Abstract
Objectives:
To understand why most stroke patients receive little therapy. We investigated the factors associated with the amount of stroke therapy delivered.
Methods:
Data regarding adults admitted to hospital with stroke for at least 72 hours (July 2013–July 2015) were extracted from the UK’s Sentinel Stroke National Audit Programme. Descriptive statistics and multilevel mixed effects regression models explored the factors that influenced the amount of therapy received while adjusting for confounding.
Results:
Of the 94,905 patients in the study cohort (mean age: 76 (SD: 13.2) years, 78% had a mild or moderate severity stroke. In all, 92% required physiotherapy, 87% required occupational therapy, 57% required speech therapy but only 5% were considered to need psychology. The average amount of therapy ranged from 2 minutes (psychology) to 14 minutes (physiotherapy) per day of inpatient stay. Unmodifiable characteristics (such as stroke severity) dominated the variation in the amount of therapy. However important, modifiable organizational factors were the day and time of admission, type of stroke team, timely therapy assessments, therapy and nursing staffing levels (qualified and support staff), and presence of weekend or early supported discharge services.
Conclusion:
The amount of stroke therapy is associated with unmodifiable patient-related characteristics and modifiable organizational factors in that more therapy was associated with higher therapy and nurse staffing levels, specialist stroke rehabilitation services, timely therapy assessments, and the presence of weekend and early discharge services.
Keywords: Stroke, physiotherapy, occupational therapy, speech and language therapy, psychology, intensity, dose
Introduction
Within the UK, approximately two-thirds of all stroke survivors are left with some form of long-term disability1 Stroke therapy, compromising physiotherapy, occupational therapy, speech therapy, and psychology are key to both patient recovery and their long-term quality of life.2 There is substantial evidence that stroke therapy is effective when provided intensively, thus the National Clinical Guideline for Stroke recommend that
People with stroke should accumulate at least 45 minutes of each appropriate therapy every day, at a frequency that enables them to meet their rehabilitation goals, and for as long as they are willing and capable of participating and showing measurable benefit from treatment.
This amount of therapy is rarely achieved, however,3 which is a major cause of service users’ dissatisfaction with stroke services.4 It has also been attributed to poorer outcomes in the United Kingdom compared to other European countries which provide more therapy even when confounding variables (such as stroke severity) were controlled.5 Recent research has indicated that although staffing levels may play a part in the amount of therapy provided, organization is also an important factor.6 Our aim was therefore to investigate the variation in the amount of stroke therapy during inpatient stroke care provided using data from Sentinel Stroke National Audit Programme (SSNAP)3 to identify the factors associated with the amount of therapy delivered.
Methods
Full details on the SSNAP are found elsewhere.6,7 In short, SSNAP collects information on over 95% of stroke hospital admissions (≈80,000/year) in England, Wales, and Northern Ireland. The programme has three components: a patient-level audit which records personal and clinical data about each stroke patient and the care they receive from entering hospital for the duration of their care by a specialist stroke team and up to six months poststroke7 and two organizational audits of acute stroke care8 and post-acute care9 recorded every two years. Acute care includes hyper-acute and acute stroke care. Post-acute care includes specialist inpatient rehabilitation units and community-based stroke teams. All National Health Service (NHS) acute inpatient stroke care teams are required to report to SSNAP’s clinical database; however, community-based teams report voluntarily. The organizational audits provide a biennial cross-sectional snapshot of the structural and organizational characteristics of stroke services providing these stages of care. The acute organizational audit from 2014 and the post-acute audit from 2015 were included here.8,9 Other than some overlap for inpatient rehabilitation care, the two organizational audits ask different questions reflecting the different ways services are organized. This meant that analyses relating to inpatient care and community stroke care were performed separately.
Adults who were admitted after a stroke between July 2013 and July 2015 and recorded in SSNAP were included. To focus on stroke patients potentially eligible for therapy, the data were restricted to patients who were inpatients for at least 72 hours and not recorded to be receiving end-of-life care. The clinical database collects information for each stroke team at each stage care, and the organizational audits record information at hospital level, which may include several stroke teams. The two data sets were linked via a codebook provided by SSNAP.
