Abstract
Objective
To test the efficacy of an innovative coronavirus disease 2019 (COVID-19) preoperative triage protocol as a way to gradually reopen and ramp-up elective surgeries.
Patients and Methods
We reviewed clinical, radiographic, and laboratory data for all patients who underwent surgery within the neurosurgery department from March 26 through April 22, 2020. We collected data on demographic information, comorbidities, preoperative COVID-19 test results, whether COVID-19 respiratory or other symptoms were developed during hospitalization, hospital length of stay, discharge disposition, and postoperative COVID-19 test results.
Results
Using a combination of both preoperative outpatient COVID-19 drive-through and inpatient testing to obtain surgical clearance with selected telemedicine evaluations, 103 nonelective neurosurgical procedures were performed in 102 patients. No patients tested positive for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) 48 hours before surgery. None of the patients developed any COVID-19 symptoms during their hospitalization or were readmitted to our emergency department postoperatively for COVID-19 symptoms.
Conclusion
We describe a multifaceted preoperative triage protocol for safely performing nonelective neurosurgical procedures during the COVID-19 pandemic, which could help other neurosurgical departments and hospitals minimize coronavirus exposure for patients and health care workers. We believe this triage strategy could be implemented at other centers to gradually restart a process toward elective surgeries in a safe way.
Abbreviations and Acronyms: COVID-19, coronavirus disease 2019; ED, emergency department; EMR, electronic medical record; PUI, patient under investigation; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
As the novel coronavirus (severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]) spread across the globe, the coronavirus disease 2019 (COVID-19) pandemic has severely affected all aspects of society.1,2 The first confirmed case of COVID-19 in the United States was reported on January 20, 2020. The virus spread rapidly across all 50 states, and on March 13, the American College of Surgeons with the Surgeon General and Centers for Medicare & Medicaid Services recommended the cessation of elective surgeries.3, 4, 5, 6
Hospitals across the United States implemented several measures, such as temperature checks for employees and “no-visitor policies” for patients, to limit cross-infection between patients and health care workers. In parallel, elective surgeries that could be postponed for 2 to 3 months were rescheduled to focus on surge projections of patients with COVID-19, free up available hospital and intensive care unit bed capacity, and minimize exposure risk for patients, caregivers, and health care workers. The consequence of canceling elective surgeries led to major revenue losses for many hospitals, followed by furloughing employees to reduce expenses. It is estimated that a quarter of rural hospital systems faced with the financial losses from COVID-19 are vulnerable to closure.7
Like many other surgical specialties during the COVID-19 pandemic, the neurosurgical practices were considerably affected by the various government mandates to stop elective surgeries. During the spring of 2020, under government stay-at-home orders, we observed a substantial drop in outpatient visits immediately followed by a downstream reduction in all categories of surgical procedures. Although the pandemic progressed across the globe, the need to treat certain urgent patients with neurosurgical conditions was recognized. This required physicians and hospital administrators to work together to manage the demands imposed by the COVID-19 government mandates and restrictions regarding elective surgery with the need to minimize the deterioration of patients without COVID-19. Examples of the latter in our neurosurgical practice include patients with brain tumors, cerebral edema, intracranial aneurysms, and acute large vessel occlusion stroke as well as patients with spinal conditions, at risk of progressive myelopathy.8, 9, 10 Therefore, the goal of this study was to report a preoperative surgical triage strategy instituted by Mayo Clinic, Jacksonville, Florida, with regard to safely performing nonelective neurosurgical procedures during the COVID-19 pandemic.
