked). Participants who indicated that they currently smoked were then asked to provide a response to an open-ended question, “If you currently smoke, how many tobacco products do you consume in an average day?” Three questions from the Alcohol Use Disorders Identification Test (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001) were included (Worksites A-D) to capture alcohol usage patterns and consumption levels. Participants were first asked, “How often do you have a drink containing alcohol?” Response options included never, monthly or less, 2 to 4 times a month, 2 to 3 times per week, and 4 or more times per week. With the exception of those who answered “never,” participants were then asked, “How many drinks containing alcohol do you have on a typical day when you are drinking?” Response options included one or two, three or four, five or six, seven to nine, and ten or more. Participants were grouped into three categories: “does not drink at all,” “drinks one to two drinks per day,” and “drinks three or more drinks per day.” Participants were also asked, “How often do you have six or more drinks on one occasion?” Response options included never, less than monthly, monthly, weekly, and daily or almost daily.
Participants (Worksites A-D) were asked to report how much sleep (hours) they usually got per night during a work week, and whether they participated in one of the on-site health screenings offered in the previous 3 months (yes/no).
The short form Positive and Negative Affect Schedule (PANAS; Thompson, 2007; Worksites A-D) was employed with instructions for participants to indicate how they normally or typically feel in responses to the five negative (upset, hostile, ashamed, nervous, and afraid) and five positive (alert, inspired, determined, attentive, and active) emotion items on a scale ranging from never (1) to always (5).
Participants were asked about a series of health promotion topics following the question: “In the future, how interested are you in . . . ?” The topics included being physically active, healthy eating, quitting or reducing smoking, reducing alcohol consumption, managing stress, and screening and early detection of cancer. Response options ranged from not at all interested (1) to extremely interested (5), or participants could choose “not applicable.”
Data Analysis
Descriptive statistics were generated and inferential analyses conducted in SPSS version 25. Adjusted multivariate linear regression models were conducted with each health promotion behavior as the dependent variable and age, BMI, level of education, income, and hours worked entered simultaneously as predictor variables. Adjusted logistic regression models were conducted for the binary outcome variables (i.e., smoker/ex-smoker vs. nonsmoker and consuming two or fewer drinks per day vs. three or more drinks per day). Finally, associations between health behaviors and interest in workplace health promotion activities were examined using one-way ANOVAs for dichotomous variables and adjusted linear regression for continuous variables, with predictor variables entered simultaneously. Worksite was entered as a control variable in all models.
Results
In total, 227 male employees across the six worksites completed the baseline survey (Table 1). Participant’s ranged in years of age from 18 to 66, with BMI’s ranging from 19 to 46 kg/m2; hours worked per day varied from 6 to 15, and the number of hours worked in the past 7 days varied from 0 to 105. Overall, 83% were Caucasian, 54% were married, 92% had completed high school or higher level of education, 94% were employed full-time, and 51% had annual incomes more than Can$100,000.
Table 1.
Characteristics of Male Study Participants (N = 227)
| M (SD) | |
|---|---|
| Age (years) | 43.6 (12.1) |
| Body mass index (kg/m2) | 28.8 (4.4) |
| Hours worked in a typical workday | 10.7 (1.8) |
| Hours worked in the past 7 days | 56.38 (21.5) |
| N (%) | |
| Ethnicity | |
| Caucasian | 188 (82.8) |
| First Nations | 12 (5.3) |
| Métis | 10 (4.4) |
| Other | 11 (4.8) |
| Marital status | |
| Married | 123 (54.2) |
| Common-law relationship/live in partner | 40 (17.6) |
| Single | 46 (20.3) |
| Separated/divorced | 17 (7.5) |
| Widowed | 1 (0.4) |
| Education | |
| Some high school | 19 (8.4) |
| Completed high school | 68 (30.1) |
| Trades certification/college diploma | 110 (48.7) |