SSNAP maintains rigorous data quality control data checks. Missing data were, however, present in the measure of stroke severity on admission – the National Institute for Health Stroke Scale (NIHSS).10 Level of consciousness is the only item of NIHSS which is mandatorily completed in SSNAP, and some patients had missing values for the remaining 14 items. For these patients, the score on the ‘Level of consciousness’ item was used as a proxy measure of stroke severity by mapping the scores to the criteria of the NIHSS used to categorize stroke severity as follows:
Level of consciousness score 0 (alert) – Mild stroke (NIHSS score = 0–4);
Level of consciousness score 1 (drowsy but rousable) – Moderate stroke (NIHSS score = 5–15);
Level of consciousness 2 (needs repeated stimulus to rouse) – Severe stroke (NIHSS score = 16–20);
Level of consciousness 3 (unconscious) – Very Severe stroke (NIHSS score = 21+).
If additional items were recorded, they were added and the patient’s severity band adjusted as necessary. Patients were excluded if level of consciousness was recorded as 0 (i.e. alert) but all other NIHSS assessments were missing, as they were thought to be a special set of cases.
SSNAP’s acute care audit8 classified inpatient teams as follows: Routinely Admitting Team, Non-Routinely Admitting Acute Team (who do not generally admit stroke patients directly but provide acute care and/or rehabilitation typically after repatriation from a hyper-acute team), or a Non-Acute Inpatient Team (who do not admit patients directly but provide inpatient rehabilitation). To distinguish between Routinely Admitting Teams providing hyper-acute/acute care and those which combine acute care and rehabilitation, we divided them based the team’s median length of stay. As SSNAP define acute stroke care as lasting up to seven days,8 this was used. Routinely Admitting Teams with median length of stay less than seven days were referred to as an acute routinely admitting team (i.e. a hyper-acute or acute stroke team), while those with a median length of stay ⩾seven days were assumed to provide combined acute care and rehabilitation.
The amount of each therapy received by patients were estimated separately by fitting a multilevel mixed effects regression model with robust standard errors in STATA version 15.11 To accurately represent the amount of therapy received and reduce reporter bias, therapy was defined as the average amount of therapy per day of stay (i.e. the total minutes of therapy divided by length of stay). Only patients reported to require each therapy were included in the analyses. To account for the lack of independence within patients clustered within stroke teams, a random intercept was fitted alongside fixed patient and organizational factors to represent variation in average amount therapy/day of stay.12 In all models, effect estimates (Coef) and associated 95% confidence intervals (95% CI) were reported for each predictor. The audits were vetted a priori by the study team for factors thought to influence access to therapy or account for any confounding. Potential confounding variables were included in the model as covariates. See Table 1 for list of all admission, patient, stroke, therapy, and organization-related factors.
Table 1.
Variables included as confounding factors in the regression analyses.
| Variables | |
|---|---|
| Admission-related factors | • The number of inpatient stroke teams the patient was treated by (1st, 2nd, 3rd . . .) • Time since stroke on admission (days) Day of the week and time of day for first admission (fitted as a categorical variable with Monday as the reference category) |
| Patient-related factors | • Age • Gender • Ethnicity • Social deprivation • Stroke related co-morbidities (congestive heart failure, hypertension, atrial fibrillation, diabetes) • Premorbid disability (modified Rankin Scale) • Stroke type (infarct/haemorrhage • Stroke severity (NIHSS on admission) • Stroke Impairment Classification (derived from the NIHSS score on admission) |
| Therapy-related factors | • Whether therapy assessments were performed within 72 hours • Average amount therapy/day of stay (min/day of stay) |
| Organization-related factors | • Was a thrombolysis service in place? • Median length of stay per unit • Type of stroke team (RATa, RATc, NRAT, NAIT) • Number of qualified nurses (WTE/10 beds) • Number of nursing support workers (WTE/10 beds) • Number of qualified therapists (WTE/10 beds) • Number of therapy support workers (WTE/10 beds) • No. of therapy disciplines available on six or seven days a week • Was there access to social worker within five days? • Was there access to ESD team or CRT team? |
NIHSS: National Institute for Health Stroke Scale; NRAT: non-routinely admitting combined team; NAIT: non-admitting inpatient team (rehabilitation unit); ESD: Early Supported Discharge; CRT: Community Rehabilitation team.
