Abstract
With the advancement in modern information technology, virtual reality (VR) is being increasingly used for the diagnosis, assessment, and treatment of mental disorders. Recently, a VR-based cognitive behavioral therapy for social phobia has been recognized as a new medical technology in South Korea. This might lead to an increase in the use of VR in the field of psychiatry. The present review provides an overview of the status of VR therapies in various psychiatric conditions such as anxiety disorder, post-traumatic stress disorder, psychosis, addiction, and eating disorder. Besides, it summarizes the role of VR therapy in the management of disorders associated with child and adolescence psychiatry as well as various other clinical applications. Additionally, we discuss the merits and limitations of VR therapy, which might serve as a useful reference for researchers. In the current environment wherein novel medical models consisting of a combination of digital devices and medicine are being developed; understanding new technologies such as VR could open new doors to mental health treatments.
Keywords: Virtual reality, Mental health, Psychiatry, Review
INTRODUCTION
Virtual reality (VR) is a computer-generated simulation of the three-dimensional environment with which one can interact in a seemingly real way [1]. The current standard VR systems use either VR headsets with head-mounted display (HMD) or multi-projected environments to generate realistic images, sounds and other sensations in a virtual environment. More specifically, VR is a phenomenon in which users are “immersed” in a computer-generated environment via a human-computer interface, wherein the user can naturally “interact” with the virtual features or items [1]. VR provides rich visual and auditory stimuli, as well as peripheral tactile and olfactory stimuli. These sensations help the users to feel and remember VR in a realistic manner [2]. The subjective feeling that a user experiences as “being there” is called “presence” [3]. Although the users are aware that VR is not real, they can be mistaken that the simulations are real instances and feel that they have experienced in reality, the events that have occurred in the VR [3,4]. Within the controlled and safe environment of VR, experimenters can manipulate the VR environment as required to test different hypotheses on human behavior. Simultaneously users can repeatedly experience a situation and control the environment themselves [5]. In addition, with the development of bio-signal recognition technology and big data technology, bio-signal data of VR users, such as head movement, body movement, and heart rate can be collected and analyzed using artificial intelligence algorithms to provide objective data on the behavior and symptoms of the patients in their specific VR states. VR is actively used in gaming, education, and business fields. It is also being used in the medical field, particularly in radiology, preoperative planning, and image-guided surgery, as well as in rehabilitation remedies such as physiotherapy and occupational therapy. Nevertheless, the use of VR in these fields is still in its infancy.
Notably, mental health is a representative field that could utilize VR for the diagnosis and treatment of various mental illnesses. There are many psychological barriers to medication-assisted treatment due to the social stigma associated with mental disorders and the burden of medications. Furthermore, psychotherapy has its limitations, owing to the shortage of counseling professionals and the high cost. Therefore, in these situations, logistics and economics of VR therapy would encourage patients to adopt a VR-based treatment regimen. VR therapy provides a realistic and immersive environment tailored to the individual’s needs, and allows for repetitive, consistent, and systematic training. It facilitates objective data measurements, their retrieval, and evaluation. In addition, psychotherapy or training using VR can reduce anxiety in the patients when compared with the traditional treatment methods. These features make VR useful for patients with mental health concerns, who have difficulty interacting with the world.
A study by Rothbaum et al. [6], reported the effectiveness of VR for treating acrophobia in 1995. Since then, the interest in using VR for psychotherapy has increased. Compared to December 2001, when there were only 739 publications with the keyword “virtual reality” in PubMed [7], the number of publications increased remarkably to 10,357, by October 2019. In addition, due to the development of information and smartphone technology, the cost of VR equipment reduced from 100,000 dollars in the 1990s, to less than 100 dollars. This costeffectiveness accelerated the development of VR therapy [8,9]. In Korea, since the first VR clinic opened in 2005 for patients with schizophrenia, social phobia, and alcohol addiction, many hospitals inclined toward VR-based treatments for patients with dementia, post-traumatic stress disorder (PTSD), and internet gaming disorders (IGD). Particularly, VR-based cognitive behavioral therapy (CBT) for social phobia was recognized as a new medical technology in July 2019, which may further contribute to an increased use of VR in psychotherapy.
This review summarizes the current state of VR therapies for mental disorders through the perusal of the available studies on psychotherapy and VR, and outlines the merits and limitations of VR therapy for each disorder. In addition, this paper discusses future directions of research on VR therapy. We believe that this review would serve as a useful resource for clinicians and mental health practitioners interested in VR therapy.