| University degree | 29 (12.8) |
| Employment status | |
| Full-time | 213 (93.8) |
| Part-time | 7 (3.1) |
| Contract | 5 (2.2) |
| Summer work/co-op student | 2 (0.9) |
| Income | |
| More than Can$100,000 | 116 (51.1) |
| Can$50,000 to Can$100,000 | 74 (32.6) |
| Less than Can$50,000 | 18 (7.9) |
| Prefer not to answer/no response | 19 (8.4) |
| Occupation | |
| Tradesperson (e.g., mechanic, engineer, welder) | 60 (26.4) |
| Truck driver | 47 (20.7) |
| Heavy equipment operator | 22 (9.7) |
| Manger/supervisor/superintendent/foreman | 18 (7.9) |
| Miner | 13 (5.7) |
| Health & Safety/paramedic/first aid attendant/nurse | 10 (4.4) |
| Laborer/warehouseperson | 10 (4.4) |
| Firefighter/fire chief | 9 (4.0) |
| Housekeeping/camp maintenance/janitorial/camp cook | 6 (2.6) |
| Operator/process operator | 4 (1.8) |
| IT support | 4 (1.8) |
| Human resources | 3 (1.3) |
| Other (e.g., lifeguard, dispatch, sales, utilities, etc.) | 18 (7.9) |
| Not reported | 3 (1.3) |
Health Behaviors
Health behaviors are summarized in Table 2. Over half the men (141; 62%) self-reported 150 minutes or more of moderate-to-vigorous physical activity (MVPA; meeting guidelines) in the previous week. However, fruit and vegetable consumption was low, with 66 (29.3%) consuming five or more servings per day, and 27 (12%) consuming seven or more servings. On average, men spent 50% of their workday sitting, and 56.8% were getting 7 or more hours per night sleep on work nights. Together, 14.4% of the men were regular or occasional smokers, although an additional 30.9% were ex-smokers. The majority (81.3%) reported drinking alcohol at least monthly, and 20.8% reported having more than five drinks on one occasion at least once a month (defined as “heavy drinking”; Statistics Canada, 2013).
Table 2.
Summary of Male Participants’ Self-Reported Health Behaviors (N = 227)
| N | % or M (SD) | |
|---|---|---|
| Met physical activity guidelines (150 minutes/week) | 141 | 62.1 |
| Stage of change for physical activity | ||
| Precontemplation | 20 | 8.8 |
| Contemplation | 12 | 5.3 |
| Preparation | 58 | 25.6 |
| Action | 10 | 4.4 |
| Maintenance | 127 | 55.9 |
| Fruit and vegetables (servings/per day) | 3.7 (2.1) | |
| Stage of change for fruit and vegetable consumptiona | ||
| Precontemplation | 95 | 42.2 |
| Contemplation | 12 | 5.3 |
| Preparation | 91 | 40.4 |
| Action | 4 | 1.8 |
| Maintenance | 23 | 10.2 |
| Hours per work day spent | ||
| Sitting | 225 | 5.4 (3.6) |
| Standing | 225 | 1.9 (1.7) |
| Walking | 225 | 2.1 (1.6) |
| Heavy labor | 225 | 1.2 (1.8) |
| Nightly sleep (hours)a | 139 | 6.58 (1.14) |
| Smoking statusa | ||
| Nonsmoker | 74 | 53.2 |
| Ex-smoker | 43 | 30.9 |
| Regular smoker | 16 | 11.5 |
| Occasional smoker | 4 | 2.9 |
| No response | 2 | 1.4 |
| Alcohol consumption (based on a standard drink)a | ||
| Never | 26 | 18.7 |
| Monthly or less | 29 | 20.9 |
| 2-4 times a month | 30 | 21.6 |
| 2-3 times per week | 33 | 23.7 |
| 4 or more times per week | 21 | 15.1 |
| How many drinks containing alcohol do you have on a typical day?a | ||
| Does not drink at all | 26 | 18.7 |
| One or two drinks | 67 | 42.2 |
| Three or more drinks | 46 | 33.1 |
| How often do you have six or more drinks on one occasion?a | ||
| Does not drink at all | 26 | 18.7 |
| Never | 35 | 25.2 |
| Less than monthly | 49 | 35.3 |
| Monthly | 20 | 14.4 |
| Weekly | 7 | 5.0 |
| Daily, or almost daily | 2 | 1.4 |
| Unknowna | ||
| Participated in on-site blood pressure health screeninga | ||
| Yes | 53 | 38.1 |
| No | 86 | 61.9 |
Question not asked at Site E or F which consisted of 88 participants.
Association Between Sociodemographic Characteristics and Health Behaviors
Results of the analyses to examine which sociodemographic characteristics were related to health behaviors are presented in Table 3. MVPA and recommended servings of fruit/vegetable per day was higher for younger men and those with lower BMI. Hours spent sitting at work was higher for those with a higher BMI, higher income, and greater hours worked. The number of hours of sleep per night was lower for men who worked more hours, whereas alcohol consumption was lower among men who were older, had higher income, and worked fewer hours. Men with higher education levels had a lower likelihood of being a smoker/ex-smoker, while younger men were more likely to consume three or more alcoholic drinks per day.