Patients and Methods
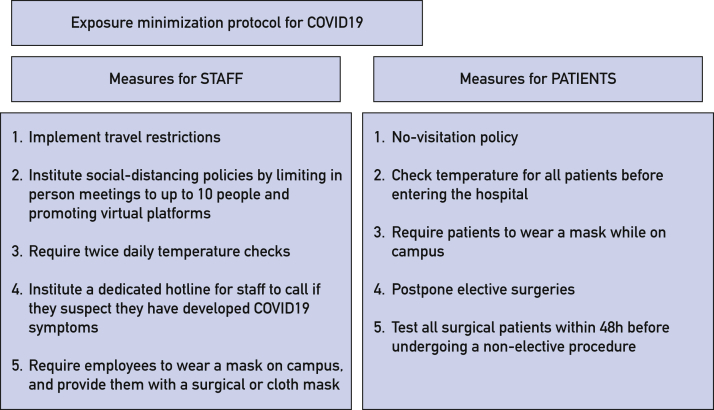
Exposure Minimization Protocol
Our latest update to the protocol, which was implemented on March 26, 2020, included both health care staff and patient safety measures (Figure 1). To minimize the risk of our staff being carriers of SARS-CoV-2, a travel ban was placed on physicians in early February 2020. Thermometers were issued to the entire health care workforce to perform self-monitoring twice a day for fever and report any COVID-19 symptoms to a dedicated hotline. Every building had a designated entrance for staff where screening checks were performed. Personnel at entrances asked staff whether they had any fever or COVID-19 symptoms before proceeding to work. In case the staff had forgotten to check their temperature, a laser surface thermometer was available to check the temperature noninvasively on the forehead. All employees were asked to wear some form of mask at work (cloth or surgical mask). Those involved in direct patient care were required to wear a surgical mask. Staff involved in high-risk aerosolizing procedures such as tracheal intubation/extubation or procedures that generate nasopharyngeal aerosols were required to use N95 respirators and eye protection. Widespread implementation of social distancing went into effect, which affected all administrative, educational, and research meetings, limiting in-person meetings to a maximum of 10 people at least 6 ft apart. Virtual meetings using videoconferencing platforms, for example, Zoom, replaced previous in-person meetings and educational conferences for residents, fellows, and staff. Clinic visits were transitioned to telemedicine, where possible, to further decrease the exposure.
Figure 1.
Protocol implemented by our institution to minimize the risk of exposure to severe acute respiratory syndrome coronavirus 2 for both patients and staff. COVID-19 = coronavirus disease 2019.
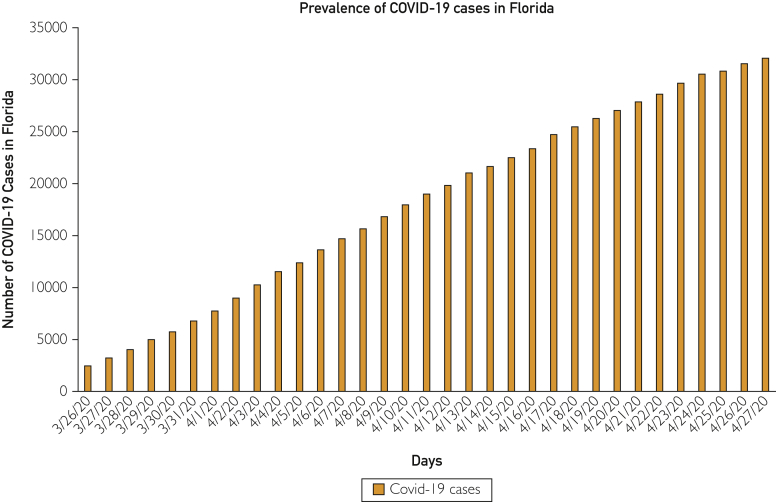
Mayo Clinic, Jacksonville, FL, created a COVID-19 triage drive-through testing facility circa March 26, 2020, that was modeled after Singapore11; Mayo Clinic, Rochester, Minnesota12; and other academic health care systems on the West Coast of the United States.13 The purpose of this strategy was to permit an urgent, safe surgical practice while balancing the dueling risks of patients deteriorating during government stay-at-home orders against the risks of cross-infecting other patients and health care workers when performing surgery in patients with unknown COVID-19 status. This effort was made while tracking rising SARS-CoV-2 cases occurring across the state of Florida during the COVID-19 pandemic (Figure 2).
