Abstract
Objective
To investigate the psycho-social factors associated with COVID-19 and the nationwide lockdown in India.
Study design
An online survey was conducted from April 11 through April 16, 2020 in 28 states and 8 union territories (UT) of India. The potential participants were recruited using snowball sampling procedure.
Methods
A cross-sectional online survey was conducted among the people of all states in India. A spatial analysis was performed and Moran's I statistic was applied to investigate the overall clustering of locations. Fisher's exact test was used to investigate associations. GeoDa and R console were used to analyze the data. A total of responses were received.
Results
Those worried for their family's health were likely to follow the lockdown measuresSignificant association was observed between following the lockdown measures and being satisfied with the government strategy to combat the COVID-19 pandemic. A significant relation was observed between the gender (p = 0.001), job profile and physical activity were observed to be associated with the psycho-social impact.
Conclusion
Government and public health officials should consider the sentiments of the community while planning strategies relating to the pandemic. The findings of this study will assist the policymakers in emphasizing the psychological well-being of individuals, along with physical health.
Keywords: SARS CoV-2, Corona virus, COVID-19, Psycho-social impact, Stress, Spatial
1. Introduction
Coronavirus Disease-2019 (COVID-19)is a public health emergency of international concern firstly reported in Wuhan, China in December 2019.1 The virus was named as severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) by the International Committee on Taxonomy of Viruses.2 It is defining the global health crisis and the global economic crisis of time the world has faced after many decades. Ever since its appearance in December 2019, the virus has proliferated to every continent, excluding Antarctica.3 Manifestations of this infectious disease include fever, tiredness, dry cough, and other symptoms include shortness of breath, aches and pains, sore throat, and fewer people will suffer from diarrhea, nausea, and running nose.4 Patients developing the extreme form of this disease constitute approximately 15% of the cases.
According to the WHO (World Health Organization) report 2020,5 almost 30% of the nations have no preparedness and response plans towards COVID-19 spread. Only a few countries have comprehensive infection prevention and control program along with water, sanitation, and hygiene standards in health-care facilities.6 In the absence of COVID-19 vaccine, maintaining social and physical distancing aims to slow down the spread of this infectious disease by interrupting the chains of transmission of COVID-19. These measures include physical distance among people (of at least 1 m) and minimize contact with infected surfaces while stimulating and sustaining active social connections within households and communities. Tele working, online learning, minimizing and avoiding crowding7 are some of the measures for the general public to engage themselves.
Public health policies requires an exceptional equilibrium between protecting the physical as well as psychological health.8 The severe acute respiratory syndrome (SARS) outbreak in 2003 indicates that infectious diseases are linked with a high level of panic emotion among the population, which further complicates in preventing the spread of the disease.9 Pandemics such as COVID-19excessively publicized in the mass media and can be associated with high levels of stress & anxiety.10 Individuals may experience distress from quarantine, lockdown, travel restrictions, side effects of treatment, or fear of the infection itself. Those who are living alone currently not able to meet their parents or family might develop mild to moderate depression.11 Older adults are also at risk of being not able to visit hospital/healthcare facilities because of not having transportation and postponing their visits to physicians.12 Few might go through withdrawal symptoms because of the sudden stopping of alcohol and other drugs.13 Uncertainty of future because of this pandemic can cause post-traumatic stress disorder, prolonged grief reaction and guilt remorse followed by loss of the loved ones because of this pandemic, loss of job leading to the financial crisis which can lead to a higher number of committing suicides in days to come.14 Stress, anxiety and depression are predators of diseases like hypertension, diabetes and depression.15 It also causes accelerated aging (approximately 9-17 years) and premature death.16
Spatial analysis is crucial in identifying the local occurrences and mapping the spread of any condition will help in formulation of public health policies at an early stage.17 , 18 The physiological processes in India have not received the attention it deserves from medical and public health fraternity. To the best of our knowledge, presenting the geographical distribution of the psycho-social impact due to COVID-19 and lockdown among Indian residents has not been previously reported. The main aim of this study is to investigate the psycho-social factors associated with COVID-19 and the nationwide lockdown in India employing the spatial analysis. The present study identifies the locations requiring special attention of the public health workers and the administrators in order to retain the positivity and hope in this public health crisis like situation.