Table 3.
Results of Adjusted Multivariate and Logistic Regressions Between Age, BMI, Education Level, Income, and Hours Worked With Health Behaviors
| Continuous health behavior outcomes | Predictor variables | F | p | R 2 | N | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age | BMI | Education | Income | Hours worked/ 7 days |
||||||
| β | β | β | β | β | ||||||
| Full models | MVPA minutes/week | −.17* | −.17* | −.02 | .05 | .06 | 2.26 | .039 | .06 | 204 |
| Servings of fruit/veg | −.04 | −.18* | .14 | .06 | .09 | 4.35 | .000 | .12 | 205 | |
| Hours sitting/day | .11 | .15* | .12 | .19** | .26* | 5.83 | .000 | .15 | 204 | |
| Hours sleep/night | .10 | −.15 | .03 | −.14 | −.20* | 1.89 | .089 | .08 | 131 | |
| Number of alcoholic beverages consumeda | −.30** | .00 | −.12 | −.06 | .12 | 2.17 | .053 | .12 | 106 | |
| How often six or more drinks on one occasiona | −.34** | −.24** | −.31** | .13 | .19* | 5.83 | .000 | .26 | 105 | |
| Dichotomous health behavior outcomes | OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
χ2 | p | R 2 | N | |
| Smoker or ex-smoker—Yes | 1.02 [0.99, 1.06] |
0.99 [0.90, 1.08] |
0.42**
[0.24, 0.73] |
1.02 [0.52, 2.01] |
1.02 [0.99, 1.05] |
15.29 | <.001 | .15 | 129 | |
| Three or more alcoholic drinks per day—Yes | 0.96*
[0.93, 0.99] |
1.05 [0.95, 1.15] |
0.86 [0.51, 1.45] |
0.61 [0.32, 1.14] |
1.01 [0.98, 1.04] |
12.13 | .05 | .12 | 131 | |
Note. BMI = body mass index; MVPA = moderate-to-vigorous physical activity; OR = odds ratio; CI = confidence interval.
Includes just those who drink alcohol; separate multivariate regressions were conducted for each continuous health behavior outcome variable with worksite entered first as a control variable, and age, BMI, education, income, and hours worked entered on the next step. Separate logistic regression analyses were conducted for each dichotomous health behavior outcome variable with worksite entered first as a control variable, and age, BMI, education, income, and hours worked entered on the next step. Adjusted βs and adjusted odds ratios are reported. Nagelkerke R2 is reported for logistic regressions.
p < .05. **p < .01.
Association Between Health Behaviors and Interest in Health Promotion Activities
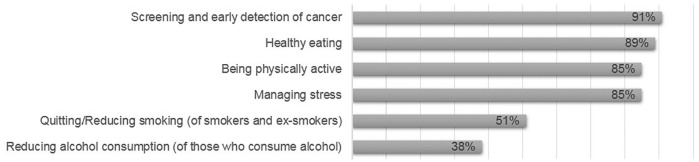
The proportion of men who were interested in workplace wellness activities related to physical activity, healthy eating, quitting/reducing smoking, reducing alcohol, managing stress, and screening for cancer is shown in Figure 1.
Figure 1.
Proportion of men who were at least moderately interested in workplace health promotion activities by topic area (n = 227).
The following includes a summary of associations between relevant health behaviors and interest in health promotion topics (data not shown). Interest in workplace physical activity programs was high in those who reported engaging in 150 minutes or more MVPA per week (M = 3.68), compared with those engaging in less than 150 minutes (M = 3.41), although this difference did not reach statistical significance (p = .071). Hours spent sitting was unrelated (β = −.02, p = .82), although higher stage of change for physical activity was related (β = .20, p = .003) to interest in physical activity. The number of servings of fruit and vegetables consumed was not significantly related to interest in healthy eating (β = −.06, p = .49), but higher stage of change for fruit/vegetable consumption was (β = .18, p = .027). How often men reported having an alcohol beverage was the only variable that made a significant independent contribution to interest in learning about reducing alcohol consumption (β = .31, p = .004). When the analysis was limited to only those who consumed alcohol, the model became nonsignificant, suggesting that it is not the amount of alcohol consumed per se, but whether or not men consumed alcohol (yes/no) that drove interest in learning about reducing alcohol. Lower ratings of general health (β = −.26, p = .005), and higher negative affect (β = .23, p = .007), but not a positive affect (β = .10, p = .26), were related to an interest in learning about managing stress. Level of interest in screening and early detection of cancer was not different among those who participated in the on-site (blood pressure) health screenings (M = 4.21) and those who did not participate (M = 4.10), p = .61. Men’s level of MVPA (β = .02, p = .72) and number of servings of fruit/vegetable consumed (β = −.001, p = .99) were not significantly related to their interest in screening and early detection of cancer.