Figure 2.
Prevalence of coronavirus disease 2019 (COVID-19) cases in Florida from March 26, 2020, through April 27, 2020. Source: Florida Department of Health (https://floridahealthcovid19.gov).
All patients had their temperature measured before entering any of the hospital buildings and were asked whether they had any of the COVID-19 symptoms. To minimize the risk of exposure to other patients and health care staff, a no-visitor policy was implemented for inpatients and for our emergency department (ED). For selected patients with difficulty communicating (eg, stroke), or international patients needing translation for home discharge needs, or other specialized needs (transplant education), one visitor was temporarily allowed to come to the clinic or the hospital with the patient. Patients were also required to wear masks while on campus.
Given the recommendation from the American College of Surgeons that all elective surgeries be postponed by 1 to 3 months, starting March 26, 2020, all patients scheduled for nonelective surgery were required to be tested first. A nasopharyngeal swab was collected within 48 hours of surgery at an outdoor drive-through testing location on our campus or in the ED if patients were admitted to the hospital. Testing was performed using the cobas SARS-CoV-2 assay (Roche Molecular System, Inc.) on the cobas 6800 System, and the test results were available within 24 hours. The outpatient drive-through system used an autonomous driving vehicle (Beep) to take samples from the collection site to the laboratory.14
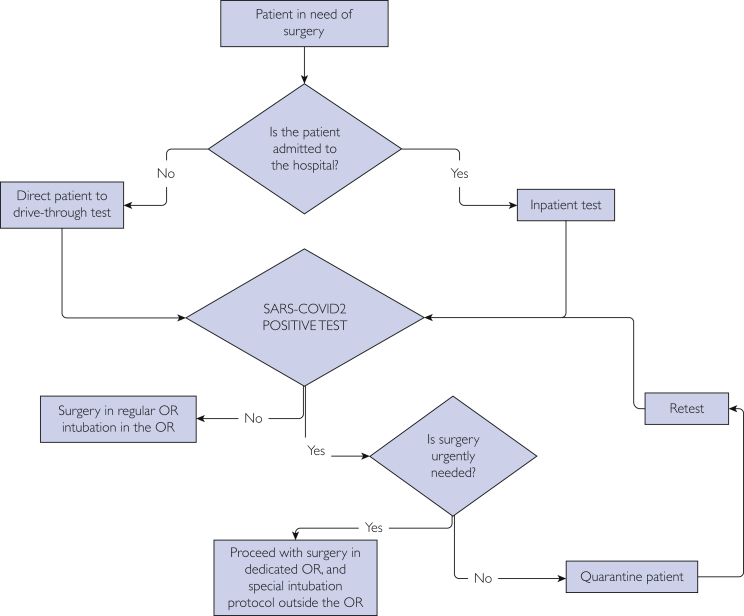
Subsequent management depended on the mode of presentation and results of COVID testing and was used to triage patients in need of nonelective surgery. Patients who were admitted to the hospital, either via our ED or as a direct transfer from elsewhere, were tested on arrival and were treated as presumed COVID-19 positive and patients under investigation (PUIs) until their test result was available.
Once patients were medically optimized for surgery and had a negative COVID-19 test result, standard operating procedures were implemented, including use of regular surgical masks, eye protection, handwashing or hand sanitization, and appropriate use of gloves and gowns.
Triage of COVID-positive patients was determined by whether surgery could be postponed safely when weighed against the risks of patient deterioration by delaying surgery. Patients who were COVID-19 positive and whose surgery could be delayed safely were quarantined and reevaluated later for operative candidacy by the team; duration of the postponement depended on the clinical stability of the patient (respiratory and cardiovascular) weighed against the risk of deterioration by delaying surgery (Figure 3).
