Abstract
OBJECTIVE:
To develop an interfacility transfer handoff intervention by applying the person-based approach method.
METHODS:
We conducted a qualitative study that used nominal group technique (NGT) and focus groups to apply the person-based approach for intervention development. NGT methods were used to determine prioritized pediatric transfer handoff elements to design the initial intervention prototype. Five focus group sessions were then held to solicit feedback on the intervention, perceptions on implementing the intervention, and outcomes for evaluating the intervention. Data were analyzed by using content analysis. Iterative improvements were made to the intervention prototype as data emerged.
RESULTS:
Forty-two clinical providers in total participated in NGT and focus group sessions, including physicians, advanced practitioners, nurses, and a respiratory therapist. The initial intervention prototype was a handoff mnemonic tool, “SHARING” (short introduction, how the patient appeared, action taken, responses and results, interpretation, next steps, gather documents). Perceived benefits of the intervention included clarifying handoff expectations, reducing handoff deficits, supporting less experienced clinical providers, and setting the stage for ongoing effective communication. Outcomes perceived to be meaningful were related to triage appropriateness, workflow and use, and communication and information sharing. The final version of the intervention consisted of a SHARING reference card and a SHARING electronic medical record note template.
CONCLUSIONS:
Using qualitative methods to apply the person-based approach to intervention development, we developed a transfer handoff intervention. Future research is needed to examine impacts of this tool; outcomes can include those identified as meaningful by participants in our present study.
An estimated 80% of serious medical errors involve miscommunication between providers during patient handoffs.1 Handoffs, which are the transfer of care between health care providers, occur in multiple settings. Interfacility handoffs, such as the handoff during hospital-to-hospital patient transfers, involve information transmission between health care team members and disparate electronic medical records located at different facilities.
Previous research has identified that pediatric interfacility transfer verbal and written communication is often incomplete, and handoff deficits are associated with increased reported errors in care.2 Additionally, verbal communication during interfacility transfers can be a contentious process filled with conflict.3,4 Standardizing the transfer communication process with a uniform handoff tool is one intervention strategy to address these challenges.3,5,6
Previous intervention implementations of standardized handoff processes have successfully decreased adverse events and medical errors.7,8 For example, the I-PASS (illness severity, patient summary, action list, situation awareness and contingency planning, synthesis by receiver) program, which includes a standardized handoff mnemonic, has been shown to decrease preventable medical errors by 30%.7 I-PASS was designed and tested for intrafacility handoffs rather than interfacility handoffs. In fact, the body of literature on handoff interventions, in general, is focused on intrafacility transfer handoffs.9 Because of inherent differences between intrafacility and interfacility communication, the intrafacility handoff interventions are not directly applicable to interfacility transfers. Handoff intervention development for interfacility transfers would thus address an important need.
The person-based approach is a systematic method that can be used in the early stages of intervention development to enhance the intervention’s acceptability and feasibility.10,11 Using iterative qualitative methods, the person-based approach ensures that the development process is grounded in the perspectives of the people who will use the intervention.11
Our objective was to optimize the potential uptake and effectiveness of an interfacility handoff intervention by applying the person-based approach to understand strategies for successful implementation, elicit meaningful outcomes for evaluation, and develop a handoff tool. We describe the development of the SHARING (short introduction, how the patient appeared, action taken, responses and results, interpretation, next steps, gather documents) handoff tool, an intervention designed to support effective pediatric interfacility verbal and written transfer communication between physicians.
