The coronavirus disease 2019 (COVID-19) pandemic has precipitated unprecedented challenges for health care, including required deferral of elective procedures by state orders. As those orders have been rescinded, health care organizations, including Mayo Clinic, have been faced with reactivating practices amid the new normal of a COVID-19 environment. To help navigate the transition from crisis operations to a sustainable practice, a Safety Management and Resource Task Force (SMaRT) was established as an additional operational layer to focus exclusively on enhancing safety in complement to practice reactivation.
SMaRT, led by a physician chair and two administrative partners, comprises 22 members, including physicians and nurses from pediatric and adult medicine along with experts from infection prevention and control (IPAC), the aerosol-generating procedures workgroup, diagnostic testing stewardship, data governance, facilities, supply chain, engineering, occupational health services, compliance and enterprise risk, patient experience, information technology, environmental services, and the personal protective equipment (PPE) task force.
By engaging department and division chairs, empowering staff on the front lines, educating and sharing best practices, collaborating and prioritizing work streams, and communicating accurate and transparent information, SMaRT leads the management and coordination of safety measures across the outpatient practice setting.
Engaging Department and Division Chairs
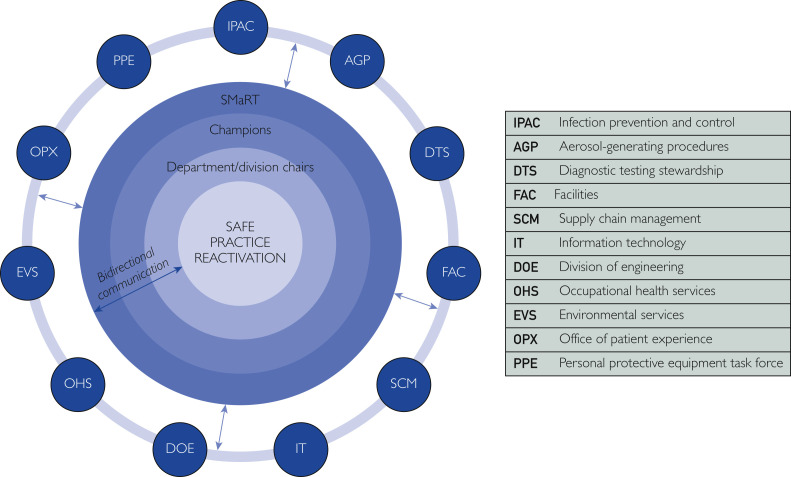
Results of a survey of health care workers during the first weeks of the pandemic showed the top concerns to be the importance of being heard, protected, and prepared.1 Department and division chairs have a key role in building confidence among their teams and must be able to respond to their colleagues’ concerns in a timely, accurate, decisive, and compassionate manner. SMaRT serves as a bidirectional communication bridge between department and division chairs and institutional practice leadership to 1) address and manage COVID-19–related safety concerns; 2) reinforce institutional safety guidelines and recommendations; 3) provide transparent data about COVID-19 testing, transmission rates, and PPE availability; and 4) ensure health care teams have a voice in the decision-making process, while supporting the reactivation of the outpatient practice (Figure ).
Figure.
Communication empowering front-line health care professionals for safe practice reactivation.
Empowering the Front-Line Health Care Professionals
During early practice reactivation, many returning staff who had not been closely involved in the evolution of safer practices during the pandemic expressed safety-related anxieties that required a consistent data-driven response. To reinforce newly implemented safety measures, a SMaRT physician champion was identified in each outpatient department and division to serve as the local safety expert, equipped with the latest recommendations and guidelines.
Champions assembled a safety team within their respective practices composed of a practice operations manager, nurse supervisor, desk supervisor, and trainee responsible for conducting daily safety rounds to identify and solve safety problems locally, when possible. For unique or emerging concerns, champions can escalate issues to SMaRT for input from subject-matter experts and tailored recommendations specific to the department/division’s needs.