Figure 3.
Testing protocol for patients in need of nonelective surgery. OR = operating room; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2.
For PUIs or COVID-positive patients in need of urgent/emergent surgery, the following strategy was used. Patients were taken to a negative pressure procedure room in which a specially trained anesthesiology team wearing full protective gear using powered air-purifying respirator equipment performed tracheal intubation and placed monitoring lines. Heat and moisture filters were placed on both the inspiratory and expiratory circuits of the anesthesia ventilator (Dräger Apollo). These heat and moisture filters screen out both bacteria and viruses to more than 99.99% level. Similarly, after the surgical procedure was complete, patients were taken to a negative pressure procedure room in which tracheal extubation was performed by the anesthesiology team wearing full protective gear. After tracheal intubation and extubation, an appropriate length of time was allowed for 99.9% of aerosols generated by these procedures to be eliminated. According to Centers for Disease Control and Prevention guidelines, this is dependent on the number of air exchanges per hour for a given procedure room. For example, a typical operating room has 20 air exchanges per hour and requires 21 minutes for 99.9% aerosol removal.15
Coronavirus Disease Intubation—Anesthesia Response Team and Virtual Reality Education Videos
A number of 360° immersive virtual reality donning, intubation, and doffing education videos were made and shared among anesthesiology and critical care staff. A dedicated negative pressure intensive care unit and ward were reserved for PUIs and COVID-positive patients.
Study Population, Demographic Information, and COVID-19 Status Information
All patients who had neurosurgery from March 26, when we started testing all surgical candidates for SARS-CoV-2, until April 22 were included in this study. From this time period, we found 102 patients who underwent 103 procedures (Table). After obtaining approval by our institutional review board (ID 18-003951), we collected clinical, laboratory, and radiographic data from the Epic (Epic Systems Corporation) electronic medical record (EMR). These data included demographic information, comorbidities, name/type of the procedure, diagnosis, time of the preoperative COVID-19 test, final test results as positive or negative, cancellation or postponement of surgery, whether patients developed any COVID-19 symptoms during hospitalization, hospital length of stay, mode of hospital admission (eg, ED and hospital-to-hospital transfer), discharge disposition, and postoperative COVID-19 test results.
Table.
Demographic and Clinical Characteristics of Patients
| Characteristic | Valueb |
|---|---|
| Median age (y) | 63 (53-71) |
| Male sex | 58 (57) |
| Comorbidity | |
| Hypertension | 59 (58) |
| Type 2 diabetes mellitus | 15 (15) |
| Obesity | 33 (32) |
| Coronary artery disease | 6 (6) |
| COPDa | 8 (8) |
| Type of admission | |
| From clinic | 99 (97) |
| From emergency department | 3 (3) |
| Preoperative positive COVIDa test result | 0 (0) |
| Median length of stay (d) | 2 (1-3) |
| Postoperative COVID symptoms | 0 (0) |
| Postoperative disposition | |
| Home | 93 (91) |
| Inpatient rehabilitation facility | 9 (9) |
COPD = chronic obstructive pulmonary disease; COVID = coronavirus disease.
Data are presented as median (interquartile range) or as No. (percentage).
Symptom Assessment
We retrospectively reviewed the EMR charts, looking for typical COVID-19 symptoms such as fever, cough, and shortness of breath as well as for atypical symptoms such as chills, malaise, myalgia, sore throat, runny nose, dizziness, diarrhea, and nausea and/or vomiting.16,17 Patients were considered COVID-19 symptom-free if they had none of the above-mentioned symptoms or if they had stable chronic symptoms (eg, chronic cough without recent worsening).
Statistical Analyses
Descriptive statistics were calculated for demographic and clinical factors by using the median as a measure of central tendency and the interquartile range as a measure of dispersion. All analyses were performed using SPSS version 21 (IBM Corporation).