Anxiety disorders
In the context of VR therapy, the most studied area is that of anxiety disorders, and several meta-analyses have reported on the effectiveness of VR intervention on the assessment and treatment of various anxiety disorders [10]. Traditionally, exposure therapy has been the most effective treatment for anxiety disorders. However, direct exposure to feared people/ situations may exacerbate the patient’s anxiety, leading to possible deterrence to treatment or total abandonment of therapy. Moreover, there can be restrictions on the number of times the patient is exposed to the actual source of fear due to their anxiety or phobic symptoms. During VR therapy, patients can experience the virtual anxiety-inducing environment more safely. Additionally, measurements of objective bio-signal data, such as changes in the heart rate and galvanic skin reflex, can be obtained using wearable devices during VR exercise [11]. In particular, bio-signals related to anxiety can be monitored in real time, and exposure to the anxiety-inducing stimulus can be gradually increased in a more logical way [12]. Due to these advantages, VR exposure therapy (VRE) is one of the most powerful treatment modalities’ that overcome the limitations of conventional therapy. Some examples on the use of VR therapy in each sub-area of anxiety disorders are described below.
Specific phobias (SPs), particularly flight phobia, are among the most studied areas of VR therapy. There was no difference in treatment efficacy between the VRE group and the group exposed to a real airplane. Both the groups showed better treatment outcomes than the control group. Moreover, these treatment effects were sustained up to 6 months after the therapy [13]. A meta-analysis on aerophobia reported that VRE not only displayed similar results to traditional therapies; but also resulted in better outcomes after treatment and during the follow-up [14]. In patients with acrophobia, VRE showed a similar therapeutic effect to in vivo exposure therapy and remained effective for approximately 6 months [15]. In addition, VR treatment for arachnophobia (spider phobia) showed similar effectiveness to in vivo exposure therapy and the effect was maintained for about 3 months [16]. Research on driving phobia [17] and claustrophobia [18] has also been conducted. However, these small-scale studies had limitations in generalizing the effectiveness of VR. VRE is actively used in SPs due to higher patient preferences (76%) and lower treatment rejections (VRE: 3%, in vivo exposure treatment: 27%) [19].
For patients with social anxiety disorder (SAD), who have difficulty interacting in social situations due to high anxiety, treatment methods include the use of computer-generated scenarios which are created using VR namely, presentations, interviews, and meetings for patients to deliver a speech [20]. The therapist controls the patient’s anxiety by gradually manipulating the number and the reaction of the virtual audience according to the patients’ response [21]. Although there have been limitations in generalizing results due to different sample characteristics, VR environments and tasks, a metaanalysis on VRE treatment for SAD reported a significant therapeutic improvement [22]. Particularly, CBT training based on VR has been deemed useful.
For patients with panic disorder with agoraphobia (PDA), VRE creates an environment in which patients often experience symptoms (e.g., bus, subway, tunnel, elevator, car driving, airplane, movie theater, and shopping mall), and upon the incidence of panic attacks, the patient is desensitized within a safe VR environment [23,24]. In the context of PDA, VRE has been reported to improve symptoms significantly, in the affected individuals [10]. In the case of obsessive-compulsive disorder (OCD) and generalized anxiety disorder (GAD), the need for VR therapy has been recognized; however, there is scant evidence on the contribution of VR in the mentioned conditions.
Earlier studies on the therapeutic efficacy of VR during anxiety disorders, except OCD and GAD, revealed no significant difference regarding its effectiveness when compared to in vivo therapy. Moreover, the effect of treatment was sustained for either as short as 1 month or, in certain cases, for as long as 12 months [25]. Alternatively, several studies consistently reported the effectiveness of VRE in reducing anxiety in patients with anxiety disorders [26].
Post-traumatic stress disorder
It is very difficult to recreate traumatic situations for PTSD patients as it could lead to excessive exacerbation of their anxiety. VRE may be employed in such patients to enable them to re-experience the traumatic situations in a virtual environment, where they would feel safer than in the real trauma situations. PTSD patients reportedly prefer VR therapy [27]. VR therapy for PTSD is primarily aimed at soldiers who have participated in war (e.g., the Vietnam War or the Iraq war) or survivors of terrorism (e.g., the 9/11 attack). Patients re-experience the traumatic situations in a gaming style [28-30]. VR therapy has been associated with very high satisfaction level when used for patients who have experienced traffic accidents [31]. A meta-analysis on VR therapy in patients with PTSD reported a significant decrease in PTSD and symptoms of depression post-treatment. The effects of the treatment were sustained for 3–6 months. However, each of these studies reported inconsistencies, and there were limitations in terms of the patient’s sex, as the studies were biased towards male soldiers [32].