Methods
Overview
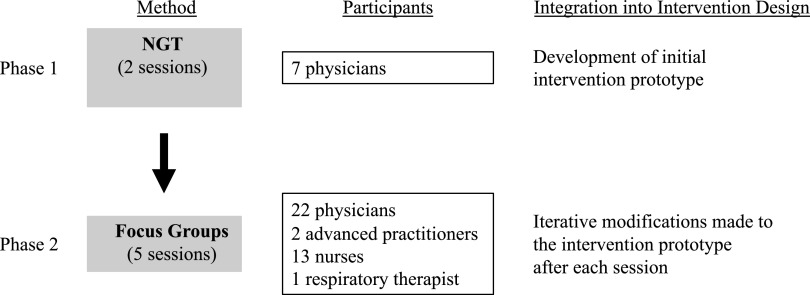
We conducted a 2-phased qualitative study that integrated core elements of the person-based approach, focusing on the intervention planning and design stages.11 Figure 1 shows an overview of the intervention development process. For intervention planning, phase 1 used nominal group technique (NGT)12,13 to elucidate referring and receiving physicians’ perceptions on how to standardize pediatric interfacility transfer handoffs. The NGT data informed the design of the initial intervention prototype. Subsequently, in phase 2, focus groups were conducted with multidisciplinary health care providers to review the intervention prototype and gather in-depth understanding of clinical providers’ perspectives on the key issues, needs, and challenges the intervention must address.10,11 The University of California, Davis Institutional Review Board determined this study to be not human subjects research.
FIGURE 1.
Overview of the intervention development process.
Study Population and Setting
We used purposive sampling14 to recruit English-speaking clinical providers representing 6 different hospitals, diverse provider types, and diverse clinical settings. Participants were identified through suggestions from our children’s hospital providers and Northern California community hospital site leads and were recruited via e-mail. Eligible participants had experienced being a referring or receiving provider for pediatric patients during interfacility transfers. Demographic information, including sex, age, provider type, clinical work setting, referring versus receiving role, and frequency of transferring pediatric patients, was collected.
The receiving hospital was a 121-bed, quaternary-care children’s hospital in Northern California. This hospital is the referral center for children across a 33-county region covering 65 000 square miles and serving >1 million children.15 The hospital receives transfers from >130 emergency departments and hospitals in the region and accepts >2500 pediatric patients annually as transfers.
Phase 1: NGT
Data Collection
Two NGT sessions were conducted in person with 7 pediatric physician stakeholders (Table 1) to solicit input on prioritized verbal and written key elements, respectively, that should be included in a standardized transfer handoff. NGT participants were physicians because physicians were the intended users of the handoff intervention. Each NGT session consisted of the 4 sequential steps of NGT: silent generation of ideas, sharing ideas in round-robin fashion, discussion of the list of ideas, and ranking ideas from the list.12,13 These sessions occurred consecutively, whereby 2 sessions were held back to back over a total duration of 120 minutes. Participants answered the question, “What are the key elements that should be included in the verbal or written handoff during a pediatric interfacility transfer?” Sessions were facilitated by 2 researchers with previous experience facilitating NGT sessions. A separate individual served as a notetaker to document field notes during each session.
TABLE 1.
Clinical Provider Participants’ Characteristics
| N (%) | |
|---|---|
| Sex | |
| Male | 15 (35.7) |
| Female | 27 (64.3) |
| Age, y | |
| ≤29 | 2 (4.8) |
| 30–44 | 20 (47.6) |
| 45–66 | 12 (28.6) |
| 67+ | 1 (2.4) |
| Unknown | 7 (16.7) |
| Provider type | |
| Physician | 26 (61.9) |
| Nurse practitioner or physician assistant | 2 (4.8) |
| Nurse | 13 (31.0) |
| Respiratory therapist | 1 (2.4) |
| Clinical setting | |
| PICU | 5 (11.9) |
| Emergency medicine | 22 (52.4) |
| Pediatric wards | 8 (19.0) |
| Newborn nursery or NICU | 3 (7.1) |
| Other or multiple settings | 4 (9.5) |
| Transfer role | |
| Exclusively or almost exclusively refer | 14 (33.3) |
| Refer and accept | 14 (33.3) |
| Exclusively or almost exclusively accept | 14 (33.3) |
| Frequency of referring or accepting pediatric patients | |
| Multiple times per day | 8 (19.0) |
| Most days | 4 (9.5) |
| Some days | 29 (69.0) |
| Almost never | 1 (2.4) |
| Never | 0 (0.0) |
There were 3 individuals who participated in both the NGT sessions and a focus group; their demographics are only listed once in the table.