Discussion
The purpose of this study was to explore men’s health behaviors and their interest in health promotion activities. In terms of reported health-promoting behaviors, the current study respondents were comparable with the 2013 profile for Canadian men. For example, 62.1% were achieving 150 minutes of MVPA a week (compared with 62.8% of men in British Columbia and 56.3% of men in Canada who were “moderately active” or “active”), 29.3% reported eating more than five servings per day (compared with 35.3% of men in British Columbia/33.7% of men in Canada), 20.8% reported having more than five drinks on one occasion at least once a month (compared with 22.4% of men in BC/25.5% of men in Canada), and 11.5% were regular smokers (similar to the BC average where 11.9% of men are daily smokers; Statistics Canada, 2013).
There was a fairly high level of activity (more than half meeting guidelines) and, in turn, an interest in physical activity promotion. There was also interest in other important health behaviors, including healthy eating, managing stress, and screening and early detection of cancer. These findings are in line with recent research suggesting that men have a high level of interest in workplace health promotion activities (Dale et al., 2016). These findings also support the notion that men at work might be considered an “untapped” group for promoting and supporting healthy lifestyle behaviors (Pringle et al., 2014). Health promotion programs that are tailored to men’s interests and include workplace changes that enable and support health behaviors hold strong potential for mustering and sustaining behavior change (Bottorff et al., 2015; Hunt et al., 2014; Morgan et al., 2011; Young, Camhi, Wu, Hagberg, & Stefanick, 2013). Given the high levels of interest in health promotion activities among men, male employees are likely to respond favorably to policy, practice, and setting changes that affirm and norm these health behaviors. Within this context, it is important that workplaces make cultural changes to enable and support men to engage in healthy behaviors rather than relying entirely on efforts for motivating men to change their behaviors. A workplace “culture” that is supportive of employee’s psychosocial needs (e.g., flexible work, respectful personal relationships, good communication) plays a significant role in the uptake of workplace health promotion (Dickson-Swift, Fox, Welch, Marshall, & Willis, 2014).
The results of this study indicate men are diverse, affirming the naivety of espousing a “one size fits all” approach for promoting men’s health in the workplace. Ever present is the need to engage men through building context as well as opportunities, especially for subgroups of men who are reluctant to take up health-promoting practices. For example, workplace-based programs to support smoking cessation will likely need to rely on innovative strategies to reach men, given the activities may only apply to the subgroup of smokers. In a recent example, Ottawa Public Health partnered with 25 construction companies to successfully engage men in the construction industry where smoking rates are high (Dupuis, McKean, & Chow, 2018). Another study used an innovative approach to health promotion by engaging lunch trucks in an effort to reach construction workers (Caban-Martinez et al., 2018). Male-dominated workplace cultures can shift to normalize such engagement, and in this regard, there are likely significant gains in lobbying men who are actively promoting their health to champion the cause (e.g., former smokers) with less informed and invested workmates. Building on this point, targeted men’s health promotion program content might fit, but the call to action needs to be thoughtfully considered in terms of both how and who petitions the more reluctant men. Kivari, Oliffe, Borgen, and Westwood (2018) offered the military example of returned service men doing the work of health promotion to aid their comrades’ well-being, and the ideals of helping out a mate might similarly solidify health-promoting practices in male-dominated workplaces.
Careful consideration of the sociodemographic characteristics of subgroups of men is important when considering the design, testing, and implementation of workplace wellness programming. For example, in the current study, older men reported lower MVPA but consumed fewer alcoholic beverages and were less likely to binge drink compared with younger men. Indeed, other research has shown that binge drinkers are more likely to be younger males (Wild, Roberts, Cunningham, Schopflocher, & Pazderka-Robinson, 2004). It may be advisable to consider the average age of a given workforce when designing workplace interventions for men. A module approach to health promotion could also allow workers and/or employers to select what they perceive as most applicable to the workplace context.