Psychosis
VR therapy targeting patients with schizophrenia or other psychoses is widely used for the analysis of psychotic symptoms, neurocognitive evaluation, and assessment of activities of daily living [10,33]. While there has been limited research on VR treatment, the scenarios has appreciably changed over the last few years. Freedman used VR-based cognitive therapy to treat major psychotic symptoms such as paranoia. It was reported that VR-based therapy was effective in reducing paranoia, persecutory delusions, and functional impairment in real life [34]. In addition, VR social-skills training, which aimed to improve patients’ social skills, increased patients’ interaction during social situations in the virtual environment, thereby improving the adaptability in actual interpersonal situations [35]. However, very few studies have been conducted on the therapeutic effects of VR on psychosis, and the treatment is limited to small-group settings, making it difficult to generalize the effectiveness.
Child and adolescence psychiatry
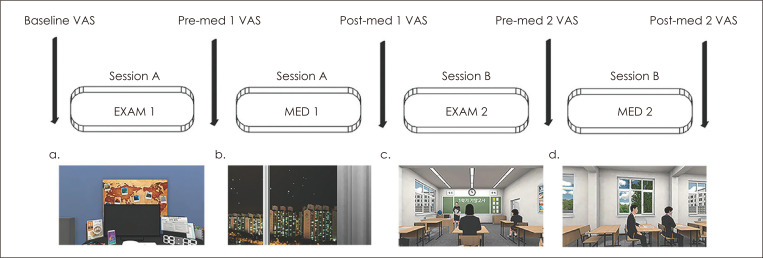
VR is used in children for attention training, social skills training, cognitive rehabilitation, and education in non-clinical groups. In the field of pediatric psychiatry, research has mainly focused on attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD). In children with ADHD or attention problems, continuous performance test (CPT) has been conducted in a VR environment to evaluate and improve children’s attention span [36]. Virtual classroom programs are also gaining attention. These programs simulate the school setting within a virtual environment to improve the attention span, academic skills, and social adaptability in real life situations (Figure 1). A meta-analysis on virtual classrooms reported that children showed more interest in participating in VR training, and results of using VR on improving attention span were akin to those observed using traditional CPT training [37]. However, further research is necessary for the generalizability of the effects of VR training to real life situations. VR is also used to teach social skills to children with ASD [38]. The biggest advantage of VR therapy is that it enables simulation of various social situations, in which each social element is planned and controlled by the therapist in a virtual situation. However, due to the social skill deficits of ASD, understanding of the interpersonal situations required during VR is often restricted, which limits the effectiveness of the treatment [39,40]. Therefore, it is necessary to take advantage of VR’s potential by creating social situations that are well designed by developmental and behavioral experts, and well understood by children with ASD. Moreover, VR is actively used for other disorders such as cerebral palsy, rehabilitation treatment for visual/auditory impairment, and pain distraction [41]. For non-clinical groups, VR is widely used in smoking-prevention education in teens [42] and safety education such as pedestrian safety education [43], as well as in promoting positive social behaviors such as prosocial behavior [44], empathy [45], social compliance, and sharing [46].
Fig. 1.
Example of virtual school program for test anxiety reduction at Gangnam Severance Hospital. Program flow and screenshots from each session (Session A and B). Each session includes sub-sessions: Exam and Meditation (Med). In each of the Exam sessions, the users were exposed to an anxiety-inducing scenario. In each of the Med session, the users were guided through a mindfulness meditation practice in at-home or at-school. Heart rate variability (HRV) and subjective feelings of anxiety using the Visual Analogue Scale (VAS), immediately after each session, were also measured to examine the changes during each of the anxiety-inducing (Exam 1, Exam 2) and meditation (Med 1, Med 2) session in the program.
In children/adolescents, neurological development makes the VR environment appear more vivid than it does in adults. Therefore, the experience of using VR can have a stronger impact on children/adolescents [47]. Despite these unique circumstances, limited research has been conducted on the relationship between VR and developmental characteristics in childhood/adolescence. Further research is needed to ensure that VR can benefit children and adolescents.