Analysis
NGT numeric ranking methods were used to determine prioritized key elements.12,13 The list of prioritized key elements was presented by e-mail to all NGT study participants to solicit feedback as a form of member checking.16 NGT prioritized key elements and field notes were reviewed to develop the initial intervention prototype.
Phase 2: Focus Groups
Data Collection
A focus group question guide was developed, and field notes from the NGT sessions were reviewed to refine these questions. The questions broadly solicited stakeholders’ reactions to the preliminary handoff intervention, perceptions of facilitators of and barriers to implementing the intervention, and meaningful outcomes for evaluating the intervention (Supplemental Information).
Five focus group sessions were held with 22 physicians, 2 advanced practitioners, 13 nurses, and 1 respiratory therapist (Table 1). Three sessions used videoconferencing, and 2 sessions were in person. We included both physician and nonphysician clinical providers in the focus group phase on the basis of feedback that our handoff intervention might be a useful intervention for other provider types in addition to physicians. Focus group size ranged from 4 to 13 individuals. All NGT participants were invited to participate in a focus group; 3 of the NGT participants agreed and thus also participated in a focus group. Participants were purposefully assigned to 1 of 5 focus group sessions to maximize each group’s diversity with regard to specialties and role. One researcher facilitated the focus group; another researcher maintained field notes with contextual observations. Focus group sessions were audio recorded, transcribed, and deidentified.
Analysis
Data were analyzed by using content analysis. Three researchers independently performed individual memo writing and open coding of the transcripts. The team met to discuss the results, compare codes, and distill open-coding results into categories. The team reviewed the coded data to identify major categories and refine our handoff intervention prototype. We then solicited feedback on the preliminary categories and intervention prototype to obtain respondent transactional validation from the focus group participants by e-mail.16 To ensure trustworthiness, additional data validation occurred through investigator triangulation.17 The qualitative analysis team consisted of a pediatrician who worked at a referring hospital that sometimes receives pediatric patient transfers, a pediatrician who worked at a receiving hospital, and a clinical research associate. We used ATLAS.ti to organize and store coding and data analysis.18
Results
The NGT top key elements, in order of importance, for the verbal handoff were brief patient introduction, physical examination, interventions and response, questions and clarifications, and assessment and/or differential. The top prioritized key elements, in order of importance, for the written handoff were written summary, laboratories and studies, medications, images, and contact information. During member checking, respondents agreed with the list of prioritized key elements.
Integration Into Intervention Planning
Informed by these NGT data, we developed the initial intervention prototype. This prototype consisted of the mnemonic “SHARING.” The decision to use a mnemonic for the handoff intervention was based on perceptions shared by NGT participants during the discussion step and supportive evidence from existing handoff literature.7,8,19
Focus Groups
We developed 3 main categories and 11 subcategories from the transcripts that pertained to the handoff intervention’s benefits, implementation strategies, and evaluation. These are explored below with representative quotes in Table 2.
TABLE 2.