Results
Our database included 94,905 patients. They were typical of the stroke population (Table 2). A total of 183 hospitals responded to the acute organizational audit representing 197 stroke teams (some hospital organizations included more than one stroke team). In all, 82 were an acute stroke team, 78 were a combined team, and 37 were a specialist rehabilitation team. The mean number of stroke beds within each service responding to the acute organizational audit was 28.7 (SD: 12.9, max = 76). Nearly three-quarters (70.4%) had access to an Early Supported Discharge team, and 58% a community rehabilitation team. Most teams (n = 100, 56.4%) only provided therapy on week days; 11% (n = 21) provided one therapy in an extended service (i.e. over six or seven days per week) and one-third (n = 62, 34%) provided an extended service of two or more therapies. The therapies provided and the days on which they are available are not specified in SSNAP. Less than two-thirds (n = 112, 61.2%) had access to clinical psychology. Inpatient therapy and nursing staffing levels are shown in Table 3. There were wide variations between the minimum and maximum staffing levels for each profession and the deployment of therapy and support workers.
Table 2.
Patient characteristics at baseline/admission (N = 94,905).
| Characteristic | Factor | Frequency (%) |
|---|---|---|
| Ethnicity | Asian including Chinese | 2669 (2.8) |
| Black | 1365 (1.4) | |
| Mixed | 294 (0.3) | |
| Unknown | 4620 (4.8) | |
| Other | 1141 (1.2) | |
| White | 84,816 (89.0) | |
| Stroke severity (NIHSS on admission) | Mild (<5) | 36,376 (38.3) |
| Moderate (5–15) | 37,527 (40.0) | |
| Severe (16–20) | 10,505 (11.1 | |
| Very severe (>20) | 10,497 (11.1) | |
| Stroke-related comorbidities | Previous stroke/TIA | 26,496 (27.9 |
| Diabetes | 19,414 (20.5 | |
| Atrial fibrillation | 21,352 (22.5 | |
| Hypertension | 52,400 (55.2) | |
| Congestive heart failure | 5690 (6.0 | |
| No. comorbidities | 0 | 22,673 (23.9) |
| 1–2 | 59,832 (63.0 | |
| 3–5 | 12,400 (13.1) | |
| Assessment within 72 hours of admission | Swallow screen by a nurse | 86,591 (91.2) |
| Swallow assessment by speech therapist | 37,504 (39.5) | |
| Communication assessment by speech therapist | 40,077 (42.2) | |
| Physiotherapy assessment | 83,204 (87.7) | |
| Occupational therapy assessment | 73,361 (77.3) | |
| Total | 94,905 |
NIHSS: National Institute of Health Stroke Scale; TIA: transient ischaemic attack.
Table 3.
Staffing levels in inpatient stroke teams.
| Inpatient care period | Median | Lower quartile range | Upper quartile range | Maximum |
|---|---|---|---|---|
| Nursing WTE/10 beds (qualified) | 9.2 | 7.8 | 12.4 | 19.5 |
| Nursing WTE/10 beds (support worker) | 5.4 | 4.6 | 6.7 | 14.9 |
| PT WTE/10 beds (qualified) | 1.3 | 1.2 | 2 | 3.3 |
| PT WTE/10 beds (support worker) | 0.5 | 0.3 | 0.7 | 1.6 |
| OT WTE/10 beds (qualified) | 1.1 | 0.9 | 1.8 | 2.8 |
| OT WTE/10 beds (support worker) | 0.4 | 0.2 | 0.6 | 3.8 |
| SLT WTE/10 beds (qualified) | 0.5 | 0.4 | 0.8 | 1.7 |
| SLT WTE/10 beds (support worker) | 0 | 0 | 0.2 | 1.1 |
| Psyc WTE/10 beds (qualified) | 0.05 | 0 | 0.3 | 1.4 |
| Psyc WTE/10 beds (support worker) | 0 | 0 | 0 | 0.5 |
PT: physiotherapy; OT: occupational therapy; SLT: speech and language therapy; Psyc: psychology; WTE: work time equivalent.