Addiction and eating disorders
VR therapy has been used in patients with addiction, such as those with substance use disorder (including alcohol abuse and drug misuse), pathological gambling, and IGD. When patients are exposed to cues reminiscent to addictive substances, they show conditional craving that could lead to a vicious cycle of repeated addictive behavior. In VR, these cues are not just in the form of photographs or videos, but they induce craving by providing social and environmental contexts that remind the patients of these cues [48]. The use of relatively safe cue exposure therapy has been studied to improve coping with psychophysiological addictions, such as alcohol, tobacco, and cocaine, as well as with behavioral addiction, such as pathological gambling and IGD. It has been reported that VR-induced craving through cue exposure, and reduction in addictive behaviors such as nicotine dependence and IGD, have effectiveness similar to that of conventional CBT [48-50]. However, further systematic approaches and meta-analyses are necessary for analyzing each of these addiction groups.
In the case of eating disorders, VR uses visual stimuli to control craving for high-calorie foods, and to change the patient’s body image [51]. A meta-analysis on the treatment of bulimia nervosa and binge eating disorder showed that VR therapy resulted in changes in the individual’s body image, increased motivation to change, increased self-esteem, and reduced body image disturbances, binge eating, and purging behavior [52]. These therapeutic effects lasted for about a year [53].
Additional clinical applications of VR
In addition to being an exposure therapy, VR is used to enhance the therapeutic outcomes, by supplementing it alongside traditional psychotherapy or counselling. Optale et al [54, 55]. used a psychodynamic approach in patients with erectile dysfunction by recreating their childhood in a virtual space, increasing their commitment to treatment, and maintaining the treatment effectiveness for more than 6 months. Moreover, the treatment process was accelerated and the number of patients who dropped out declined. Applications are being developed to reduce insomnia with CBT, utilizing real-time biofeedback of VR [56]. In addition, research into the use of VR for neuropsychological assessment [57] has been actively conducted. Furthermore, VR is being used to create vocational education and training programs that improve attention, memory, and problem-solving skills in patients with traumatic brain injury or schizophrenia [58,59]. The field of VR has been extended to include general education on character, including VR training programs where students, teachers, and guardians learn how to cope with bullying [60].
DISCUSSION
We have reviewed previous studies on VR therapy for various mental disorders. In the face of rapid technological advances, there is an increased use of VR in psychiatry. It has enhanced the effects of traditional therapeutics, and enabled new treatment approaches that were previously impossible. As the price of VR devices reduce and the development of VR hardware in the form of wearable devices and smartphones lead to more space and physical freedom, patients can freely use VR in their own homes for a therapeutic experience and not just hospitals or treatment rooms.
However, since VR technology has been newly introduced in the medical field, there are many challenges that need to be addressed for it to become a well-established technology in the diagnosis and treatment of mental disorders. It is necessary to verify how effective, harmful, or safe VR therapy is, compared to traditional treatment. To date, VR-related clinical trials have had several limitations including a small size, lack of adequate controls, and lack of double-blind studies, which brings up the necessity to be more rigorous in methodological terms. The effectiveness of VR therapy needs to be analyzed and compared with the current gold-standard therapies for each disease. Currently, the effectiveness of VR has only been shown in some areas, such as SPs and SAD, while the evidence on other diseases are currently lacking. In addition, more evidence is necessary to the extent of similarity between human behaviors in VR to those in real life, as certain behaviors in games and VR often differ from those in reality. Based on the results of these clinical studies, it is necessary to establish parameters for VR treatment that would be optimal for functional improvement in real life, and to identify the elements required for treatment.
Currently, research is mainly focused on the merits and therapeutic effects of VR, and further studies on the anticipated side effects and safety of VR are necessary. Simulator sickness is a representative side effect of VR, induced when VR devices are used for a long period. Technology needs to be developed to reduce such side effects. Moreover, much like the addiction to Internet or the smartphone, there are concerns regarding VR addiction. Research and institutional measures on safety will be crucial for the growth of the VR industry.
It is necessary to develop a technology that allows for more natural interaction with avatars in VR. For example, avatars should be able to analyze the users’ words and texts, and automatically communicate using one of the many scripts that fit the situation. Moreover, they should have natural facial expressions for more realistic interactions. In addition, further research is necessary on the accuracy of bio-signals collected from the wearable devices linked to VR. Notably, although the development of wearable devices enabled the measurement of various bio-signals, their accuracy has not yet been medically verified.
CONCLUSION
Approximately 15 years ago, the first VR clinic opened in Korea. After 15 years, VR therapy was selected as a new medical technology in psychiatry in 2019. With a high smartphone penetration rate and Korea’s leading position in information technology, as well as the immense scope for the improvement of VR, further development will allow VR to be used more safely and effectively in various disabilities and clinical scenarios.
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF), funded by the Ministry of Science, and ICT (NRF2017M3C1B6071066).