Exemplary Quotes Supporting the Categories
| Category | Subcategory | Quote |
|---|---|---|
| Benefits of the handoff intervention | Clarifying expectations around handoff elements | “The other thing I think is helpful is even if this doesn’t get used every time, the education piece, that, ‘Hey, the accepting doc actually does want to know about the lines…and I suspect you guys don’t know that.’ So kind of knowing that there are some pieces we want to hear they may incorporate that into their usual flow.” |
| Reducing patient clinical information handoff deficits | “It reminds you to be more complete because this is a process fraught with pitfalls, transferring these really sick kids. So, I do think it adds a nice framework for that handoff. These handoffs are super high risk.” | |
| Supporting less experienced providers | “I think it is important to remember who it is that’s actually making the referrals, and there are a lot of people who have a lot less experience … [The handoff tool is] important for those folks who aren’t transferring as often.” | |
| Setting the stage for ongoing effective communication | “When my mom, who can’t travel because she’s having a postpartum hemorrhage and has to stay in our facility, I know you guys call her, but I don’t know when, or why, or when that’s going to happen, and I’d love to be able to understand when I’m going to hear something or when the parent is going to hear something, when parents and children are separated. So having a reminder for a plan for that would be fantastic.” | |
| Strategies for successful implementation | Permitting flexibility in use | “My notes are almost never done before the end of my shift … Putting a fax number there where we can fax it, try to get it done in the next h or so and get it faxed over to you guys, just some way to get that to you quickly…maybe with that preferred way to communicate updates from there, a way to communicate or to send over a transfer summary that’s not yet completed or whatever.” |
| Integrating into the electronic medical record | “If you were able to operationalize this note in [the] EMR, that sort of gets the transfer center on board. And then, the conversation [is] documented with the accepting physician.” | |
| Being a receiver-driven process | “Having the receiving clinician being the one driving it, I think that’s probably going to be your easiest way to implement it because you can train everybody at [the receiving hospital]. There’s much less people that are receiving than are transferring.” | |
| Meaningful outcome measures | Triage appropriateness: level of care and preparedness | “Did your clinical impression of the patient who arrived, did that match what you received over reports? ... I think that a good report will result in the accepting doctor getting a patient that they were mentally and physically prepared for, like with team members, tubes, lines.” |
| Triage appropriateness: necessity of transfer | “Transferring patients is a big deal for the patient’s family as well, kind of taking them out of their community. And knowing that we didn’t shift them in the middle of the night just to be discharged from the ED is, I think, good information to know as well.” | |
| Workflow and use | “The other thing I keep thinking about is, ideally, this [handoff mnemonic] would improve efficiency so that not every provider the patient sees is asking the exact same questions over again.” | |
| Communication and information sharing | “That people are communicated with appropriately…that the parents know what to expect a little bit when they come [to the posttransfer hospital].” |
ED, emergency department; EMR, electronic medical record.
Category 1: Benefits of the Handoff Intervention
Clarifying Expectations Around Handoff Elements
A perceived benefit of the handoff intervention was clarifying expectations for the individuals involved in the handoff. Receiving providers reported that referring providers frequently omit clinical information that is needed to remotely understand the medical needs of the patient. Participants stated that standardization would inform the referring providers what information is desired by the receiving providers.
Reducing Patient Clinical Information Handoff Deficits
Referring and receiving participants reported that handoffs are fraught with information gaps. Such handoff deficits impede the receiving hospital’s ability to prepare appropriate staffing, medications, and equipment. Additionally, necessary clinical documents, such as the transfer summary or images on discs, are missing during patient transfers. Participants thought this intervention was a solution to these issues by reminding providers to conduct more complete verbal and written handoffs.
Supporting Less Experienced Providers
Although some stakeholders reported the intervention might not be necessary for more experienced providers, others disagreed and felt it would be beneficial to all. However, stakeholders unanimously expressed the intervention would be particularly useful for providers with less experience. Participants measured experience in years in practice, pediatric encounter volume, and transfer frequency.
Setting the Stage for Ongoing Effective Communication
The majority of participants reported that their favorite aspect of the intervention was that it promotes users establishing plans for future communication. They stated that the importance of communicating plans was in providing updates to one another and providing phone numbers to facilitate that process. Stakeholders also talked about communicating updates to families, particularly when family members are not with their transferred children. Lastly, stakeholders remarked the intervention should include a reminder to clarify the family’s understanding and expectations to ensure that families are informed and have realistic expectations.