The stroke therapy
Table 4 indicates that physiotherapy and occupational therapy assessments were completed for most patients, while 91% of patients received a swallow assessment by a nurse and 50% by a speech and language therapist. Nearly all patients required physiotherapy and occupational therapy (92% and 87%, respectively), while 57% required speech and language therapy; however, only 5% were considered to need psychology.
Table 4.
Requirement for and provision of stroke therapy.
| Therapy characteristic | PT | OT | SLT | Psych |
|---|---|---|---|---|
| Inpatient therapy (N, med, IQR) | ||||
| Proportion patients required therapy (n, %) | 87,561 (92.3) | 83,575 (88.1) | 54,068 (57.0) | 4466 (4.7) |
| No. of days in which patients received therapy (n, median, IQR, median % of length of stay) | 106,294, 5 (2.11), 40% | 102,001, 4 (2.8), 31% | 67,314, 3 (1.7), 12% | 7697, 1 (1.2), 5% |
| Duration of treatment per day (min/day treated, n, median, IQR) | 106,294, 34.5 (26.6, 45.0) | 102,001, 40 (30, 49.8) | 67,314, 31.3 (23.3, 44.4) | 7697, 42 (30, 53.6) |
| Amount of therapy (min/day of stay) received (n, median, IQR) | 106,294, 13.8 (7.5, 21.7) | 102,001, 12.9 (6.8, 21.1) | 67,314, 6.7 (3.3, 12.3) | 7697, 1.9 (0.6, 4.5) |
| Amount of therapy (min/day of stay) in RATa | 49,667, 13.5 (7.6, 21) | 47,509, 12.8 (6.8, 21.0) | 31,174, 7.0 (3.5,21.5) | 2073, 2.3 (0.8, 5.7) |
| Amount of therapy (min/day of stay) in RATc | 39,575, 12.5 (7.1, 20.0) | 37,671, 12, (6.2, 19.7) | 24,078, 6.3 (3.2, 11.3) | 2544, 1.3 (0.3, 2.9) |
| Amount of therapy (min/day of stay) in NRAT | 10,417, 16.8 (9.8, 25.5) | 10,243, 15.5 (8.3, 25.5) | 7743, 7.9 (3.8, 15.0) | 1812, 2.9 (1.1, 6.4) |
| Amount of therapy (min day of stay) in NAIT | 6635, 17.5 (10.5, 26.8) | 6578, 15.0 (8.57, 24.0) | 4319, 5.8 (2.4, 12.9) | 1268, 2.1 (0.8, 4.1) |
PT: physiotherapy; OT: occupational therapy; SLT: speech and language therapy; RATa = routinely admitting acute team; RATc = routinely admitting combined team; NRAT = non-routinely admitting combined team; NAIT = non-admitting inpatient team (rehabilitation unit), N = number.
The table involved the records for every stroke team that each individual patient was treated by. As some patients were treated by more than one team, the totals may be greater than the size of the cohort (n = 9490).
Most patients (87%) required input from two or three therapy disciplines. The average duration of a therapy treatment session (Table 4) varied from 31 min/day for speech and language therapy to 42 min/day for psychology (Figure 1). However, therapy was received infrequently. On average, patients received physiotherapy on only five days of their inpatient stay, averaging 14 min/inpatient day of stay, and only one session of psychology (i.e. an assessment without ongoing treatment) which amounted to an average of 2 min/inpatient day of stay (Table 4, Figure 2).
Figure 1.
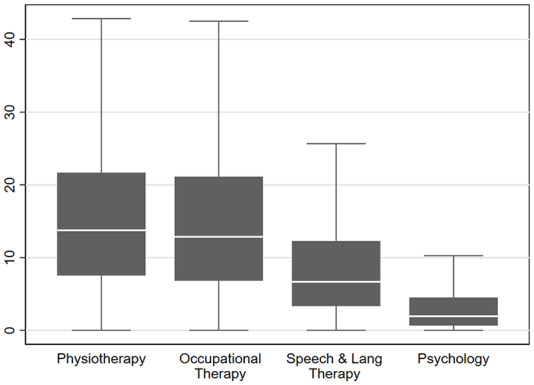
Box plot of the amount of therapy per day of stay.
Figure 2.