Educate and Share Best Practices
The integrated operational and communication network between department/division chairs, SMaRT champions, the SMaRT executive group, and institutional practice leadership not only helps educate and empower the front-line health care professionals of the practice, but it also enables rapid scaling and dissemination of best safety practices across the campuses. SMaRT champions have access to a continually updated toolkit that includes the latest IPAC guidelines, diagnostic testing and screening protocols, environmental assessment tools, COVID-19–specific educational material, and appropriate PPE use and stewardship requirements.
Health care workers are acutely aware of regional and international differences in PPE guidance and practice. Staff members report that they feel safer about PPE when they have accurate information, and PPE guidance reflects their understanding of risk. IPAC is responsible for creating evidence-based guidelines for proper PPE usage. SMaRT then shares strategies for staff to use the appropriate PPE given the exposure risk, while ensuring ongoing availability of supply.
Prioritize, Collaborate, and Innovate
To manage and mitigate the risk of COVID-19 transmission in outpatient practice, SMaRT created subsets of teams to oversee five prioritized work streams:
-
1.
SMaRT Facilities partners with practice areas to promote physical distancing on campus. Implementing safe-spacing measures requires a combination of data modeling of patient volume, creative use of existing spaces, modified patient flows, and leveraging telemedicine and remote work.
-
2.
SMaRT Procedural Practice sponsors three highly collaborative and innovative project teams to support the surgical, procedural, and clinical practices. The first team characterizes aerosol clearance in operating and procedure rooms to help guide data-driven recommendations for safe room turnover times. The second team focuses on source control and aerosol mitigation to pilot new, innovative tools to be used when aerosolized contaminates are of concern. The third team studies the dynamics of masking, physical distancing, and variables related to source activities of coughing, talking, and interacting at variable distances.
-
3.
SMaRT Patient Experience oversees patient perception of the safety measures deployed by Mayo Clinic. To understand what is important for patients to feel safe on campus, SMaRT surveys patients and also obtains feedback from a patient advisory group.
-
4.
SMaRT PPE partners with the Mayo Clinic PPE task force, supply chain, and engineering to conserve PPE, activate acquisition of nontraditional sources of PPE, and pilot safety innovations generated at the grassroots level of the practice.
-
5.
SMaRT Safety Technology Innovation collaborates with information technology, the Mayo Center for Digital Health, security, and facilities to explore technological solutions to further protect the safety of patients, visitors, and staff.
Communicate Accurate and Transparent Information
Communicating reliable information to health care teams throughout the pandemic has been essential for promoting a sense of unity, managing the unprecedented rate of operational change, and ensuring rapid adoption of safety measures. To disseminate relevant information, SMaRT launched a weekly newsletter, Safer Together, which includes the latest safety guidelines, tailored recommendations for safety interventions in individual outpatient practice areas, safety initiatives underway, patient experience feedback, educational materials, and highlights of the novel and innovative safety measures work units have deployed.
Regular sharing of safety data enables proactive decision-making based on leading and lagging indicators. SMaRT provides input to leadership dashboards developed by occupational health and enterprise analytics that ensure practice leadership can see trends in exposures or infections among staff and patients to ensure the continued safe reactivation of the practice. The dashboards monitor staff safety related to COVID-19 across all Mayo Clinic campuses and sites. These dashboards include aggregate data on health care workers who have tested positive for COVID-19, exposure incidents, and work-status impact.
Use of the SMaRT Network to Promote Safe Practices
Since implementation, SMaRT has prepared more than 50 tailored recommendations to address specific department/division needs in a matter of weeks. A few examples are described below.
Coordinated Response
In the ear, nose, and throat (ENT) procedural practice, practitioners raised questions regarding the safest manner for performing ENT outpatient procedures, given the concerns of asymptomatic transmission and a presumably high viral load from the nasopharynx. SMaRT engaged with experts in environmental services, PPE conservation, IPAC, occupational health, and diagnostic stewardship to seek coordinated input for preparing a unified recommendation. The recommendation was shared with the ENT champion, along with educational recommendations for staff, areas of opportunity for innovation, and future considerations for mitigating risk. Using the SMaRT network to escalate this concern allowed clear communication to ENT practitioners of what was expected to provide safe care and eliminated contradictions that may have undermined confidence in safety measures.
