Highlights
-
•
Cancer patients face pressure from virus and tumor progression during COVID-19.
-
•
Ensuring that patients receive radiotherapy safely is particularly important.
-
•
With proper prevention and control measures, radiotherapy could be safely performed.
Keywords: COVID-19, Epidemic prevention and control, Radiotherapy, Radiotherapy center, Consensus
Abstract
After the outbreak of COVID-19, medical institutions in China and even around the world are facing unprecedented challenges. In order to minimize the adverse impact of this unexpected epidemic on patients who need radiotherapy, the expert group of our radiotherapy center immediately formulated comprehensive emergency plans and prevention and control measures, partitioned the work area, launched online staff training, and optimized the radiotherapy process after the outbreak, which provided a strong guarantee for the safe and orderly operation of our radiotherapy center and kept the infection rate to an extremely low level. We hope our experience could provide reference and suggestions for other medical institutions.
1. Introduction
The current outbreak of Coronavirus Disease 2019 (COVID-19) was first reported in Wuhan, China, in December 2019. It is caused by a virus named Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [1], [2], [3]. The recognized symptoms of infection range from asymptomatic to a mild respiratory illness without fever to the more severe manifestations. Diarrhea may also be among the complaints. As of March 3, there are 80,303 confirmed cases nationwide (including 6,806 severe cases), 47,506 patients cured and 2,948 deaths. A total of 538 confirmed cases have been reported to date in Sichuan Province.
Following the outbreak of COVID-19, medical institutions in China and around the world have faced unprecedented challenges. The composition of the radiotherapy centers staff is especially complicated because it is always one of the most densely populated places in a hospital. About 50% of patients with cancers need radiation therapy throughout their lifetime [4]. Since cancer patients may have even worse resistance to viruses, ensuring patients receive treatment in an organized and safe way during the COVID-19 epidemic is of great importance [5]. However, the complicated personnel structure including patients, caregivers, radiation therapists, physicists, oncologists, nurses, and other relevant staff, makes it harder to control for cross-infection risk during treatment. To resume normal treatment as soon as possible, a multidisciplinary group of experts from Sichuan Cancer Hospital set up guidelines for the precise prevention and control of COVID-19 in our radiotherapy center. Spring Festival this year was from January 24 to February 2, 2020. Our radiotherapy center has resumed work since January 30, 2020. As of March 3, more than 2,000 patients have received safe and orderly treatment.
2. Methods
At the beginning of the COVID-19 outbreak, a group of about 30 experts including experts in infection, radiotherapy, medical physics, nursing, therapists, etc. in our hospital convened an online meeting, to formulate emergency plans and prevention and control measures. The consensus was quickly formulated right by the end of January and published in the Chinese Journal of Cancer Control and Treatment on February 21st to be available to the whole country [6].
3. Results
3.1. Patient’s access to the hospital
During the COVID-19 outbreak, every patient needs to make an appointment via our official website or WeChat before coming to the hospital, and the instant registration feature was no more available. Patients can be accepted only under inpatient status, and the number of patients to be admitted is based on the number of available wards. To avoid admission of suspected patients, the patients are admitted only after the hospital perform a complete and detailed epidemiological investigation; therefore, outpatients cannot be accepted for radiotherapy.
Patients who did not complete radiotherapy before the Spring Festival received priority admission. Patients should not be accompanied by anyone. If it is indeed impossible for them to take care of themselves due to old age, poor physical condition, mobility difficulties, or critical illness, only one caregiver may stay in the ward. The caregivers have to wear masks and monitor their body temperature daily. Visits with patients are prohibited. Those patients without caregivers may have one companion visit at a fixed time every day. Visitors are strictly screened for temperature, contact history, and symptoms before entering the ward.
Patients need to perform hand hygiene disinfection and wear masks and overshoes correctly, every time they enter the radiotherapy center. Double temperature monitoring is performed in the ward and radiation center. Depending on the radiotherapy appointment system, the treatment time of patients is accurately controlled within 30 min. Patients in the waiting area are required to be more than 2 m each other. Non-essential companions are not permitted to enter the radiation center.
3.2. Completion of detailed epidemiological investigation before admission to hospital
The doctor in charge should contact the patient before admission by phone to understand their respiratory symptoms, such as temperature, cough, dyspnea, fatigue, and epidemiological history, whether they have ever been to Wuhan or surrounding areas, and so on. For highly suspected patients (such as those who have had contact with diagnosed COVID-19 patients), further examinations should be conducted in designated nearby hospitals and be reported to committees and local disease control centers. All patients need to have a chest CT scan and blood routine examination which includes the white blood cell count, lymphocyte count, etc, within seven days before being admitted to the hospital.