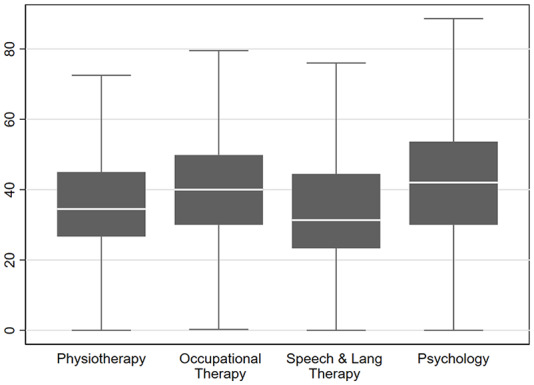
Box plot of the average treatment session duration.
Supplementary Table 1 reports the influence of each factor on the average amount therapy/day of stay (min/inpatient day of stay). Patient-related factors had the strongest influence. Premorbid disability was associated with less therapy/day of stay than those who were independent. Patients with very/severe strokes received less physiotherapy and occupational therapy per day of stay than those who were more mildly affected, whereas speech and language therapy/day of stay increased. The number of impairments were also important. Patients with a stroke that involved only motor impairments received the most physiotherapy and occupational therapy, with the amount of physiotherapy and occupational therapy decreasing as the number of impairments increased. Patients with cognitive impairments (including aphasia) tended to receive more speech and language therapy than those who did not. Men tended to receive more physical and speech therapy, but less occupational therapy than women, and people from all ethnic minorities received less therapy than ‘white’ patients.
Although a less strong influence than the personal factors, several organizational factors were associated with the amount of therapy. First, the day and time of admission were important. For all therapies, patients admitted on Sunday received the most therapy; this decreased with each subsequent day of the week. Patients admitted ‘out of hours’ (00:00–07:59 hours) received more physiotherapy and occupational therapy than those admitted during the day. Connected to this, an extended weekend service was associated with more physiotherapy and occupational therapy per day of stay. Also completion of timely assessments (within 72 hours of admission) for physical, occupational, and speech therapy was associated with more therapy.
The type of stroke team was another important factor. Patients treated by a specialist rehabilitation team received more therapy than those treated by a combined teams, both of which provided more therapy than acute stroke teams. For all four therapies, staffing levels (both qualified and support staff) were an important factor. For every additional staff member (work time equivalent (WTE)/10 beds) patients received 1.35, 3.45, 2.50, and 0.96 more minutes of physical, occupational and speech therapy, and psychology/day of stay, respectively, and 1.66, 1.15, 1.10, and 4.62 more minutes per WTE/10 beds of therapy support worker. Patients in teams with access to an Early Supported Discharge team received 1.56, 1.13, 1.38, and 0.37 more minutes of inpatient therapy per day of stay, while access to a Community Rehabilitation Team received 0.58, 0.21, 0.21, and 0.05 more minutes of inpatient therapy/day of stay than those without access to community teams.
Discussion
The results of this study revealed that most stroke patients receive little therapy and several individual and organizational factors were associated with the amount of therapy received. The amount of therapy was well below the recommended levels of 45 minutes of each relevant therapy per day even with adjustment for need and capacity.3 The frequency of therapy was also low. Given that the average length of stay for inpatients was 11 days, then most patients received very little therapy because the treatment was too short but also too infrequent.
Provision of clinical psychology was very limited. Only 5% were thought to need therapy, which generally consisted of a single assessment session lasting around 45 minutes. Given that the incidence of emotional and cognitive disorders after stroke is around 30%,13,14 this may suggest the need for psychology input is under-estimated, especially where services are not available. This is clearly a suboptimal situation with staffing levels for psychologists approximately half the levels recommended for hyper/acute stroke units in the National Clinical Guideline for Stroke.7 Improved access to psychological services has been raised as a priority by both the SSNAP7,8 and the Stroke Association.15 Our data further illustrate the urgency of this need.
Gender and ethnicity were found to influence the amount therapy received. Although these factors are unmodifiable, the way that these factors are managed can be modified and improved. The apparent disparities between ethnic minorities need to be treated with caution as the proportion of patients from ethnic minorities was small (~20%); however, our findings concur with a body of evidence that people from ethnic minorities often experience poorer care than the white population.16,17 Further research is needed to better understand the mechanisms behind these possible disparities and how to overcome them.