Footnotes
Conflicts of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Suji Kim, Eunjoo Kim. Data curation: Suji Kim. Funding acquisition: Eunjoo Kim. Investigation: Suji Kim, Eunjoo Kim. Project administration: Eunjoo Kim. Supervision: Eunjoo Kim. Validation: Eunjoo Kim. Visualization: Suji Kim. Writing—original draft: Suji Kim. Writing—review & editing: Eunjoo Kim.
ORCID iDs
Suji Kim https://orcid.org/0000-0001-9076-4677
Eunjoo Kim https://orcid.org/0000-0003-3061-2051
REFERENCES
- 1.Schultheis MT, Rizzo AA. The application of virtual reality technology in rehabilitation. Rehabil Psychol. 2001;46:296–311. doi: 10.1037/0090-5550.46.3.296. [DOI] [Google Scholar]
- 2.Dinh HQ, Walker N, Hodges LF, Song C, Kobayashi A Evaluating the importance of multi-sensory input on memory and the sense of presence in virtual environments. Proceedings IEEE Virtual Reality (Cat. No. 99CB36316);1999 Mar 13-17. Houston, TX: IEEE; 1999. pp. 222–228. [Google Scholar]
- 3.Slater M. Place illusion and plausibility can lead to realistic behaviour in immersive virtual environments. Philos Trans R Soc Lond B Biol Sci. 2009;364:3549–3557. doi: 10.1098/rstb.2009.0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Slater M, Sanchez-Vives MV. Enhancing our lives with immersive virtual reality. Front Robot AI. 2016;3:74. doi: 10.3389/frobt.2016.00074. [DOI] [Google Scholar]
- 5.Maples-Keller JL, Bunnell BE, Kim SJ, Rothbaum BO. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv Rev Psychiatry. 2017;25:103–113. doi: 10.1097/HRP.0000000000000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rothbaum BO, Hodges LF, Kooper R, Opdyke D, Williford JS, North M. Effectiveness of computer-generated (virtual reality) graded exposure in the treatment of acrophobia. Am J Psychiatry. 1995;152:626–628. doi: 10.1176/ajp.152.4.626. [DOI] [PubMed] [Google Scholar]
- 7.Riva G. Virtual reality for health care: the status of research. Cyberpsychol Behav. 2002;5:219–225. doi: 10.1089/109493102760147213. [DOI] [PubMed] [Google Scholar]
- 8.Cha KR, Kim CH. Virtual reality in current and future psychiatry. Korean J Biol Psychiatry. 2007;14:28–41. [Google Scholar]
- 9.Parsons TD, Riva G, Parsons S, Mantovani F, Newbutt N, Lin L, et al. Virtual reality in pediatric psychology. Pediatrics. 2017;140(Suppl 2):S86–S91. doi: 10.1542/peds.2016-1758I. [DOI] [PubMed] [Google Scholar]
- 10.Freeman D, Reeve S, Robinson A, Ehlers A, Clark D, Spanlang B, et al. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol Med. 2017;47:2393–2400. doi: 10.1017/S003329171700040X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pallavicini F, Algeri D, Repetto C, Gorini A, Riva G. Biofeedback, virtual reality and mobile phones in the treatment of generalized anxiety disorder (gad): a phase-2 controlled clinical trial. J Cyber Ther Rehabil. 2009;2:315–327. [Google Scholar]
- 12.Wiederhold BK, Jang DP, Kim SI, Wiederhold MD. Physiological monitoring as an objective tool in virtual reality therapy. Cyberpsychol Behav. 2002;5:77–82. doi: 10.1089/109493102753685908. [DOI] [PubMed] [Google Scholar]
- 13.Rothbaum BO, Hodges L, Smith S, Lee JH, Price L. A controlled study of virtual reality exposure therapy for the fear of flying. J Consult Clin Psychol. 2000;68:1020–1026. doi: 10.1037/0022-006X.68.6.1020. [DOI] [PubMed] [Google Scholar]
- 14.Cardoş RAI, David OA, David DO. Virtual reality exposure therapy in flight anxiety: a quantitative meta-analysis. Comput Hum Behav. 2017;72:371–380. doi: 10.1016/j.chb.2017.03.007. [DOI] [Google Scholar]
- 15.Emmelkamp PM, Krijn M, Hulsbosch AM, de Vries S, Schuemie MJ, van der Mast CA. Virtual reality treatment versus exposure in vivo: a comparative evaluation in acrophobia. Behav Res Ther. 2002;40:509–516. doi: 10.1016/S0005-7967(01)00023-7. [DOI] [PubMed] [Google Scholar]