Results
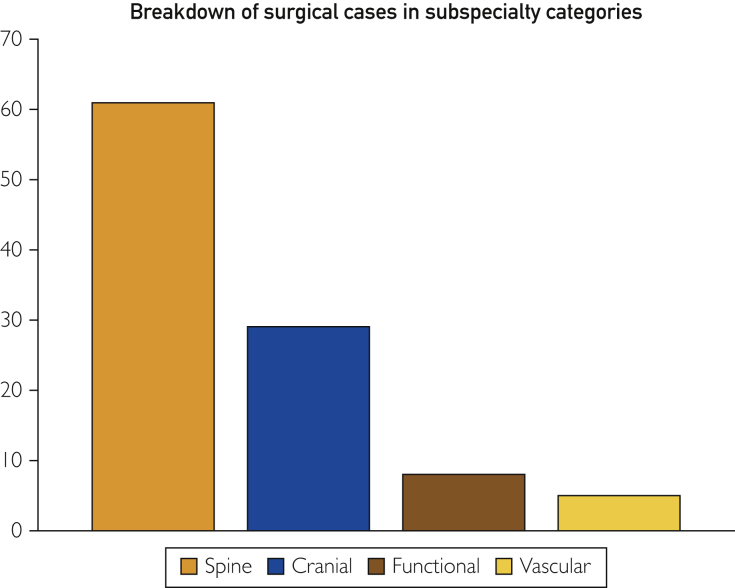
During a relatively short timeframe, we report that 103 nonelective surgeries were performed in the neurosurgery department at our institution in 102 patients between March 26, 2020, and April 22, 2020. Cases ranged from ruptured intracerebral aneurysm clipping to spine surgeries for patients with progressive myelopathy to craniotomies for patients with symptomatic brain tumors. Of the 103 surgeries, 61 (59%) were spine cases, 37 (61%) of which involved a fusion; 29 (28%) were cranial cases; 8 (8%) functional surgeries; and 5 (5%) vascular surgeries (Figure 4).
Figure 4.
Breakdown of surgical cases in subspecialty categories. y-axis: number of surgical cases
The median age of patients was 63 years, with an interquartile range of 53 to 71 years. Fifty-eight patients (57%) were male. Ninety-nine patients (97%) were direct admission from the clinic, while 3 (3%) came directly to our ED. Fifty-nine patients (58%) had hypertension; 15 (15%) had type 2 diabetes mellitus; 33 (32%) were obese; 6 (6%) had coronary artery disease; 8 (8%) had chronic obstructive pulmonary disease.
None of the surgeries had to be canceled or delayed because of the SARS-CoV-2 test. All 102 patients underwent the SARS-CoV-2 test within 48 hours before surgery, and 0 patients had a positive SARS-CoV-2 assay result. The median length of stay was 2 days, with an interquartile range of 1 to 3 days. None of the patients developed any COVID-19 symptoms during their hospitalization or were readmitted to the hospital because of COVID-19 symptoms. Ninety-three patients (91%) were discharged home, while 9 (9%) were discharged to an inpatient rehabilitation facility. Eight patients (8%) underwent a second SARS-CoV-2 test before discharge because of longer hospitalization or per patient’s request, and all 8 patients tested negative; 5 patients (5%) were tested after discharge at our drive-through facility, after meeting symptomatic criteria, and all 5 tested negative.
Discussion
In this study, 102 patients underwent nonelective neurosurgical operations during the COVID-19 pandemic. We found that the multifaceted strategy our center implemented focusing on preoperative screening was effective in minimizing the risk of exposure to COVID-19 to other patients and health care staff. We also note that none of these neurosurgical patients developed COVID-19 symptoms during their hospitalization, nor were they later admitted to the ED for COVID-19 symptoms postoperatively or had a positive postoperative COVID-19 test result. This likely reflects multiple other efforts at the national level by various government agencies, including stay-at-home orders, social distancing of 6 ft between people, smaller group sizes, and routine and repeated handwashing efforts.