2. Methods
An online survey was conducted from April 11 through April 16, 2020 in 28 states and 8 union territories (UT) of India. The potential participants were recruited using snowball sampling procedure. A google form was created in the English language with relevant 20 items, including demographic variables, basic knowledge on COVID-19, perspective on the complete lockdown, and stress related to the pandemic spread leading to lockdown in India. The google form included a basic description of the purpose for which this survey was conducted. Potential participants received the google form link along with the description and purpose of this study, either through mail or social media platforms. Informed consent was obtained from all individual participants included in the study. Ethical approval for survey research in the pandemic situation was obtained from Institutional Research Board of Indian Institute of Health Management Research University, Jaipur, In-principle. No personal identifiers were collected in the form and confidentiality of the responses are maintained.
3. Measures
3.1. Outcome
The primary outcome (psycho-social (PS) impact) is a composite score assessed based on the participant's responses to the following five questions, “Do you get upset by thinking about COVID-19?” (Not at all 0; Yes, sometimes 1; Yes, often 2; Always 3), “Do you get panic and overreact to news relating to COVID-19” (Not at all 0; Yes, sometimes 1; Yes, often 2; Always 3), “Are you worried about losses/your job during the lockdown?” (Not at all 0; Yes, little 1; yes, a lot 2), “Do you get worried about your family's health more than usual?” (Not at all 0; Sometimes 1; Often 2) “Are you sleeping more/less than you normally do?” (I sleep as usual 0; more than usual 1; less than usual 2). The plausible range of PS score is zero to twelve. Under an assumption that everyone is having an impact, the individuals who scored between 0 and 5, 6–7, and 8–12 were considered to have a mild, moderate, and severe psycho-social impact.
3.2. Other characteristics
Characteristics including the state they currently stay, residential area (urban; rural), age (in years), gender (male; female; prefer not to say), occupation (Salaried–Private; Salaried-Government; Contractual; Healthcare; Daily wage; Business/Entrepreneur; Students; Housewife; Retired; Unemployed; Others), and educational qualification (up to secondary; secondary to graduate; postgraduate and above) were collected. The participant's perception of lockdown and whether they follow it or not was reviewed using the following questions, “Are you following the lockdown measures?” (Yes, always; Yes, sometimes; No) “For what you step out of the house during the lockdown?” (Grocery/Kirana Store/Vegetable & Fruit Shops; Hospital and other healthcare facilities; Bank; Office/For work; For socializing; Physical activity; I do not go out at all), “Do you think lockdown can prevent community spread of COVID-19 in India?” (Yes; No; Maybe).
Apart from the above-listed, few more questions on awareness regarding COVID-19 were asked viz. “Which among the following are true about COVID -19?” (It is a viral infection spread by coughing or sneezing; Fever, fatigue, cough, and breathing difficulty are symptoms; It is a deadly disease; All of the above; None of the above), “What are the preventive measures against the spread of COVID-19?” (Sanitizing/washing hands regularly for at least 20 s; Social distancing; Practice respiratory hygiene; All of the above). Additionally, two more questions asked were, “Are you satisfied by the government's strategy to combat this pandemic?” (Yes, No, maybe) and “Are you able to do indoor physical activity?” (Daily; Twice-a-week; Rarely; Not at all).
3.3. Statistical analysis
The quantitative measures were summarized using ‘mean ± standard deviation (min, max)’.The qualitative response was summarized using frequency and percentages. Fisher's exact test was used to investigate associations. R console was used to analyze the data. A was considered significant throughout. A choropleth map was used to present the state-wise descriptive plot relating to lockdown measures and the psycho-social impact due to. Spatial analysis plays a vital role in analyzing the data and presenting the hotspots and other essential clusters. Moran's I statistic was used to investigate the overall clustering in locations.19 Upon investigation, in the presence of spatial autocorrelation, the local measure of spatial association was employed to reveal the clusters.