Category 2: Strategies for Successful Implementation of the Handoff Intervention
Permitting Flexibility in Use
All stakeholders emphasized strongly that the handoff intervention needed to be easily integrated into the workflow. They wanted a brief reference tool that permitted flexibility in use. Some stakeholders commented that different hospitals, with different workflows and resources, might want a clerk to communicate some of the mnemonic elements.
Integrating Into the Electronic Medical Record
One popular strategy suggested was to integrate the handoff intervention into the receiving hospital’s electronic medical record. Stakeholders talked of using a template note with the mnemonic components in the patient’s electronic chart so that the information could be easily documented, shared, and stored. Participants shared that, in doing so, families might not have to answer the same questions repeatedly, and there might be less decay of information transmission when multiple handoffs are involved.
Being a Receiver-Driven Process
Although stakeholders discussed the importance of broadly educating all potential users of the handoff intervention, the majority of stakeholders thought implementation of the intervention needed to be a receiver-driven process. The referring providers should have access to the handoff mnemonic and know to use it; however, stakeholders believed the receiving providers would likely be more motivated and able to promote adoption of the intervention.
Category 3: Meaningful Outcomes the Handoff Intervention Should Address
Triage Appropriateness: Level of Care and Preparedness
Repeatedly, stakeholders expressed the importance of addressing triage appropriateness. Referring and receiving participants highlighted how important it was that patients arrived to the appropriate level of care at the posttransfer hospital. The phrase “arrived as billed” was frequently used. Participants explained that arriving as billed helps ensure that the receiving providers are prepared to care for the patient on arrival. Preparedness included being mentally prepared as well as prepared with the necessary resources or equipment.
Triage Appropriateness: Necessity of Transfer
Another valued outcome was the necessity of transfer. Stakeholders explained how they did not want to transfer a patient unless it was necessary, sharing that transferring a pediatric patient imposes significant burdens on and distress to the family.
Workflow and Use