Several modifiable organizational factors were associated with the amount of therapy received. The day and time of admission may be considered unmodifiable, but the services received throughout the week are. Those admitted to hospital at the beginning of the week received the most therapy/day of stay. Several patterns of variation in the quality of stroke care during the week have been reported.18 Our findings expand these to include therapy. We postulate that the variability during the week seen here is a reflection of the availability of therapists which, for most inpatient services, is limited to the normal working week (8:30 a.m.–4:30 p.m., Monday–Friday). We found patients in a team providing an extended (weekend) therapy service tended to receive quicker assessment and more therapy/day of stay, which can reduce hospital length of stay and costs.19 Further research is needed to establish the most effective model of extended service including optimal skill mix and staffing levels. A key question is whether an effective extended service requires an increase in therapy staffing levels to cover the weekend input or whether spreading the existing therapy workforce to cover the whole week, but more thinly is adequate.
A further modifiable factor was inpatient staffing levels for both qualified and unqualified therapists and nurses. Previous studies have suggested that the amount of therapy received may be secondary to the way that staff workload is organized rather than staffing levels per se: teams which prioritize administration and non-direct contact over the face-to-face contact with patients tend to provide less therapy and may have poorer outcomes.5,10,20 This study is much larger than previous work and is the first study to show such a clear association between staffing and the amount of therapy. The way that stroke rehabilitation teams operate day-to-day has received little research attention and there has been little work to investigate, develop, or implement effective organization-level interventions as most research focusses on the clinical effectiveness of interventions on individual patients’ impairments and activities. Such research is clearly warranted, as is work to establish optimal staffing levels.
Further to staffing levels, the type of stroke team was also associated with the amount of therapy received. Specialist inpatient rehabilitation teams provided more therapy than combined stroke teams and all provided more therapy/day of stay than hyper-acute or acute stroke teams, even when case mix was accounted for. This is to be expected and probably reflects the priority given to rapid assessment and organization of early discharge over provision of ongoing ‘rehabilitation-focussed’ therapy during acute stroke care. This highlights the potential benefit of providing rehabilitation in a stand-alone specialist rehabilitation unit for patients who require ongoing rehabilitation and for whom early supported discharge is inappropriate. The implementation of specialist acute stroke services and centralized hyper-acute services has improved outcomes and the quality of acute stroke care,21 but the provision of inpatient stroke rehabilitation has been neglected.1,22 Further research is needed to investigate the optimal way to configure stroke rehabilitation services for patients with different needs and levels of ability.
Our findings indicate that the patients treated by an inpatient team with access to a community-based therapy team tended to receive more therapy/day of stay while an inpatient than those without access to community therapy. This may be considered counter-intuitive as many therapists consider lack of access to the community therapy to be a reason to extend inpatient stay so that patients can receive the therapy they need. However, this may represent patients who continue to receive therapy, while their discharge is delayed until a place with the community team became available.
Limitations
Any interpretation of factors associated here with the amount of therapy should be treated with caution. This is an exploratory investigation of a routinely collected observational data, thus no inference of causality can be made. Although SSNAP has stringent quality control processes, it is dependent on the accuracy of the original data entered and may be subject to observer and reporter bias. Inconsistencies in the way that therapists record therapy have been noted previously23 with a tendency to over-estimate the duration of treatment sessions, and so the accuracy of estimates of the amount of therapy should be treated with some caution. However, with such a large data set, any individual bias is unlikely to have a systematic effect. In addition, therapy is reported from the point of view of the therapists, meaning if a patient receives 1 hour of treatment three from three therapists working together, it would be reported as three hours of therapy. We also cannot make any comment on the structure or quality of the sessions being provided based on the information available.