For employing the spatial analysis, eight individual-level measures from the data were aggregated to the state level. The eight lockdown and psycho-social measures were converted to a percentage of respondents, who follow the lockdown measures (follow lockdown), who are satisfied with the government strategy to combat the pandemic(satisfied with government strategy), who think lockdown can prevent the spread of this pandemic (lockdown can prevent the spread), who are worried about losses/your job during the lockdown (worried about loss/job), who get upset by thinking aboutCOVID-19 (upset due toCOVID-19), who get panic and overreact to news relating to COVID-19 (panic and overreact to news), who get worried about our family's health more than usual (worried of family health), and who sleep as usual (Sleep as usual). The data were merged into the shapefile and analyzed using GeoDa software.
4. Results
A total of responses were received out of which majority were from Karnataka), Delhi), UP, Kerala, Assam and Bihar each. The data from Andaman & Nicobar Island, Daman and Diu, Dadra and Nagar Haveli and Lakshadweep were not received and hence are not analyzed. Data were visualized, and numerical summaries were obtained to explore mistakes, if any. In the question relating to age, one of the entries was ‘three’ years, and was excluded from the analysis considering it to be an entry mistake. The respondents were age 30 ± 9 years. A total of responses were from the rural residents in India. of the respondents were male, and preferred not to disclose their gender. of the respondents were educated up to secondary. had attained postgraduate and higher education qualification. The majority of respondents were salaried, student, healthcare worker and businessman/entrepreneur.
Among the respondents, were following the lockdown measures always, whereas were reportedly not following the measures at all. Among those who don't follow the lockdown measures at all, are stepping out of the house to reach their office and are visiting a hospital and other healthcare facilities. All five individual stepping out of the house to visit either a healthcare facility or their respective offices, were observed to have a sound idea on prevention from COVID-19 and its symptoms. Out of individuals who don't go out at all, were student, were salaried-private/semi-government. Worrying for the health of family members and following the lockdown measures were found to be associated Out of all who worry about their family's health more than usual, almost follow the lockdown measures always.
A total of 1045 (79.41%) out of 1316 knew all the three preventive measures necessary against COVID-19 spread. The majority of the respondents (n = 909, 69.07%) knew all the symptoms of COVID-19. It is to be noted than 14 (1.06%) were not aware of any symptoms relating to COVID-19. Over 102 (7.83%) reported that only fever, fatigue, cough, and breathing difficulty are the symptom of COVID-19. Another 33 (2.51%) knew that it is a deadly disease. COVID-19 is a viral infection spread by coughing, and sneezing was reported by 131 (9.95%) of the respondent. There were several mixed responses too, where more than one right symptom was chosen but not all.
A significant relationship was observed between following the lockdown measures and being satisfied with the government strategy to combat the COVID-19 pandemic. Out of all who don't follow the lockdown measures were not satisfied by the government's strategy. In contrast, those who follow the measures always were not satisfied by the government's strategy to combat the pandemic. The PS impact score was as assessed using complete responses. The categorized PS score revealed that had mild, whereas had a moderate level of impact. Almost of the respondents had a major PS impact.
Further investigations on the association of gender, job profile, physical activity, following lockdown measures, believing in lockdown being able to prevent the spread, and satisfaction with the government measures to combat the pandemic with the PS impact revealed notable findings as presented in Table 1 .
Table 1.