- 16.Michaliszyn D, Marchand A, Bouchard S, Martel MO, Poirier-Bisson J. A randomized, controlled clinical trial of in virtuo and in vivo exposure for spider phobia. Cyberpsychol Behav Soc Netw. 2010;13:689–695. doi: 10.1089/cyber.2009.0277. [DOI] [PubMed] [Google Scholar]
- 17.Wald J, Taylor S. Efficacy of virtual reality exposure therapy to treat driving phobia: a case report. J Behav Ther Exp Psychiatry. 2000;31:249–257. doi: 10.1016/S0005-7916(01)00009-X. [DOI] [PubMed] [Google Scholar]
- 18.Botella C, Baños RM, Perpiñá C, Villa H, Alcañiz M, Rey A. Virtual reality treatment of claustrophobia: a case report. Behav Res Ther. 1998;36:239–246. doi: 10.1016/S0005-7967(97)10006-7. [DOI] [PubMed] [Google Scholar]
- 19.Garcia-Palacios A, Botella C, Hoffman H, Fabregat S. Comparing acceptance and refusal rates of virtual reality exposure vs. in vivo exposure by patients with specific phobias. Cyberpsychol Behav. 2007;10:722–724. doi: 10.1089/cpb.2007.9962. [DOI] [PubMed] [Google Scholar]
- 20.Kim HY, Chad E, Kim M. The effects of virtual reality exposure therapy on public speaking anxiety in female university students. Korean J Health Psychology. 2017;22:833–847. doi: 10.17315/kjhp.2017.22.4.002. [DOI] [Google Scholar]
- 21.Anderson PL, Price M, Edwards SM, Obasaju MA, Schmertz SK, Zimand E, et al. Virtual reality exposure therapy for social anxiety disorder: a randomized controlled trial. J Consult Clin Psychol. 2013;81:751–760. doi: 10.1037/a0033559. [DOI] [PubMed] [Google Scholar]
- 22.Kampmann IL, Emmelkamp PM, Morina N. Meta-analysis of technology-assisted interventions for social anxiety disorder. J Anxiety Disord. 2016;42:71–84. doi: 10.1016/j.janxdis.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Botella C, García-Palacios A, Villa H, Baños RM, Quero S, Alcañiz M, et al. Virtual reality exposure in the treatment of panic disorder and agoraphobia: a controlled study. Clin Psychol Psychother. 2007;14:164–175. doi: 10.1002/cpp.524. [DOI] [Google Scholar]
- 24.Pelissolo A, Zaoui M, Aguayo G, Yao SN, Roche S, Ecochard R, et al. Virtual reality exposure therapy versus cognitive behavior therapy for panic disorder with agoraphobia: a randomized comparison study. J Cyber Ther Rehabil. 2012;5:35–43. [Google Scholar]
- 25.Rothbaum BO, Hodges L, Anderson PL, Price L, Smith S. Twelvemonth follow-up of virtual reality and standard exposure therapies for the fear of flying. J Consult Clin Psychol. 2002;70:428–432. doi: 10.1037/0022-006X.70.2.428. [DOI] [PubMed] [Google Scholar]
- 26.Fodor LA, Coteţ CD, Cuijpers P, Szamoskozi Ş, David D, Cristea IA. The effectiveness of virtual reality based interventions for symptoms of anxiety and depression: a meta-analysis. Sci Rep. 2018;8:10323. doi: 10.1038/s41598-018-28113-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rizzo A, Shilling R. Clinical virtual reality tools to advance the prevention, assessment, and treatment of PTSD. Eur J Psychotraumatol. 2017;8(sup 5):1414560. doi: 10.1080/20008198.2017.1414560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rothbaum BO, Hodges L, Alarcon R, Ready D, Shahar F, Graap K, et al. Virtual reality exposure therapy for PTSD Vietnam Veterans: a case study. J Trauma Stress. 1999;12:263–271. doi: 10.1023/A:1024772308758. [DOI] [PubMed] [Google Scholar]
- 29.Rizzo A, Pair J, Graap K, Manson B, McNerney PJ, et al. A virtual reality exposure therapy application for Iraq War military personnel with post traumatic stress disorder: from training to toy to treatment. In: Roy M, editor. NATO Advanced Research Workshop on novel approached to the diagnosis and treatment of posttraumatic stress disorder. Washington DC: IOS Press; 2006. pp. 235–250. [Google Scholar]
- 30.Difede J, Hoffman HG. Virtual reality exposure therapy for World Trade Center Post-traumatic stress disorder: a case report. Cyberpsychol Behav. 2002:529–535. doi: 10.1089/109493102321018169. [DOI] [PubMed] [Google Scholar]