Although we believe the classifications of stroke services and stroke severity used here to be valid, there may be some misclassification in terms of patient location, the designated type of stroke team, and stroke severity. Although our classifications were driven by the data in consultation with experts in the field, we understand any future work would be greatly improved if the stroke team in which the patient is located could be designated to reflect the care received by the patient throughout the inpatient care pathway (e.g. an hyper-acute, acute, combined, or rehabilitation units). Furthermore, the data set used in this project covered a period of change in UK stroke services with many being re-organized to deliver hyper-acute care and specialist community services. This means that some stroke teams may have changed classification during the study period. To prevent possible patient identification, the exact date of admission was not available and so the classification designated by SSNAP at the mid-point of the study (June 2014) was applied meaning potential misclassification in team type for patients admitted at a different time period. To reduce misclassification, an experienced member of the SSNAP team was consulted and the definitions we produced vetted; however, misclassification may still be present. In addition, there may have been classification errors in stroke severity using the NIHSS.
To focus on the clinically important effect, and not the statistical significance, we have reported the effect estimates and corresponding CIs. The large sample size and the large number of statistical tests will increase the presence of a statistically significant result even if a clinically significant one is not present. Although all analyses were preplanned, multiple testing may increase the likelihood of a statistically significant result. A Bonferroni adjustment was considered but if applied might increase a false-negative conclusion.24
In conclusion, the findings of this study indicate that increasing therapy and nursing staffing levels, extending the availability of therapy services outside ‘normal working hours’, and providing rehabilitation in specialist ‘stand-alone’ rehabilitation units could increase the amount of therapy provided. Further research is needed to establish how best to achieve this for patients with different levels of need and the impact of implementation.
Clinical messages.
Provision of greater amounts of stroke therapy is associated with
Higher therapy and nursing staffing levels;
A weekend therapy service;
Specialist stroke rehabilitation teams.
Supplemental Material
Supplemental material, Supplementary_Material for Factors influencing the amount of therapy received during inpatient stroke care: an analysis of data from the UK Sentinel Stroke National Audit Programme by Matthew Gittins, Andy Vail, Audrey Bowen, David Lugo-Palacios, Lizz Paley, Benjamin Bray, Brenda Gannon and Sarah Tyson in Clinical Rehabilitation
Acknowledgments
We thank the people and organizations participating in the Sentinel Stroke National Audit Programme (SSNAP). The authors acknowledge and thank Dr Martin James, Ms Alex Hoffman, and the Intercollegiate Stroke Working Party of the Sentinel Stroke National Audit Programme for their invaluable discussion and insights regarding interpretation of the results.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Professors Tyson, Vail, Bowen, and Dr Bray declare research grant funding from NIHR. Professor Tyson is currently a member of the Intercollegiate Stroke Working Party that produces SSNAP from which the SSNAPIEST data were drawn. Professor Bowen was also a member 2002–2016.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by the National Institute for Health Research (NIHR) under its Health Service and Development Research Programme (Grant Reference 14/198/09). The views expressed are those of the authors and not necessarily those of the NHS, NIHR, or the Department of Health and Social Care.
ORCID iD: Sarah Tyson  https://orcid.org/0000-0001-6301-8791
https://orcid.org/0000-0001-6301-8791
Supplemental material: Supplemental material for this article is available online.
References
- 1. Association S. State of the Nation: Stroke Statistics, 2020, https://www.stroke.org.uk/resources/state-nation-stroke-statistics (accessed May 2020).
- 2. Langhorne P, Collaboration SUT. Organized inpatient (Stroke Unit) care for stroke. Stroke 2014; 45(2): E14–E15. [Google Scholar]
- 3. Physicians RCo. Sentinel stroke national audit programme (SSNAP) Clinical audit July-Sept 2014 Public Report, 2015, https://www.strokeaudit.org/Documents/National/Clinical/JulSep2014/JulSep2014-PublicReport.aspx (accessed October 2018).
- 4. Pound P, Gompertz P, Ebrahim S. Patients’ satisfaction with stroke services. Clinical Rehabilitation Clin Rehabil 1994; 8(1): 7–17. [Google Scholar]
- 5. De Wit L, Putman K, Schuback B, et al. Motor and functional recovery after stroke: a comparison of 4 European rehabilitation centers. Stroke 2007; 38(7): 2101–2107. [DOI] [PubMed] [Google Scholar]
- 6. Clarke DJ, Burton LJ, Tyson SF, et al. Why do stroke survivors not receive recommended amounts of active therapy? Findings from the ReAcT study, a mixed-methods case-study evaluation in eight stroke units. Clin Rehabil 2018; 32(8): 1119–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Physicians RCo. Sentinel Stroke National Audit Programme (SSNAP) Acute care organisational audit 2017, https://www.strokeaudit.org/results/Clinical-audit.aspx (accessed June 2019).
