Corresponding Author

Key Words: AED, bystander, cardiopulmonary resuscitation, citizen responder, OHCA, smartphone app, volunteer
Citizen responders have risen to the occasion ever since communities have been in existence. For centuries, a bell was used to indicate alarm, and community volunteers of the fire company would respond with buckets, hose carts, and hand pumpers. In the 19th century, the bell was replaced by the siren, alerting entire communities of impending danger of fire or tornado, or the need for civil defense. In the 21st century, we do not require bell or siren because “there’s an app for that.”
In this issue of the Journal, Andelius et al. (1) report findings from a prospective observational study in Denmark that used a smartphone application (app) to dispatch citizen responders to the scene of out-of-hospital cardiac arrest (OHCA). The app alerted citizen responders in 819 cases of suspected OHCAs, of which 438 (53.5%) were confirmed OHCAs that met inclusion criteria for the study. At least 1 citizen responder arrived before the emergency medical services (EMS) ambulance crew in 42.0% (184 of 438) of the confirmed OHCAs. In these situations when app-dispatched citizen responders arrived at the scene before EMS, there was a 2-fold and 3-fold higher likelihood of bystander CPR and defibrillation, respectively. Citizen responders initiated CPR in 69% (126 of 184), applied an automated external defibrillator (AED) in 50% (91 of 184), and performed defibrillation in 10% (19 of 184) of the OHCAs where they arrived before EMS. As the EMS response time increased, the proportion of citizen responders who arrived before EMS and performed CPR and/or defibrillation also increased. These are important findings that could have far-reaching ramifications. It would be useful to provide some context and discuss some lessons and limitations of this study.
OHCA remains a major public health challenge (2), with annual incidence exceeding 350,000 in the United States and 620,000 in Europe (3,4). Emergency medical response systems linked to community efforts and advanced care continue to save lives, but survival to discharge from the hospital has plateaued at ≈10% (3,5), leaving significant room for improvement. Bystander CPR and early defibrillation have long been recognized as 2 critical determinants of survival. In a 1985 clinical trial, Cummins et al. (6) demonstrated the benefit of early CPR undertaken by lay persons, firmly reinforcing the concept of bystander CPR. A subsequent meta-analysis reported an approximate doubling of survival with bystander CPR (7). In parallel, the potential role of early defibrillation by lay rescuers using AEDs deployed in the community was explored. In the Public Access Defibrillation trial (8), training of laypersons to perform CPR and use the AED was associated with increased survival of OHCA. Bystander CPR rates range from 25% to 80%, depending on region, but bystander defibrillation is only performed in <10% of OHCAs. More recently, trained bystanders have been connected to OHCAs occurring in their neighborhood by text messages as well as smartphone apps. However, it has been a challenge to make these processes function efficiently (9). Based on the results of their study, Andelius et al. (1) were able to accomplish this goal.
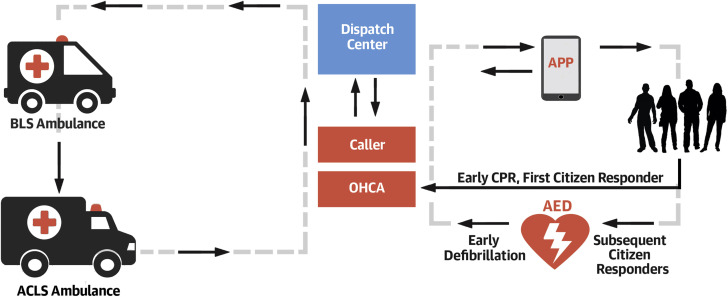
Why were they more successful than other smartphone-app-assisted bystander CPR studies? In large part, this can be attributed to innovative aspects of study design, with an ongoing, continuous feedback loop (Figure 1 ) that involved the dispatch center, EMS, citizen responders, and the caller who informed the dispatch center. The Heartrunner app used in their study activated the citizen responders simultaneously with the 2-tiered EMS system, and the dispatch center stayed involved throughout the process. Unlike other existing smartphone app workflows, these responders acknowledged their acceptance to the dispatch center. The first citizen responder to accept the alarm was instructed to go directly to the OHCA location to start CPR, and the next 4 who accepted were sent to retrieve AEDs that were accurately geo-localized, and to take the AEDs to the OHCA location. This unique dual assignation is likely to have facilitated both early bystander CPR and defibrillation. Furthermore, the Heartrunner app dispatched responders to homes, not just public locations. In fact, 80% of the citizen responders arrived in residential locations, another process that cannot be accomplished without involvement of the dispatch center keeping the original caller informed. Because the majority of OHCAs (70% to 80%) occur at home, this potentially enhances the effectiveness compared to existing apps that direct lay responders only to public locations. The Capital Region of Denmark where this study was conducted is the wealthiest region in Denmark, with high general education level, high bystander CPR education rates, and high population density in a largely urban environment. A fourth of the responders were healthcare professionals and 99% had received CPR training before registration. The societal environment appears to have been accepting of citizen responders gaining access to private home locations in emergency situations.