- 31.Beck JG, Palyo SA, Winer EH, Schwagler BE, Ang EJ. Virtual reality exposure therapy for PTSD symptoms after a road accident: an uncontrolled case series. Behav Ther. 2007;38:39–48. doi: 10.1016/j.beth.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 32.Kothgassner OD, Goreis A, Kafka JX, Van Eickels RL, Plener PL, Felnhofer A. Virtual reality exposure therapy for posttraumatic stress disorder (PTSD): a meta-analysis. Eur J Psychotraumatol. 2019;10:1654782. doi: 10.1080/20008198.2019.1654782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rus-Calafell M, Garety P, Sason E, Craig TJK, Valmaggia LR. Virtual reality in the assessment and treatment of psychosis: a systematic review of its utility, acceptability and effectiveness. Psychol Med. 2018;48:362–391. doi: 10.1017/S0033291717001945. [DOI] [PubMed] [Google Scholar]
- 34.Freeman D, Bradley J, Antley A, Bourke E, DeWeever N, Evans N, et al. Virtual reality in the treatment of persecutory delusions: randomised controlled experimental study testing how to reduce delusional conviction. Br J Psychiatry. 2016;209:62–67. doi: 10.1192/bjp.bp.115.176438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park KM, Ku J, Choi SH, Jang HJ, Park JY, Kim SI, et al. A virtual reality application in role-plays of social skills training for schizophrenia: a randomized, controlled trial. Psychiatry Res. 2011;189:166–172. doi: 10.1016/j.psychres.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 36.Pollak Y, Weiss PL, Rizzo AA, Weizer M, Shriki L, Shalev RS, et al. The utility of a continuous performance test embedded in virtual reality in measuring ADHD-related deficits. J Dev Behav Pediatr. 2009;30:2–6. doi: 10.1097/DBP.0b013e3181969b22. [DOI] [PubMed] [Google Scholar]
- 37.Parsons TD, Duffield T, Asbee J. A comparison of virtual reality classroom continuous performance tests to traditional continuous performance tests in delineating ADHD: a meta-analysis. Neuropsychol Rev. 2019;29:338–356. doi: 10.1007/s11065-019-09407-6. [DOI] [PubMed] [Google Scholar]
- 38.Bellani M, Fornasari L, Chittaro L, Brambilla P. Virtual reality in autism: state of the art. Epidemiol Psychiatr Sci. 2011;20:235–238. doi: 10.1017/S2045796011000448. [DOI] [PubMed] [Google Scholar]
- 39.Parsons TD, Rizzo AA, Rogers S, York P. Virtual reality in paediatric rehabilitation: a review. Dev Neurorehabil. 2009;12:224–238. doi: 10.1080/17518420902991719. [DOI] [PubMed] [Google Scholar]
- 40.Parsons S, Cobb S. State-of-the-art of virtual reality technologies for children on the autism spectrum. Eur J Spec Needs Educ. 2011;26:355–366. doi: 10.1080/08856257.2011.593831. [DOI] [Google Scholar]
- 41.Bailey JO, Bailenson JN. Considering virtual reality in children's lives. J Child Media. 2017;11:107–113. doi: 10.1080/17482798.2016.1268779. [DOI] [Google Scholar]
- 42.Andrade AD, Idrees T, Karanam C, Anam R, Ruiz JG. Effects of an avatar-based anti-smoking game on smoking cessation intent. In: Westwood JD, Westwood SW, Felländer-Tsai L, Fidopiastis CM, Liu A, et al., editors. Medicine meets virtual reality 22: NextMed/ MMVR22. Amsterdam: IOS Press; 2016. pp. 15–18. [PubMed] [Google Scholar]
- 43.Schwebel DC, Gaines J, Severson J. Validation of virtual reality as a tool to understand and prevent child pedestrian injury. Accid Anal Prev. 2008;40:1394–1400. doi: 10.1016/j.aap.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 44.Shriram K, Oh SY, Bailenson JN. Virtual reality and prosocial behavior. In: Burgoon JK, Magnenat-Thalmann N, Pantic M, Vinciarelli A, editors. Social signal processing. Cambridge: Cambridge University Press; 2017. pp. 304–316. [DOI] [Google Scholar]
- 45.van Loon A, Bailenson J, Zaki J, Bostick J, Willer R. Virtual reality perspective-taking increases cognitive empathy for specific others. PLoS One. 2018;13:e0202442. doi: 10.1371/journal.pone.0202442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bailey JO, Bailenson JN, Obradovic J, Aguiar N. Virtual reality's effect on children's inhibitory control, social compliance, and sharing. J Appl Dev Psychol. 2019;64:101052. doi: 10.1016/j.appdev.2019.101052. [DOI] [Google Scholar]