Associations of socio-demographic and lockdown measures with the psycho-social impact of COVID-19 pandemic, India.
| Characteristics | Psycho-socio impact | p- value | ||||
| Mild | Moderate | Severe | ||||
| Socio-demographic | Age (in years) Mean ± standard deviation | 30 ± 10 | 29 ± 9 | 30 ± 10 | 0.484 | |
| Gender | Male | 363 (57.3) | 196 (48.6) | 118 (43.2) | 0.001 | |
| Female | 267 (42.1) | 205 (50.9) | 152 (55.7) | |||
| Prefer not to say | 4 (0.6) | 2 (0.5) | 3 (1.1) | |||
| Job profile | Salaried- Government | 86 (13.6) | 55 (13.6) | 14 (5.1) | <0.001 | |
| Salaried- Private/Semi-government | 186 (29.3) | 116 (28.8) | 63 (23.1) | |||
| Student | 175 (27.6) | 108 (26.8) | 76 (27.8) | |||
| Unemployed | 17 (2.7) | 12 (3.0) | 6 (2.2) | |||
| Healthcare | 90 (14.2) | 48 (11.9) | 28 (10.3) | |||
| Housewife | 19 (3.0) | 17 (4.2) | 23 (8.4) | |||
| Contractual | 14 (2.2) | 13 (3.2) | 11 (4.0) | |||
| Business/Entrepreneur | 27 (4.3) | 25 (6.2) | 43 (15.8) | |||
| Daily wage | 1 (2.0) | 1 (2.0) | 1 (4.0) | |||
| Retired | 6 (0.9) | 1 (0.2) | 2 (0.7) | |||
| Others | 11 (1.7) | 7 (1.7) | 6 (2.2) | |||
| Physical activity | Not at all | 57 (9.0) | 40 (9.9) | 48 (17.6) | <0.001 | |
| Rarely | 169 (26.7) | 162 (40.2) | 124 (45.4) | |||
| Twice a week | 73 (11.5) | 48 (11.9) | 23 (8.4) | |||
| Daily | 335 (52.8) | 153 (38.0) | 78(28.6) | |||
| Lockdown Measures | Follow lockdown | No | 07 (1.1) | 1 (0.2) | 0(0.0) | 0.002 |
| Yes, sometimes | 28 (4.4) | 34 (8.4) | 26 (9.5) | |||
| Yes, always | 599 (94.5) | 368 (91.3) | 246 (90.1) | |||
| Satisfied with government strategy | Yes | 496 (78.5) | 309 (76.9) | 206 (75.5) | 0.282 | |
| No | 43 (6.8) | 35 (8.7) | 32 (11.7) | |||
| May be | 92 (14.7) | 58 (14.4) | 35 (12.8) | |||
| Lockdown can prevent the spread | Yes | 550 (86.8) | 343 (85.1) | 228 (83.5) | 0.238 | |
| No | 17 (2.7) | 16 (4.0) | 16 (5.9) | |||
| Maybe | 67(10.6) | 44 (10.9) | 29 (10.6) | |||
Table 1 Associations of socio-demographic and lockdown measures with the psycho-social impact of COVID-19 pandemic, India.
Individuals with mild PS impact are likely males, those who always follow the lockdown measures, and those who do indoor physical activity daily. Gender of participants, following lockdown, and physical activity were significantly associated with the PS impact, as presented in Table 1.