In the present study, hours worked was related to more hours spent sitting, fewer hours sleeping, and binge drinking. Other research indicates that working longer hours is related to an increase in smoking and unhealthy weight gain among Canadian men (Shields, 1999), and to poor mental health, smoking, sleep deficits, and lower physical activity (Artazcoz, Cortes, Escriba-Aguir, Cascant, & Villegas, 2009). Sedentary behavior (hours spent sitting) was positively related to BMI as well as income, yet was unrelated to interest in physical activity.
We found that men in a higher stage of change for physical activity and fruit and vegetable consumption were more likely to be interested in these health-promoting activities; however, interest in physical activity, healthy eating, and screening was not consistently related to health behaviors. Instead, it is possible that men were interested in physical activity, healthy eating, and screening for diverse reasons, highlighting the plurality of this group and the need for interventions that target individuals with varying levels of these health behaviors. Interest in learning about health-promoting behaviors may not necessarily translate into taking action (behaviors). In a study of Canadian workers, both men and women with lower levels of awareness about their cardiovascular disease risk reported fewer preventive health behaviors than those with higher levels of awareness (J. C. Jacobs, Burke, Rouse, Sarma, & Zaric, 2016). Future studies might explore the association between health risk awareness or health literacy and interest in wellness activities.
In other research, men with higher alcohol consumption were also more likely to be interested in a self-help intervention for reducing alcohol consumption (Wild et al., 2004). The current study findings that men who drank more often expressed more interest in workplace health promotion activities focused on alcohol reduction suggest that this finding extends to men working in male-dominated workplaces. Given the interest in reducing alcohol was lower overall among current study respondents, it may be important to offer confidential supports for those interested in reducing their alcohol consumption.
In the present study, men who perceived their general health to be poorer as well as men who had higher levels of negative affect were more interested in activities related to managing stress. Here, it may be notable that we did not ask about “reducing” but about “managing” stress; recent qualitative research suggested the possibility that men may only talk openly about stress at work if they are perceived to be controlling it (Seaton, Bottorff, Oliffe, Medhurst, & DeLeenheer, 2018). The present results suggest that men who are likely feeling more stress are most interested in workplace activities related to managing stress. Here again, knowing the population being targeted can help in the design of tailored interventions to better support men at work.
Limitations and Suggestion for Future Research
The current study sample included working men, who were Canadian-based and predominately Caucasian, and had high incomes, limiting generalization of the study results to other populations. This limitation is particularly relevant when considering the findings for income, as the results may be different in lower income groups (including the working poor). The surveys for two sites were shorter and were completed 2 to 3 years after those completed at the other four sites, possibly influencing the results. Although all men in the workplace were invited and encouraged to participate in the survey, it was primarily completed by men who subsequently signed up for the POWERPLAY health promotion program. Men’s interest in health promotion activities may have been influenced by anticipation of the program, or self-selection may have played a role in the results. The sample was comparable with Canadian averages in terms of health behaviors and included men from a range of male-dominated workplaces. We did reach men that we wanted to target with a health promotion program, given the average BMI was more than 25, the low fruit/vegetable consumption, and high proportion of workday spent sitting. Future research could explore the preferences and characteristics of men who are not already meeting national recommendations related to health behaviors (e.g., physical activity guidelines, servings of fruit/vegetable, smoking, and alcohol consumption) to better inform interventions to effectively reach these groups.
Conclusion
Overall, effective workplace health promotion programs hold potential for reducing the risk of chronic disease and improving health among working men. The results of the current study suggest that men are a diverse group with a high level of interest in several workplace health promotion topics. Because there is limited evidence about how men’s health behaviors might relate to their interest in workplace health promotion programs, the current study contributes important understandings. In particular, the current study reveals high levels of interest in health promotion activities among working men, a finding that prevails across diverse respondent contexts and readiness to change. As might be expected, men in a higher stage of change were more likely to be interested in physical activity and healthy eating—those who intended to engage in these behaviors were most interested in them. Building on this, there are likely benefits for all men from targeted workplace health promotion programs, notwithstanding the magnitude of those gains varies across a range of variables, including readiness to change. A significant challenge within this context is to target specific subgroups of less healthy men within tailored interventions that satiate the needs of men with higher levels of change. The present findings poignantly reminds occupational health care providers of the need to both target health promotion interventions for men and tailor those programs to reach subgroups within male-dominated workplaces.