Stakeholders stated that pediatric transfers that are conducted efficiently drive provider satisfaction. Referring and receiving providers wanted to have timely transfers without delays in getting the patient to the posttransfer hospital. Stakeholders explained the importance of receiving all necessary documents (especially laboratory results and images on discs) to avoid repeating unnecessary tests. Another important aspect of not duplicating work was not repeating the same questions to families.
Communication and Information Sharing
Referring providers, particularly referring physicians, prioritized feedback and updates as a meaningful outcome. They wanted to receive follow-up information about every transfer they send from their emergency department. They stated that feedback could provide opportunities to learn and adjust practices. Updates could provide closure. Receiving providers wanted families of transferred pediatric patients to have appropriate understanding and expectations on arrival to the posttransfer hospital.
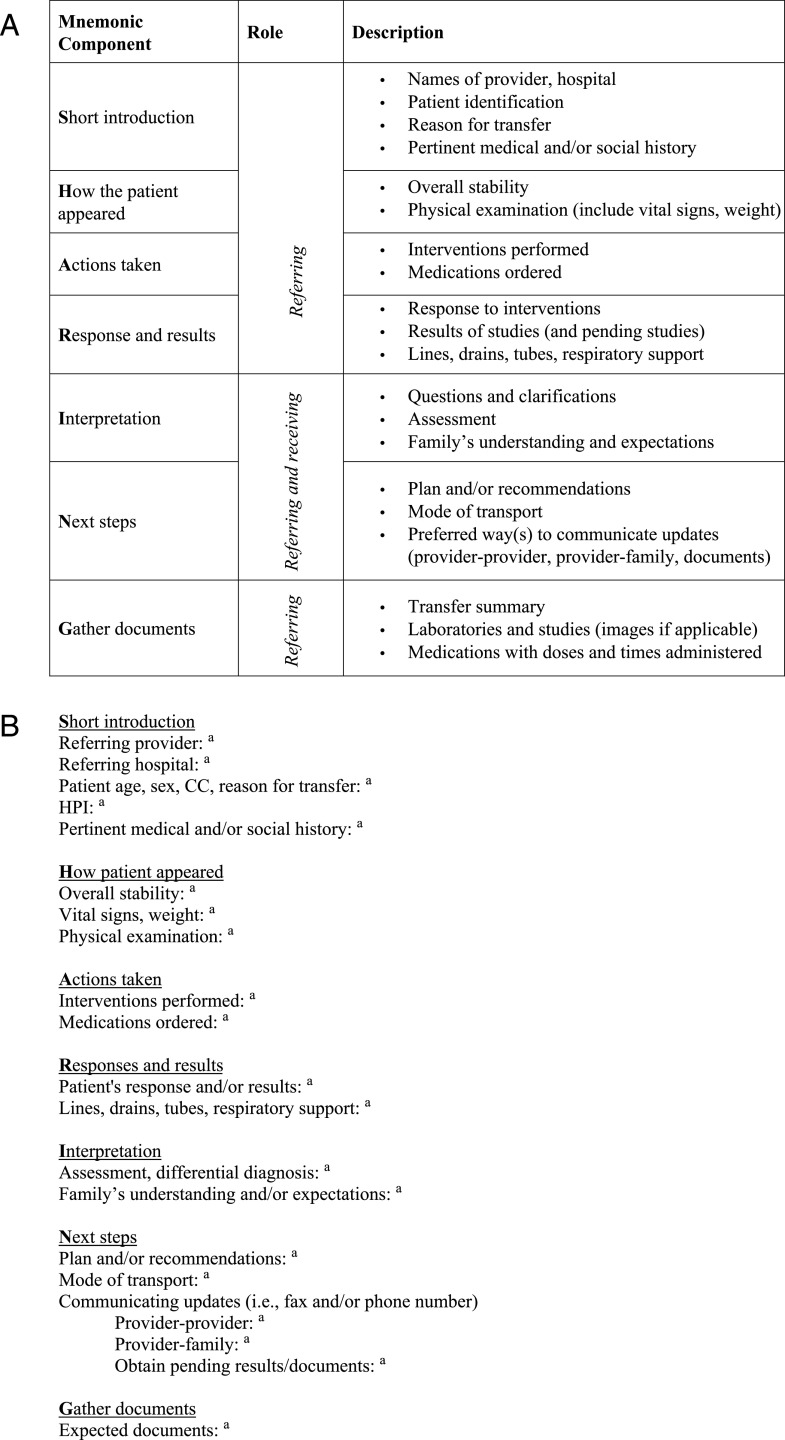
Integration Into Intervention Design
Informed by the focus group data, minor iterative modifications were made to the intervention prototype. These changes included removing or combining items in the description section of individual mnemonic components to simplify and shorten the descriptions. The order of items within each component was also adjusted. The initial intervention prototype had footnotes with additional handoff elements for specific patient populations (eg, neonates), but these footnotes were perceived to be unnecessary and thus removed. Importantly, the last 2 focus groups responded favorably to the intervention prototype and suggested no further modifications.
As shown in Fig 2, the final intervention consists of a reference card and an electronic medical record note template with the SHARING mnemonic.
FIGURE 2.
A, SHARING reference card for the transfer handoff. B, SHARING electronic medical record note template for the transfer handoff. a Required field for note writer. CC, chief complaint; HPI, history of present illness.
Discussion
This explorative qualitative study applied the person-based approach method to the early stages of developing a handoff intervention: the “SHARING” mnemonic tool. This study expanded our understanding of what key elements should be included in a standardized transfer handoff. We also gained in-depth understanding of the benefits of our proposed handoff intervention, strategies for its successful implementation, and meaningful outcomes to use when evaluating it. Importantly, these lessons learned came from the perspectives of the potential users of the intervention, and these data were iteratively integrated into the planning and design of our handoff intervention.