4.1. Spatial analysis
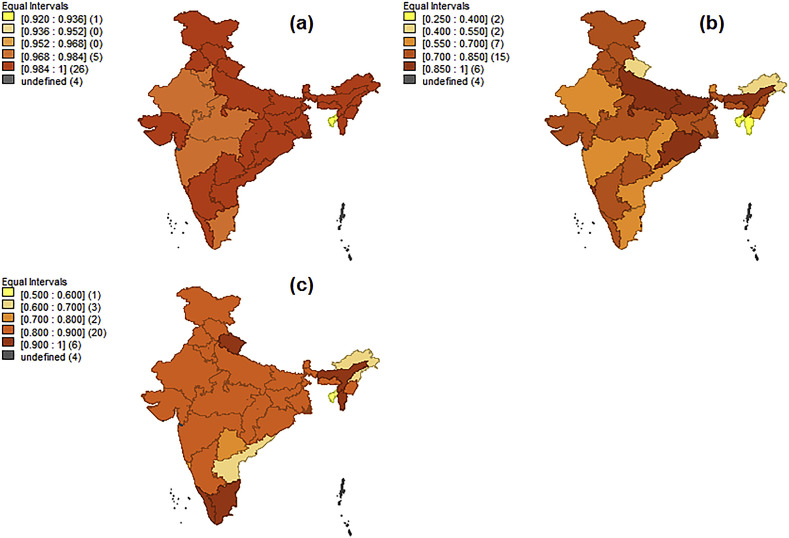
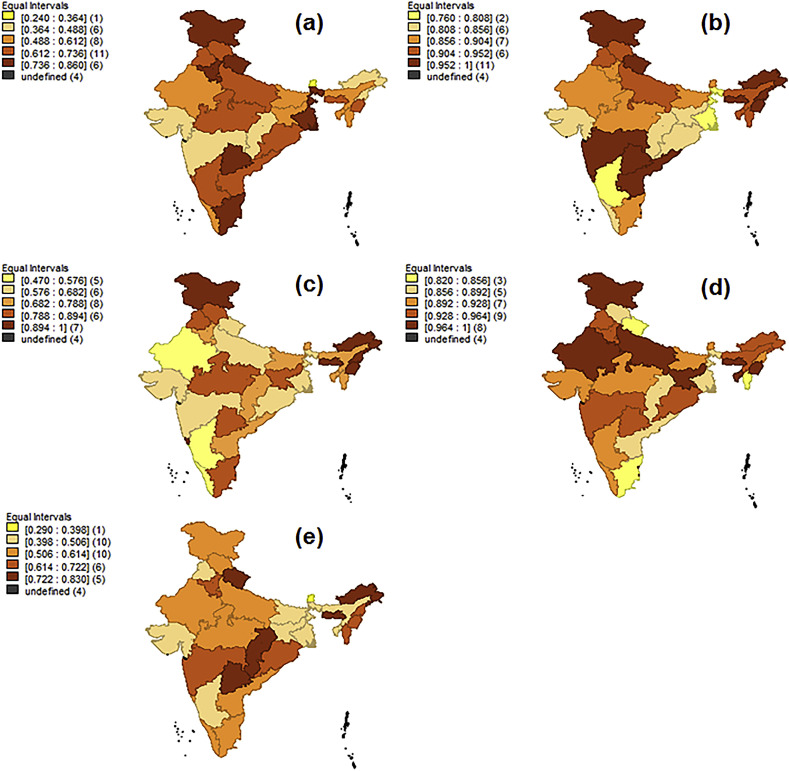
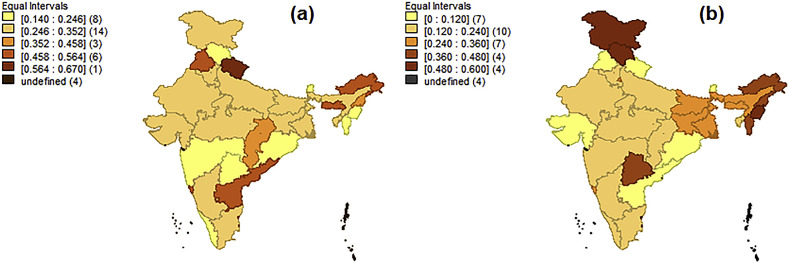
Six out of the eight aggregated measures reveal almost negligible Moran's I value. The negligible Moran's I value highlights the absence of spatial autocorrelation. The two measures which showed relatively high Moran's I statistic were ‘percentage of respondents who get upset by thinking about COVID-19 and ‘percentage of respondents who get worried about our family's health more than usual’. However, reporting a local measure when I is less than is not found suitable. A choropleth map describing the measures relating to complete lockdown is presented in Fig. 1 , whereas the psycho-social measures and impact of COVID-19 illustrated in Fig. 2 and Fig. 3 respectively. The eight lockdown and psycho-social impact measures examined in the presented study are described in Table 2 .