3.3. Psychological care
Science popularization and psychological consultation can stabilize patients’ emotions, actively guide patients, and reduce the impact of psychological factors. Because many work processes must be adjusted during the epidemic, patients should be clear about the changes. Staff should avoid centralized or face-to-face work if possible when educating staff on the epidemic and work processes.
3.4. Division of the working area into different security levels
To minimize the risk of cross-infection, radiotherapy centers should adjust entrances and exits to separate patient passages from medical staff passages and form a one-way channel in the internal area if possible. Our center is divided into four areas according to the flow of patients. Everyone can access the level I area, such as the central hall, which has an extremely high risk of cross-infection. Only patients and medical workers can access the level II area, such as the accelerator room, which has relatively less risk. The level III area, such as the operator room of the accelerator, is where medical staff go after contact with patients and is classified as intermediate risk. Level IV areas, such as the physical planning room and administrative offices, are clean and low-risk (Table 1).
Table 1.
Classification of different sections and corresponding disinfection methods.
| Section | Risk level | Disinfection method |
|---|---|---|
| Isolation waiting area | Level I | SD/Ventilation |
| Accelerator room | Level I | SD/Ventilation/AD |
| Accelerator operation room | Level II | SD/Ventilation |
| CT position (machine room) | Level I | SD/Ventilation/AD |
| CT position (operation room) | Level II | SD/Ventilation |
| Simulation (machine room) | Level I | SD/Ventilation/AD |
| Simulation (operation room) | Level II | SD/Ventilation |
| Mold room | Level I | SD/Ventilation/AD |
| Main entrance | Level I | SD/Ventilation/AD |
| Bathroom | Level I | SD/Ventilation/AD |
| Information office | Level III | SD/Ventilation |
| Physical planning room | Level IV | SD/Ventilation |
| Administrative office | Level IV | SD/Ventilation |
Note: SD = Surface disinfection; AD = Air disinfection.
3.5. Area disinfection and management
For Infrastructure and equipment, it is required to wipe the Level I area with 1,000 mg/L chlorine-containing disinfection solution, or 75% ethanol wipe disinfection for noncorrosive equipment. The Level II and III areas can be wiped and disinfected with 500 mg/L of chlorine-containing disinfectant or alcohol-containing disposable disinfection wipes, more than twice a day, or any time an area is contaminated. Whenever there are visible pollutants, first use disposable absorbent materials to remove the pollutants, and then routinely disinfect it.
In the public ground, staff should use 1,000 mg/L chlorine-containing disinfectant for the level I and level II areas and 500 mg/L chlorine-containing disinfectant for level III areas. Whenever there are visible pollutants, they should first use disposable absorbent materials to remove the pollutants and then routinely disinfect it, more than twice a day.
Air ventilation should be performed twice a day for at least 30 min throughout the area. In the operation room, can be used for periodic disinfection; ultraviolet radiation can be used for disinfection for over 60 min, twice a day.
All medical waste from the level I area should be considered infectious medical waste. Staff should strictly follow the Medical Waste Management Regulations and the Medical Waste Management Measures of Medical and Health Institutions. Disinfection and waste management should be supervised by a specialist.
To avoid any contact between people's hands and surfaces, paper handkerchiefs are placed where necessary (door handles, lift buttons etc.).