The development processes of previous handoff interventions have been previously described in the literature.20–22 To our knowledge, this is the first published application of the person-based approach to the development of a handoff intervention. We anticipate that this present description of the intervention planning and design process helps other researchers identify and incorporate this useful systematic method. Increased adoption of the person-based approach among intervention developers has the potential to increase the acceptability, feasibility, and impact of interventions.
Additional stages of the person-based approach are still needed to further develop the SHARING handoff intervention. Next steps will include think-aloud interviews and intervention field testing. Future adaptations to the intervention might be needed as we proceed with ongoing intervention development stages. Subsequently, the SHARING handoff intervention needs to be tested to determine its impact on outcomes. When examining this handoff intervention, we suggest using the meaningful outcomes identified in our study, which are related to triage appropriateness, workflow and use, and communication and information sharing. By measuring such outcomes when studying pediatric transfers, the research will be more relevant to the individuals using the intervention for the transfer process.
This study has several limitations. Transferability is limited by use of a single receiving facility. However, the referring physicians, without being prompted to do so, shared experiences and perceptions involving other receiving facilities. Results of this study were informed by only clinical provider participants. Although the participants represented a diverse group of specialties, this study did not include input from other individuals involved in the transfer process, such as patients and families. However, the participants in this study were chosen to represent the intended users of the intervention. Physicians represented a disproportionately high number of participants. Therefore, future steps of intervention development, such as think-aloud interviews and field testing, might result in significant adaptations to the intervention when applied to nonphysician users. Stakeholders in this study could have recall bias. Individuals who agreed to be in this study could also have atypical perceptions because of unusually negative or positive transfer experiences. This handoff intervention is designed for use during the initial handoff communication; however, subsequent handoff communication (eg, updates) might also benefit from standardization but was not included in this iteration of development. Despite these limitations, our study provided insight into referring and receiving provider perceptions on standardization of pediatric interfacility transfer handoffs.
Conclusions
The application of the person-based approach to the planning and design of our handoff intervention resulted in the development of a novel handoff intervention that was iteratively refined in response to needs and challenges identified from clinical providers’ perspectives. Future research is needed to examine the impacts of this or similar handoff tools; outcomes can include those perceived to be meaningful by participants in our present study.
Footnotes
Dr Rosenthal conceptualized the study design, facilitated the data collection sessions, analyzed and interpreted the data, and drafted and revised the manuscript; Ms Sauers-Ford assisted with the conceptualization of the study design, facilitated the data collection sessions, analyzed and interpreted the data, and revised the manuscript; Dr Hamline analyzed and interpreted the data and revised the manuscript; Drs Natale and Marcin assisted with interpretation of the data and revised the manuscript; Dr Li provided oversight for the analysis and interpretation of the data and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Center for Advancing Translational Sciences of National Institutes of Health (grant UL1 TR001860 and linked award KL2 TR001859), a University of California, Davis Academic Senate New Research Grant, and a Children’s Miracle Network Research Award. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health; University of California, Davis Academic Senate; or Children’s Miracle Network. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.The Joint Commission. Joint Commission Center for Transforming Healthcare releases targeted solutions tool for hand-off communications. 2012. Available at: https://www.jointcommission.org/assets/1/6/tst_hoc_persp_08_12.pdf. Accessed August 31, 2018