Implications for Occupational Health Nursing Practice
The high level of interest in health promotion activities among men in this study, coupled with previous research suggesting that men are less likely to participate in workplace health activities (Robroek et al., 2009), suggests that men are an underserved group. Occupational health practitioners are ideally positioned to design, deliver, and formally evaluate workplace health promotion activities that engage men with diverse health behaviors and varying levels of change. This relates to structural issues as well as efforts for garnering men’s behavior change. Health promotion as a mandate for most workplaces offers important opportunities to bolster access to health information and services for men (bypassing barriers some men experience accessing traditional health services and systems). That paid work is deeply tied to masculine ideals of physical prowess and productivity also bodes well for building male-dominated workplace cultures that value health-promoting behaviors, and the adjustments thereof, as performance enhancing. Playing to masculine ideals can also inform friendly competitions (e.g., step challenges) to make accessible and reward men’s physical efforts and conditioning (e.g., easily accessible stairs, bike racks, gazebo to encourage taking breaks outdoors, etc.). The present findings offer beginning insights to guide occupational health practitioners targeted and tailored men’s workplace health promotion programs.
Applying Research to Practice.
The findings of this research suggest that there are high levels of interest in health promotion activities among working men, although men are a diverse group in terms of their readiness to change and reasons for this interest. Occupational health practitioners should support targeted and tailored approaches to engage men in health promotion in addition to advocating for practices and policies that support men’s health behavior change in the workplace. Within specific workplaces, the sociodemographic characteristics of the target population can guide tailored interventions to address specific health behaviors such as reducing alcohol consumption among younger male workforces.
Author Biographies
Cherisse L. Seaton is a research coordinator at the University of British Columbia’s Okanagan Campus and an adjunct professor at the University of Northern British Columbia (UNBC). Her research focuses on individual differences and the promotion of health and well-being among adult populations.
Joan L. Bottorff is a professor in the School of Nursing and director of the Institute for Healthy Living and Chronic Disease Prevention at the University of British Columbia’s Okanagan campus. Her research program focuses on health promotion and health behavior change in the context of cancer prevention.
Cristina M. Caperchione is an associate professor in the sports and exercise science program at the University Technology Sydney. Her research interests include health-related physical activity and the use of behavioral change strategies in the prevention, reduction, and management of chronic disease.
Steven T. Johnson is an associate professor in the Centre for Nursing and Health Studies at Athabasca University. His research interests include clinical and community-based lifestyle interventions for preventing and managing obesity, type 2 diabetes, and cardiovascular disease, as well as workplace wellness for men and sleep health.
John L. Oliffe is a professor in the School of Nursing at the University of British Columbia. His internationally recognized research is focused on gender and health, particularly men’s health.
Footnotes
Author Contributions: C.L.S. was involved in the study conception and design, data analysis and interpretation of results, and drafting and revising the article. J.L.B. was involved in the study conception and design, data interpretation, and in drafting and revising the article. C.M.C. was involved in data interpretation and in drafting and critically revising the article. S.T.J. participated in data interpretation and in drafting and critically revising the article. J.L.O. participated in data interpretation and in drafting and critically revising the article. All authors reviewed and approved the final article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Canadian Cancer Society Research Institute (Grant No. 701259-02).
ORCID iD: Cherisse L. Seaton  https://orcid.org/0000-0003-4646-9894
https://orcid.org/0000-0003-4646-9894
References
- Artazcoz L., Cortes I., Escriba-Aguir V., Cascant L., Villegas R. (2009). Understanding the relationship of long working hours with health status and health-related behaviours. Journal of Epidemiology & Community Health, 63, 521-527. doi: 10.1136/jech.2008.082123 [DOI] [PubMed] [Google Scholar]