3.6. Protection of the workforce
To prevent infection among the staff, the hospital has established return to work procedures after the COVID-19 outbreak. The staff returning from Spring Festival with public transport (train, flights, etc.), or staff that had direct or indirect contact with persons potentially infected need to be quarantined at home for 14 days, monitoring the body temperature twice a day. Before they can return to work, staff must follow an online training course on the new procedures to be adopted and pass an examination to assess their understanding. The training should include the epidemiological history screening of patients, the seven steps for hand washing, the correct procedure for wearing masks, overshoes, protective dresses, protective measures in different areas, and adjusted work processes in different areas, etc. [7], [8] (Table 2). Staff is required to measure body temperature twice a day and report to the designated person; staff should avoid unnecessary physical contact, use internal phones, pagers, or cell-phones if possible; a minimum working distance of 2 m is recommended in working areas and no more than three persons are allowed in the same room. All the staff must follow basic protective measures following hand hygiene regulations and wearing surgical masks. In addition, i) staff in extremely high-risk areas (Level I)such as Linac, mold, CT, and simulation rooms, such as radiation therapists, should be also equipped with work clothes (washable uniforms), isolation gowns, work caps, isolation masks, latex gloves, and PE gloves; ii) Staff in high-risk areas (Level II) as the main hall, having themain dutyto measure the body temperature and to limit the number of patients in the waiting area, need also to wear work clothes, isolation gowns, work caps, latex gloves, and PE gloves; iii)staff in intermediate-risk (Level III) at the information desk should also wear work clothes, work caps, and latex gloves; iv)staff in the low-risk area (Level IV)such as administrative offices shallalso wear work clothes. In general, other staff entering a specific risk zone, should wear the appropriate equipment of the zone.
Table 2.
Protective equipment for medical staff of different risk levels.
| Risk level | Protective Equipment |
|---|---|
| Level I | Hand hygiene, surgical mask, work clothes, isolation gown, work cap, isolation mask, latex gloves, PE gloves |
| Level II | Hand hygiene, surgical mask, work clothes, isolation gown, work cap, latex gloves, PE gloves |
| Level III | Hand hygiene, surgical mask, work clothes, latex gloves |
| Level IV | Hand hygiene, surgical mask, work clothes |
3.7. Measures of prevention and control for the different radiotherapy procedures
In the mould room, the environment should be disinfected before the start of the day's work. Staff should use an air sterilizer 3 times a day for 2 h each time. The floor should be disinfected following recommendations of the level I area. Patients must be required to wear masks during the process. For head and neck cancer patients, the masks need to be removed, and a separate space must be maintained in the mask production area. During the process, direct contact and language exchange should be minimized as much as possible. Additionally, 75% of alcohol should be used to disinfect the bed before and after use. The thermoplastic mould should also be wiped and disinfected with 75% alcohol and stored in the right place. After the procedure, both patients and medical staff must perform hand hygiene.
The computed tomography scan is performed in the CT room. Dedicated CT are used for patients suspected to be infected. In this area, continuous air disinfection can be used during the procedures. Disposable sheets should be used and changed after each patient. The fixation device needs to be disinfected with 75% alcohol before and after use. It is recommended that staff use disposable PE gloves outside of their rubber gloves. PE gloves should be replaced and hand hygiene should be performed after each patient. Positioning lead beads are not recommended for repeated use without disinfection. When enhanced CT images are needed, an invasive procedure is performed. Staff should prepare the contrast medium syringe and disinfect the environment in the level I area before the work of the day commences.
The target contouring on the CT images and the treatment planning are performed by the staff in dedicated areas. There is no patient participation in these sessions. The process is mainly based on informational processes. The disinfection can refer to the level IV area.
The radiotherapy treatment is performed in the linac area. Through the information system, appointments are given to have no more than two patients in the waiting area. Patients in the waiting area are required to be protected, according to public protection, with an interval of more than 2 m. Disposable sheets should be used and changed after each patient. The fixation device needs to be disinfected with 75% alcohol before and after use. Staff should use disposable PE gloves outside of their rubber gloves. PE gloves should be replaced, and hand hygiene should be performed after each patient. The thermoplastic mould needs to be disinfected with 75% alcohol before and after use.
Some invasive or special fixed radiotherapy technologies, such as FRAXION fixed frame, ABC respiratory gating, and so on require radiotherapy devices to be in close contact with the mucous membrane (such as oral mucosa). This equipment should only be used once. The fixing device needs to be thoroughly disinfected and cleaned before and after use. When radiation therapy is performed under general anaesthesia environmental disinfection of the operating room (accelerator room or CT simulation room) must be strictly implemented. It should be disinfected following the level I area recommendations of 1000 mg/L chlorine-containing disinfectant.
Brachytherapy usually includes iridium and cobalt sources for cervical cancer, and some institutions carry out particle implantation. The brachytherapy room should be divided into different internal sections. Patients’ operating areas should be disinfected following the level I area. Intrusive appliances should be subjected to high-pressure disinfection by the disinfection supply center. The environment should be disinfected before the start of the day's work. Staff should use air sterilizers to sterilize the air 3 times a day for 2 h each time. At the same time, the ground should be disinfected in accordance with the level I area after each operation. The environmental disinfection of the brachytherapy room is the same as the CT simulation room. During brachytherapy, an appointment system should be strictly implemented to avoid patient physical contact. A nurse will guide patients into the treatment area for dressing, hand hygiene, and alcohol wipe disinfection. Patients who need bladder management should perform hand hygiene again before and after the operation. After the treatment is completed, the area where the patient is released should be disinfected in advance.