Rapid Response
In early stages of practice reactivation, maintaining physical distancing in patient and staff areas quickly emerged as a leading safety barrier. In response, SMaRT formed a rapid response team to assess and quickly implement physical distancing strategies for prime bottleneck areas, including elevators and patient lobbies. With close facilities collaboration, the first safety procedures were in place within 48 hours. In elevators, floor markings, appropriate signage, and sanitizing stations were added. Chairs in outpatient lobbies were positioned strategically to preserve maximum seating and attain needed distancing, and a physical distancing toolkit was developed for SMaRT champions. By applying both centralized and decentralized physical distancing strategies as part of a rapid response effort, SMaRT was able to promote safe distancing.
Data-Driven Response
The Centers for Disease Control and Prevention guidance for time required to remove 99.9% of air contaminants based on air changes/hour caused risk concern for aerosol-generating procedures in the practice and also caused inefficient room turnover. As a result, the SMaRT group initiated a collaborative effort among engineering, facilities, and the practice to improve aerosol clearance. This workgroup measured aerosol clearance rates and found that clearance was two times faster in laminar flow rooms than predicted, providing both staff confidence and improved efficiency for the practice.
Conclusion
With countless variables and evolving science, eliminating risk from COVID-19 is unlikely anytime soon. However, in partnership with the clinical practice, SMaRT has created a robust network of safety professionals that ensures Mayo Clinic achieves unparalleled and uncompromising confidence and trust among patients and staff. At Mayo Clinic, a culture of teamwork, mutual respect, and professionalism sets the tone for the practice. In a recent opinion piece, Atul Gawande, MD, MPH,2 a surgeon and public health researcher, wrote about culture as an important element of success in health care institutions’ response to COVID-19: “It’s one thing to know what we should be doing; it’s another to do it, rigorously and thoroughly… [and feel] you can comfortably call one another out when you see a standard slipping.” For more than 150 years, Mayo Clinic has adhered to the highest safety standards and will continue to do so during the COVID-19 era.
Acknowledgments
Members of the SMaRT Executive Committee include: Kimberly K. Amrami, MD; Jean E. Barth, MPH, RN, CIC; Laura E. Breeher, MD, MPH; Matthew R. Callstrom, MD, PhD; Sean C. Dowdy, MD; Theresa S. Evers, APRN, CNS, MSN; Dawn L. Hucke, MAOL; Ryan T. Hurt, MD, PhD; Amie E. Jones, MD; Claudia F. Lucchinetti, MD; Jill J. Nagel, MBA, PA-C; John C. O’Horo, MD, MPH; Kimberly K. Otte, JD; Rachel L. Pringnitz; Maureen E. Prunty, MHA; Prajnashree Ravikumar, MS; David R. Rushlow, MD; William Sanchez, MD; Melanie D. Swift, MD, MPH; Christopher P. Tommaso, MS; Alexander G. von Bormann, MBA, MSc; Mark B. Wehde, MS, MBA.
Editing, proofreading, and reference verification were provided by Scientific Publications, Mayo Clinic.
Footnotes
This supplement is sponsored by Mayo Clinic Foundation for Medical Education and Research and is authored by experts from multiple Departments and Divisions at Mayo Clinic.
Potential Competing Interests: The authors report no competing interests.
Contributor Information
SMaRT Executive Committee:
Kimberly K. Amrami, Jean E. Barth, Laura E. Breeher, Matthew R. Callstrom, Sean C. Dowdy, Theresa S. Evers, Dawn L. Hucke, Ryan T. Hurt, Amie E. Jones, Claudia F. Lucchinetti, Jill J. Nagel, John C. O’Horo, Kimberly K. Otte, Rachel L. Pringnitz, Maureen E. Prunty, Prajnashree Ravikumar, David R. Rushlow, William Sanchez, Melanie D. Swift, Christopher P. Tommaso, Alexander G. von Bormann, and Mark B. Wehde
References
- 1.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 2.Gawande A. Amid the Coronavirus Crisis. A Regimen for Reentry. The New Yorker. May 13, 2020 [Google Scholar]