- Babor T. F., Higgins-Biddle J. C., Saunders J. B., Monteiro M. G. (2001). AUDIT: The Alcohol Use Disorders Identification Test guidelines for use in primary care (2nd ed.). Geneva, Switzerland: World Health Organization. [Google Scholar]
- Bottorff J. L., Seaton C. L., Johnson S. T., Caperchione C. M., Oliffe J. L., More K., . . . Tillotson S. M. (2015). An updated review of interventions that include promotion of physical activity for adult men. Sports Medicine, 45, 775-800. doi: 10.1007/s40279-014-0286-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caban-Martinez A. J., Moore K. J., Clarke T. C., Davila E. P., Clark J. D., Lee D. J., Fleming L. E. (2018). Health promotion at the construction work site: The lunch truck pilot study. Workplace Health and Safety, 66(12), 571-576. doi: 10.1177/2165079918764189 [DOI] [PubMed] [Google Scholar]
- Canadian Society for Exercise Physiology. (2011). Canadian physical activity guidelines for adults aged 18-64. Retrieved from https://csepguidelines.ca/wp-content/uploads/2018/03/CSEP_PAGuidelines_adults_en.pdf
- Caperchione C. M., Sharp P., Bottorff J. L., Stolp S., Oliffe J. L., Johnson S. T., . . . Lamont S. (2015). The POWERPLAY workplace physical activity and nutrition intervention for men: Study protocol and baseline characteristics. Contemporary Clinical Trials, 44, 42-47. doi: 10.1016/j.cct.2015.07.013 [DOI] [PubMed] [Google Scholar]
- Caperchione C. M., Vandelanotte C., Kolt G. S., Duncan M., Ellison M., George E., Mummery W. K. (2012). What a man wants: Understanding the challenges and motivations to physical activity participation and healthy eating in middle-aged Australian men. American Journal of Men’s Health, 6, 453-461. doi: 10.1177/1557988312444718 [DOI] [PubMed] [Google Scholar]
- Chau J. Y., Van Der Ploeg H. P., Dunn S., Kurko J., Bauman A. E. (2012). Validity of the occupational sitting and physical activity questionnaire. Medicine & Science in Sports & Exercise, 44, 118-125. doi: 10.1249/MSS.0b013e3182251060 [DOI] [PubMed] [Google Scholar]
- Dale L., Hartley-Folz S., Blackman F., Dobson B., Gotay C. (2016). Men in rural and remote locations: Their preferences for worksite wellness programs. Journal of Occupational and Environmental Medicine, 58, e279-e280. doi: 10.1097/JOM.0000000000000780 [DOI] [PubMed] [Google Scholar]
- Dickson-Swift V., Fox C., Welch N., Marshall K., Willis J. (2014). What really improves employee health and wellbeing: Findings from regional Australian workplaces. International Journal of Workplace Health Management, 7, 138-155. doi: 10.1108/IJWHM-10-2012-0026 [DOI] [Google Scholar]
- Dupuis L., McKean H., Chow H. (2018). Quitting the smoke break: A successful partnership with the construction industry. Canadian Journal of Public Health, 109, 128-133. doi: 10.17269/s41997-018-0019-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godin G., Shephard R. J. (1985). A simple method to assess exercise behavior in the community. Canadian Journal of Applied Sport Sciences, 10, 141-146. [PubMed] [Google Scholar]
- Hunt K., Wyke S., Gray C. M., Anderson A. S., Brady A., Bunn C., . . . Leishman J. (2014). A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish premier league football clubs (FFIT): A pragmatic randomised controlled trial. The Lancet, 383, 1211-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs D. R., Jr., Ainsworth B. E., Hartman T. J., Leon A. S. (1993). A simultaneous evaluation of 10 commonly used physical activity questionnaires. Medicine & Science in Sports & Exercise, 25, 81-91. [DOI] [PubMed] [Google Scholar]
- Jacobs J. C., Burke S., Rouse M., Sarma S., Zaric G. (2016). Cardiovascular disease risk awareness and its association with preventive health behaviors: Evidence from a sample of Canadian workplaces. Journal of Occupational and Environmental Medicine, 58, 459-465. doi: 10.1097/JOM.0000000000000694 [DOI] [PubMed] [Google Scholar]
- Kivari C. A., Oliffe J. L., Borgen W. A., Westwood M. J. (2018). No man left behind: Effectively engaging male military veterans in counseling. American Journal of Men’s Health, 12, 241-251. doi: 10.1177/1557988316630538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushi L. H., Doyle C., McCullough M., Rock C. L., Demark-Wahnefried W., Bandera E. V., . . . Nutrition and Physical Activity Guidelines Advisory Committee. (2012). American cancer society guidelines on nutrition and physical activity for cancer prevention: Reducing the risk of cancer with healthy food choices and physical activity. CA: A Cancer Journal for Clinicians, 62, 30-67. doi: 10.3322/caac.20140 [DOI] [PubMed] [Google Scholar]
- Lee C., Owens R. G. (2002). Issues for a psychology of men’s health. Journal of Health Psychology, 7, 209-217. doi: 10.1177/1359105302007003215 [DOI] [PubMed] [Google Scholar]