- 2.Rosenthal JL, Romano PS, Kokroko J, Gu W, Okumura MJ. Receiving providers’ perceptions on information transmission during interfacility transfers to general pediatric floors. Hosp Pediatr. 2017;7(6):335–343 [DOI] [PubMed] [Google Scholar]
- 3.Rosenthal JL, Okumura MJ, Hernandez L, Li ST, Rehm RS. Interfacility transfers to general pediatric floors: a qualitative study exploring the role of communication. Acad Pediatr. 2016;16(7):692–699 [DOI] [PubMed] [Google Scholar]
- 4.Bosk EA, Veinot T, Iwashyna TJ. Which patients and where: a qualitative study of patient transfers from community hospitals. Med Care. 2011;49(6):592–598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jewell JA; Committee on Hospital Care. Standardization of inpatient handoff communication. Pediatrics. 2016;138(5):e20162681. [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics Committee on Pediatric Emergency Medicine American College of Emergency Physicians Pediatric Emergency Medicine Committee Emergency Nurses Association Pediatric Committee. Handoffs: transitions of care for children in the emergency department. Pediatrics. 2016;138(5):e20162680. [DOI] [PubMed] [Google Scholar]
- 7.Starmer AJ, Spector ND, Srivastava R, et al. ; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–1812 [DOI] [PubMed] [Google Scholar]
- 8.Benjamin MF, Hargrave S, Nether K. Using the targeted solutions tool® to improve emergency department handoffs in a community hospital. Jt Comm J Qual Patient Saf. 2016;42(3):107–118 [DOI] [PubMed] [Google Scholar]
- 9.Rosenthal JL, Doiron R, Haynes SC, Daniels B, Li ST. The effectiveness of standardized handoff tool interventions during inter- and intra-facility care transitions on patient-related outcomes: a systematic review. Am J Med Qual. 2018;33(2):193–206 [DOI] [PubMed] [Google Scholar]
- 10.Yardley L, Ainsworth B, Arden-Close E, Muller I. The person-based approach to enhancing the acceptability and feasibility of interventions. Pilot Feasibility Stud. 2015;1(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yardley L, Morrison L, Bradbury K, Muller I. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res. 2015;17(1):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McMillan SS, Kelly F, Sav A, et al. Using the nominal group technique: how to analyse across multiple groups. Health Serv Outcomes Res Methodol. 2014;14(3):92–108 [Google Scholar]
- 13.Potter M, Gordon S, Hamer P. The nominal group technique: a useful consensus methodology in physiotherapy research. N Z J Physiother. 2004;32:126–130 [Google Scholar]
- 14.Tongco MDC. Purposive sampling as a tool for informant selection. Ethnobot Res Appl. 2007;5:147–158 [Google Scholar]
- 15.Dayal P, Hojman NM, Kissee JL, et al. Impact of telemedicine on severity of illness and outcomes among children transferred from referring emergency departments to a children’s hospital PICU. Pediatr Crit Care Med. 2016;17(6):516–521 [DOI] [PubMed] [Google Scholar]
- 16.Cho J, Trent A. Validity in qualitative research revisited. Qual Res. 2006;6(3):319–340 [Google Scholar]
- 17.Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res. 1999;34(5 pt 2):1189–1208 [PMC free article] [PubMed] [Google Scholar]
- 18.ATLAS.ti Scientific Software Development GmbH. Version 7 [computer software]. Berlin, Germany: Available at: https://atlasti.com/ [Google Scholar]
- 19.Alert SE. Inadequate hand-off communication. Sentinel Event Alert. 2017;(58):1–6 [PubMed] [Google Scholar]
- 20.Starmer AJ, O’Toole JK, Rosenbluth G, et al. ; I-PASS Study Education Executive Committee. Development, implementation, and dissemination of the I-PASS handoff curriculum: a multisite educational intervention to improve patient handoffs. Acad Med. 2014;89(6):876–884 [DOI] [PubMed] [Google Scholar]
- 21.Moy NY, Lee SJ, Chan T, et al. Development and sustainability of an inpatient-to-outpatient discharge handoff tool: a quality improvement project. Jt Comm J Qual Patient Saf. 2014;40(5):219–227 [DOI] [PubMed] [Google Scholar]
- 22.Goldsmith D, Boomhower M, Lancaster DR, et al. Development of a nursing handoff tool: a web-based application to enhance patient safety. In: Proceedings from the AMIA Annual Symposium Proceedings. November 13, 2010 2010:256–260 [PMC free article] [PubMed] [Google Scholar]