3.8. Emergency plan
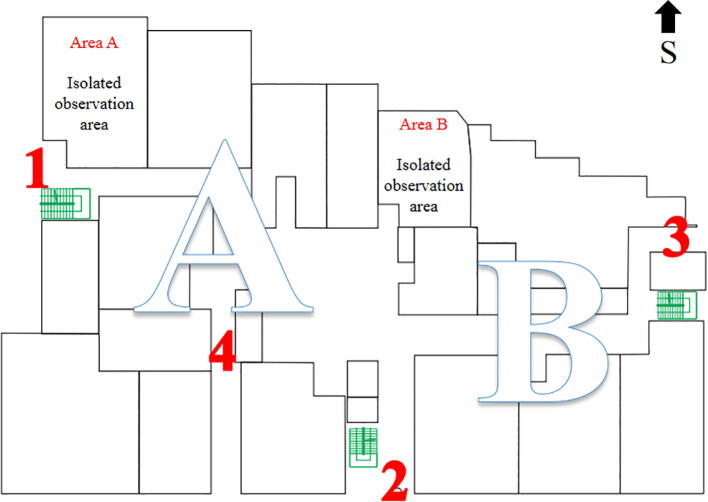
For patients starting the radiotherapy in good conditions and unexpectedly during the radiotherapy process are suspected to be infected, an emergency plan should be implemented immediately. Taking our radiotherapy center as an example: the10 linac rooms are located over the entire floor, which is divided into areas A and B (Fig. 1). The patient is assigned to a specific area depending on which linac he will be treated. When a suspected patient appears in area A, the area should be cleared and closed for disinfection immediately. The suspected patient should be temporarily isolated in the observation room of the same area. Furthermore, the accelerator room should be thoroughly disinfected and all the staff that has close contact should be immediately isolated in the observation area.
Fig. 1.
Schematic diagram of the isolation area. Note: 1,2,3,4 are exit numbers.
4. Discussion
Before the COVID-19 outbreak, the number of patients treated each day was over 700 in our radiotherapy center. After January 30, the number of patients treated per day was reduced to around 400. In total, since the end of January to date, more than 2000 patients have been treated. Five patients were suspected of being infected and underwent nucleic acid testing. None of the patients tested positive for COVID-19 and each patient completed the radiotherapy treatment as scheduled. Twenty-one patients had febrile conditions during treatment and were isolated in a specific room for the time necessary to rule out infection (repeat CT scan, blood tests and, if necessary, nucleic acid tests). Our radiotherapy center consists of about 300 doctors, nurses, therapists and administrative employees. No staff member has been infected; three staff members have conducted medical quarantine observations because of their history of high-risk contacts.
The epidemic situation all over the world is still grim. At this critical moment, we hope our experience can help provide some guidance for radiotherapy colleagues and help provide patients with radiation therapy in an organized and safe way.
Funding
This work is supported by the Sichuan Science and Technology Department, China, 2020YFS0424; National Key research and development Plan, China, 2017YFC0113100; Sichuan Province Science and Technology Support Program, China, 20ZDYF1675; Sichuan Province Science and Technology Support Program, China, 2019JDKP0057.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barton M.B., Jacob S., Shafiq J. Estimating the demand for radiotherapy from the evidence: a review of changes from 2003 to 2012. Radiother Oncol. 2014;112:140–144. doi: 10.1016/j.radonc.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 5.Liang W., Guan W., Chen R., Wang W., Li J., Xu K. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Experts consensus of Sichuan Anti-Cancer Association on the prevention and control in radiotherapy places during the COVID-19 epidemic (first edition in Chinese). Journal of Cancer Control and Treatment 2020,33(02):94-99.
- 7.National Health Committee of the People's Republic of China. Technical Guidelines for the Prevention and Control of New Coronavirus Infection in Medical Institutions (First Edition in Chinese) 2020.
- 8.National Health Committee of the People's Republic of China. Diagnosis and Treatment of Pneumonia Caused by New Coronavirus Infection (Trial Version 5 in Chinese), 2020.