Figure 1.
Study Design
The workflow involves ongoing communication between the dispatch center and citizen responders via the Heartrunner application (APP), as well as the caller who is at the location of the out of hospital cardiac arrest (OHCA). The first citizen responder is dispatched directly to the OHCA location to perform cardiopulmonary resuscitation (CPR), and the next 4 responders are sent to retrieve automated external defibrillators (AEDs) and bring these to the OHCA location. This facilitates early delivery of both CPR and defibrillation when citizen responders arrive before the ambulance. ACLS = advanced cardiac life support; BLS = basic life support.
The generalizability of these findings will need to be evaluated further. Regions with less favorable socioeconomic status, education level, and cultural cohesiveness may not be able to duplicate these results. Rural areas with low population density as well as AEDs may need unique approaches to improve early defibrillation, such as drone delivery of AEDs, which is currently being piloted or used in several regions. Although only one-half of the suspected OHCA cases were eventually confirmed (438 of 819), >6,800 potential responders were alerted for these. Therefore, an unspecified, large number of additional citizen responders received an alarm that did not require their services. In practical terms, there is potential for “burnout” of citizen responders. Even though citizen responders perform hands-only CPR, it is possible that natural calamities such as the current coronavirus disease-2019 pandemic will adversely affect the citizen response due to fear of contagion.
Andelius et al. (1) are to be congratulated for their seminal findings from this carefully conducted, innovative study. Their study was not designed to evaluate effects of their methodology on survival from OHCA, and a large clinical trial specifically designed for this purpose is ongoing (The Heartrunner Trial; NCT03835403). Their findings highlight the role of the citizen responder equipped with a smartphone app as a potentially effective first line of defense in the community response to OHCA. Generalizability of these findings to other communities and regions still needs to be assessed, but many of these useful concepts could immediately be applied in other communities. Another novel aspect of this study was the assessment of the physical and psychological impact of the process on citizen responders, and the outcome was favorable. Most importantly, to ensure longevity and consistency of the response, citizen responders need to be valued, encouraged, and protected. In the final analysis, the app sounds an alarm, but it is the smart bystander’s goodwill, motivation, and citizenship that saves a life.
Footnotes
Funded by the National Institutes of Health, National Heart, Lung, and Blood Institute (NHLBI) grants R01HL145675 and R01HL147358 (to Dr. Chugh). All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
References
- 1.Andelius L., Malta Hansen C., Lippert F.K. Smartphone activation of citizen responders to facilitate defibrillation in out-of-hospital cardiac arrest. J Am Coll Cardiol. 2020;76:43–53. doi: 10.1016/j.jacc.2020.04.073. [DOI] [PubMed] [Google Scholar]
- 2.Stecker E.C., Reinier K., Marijon E. Public health burden of sudden cardiac death in the United States. Circ Arrhythm Electrophysiol. 2014;7:212–217. doi: 10.1161/CIRCEP.113.001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benjamin E.J., Muntner P., Alonso A. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 4.Grasner J.T., Lefering R., Koster R.W. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Grasner J.T., Wnent J., Herlitz J. Survival after out-of-hospital cardiac arrest in Europe - Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 6.Cummins R.O., Eisenberg M.S., Hallstrom A.P., Litwin P.E. Survival of out-of-hospital cardiac arrest with early initiation of cardiopulmonary resuscitation. Am J Emer Med. 1985;3:114–119. doi: 10.1016/0735-6757(85)90032-4. [DOI] [PubMed] [Google Scholar]
- 7.Sasson C., Rogers M.A., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 8.Hallstrom A.P., Ornato J.P., Weisfeldt M. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 9.Brooks S.C., Simmons G., Worthington H., Bobrow B.J., Morrison L.J. The PulsePoint Respond mobile device application to crowdsource basic life support for patients with out-of-hospital cardiac arrest: challenges for optimal implementation. Resuscitation. 2016;98:20–26. doi: 10.1016/j.resuscitation.2015.09.392. [DOI] [PubMed] [Google Scholar]