After government agencies legislated that most US hospitals postpone elective surgery, hospitals and surgical departments faced the double-edged sword of huge reductions in revenue while struggling to pay for staff and overhead costs. A prolonged period without normal surgical volumes resulted in many hospital systems enacting salary reductions and furloughing staff. The COVID-19 pandemic forced a black swan (ie, unpredictable and sudden) organizational effect on hospitals and surgical teams to adapt rapidly to the loss of elective surgical volume amidst the need to respond to the potential surge in patients with COVID-19 and their needs.18 There were many lessons learned from the COVID-19 pandemic that required organizations and surgical teams to adapt quickly. One existential lesson was how to balance the reduction in elective surgery with a need to serve patients without COVID while maintaining economic viability in the face of a global pandemic. Such adaptations learned from the COVID-19 pandemic can also help prepare for future pandemics and similar surgical challenges. We acknowledge that one of the limitations of this work is that it is largely retrospective. We also recognize that some centers without a similar testing capacity would be unable to respond as nimbly as our organization without forcing significant delays in surgical care of patients with and without COVID alike. Clearly, from a US perspective, many patients incurred immeasurable suffering and harm as our health care systems struggled to cope with this unexpected catastrophe.19
Many lessons were learned that will become the new normal. Examples include the value of rapid and reliable preoperative testing with appropriate capacity; telemedicine visits with remote reviewing of imaging to prioritize urgency in operative case selection. Responding to the COVID-19 crisis required a proactive and iterative learning process. It required multidisciplinary teams working together to innovate and advance the science of medical delivery. At the start of the pandemic, when our testing capability was insufficient to test high volumes of surgical patients upfront, we performed symptom screening of patients with COVID-19 and tested moderate- to high-risk patients. As the scale of tests grew and turnaround time reduced to less than 24 hours, we were able to achieve universal clearance of outpatient surgical patients preoperatively and all patients admitted to the hospital.
Another limitation of our study is the fact that not all patients underwent a SARS-CoV-2 test postoperatively. However, to account for that, the EMR was reviewed for a 2-week period after surgery to see whether any patient complaining of symptoms associated with COVID-19 accessed our ED. If this were the case, our surgical team followed up with these patients via telephone or telemedicine visit to see if they became symptomatic. Repeat SARS-CoV-2 testing at the drive-through facility was ordered for any patient who met symptomatic criteria. Therefore, a limitation of our study is the fact that we were unable to detect patients that might have been infected but remained asymptomatic. The model we described and now propose also allows for a much more limited use of personal protective equipment by triaging patients on the basis of rapid preoperative COVID testing. This model can easily be duplicated elsewhere given the increasing availability of COVID-19 testing. We acknowledge that each state and each health care facility have different COVID-19 patient population pressures, personal protective equipment limitations, and testing capability.
As the United States starts to flatten the COVID-19 curve, states are looking into gradually lifting their COVID-19 restrictions on hospital care and business activity. This poses the dueling need to minimize cross-infection between healthy and COVID-19–positive patients and health care staff while not delaying urgent and elective surgical care while waiting for a vaccine or specific antiviral therapy. Our preliminary efforts may help other surgical departments move forward while the methods described here can undergo external validation. Our study, reporting the performance of 103 nonelective surgeries without patients contracting SARS-CoV-2, is a small but important victory in the right direction. Reopening of surgical practices will require an individualized approach, but the model described in this study would be a useful guideline for other surgical departments and institutions looking to restart their elective surgical program.
Conclusion
Despite considerable workforce and other challenges, we report a preoperative surgical clearance pathway to triage patients safely for nonelective surgeries during the COVID-19 pandemic. None of these patients or health care staff developed COVID-19 infection during the postoperative follow-up. As states lift restrictions imposed during the height of the COVID-19 pandemic, we propose a multifaceted approach using outpatient testing and telemedicine and a similar inpatient approach as a potential safe way to gradually restart elective surgery.