- 47.Bailey JO, Bailenson JN. Immersive virtual reality and the developing child. In: Brooks P, Blumberg F, editors. Cognitive development in digital contexts. San Diego, CA: Elsevier; 2017. pp. 181–200. [DOI] [Google Scholar]
- 48.Hone-Blanchet A, Wensing T, Fecteau S. The use of virtual reality in craving assessment and cue-exposure therapy in substance use disorders. Front Hum Neurosci. 2014;8:844. doi: 10.3389/fnhum.2014.00844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Park SY, Kim SM, Roh S, Soh MA, Lee SH, Kim H, et al. The effects of a virtual reality treatment program for online gaming addiction. Comput Methods Programs Biomed. 2016;129:99–108. doi: 10.1016/j.cmpb.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 50.Shin YB, Kim JJ, Kim MK, Kyeong S, Jung YH, Eom H, et al. Development of an effective virtual environment in eliciting craving in adolescents and young adults with internet gaming disorder. PLoS One. 2018;13:e0195677. doi: 10.1371/journal.pone.0195677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clus D, Larsen ME, Lemey C, Berrouiguet S. The use of virtual reality in patients with eating disorders: systematic review. J Med Internet Res. 2018;20:e157. doi: 10.2196/jmir.7898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.de Carvalho MR, Dias TRS, Duchesne M, Nardi AE, Appolinario JC. Virtual reality as a promising strategy in the assessment and treatment of bulimia nervosa and binge eating dsorder: a systematic review. Behav Sci (Basel) 2017;7:E43. doi: 10.3390/bs7030043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Manzoni GM, Cesa GL, Bacchetta M, Castelnuovo G, Conti S, Gaggioli A, et al. Virtual reality-enhanced cognitive-behavioral therapy for morbid obesity: a randomized controlled study with 1 year follow-up. Cyberpsychol Behav Soc Netw. 2016;19:134–140. doi: 10.1089/cyber.2015.0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Optale G, Marin S, Pastore M, Nasta A, Pianon C. Male sexual dysfunctions and multimedia immersion therapy (follow-up) Cyberpsychol Behav. 2003;6:289–294. doi: 10.1089/109493103322011588. [DOI] [PubMed] [Google Scholar]
- 55.Optale G, Munari A, Nasta A, Pianon C, Baldaro Verde J, Viggiano G. Multimedia and virtual reality techniques in the treatment of male erectile disorders. Int J Impot Res. 1997;9:197–203. doi: 10.1038/sj.ijir.3900316. [DOI] [PubMed] [Google Scholar]
- 56.de Zambotti M, Colrain IM, Baker FC, Kumar R, Sizintsev M, Samarasekera S, et al. inventors. SRI International assignee, Biofeedback virtual reality sleep assistant. United States patent US 20140316191A1. 2014 Oct 23. [Google Scholar]
- 57.Rizzo AA, Schultheis M, Kerns KA, Mateer C. Analysis of assets for virtual reality applications in neuropsychology. Neuropsychol Rehabil. 2004;14:207–239. doi: 10.1080/09602010343000183. [DOI] [Google Scholar]
- 58.Man DW, Poon WS, Lam C. The effectiveness of artificial intelligent 3-D virtual reality vocational problem-solving training in enhancing employment opportunities for people with traumatic brain injury. Brain Inj. 2013;27:1016–1025. doi: 10.3109/02699052.2013.794969. [DOI] [PubMed] [Google Scholar]
- 59.Tsang MM, Man DW. A virtual reality-based vocational training system (VRVTS) for people with schizophrenia in vocational rehabilitation. Schizophr Res. 2013;144:51–62. doi: 10.1016/j.schres.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 60.Stavroulia K, Ruiz-Harisiou A, Manouchou E, Georgiou K, Sella F, Lanitis A. Lemesos, Cyprus: IEEE; 2016. A 3D virtual environment for training teachers to identify bullying. 2016 18th Mediterranean Electrotechnical Conference (MELECON); 2016 Apr 18-20; pp. 1–6. [DOI] [Google Scholar]