Fig. 1.
Choropleth maps describing the percentage of participants (a) following lockdown (b) satisfied by the government policy (c) believing lockdown can prevent form COVID-19, India, 2020.
Fig. 2.
Illustrating the geographical distribution of psycho-social measures (a) worried about loss/job (b) upset due to COVID-19 (c) Panic and overreact to news (d) Worried about family health (e) Sleep as usual, of COVID-19 in India, 2020.
Fig. 3.
Illustrating the geographical distribution of states with (a) moderate and (b) severe psycho-social impact of COVID-19 in India, 2020.
Table 2.
Descriptive of lockdown and psycho-social measures due toCOVID-19 pandemic, India.
| Characteristics | Mean Prevalence (95% CI) ∗ | Least prevalent state, the prevalence | Most prevalent state, the prevalence | |
|---|---|---|---|---|
| Lockdown Measures | follow lockdown | 0.993(0.988,0.998) | Tripura, 0.92 | Sikkim, Punjab, Assam, Gujarat, Chandigarh, West Bengal, Jharkhand, Puducherry, NCT of Delhi, Kerala, Goa, Uttar Pradesh, Himachal Pradesh, Jammu & Kashmir, Andhra Pradesh, Odisha, Mizoram, Nagaland, Manipur, Chhattisgarh, Meghalaya, Arunachal Pradesh, Telangana, Uttarakhand, 1.00 |
| Satisfied with government strategy | 0.721(0.667,0.772) | Tripura, 0.25 | Puducherry, 1.00 | |
| lockdown can prevent the spread | 0.836(0.801,0.868) | Tripura, 0.5 | Uttarakhand, Puducherry, 1.00 | |
| Psycho-socio measures | worried about loss/job | 0.613(0.564,0.661) | Sikkim, 0.24 | J&K, 0.86 |
| upset due to | 0.910(0.887, 0.931) | West Bengal, 0.76 | Arunachal Pradesh, Nagaland, Puducherry, Goa, Manipur, Meghalaya, Uttarakhand, Jammu & Kashmir, 1.00 | |
| Panic and overreact to news | 0.754(0.703,0.806) | Chandigarh, 0.47 | Arunachal Pradesh, Nagaland, Puducherry, Goa, Manipur, Jammu & Kashmir, 1.00 | |
| Worried about family health | 0.928(0.910,0.946) | Mizoram, 0.82 | Tripura, Jharkhand, Meghalaya, Puducherry, Manipur, Jammu & Kashmir, 1.00 | |
| Sleep as usual | 0.569(0.525,0.613) | Sikkim, 0.29 | Uttarakhand, 0.83 | |
BCa (Bias corrected accelerated) confidence interval was obtained using 1000 bootstrap samples; CI: Confidence Interval.
Table 2 Descriptive of lockdown and psycho-social measures due toCOVID-19 pandemic, India.
5. Discussion
In the present study,92.6% of the respondents were following the lockdown measures, which is a very important step to minimize the spread of COVID-19. An analytical study conducted in India also signifies that lockdown and social distancing will only aid in the prevention of this pandemic.20 The present study had similar findings as there was a significant association between following lockdown measures and government strategy to combat this pandemic. A significant association among worrying for the health of family members and supporting the lockdown measures has been observed. A recent study from the United Kingdom had similar findings emphasizing that people are more worried about their family and economic condition due to the pandemic spread.21
Moreover, the findings reveal that 79.41% of the people had a sound knowledge about the symptoms of COVID-19. Studies reveal that excellent awareness and knowledge among people will help in reducing the initial number of cases making the outbreak easier to control.22 It has been observed that the majority of those having severe stress do indoor physical activities rarely. Physical activity promotes well-being and recovery from stress.23 , 24 The present study also reports that people in the state of Tripura were not following the lockdown measures, and they were not satisfied with the government measures. Tripura is a state in north-east India with very few numbers of COVID-19 confirmed cases. A study conducted in Tripura concludes preventive measures to be best to tackle this pandemic, which contrasts the presented study finding.25 People of Sikkim were least worried while those in Jammu & Kashmir were highly stressed about the losses and jobs. In most of the Northeastern states, along with Jammu & Kashmir, people were stressed and were overreacting to the situation. The distress could be because of the inequity in healthcare in these states concerning many determinants.26 , 27 However, respondents from ten states and one UT have been observed not in stress due to COVID-19 and related lockdown measures. Respondents from twenty states and four UT have confirmed following the complete lockdown measures and the majority of them were also satisfied with government strategies.