- Lee I. M., Shiroma E. J., Lobelo F., Puska P., Blair S. N., Katzmarzyk P. T., & Lancet Physical Activity Series Working Group. (2012). Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet, 380, 219-229. doi: 10.1016/S0140-6736(12)61031-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim S. S., Vos T., Flaxman A. D., Danaei G., Shibuya K., Adair-Rohani H., . . . Memish Z. A. (2012). A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet, 380, 2224-2260. doi: 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J., Betts N. M., Horacek T., Georgiou C., White A. (2003). Assessing stages of change for fruit and vegetable intake in young adults: A combination of traditional staging algorithms and food-frequency questionnaires. Health Education Research, 18, 224-236. [DOI] [PubMed] [Google Scholar]
- Morgan P. J., Collins C. E., Plotnikoff R. C., Cook A. T., Berthon B., Mitchell S., Callister R. (2011). Efficacy of a workplace-based weight loss program for overweight male shift workers: The workplace POWER (preventing obesity without eating like a rabbit) randomized controlled trial. Preventive Medicine, 52, 317-325. doi: 10.1016/j.ypmed.2011.01.031 [DOI] [PubMed] [Google Scholar]
- Nigg C. R. (2005). There is more to stages of exercise than just exercise. Exercise and Sport Sciences Reviews, 33, 32-35. doi:00003677-200501000-00006 [PubMed] [Google Scholar]
- Ontario Tobacco Research Unit. (2011). Tobacco Informatics Monitoring System (TIMS). https://www.otru.org/resources/tims/
- Pringle A., Zwolinsky S., McKenna J., Robertson S., Daly-Smith A., White A. (2014). Health improvement for men and hard-to-engage-men delivered in English premier league football clubs. Health Education Research, 29, 503-520. doi: 10.1093/her/cyu009 [DOI] [PubMed] [Google Scholar]
- Prochaska J. O., DiClemente C. C. (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51, 390-395. [DOI] [PubMed] [Google Scholar]
- Robertson S., White A., Gough B., Robinson M., Seims A., Raine G., Hanna E. (2015). Promoting mental health and wellbeing in men and boys: What works? Leeds, UK: Leeds Beckett University. [Google Scholar]
- Robroek S. J., van Lenthe F. J., van Empelen P., Burdorf A. (2009). Determinants of participation in worksite health promotion programmes: A systematic review. The International Journal of Behavioral Nutrition and Physical Activity, 6, 2-26. doi: 10.1186/1479-5868-6-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seaton C. L., Bottorff J. L., Oliffe J. L., Medhurst K., DeLeenheer D. (2018). Mental health promotion in male-dominated workplaces: Perspectives of male employees and workplace representatives. Psychology of Men & Masculinity, 204, 541-552. doi: 10.1037/men0000182 [DOI] [Google Scholar]
- Shields M. (1999). Long working hours and health. Health Reports, 11, 33-48. [PubMed] [Google Scholar]
- Statistics Canada. (2013). Health profile, December 2013 (table) (Statistics Canada Catalogue No. 82-228-XWE). Ottawa: Retrieved from https://www12.statcan.gc.ca/health-sante/82-228/index.cfm?Lang=E [Google Scholar]
- Taylor P. J., Kolt G. S., Vandelanotte C., Caperchione C. M., Mummery W. K., George E. S., . . . Noakes M. J. (2013). A review of the nature and effectiveness of nutrition interventions in adult males–a guide for intervention strategies. The International Journal of Behavioral Nutrition and Physical Activity, 10, 1-13. doi: 10.1186/1479-5868-10-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson E. R. (2007). Development and validation of an internationally reliable short-form of the Positive and Negative Affect Schedule (PANAS). Journal of Cross-Cultural Psychology, 38, 227-242. doi: 10.1177/0022022106297301 [DOI] [Google Scholar]
- Vandelanotte C., Duncan M. J., Hanley C., Mummery W. K. (2011). Identifying population subgroups at risk for underestimating weight health risks and overestimating physical activity health benefits. Journal of Health Psychology, 16, 760-769. doi: 10.1177/1359105310390543 [DOI] [PubMed] [Google Scholar]
- Wild T. C., Roberts A. B., Cunningham J., Schopflocher D., Pazderka-Robinson H. (2004). Alcohol problems and interest in self-help: A population study of Alberta adults. Canadian Journal of Public Health, 95, 127-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2011). Recommended levels of physical activity for adults aged 18-64. Retrieved from https://www.who.int/dietphysicalactivity/factsheet_adults/en/
- Young D., Camhi S., Wu T., Hagberg J., Stefanick M. (2013). Relationships among changes in C-reactive protein and cardiovascular disease risk factors with lifestyle interventions. Nutrition, Metabolism, & Cardiovascular Diseases, 23, 857-863. doi: 10.1016/j.numecd.2012.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]