Acknowledgments
We would like to acknowledge Jorge Pascual, John Casler, and Chris Hasse for their contribution to this paper.
Footnotes
Potential Competing Interests: The authors report no competing interests.
References
- 1.Zhu N., Zhang D., Wang W., et al. China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P., Yang X.-L., Wang X.-G., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.COVID-19: recommendations for management of elective surgical procedures. American College of Surgeons website. https://www.facs.org/covid-19/clinical-guidance/elective-surgery
- 4.Stahel P.F. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. 2020;14(1):8. doi: 10.1186/s13037-020-00235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CMS Releases recommendations on adult elective surgeries, non-essential medical, surgical, and dental procedures during COVID-19 response. CMS.gov. https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental
- 6.ASA-APSF joint statement on non-urgent care during the COVID-19 outbreak. American Society of Anesthesiologists website. https://www.asahq.org/about-asa/newsroom/news-releases/2020/03/asa-apsf-joint-statement-on-non-urgent-care-during-the-covid-19-outbreak
- 7.O’Brien J. A quarter of rural hospitals at ‘high risk’ of closure, COVID-19 likely to make it worse. Healthleaders Media website. https://www.healthleadersmedia.com/finance/quarter-rural-hospitals-high-risk-closure-covid-19-likely-make-it-worse
- 8.Lee Z.D., Chyi Yeu D.L., Ang B.T., Ng W.H., Seow W.T. Editorial: COVID-19 and its impact on neurosurgery: our early experience in Singapore [published online ahead of print April 17, 2020] https://doi.org/10.3171/2020.4.JNS201026 J Neurosurg. [DOI] [PMC free article] [PubMed]
- 9.Ghogawala Z., Kurpad S., Falavigna A., et al. Editorial: COVID-19 and spinal surgery [published online ahead of print April 17, 2020] https://doi.org/10.3171/2020.4.SPINE20468 J Neurosurg Spine. [DOI] [PMC free article] [PubMed]
- 10.Ammar A., Stock A.D., Holland R., Gelfand Y., Altschul D. Managing a specialty service during the COVID-19 crisis: lessons from a New York City health system [published online ahead of print April 17, 2020] https://doi.org/10.1097/ACM.0000000000003440 Acad Med J Assoc Am Med Coll. [DOI] [PMC free article] [PubMed]
- 11.Drive-thru testing launched to stop coronavirus spread in South Korea | NBC News. https://www.youtube.com/watch?v=w_QMuLUoAAo
- 12.Mayo Clinic offers pre-screened patients drive-through specimen collection for COVID-19 testing. Mayo Clinic website. https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-offers-pre-screened-patients-drive-through-specimen-collection-for-covid-19-testing/
- 13.Drive-through medicine: drive-through triage template. Developed by Division of Emergency Medicine and Department of health Research & Policy, Stanford University. https://www.calhospitalprepare.org/sites/main/files/file-attachments/drive-throughtriage_county_template_11-23-2009.pdf
- 14.Autonomous shuttles help transport COVID-19 tests at Mayo Clinic in Florida. Mayo Clinic website. https://newsnetwork.mayoclinic.org/discussion/autonomous-shuttles-help-transport-covid-19-tests-at-mayo-clinic-in-jacksonville/
- 15.Appendix B. Air: Guidelines for environmental infection control in health-care facilities (2003). Centers for Disease Control and Prevention website. https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html
- 16.Guan W.-J., Ni Z.-Y., Hu Y., et al. China Medical Treatment Expert Group for Covid-19 Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen N., Zhou M., Dong X., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Is the COVID-19 outbreak a black swan or the new normal? MITSloan Management Review website. https://sloanreview.mit.edu/article/is-the-covid-19-outbreak-a-black-swan-or-the-new-normal/
- 19.Rosenbaum L. The untold toll—the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382(24):2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]