5.1. Significance of the study
Controlling the spread of COVID-19 requires a comprehensive strategy, which the Indian government has managed well so far. However, the pandemic seems to affect the masses indirectly by creating a psycho-social impact due to the growing concern about their losses, job, health, and family. Moreover, these factors might have a long-term influence on wellbeing of the community.
5.2. Limitations
Despite several advantages, there are few limitations of the present study, including less participation from the areas with limited internet facilities. Demerits of an online survey are also limitations of the presented study. However, in this pandemic situation, an online survey was the only alternative to grasp the notion of the residents of India.
6. Conclusion
Nationwide lockdown measures have been followed by the majority of states in India. Tailored intervention should be innovated for states requiring more attention. Government and public health officials should consider the sentiments of the community while planning strategies relating to the pandemic. The findings of this public data driven study will provide some insights to the policymakers in emphasizing the psychological well-being of individuals, along with physical health. Decision makers must come up with customized interventions for those affected due to staying alone, idle, loss of job, salary cut, and are worried about family's well-being. It will also assist health care providers (e.g., psychologists and psychiatrists) to offer timely services to the people of selected locations.
Authors contributions
NN and BT contributed to the study conception and material preparation. Design, data collection and analysis were performed by PKP, BT and NN respectively. SK wrote the manuscript. All authors read and approved the manuscript.
Funding
This research received no external funding.
Ethical approval
Ethical approval for survey research in the pandemic situation was obtained from Institutional Research Board of Indian Institute of Health Management Research, IIHMR University, Jaipur, In-principle.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
Authors are grateful to Dr. Shwetha TS (Assistant Professor, Department of Clinical Psychology, Manipal College of Health Professions, Manipal, Karnataka) for providing insightful knowledge and proof reading this article. Authors are also thankful to each and every participant & individual engaged directly or indirectly with this study.
References
- 1.Bian X., Wang L., MacAlpine J.M., Guan Z., Hui J., Chen Y. Positive corona inception voltages and corona currents for air at various pressures and humidities. IEEE Trans Dielectr Electr Insul. 2010 Feb 17;17(1):63–70. [Google Scholar]
- 2.World Health Organization . World Health Organization; 2020. Coronavirus.https://www.who.int/health-topics/coronavirus cited january 19. Available. [Google Scholar]
- 3.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama. 2020 Feb 24 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 4.Norris SL. WHO and Rapid Advice Guidelines: History and Future Directions.
- 5.NUMBERS S.I., ASSESSMENT W.R. Coronavirus disease 2019 (COVID-19) Americas. 2020 Mar 23;10(2):1. [Google Scholar]
- 6.Usher A.D. WHO launches crowdfund for COVID-19 response. Lancet. 2020 Mar 28;395(10229):1024. doi: 10.1016/S0140-6736(20)30719-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. reportCoronavirus Disease 2019 (COVID-19): Situation Report, 72.