- 8. Physicians RCo. Sentinel Stroke National Audit Programme (SSNAP) Acute care organisational audit 2014, https://www.strokeaudit.org/results/Organisational.aspx (accessed March 2018).
- 9. Physicians RCo. Sentinel Stroke National Audit Programme (SSNAP) Post –acute care organisational audit 2015, https://www.strokeaudit.org/results/PostAcute/National.aspx (accessed March 2018).
- 10. Brott T, Adams HP, Jr, Olinger CP, et al. Measurements of acute cerebral infarction – a clinical examination Scale. Stroke 1989; 20(7): 864–870. [DOI] [PubMed] [Google Scholar]
- 11. Stata Statistical Software: Release 15 [program]. College Station, TX: Statacorp LLC, 2017. [Google Scholar]
- 12. Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical models. Cambridge: Cambridge University Press, 2007. [Google Scholar]
- 13. Hackett ML, Anderson CS. Frequency, management, and predictors of abnormal mood after stroke: the Auckland Regional Community Stroke (ARCOS) study, 2002 to 2003. Stroke 2006; 37(8): 2123–2128. [DOI] [PubMed] [Google Scholar]
- 14. Rist PM, Chalmers J, Arima H, et al. Baseline cognitive function, recurrent stroke, and risk of dementia in patients with stroke. Stroke 2013; 44(7): 1790–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stroke Association. Feeling overwhelmed: the emotional impact of stroke, 2013, https://www.stroke.org.uk/sites/default/files/feeling_overwhelmed_final_web_0.pdf (accessed January 2020).
- 16. Bhandari VK, Kushel M, Price L, et al. Racial disparities in outcomes of inpatient stroke rehabilitation. Arch Phys Med Rehabil 2005; 86(11): 2081–2086. [DOI] [PubMed] [Google Scholar]
- 17. Roth DL, Haley WE, Clay OJ, et al. Race and gender differences in 1-year outcomes for community-dwelling stroke survivors with family caregivers. Stroke 2011; 42(3): 626–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bray BD, Cloud GC, James MA. Weekly variation in health-care quality by day and time of admission: a nationwide, registry-based, prospective cohort study of acute stroke care. Lancet 2016; 388(10040): 170–177. [DOI] [PubMed] [Google Scholar]
- 19. English C, Shields N, Brusco NK, et al. Additional weekend therapy may reduce length of rehabilitation stay after stroke: a meta-analysis of individual patient data. J Physiother 2016; 62(3): 124–129. [DOI] [PubMed] [Google Scholar]
- 20. De Wit L, Putman K, Lincoln N, et al. Stroke rehabilitation in Europe: what do physiotherapists and occupational therapists actually do. Stroke 2006; 37(6): 1483–1489. [DOI] [PubMed] [Google Scholar]
- 21. Morris S, Hunter RM, Ramsay AIG, et al. Impact of centralising acute stroke services in English metropolitan areas on mortality and length of hospital stay: difference-in-differences analysis. BMJ 2014; 349: g4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rudd AG, Hoffman A, Paley L, et al. 20 years of researching stroke through audit. Clin Rehabil 2018; 32(8): 997–1006. [DOI] [PubMed] [Google Scholar]
- 23. Kaur G, English C, Hillier S. Physiotherapists systematically overestimate the amount of time stroke survivors spend engaged in active therapy rehabilitation: an observational study. J Physiother 2013; 59(1): 45–51. [DOI] [PubMed] [Google Scholar]
- 24. Sterne JAC, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009; 338: b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_Material for Factors influencing the amount of therapy received during inpatient stroke care: an analysis of data from the UK Sentinel Stroke National Audit Programme by Matthew Gittins, Andy Vail, Audrey Bowen, David Lugo-Palacios, Lizz Paley, Benjamin Bray, Brenda Gannon and Sarah Tyson in Clinical Rehabilitation