- 8.Tao N. An analysis on reasons of SARS-induced psychological panic among students. J Anhui Inst Educ. 2003;21:78–79. [Google Scholar]
- 9.Person B., Sy F., Holton K., Govert B., Liang A. Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis. 2004 Feb;10(2):358. doi: 10.3201/eid1002.030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognit Ther Res. 2012 Jun 1;36(3):210–218. [Google Scholar]
- 11.Diamond G.S., Reis B.F., Diamond G.M., Siqueland L., Isaacs L. Attachment-based family therapy for depressed adolescents: a treatment development study. J Am Acad Child Adolesc Psychiatr. 2002 Oct 1;41(10):1190–1196. doi: 10.1097/00004583-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Armitage R., Nellums L.B. COVID-19 and the consequences of isolating the elderly. Lancet Publ Health. 2020 Mar 19 doi: 10.1016/S2468-2667(20)30061-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duka T., Gentry J., Malcolm R., et al. Consequences of multiple withdrawals from alcohol. Alcohol Clin Exp Res. 2004 Feb;28(2):233–246. doi: 10.1097/01.alc.0000113780.41701.81. [DOI] [PubMed] [Google Scholar]
- 14.Fountoulakis K.N., Grammatikopoulos I.A., Koupidis S.A., Siamouli M., Theodorakis P.N. Health and the financial crisis in Greece. Lancet. 2012 Mar 17;379(9820):1001–1002. doi: 10.1016/S0140-6736(12)60422-X. [DOI] [PubMed] [Google Scholar]
- 15.Fearon I.M., Faux S.P. Oxidative stress and cardiovascular disease: novel tools give (free) radical insight. J Mol Cell Cardiol. 2009 Sep 1;47(3):372–381. doi: 10.1016/j.yjmcc.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 16.Bustos-Obregón E, Esponda P. Ageing Induces Apoptosis and Increases HSP70 Stress Protein in the Epididymis of Octodon degus.
- 17.Nilima Nilima, Kamath A., Shetty K., Unnikrishnan B., Kaushik S., Rai S.N. Prevalence, patterns, and predictors of diarrhea: a spatial-temporal comprehensive evaluation in India. BMC Public Health. 2018 Dec 1;18(1):1288. doi: 10.1186/s12889-018-6213-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.John A.E., Nilima, Binu V.S., Unnikrishnan B. Determinants of antenatal care utilization in India: a spatial evaluation of evidence for public health reforms. Public Health. 2019 Jan 1;166:57–64. doi: 10.1016/j.puhe.2018.09.030. [DOI] [PubMed] [Google Scholar]
- 19.Nilima Puranik A., Shreenidhi S.M., Rai S.N. Spatial evaluation of prevalence, pattern and predictors of cervical cancer screening in India. Public Health. 2020 Jan 1;178:124–136. doi: 10.1016/j.puhe.2019.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Y., Jiang B., Yuan J., Tao Y. The impact of social distancing and epicenter lockdown on the COVID-19 epidemic in mainland China: a data-driven SEIQR model study. medRxiv. 2020 Jan 1 [Google Scholar]
- 21.Kleinberg B., van der Vegt I., Mozes M. 2020 Apr 8. Measuring Emotions in the COVID-19 Real World Worry Dataset. arXiv preprint arXiv:2004.04225. [Google Scholar]
- 22.Hellewell J., Abbott S., Gimma A., et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020 Feb 28 doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hansmann R., Hug S.M., Seeland K. Restoration and stress relief through physical activities in forests and parks. Urban For Urban Green. 2007 Nov 15;6(4):213–225. [Google Scholar]
- 24.Haskell W.L., Montoye H.J., Orenstein D. Physical activity and exercise to achieve health-related physical fitness components. Publ Health Rep. 1985 Mar;100(2):202. [PMC free article] [PubMed] [Google Scholar]
- 25.Jahangir M.A., Muheem A., Rizvi M.F. Coronavirus (COVID-19): history, current knowledge and pipeline medications. Int J Pharm Pharmacol. 2020;4:140. doi: 10.31531/2581.2020. 3080(2) [DOI] [Google Scholar]
- 26.World Health Organization . WHO Regional Office for South-East Asia; 2008. Social Determinants of Health. [Google Scholar]
- 27.Joe W., Mishra U.S., Navaneetham K. Health inequality in India: evidence from NFHS 3. Econ Polit Wkly. 2008 Aug 2:41–47. [Google Scholar]