One of the primary reasons for high mortality in the advanced-stage coronavirus disease-2019 (COVID-19) patients is the uncontrolled inflammation in the lungs leading to acute respiratory distress syndrome (ARDS). Controlling the pathological inflammation in the ARDS lungs without compromising the immune system’s fight against the virus is indeed a daunting task. In this situation, an appropriate therapeutic target would be the one that will not only reverse the damaging inflammation and promote resolution but also helps to check the root cause of the virus infection. Akt is a potential therapeutic target for the advanced-stage COVID-19 patients; its inhibition will potentially suppress the pathological inflammation, cytokine storm, fibroproliferation, and platelet activation associated with COVID-19, and at the same time prevent scarring and promote resolution in injured lungs. As pharmacological inhibition of Akt has also been reported to inhibit angiotensin-converting enzyme 2 (ACE2) expression, a receptor for the virus entry into the lung cells, targeting Akt for COVID-19 looks a viable option.
Severe acute respiratory syndrome (SARS), an acute respiratory distress syndrome (ARDS) caused by the coronavirus-2 (SARS-CoV-2), is the primary reason for high mortality associated with coronavirus disease-2019 (COVID-19) (25). The prolonged asymptomatic incubation period in COVID-19 patients ranging between 1 and 14 days (5.1 days median) is a major bottleneck in its early detection and preventing it from infecting the lungs of some patients (12). Additionally, comorbidities such as diabetes and hypertension (10, 24) and a history of medications such as angiotensin receptor blockers (ARBs) and angiotensin-converting enzyme (ACE) inhibitors (9) further worsens the COVID-19 associated ARDS. The effect of comorbidities (14) and the use of cardiovascular medications (19) are believed to be due to the increased expression of ACE2, a putative receptor for SARS-CoV-2 (23). As current treatment options for ARDS are very limited (21, 22), treating advanced COVID-19 patients is a bigger challenge due to the reasons above.
Early detection and preventing a lung infection would be the most desirable approach to treat COVID-19 patients. Although some COVID-19 patients present early symptoms, many patients harboring SARS-CoV-2 remain on a long asymptomatic period and are undetected until complications arise (10, 12). Having a large population suffering from metabolic diseases and hypertension in Western countries (17), the potential risk of COVID-19 associated ARDS is also higher. Hence, it is not always possible to cure COVID-19 patients before severe lung infection takes hold. The next obvious question is, how do we treat advanced-stage COVID-19 patients with lung infections? One potential option would be to target ACE2 or pathways promoting ACE2 expression or activation. Alternately, COVID-19 patients can also be treated by engineered peptides, antibodies, or compounds to disrupt or prevent the interaction between SARS-CoV-2 spike protein and ACE2 (23) that will prevent reinfections and limit the lung damage. A better option to manage advanced-stage COVID-19 patients would be a drug that can not only suppress inflammation but also promote the resolution of lung injury and prevent scarring (Fig. 1).
Fig. 1.
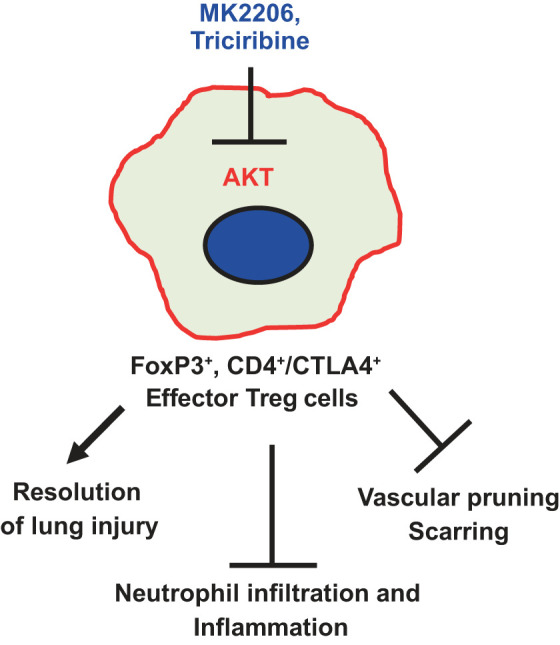
Akt inhibition will increase the number of CD4+/FoxP3+/CD103+/CTLA4+ effector regulatory T cells (Tregs) in the acute respiratory distress syndrome (ARDS) lung to suppress inflammation and promote injury resolution. In the ARDS lung, reduced Akt activity in conventional T cells will promote their differentiation to effector Tregs, limiting inflammation and scar formation, and promoting vascular regeneration and wound resolution, revealing the potential therapeutic benefits of Akt inhibitors such as triciribine and MK2206 to treat ARDS in advanced-stage coronavirus disease-2019 (COVID-19) patients.
The phosphoinositide 3 (PI3)-kinase/Akt pathway promotes inflammation in several disease states (8). Whereas genetic deletion of Akt1 gene reduced inflammation and improved cardiac function in mice following myocardial ischemia (13, 16), pharmacological Akt inhibition suppressed inflammation in mice, myofibroblast differentiation, and prevented vascular rarefaction to halt pulmonary fibrosis progression (1, 2). Furthermore, whereas Akt1 deficiency in macrophages resulted in reduced foam cell formation (13), inhibition of phosphatase and tensin homolog deleted on chromosome 10 (PTEN) leading to Akt activation in the regulatory T cells (Tregs) promoted inflammation (18). Adoptive transfer of Tregs has demonstrated to suppress fibroproliferation and improve injury resolution in an animal model of experimental lung injury (6, 15), suggesting that increasing the number of Tregs in ARDS lungs would be an ideal strategy to treat COVID-19 patients in the advanced stages. However, the pharmacological means to increase the number of Tregs in ARDS lung was not available until we recently demonstrated that the number of the effector (activated) Tregs in the advanced stages of bacterial endotoxin-induced experimental lung injury in mouse lungs can be increased by Akt inhibition with compounds such as triciribine and MK2206, promoting injury resolution and recovery (3). Whereas ACE2 has been implicated in pulmonary arterial hypertension (7) and lung inflammation (11), Akt inhibition with MK2206 and triciribine has been reported to ameliorate the pathological effects of ACE2 in hepatic steatosis (4). However, a link between the Akt pathway and ACE2 activation in COVID-19 patients needs to be investigated.
Although the host PI3-kinase/Akt pathway is utilized by the viruses in general for its survival and replication (5, 20), this has not been demonstrated in the case of the SARS-CoV-2 virus replication in the lung epithelial cells. On the contrary, an adverse effect of Akt suppression by promoting the SARS-CoV-2 virus replication in the patient lung epithelial cells also cannot be ruled out. Nevertheless, pharmacological inhibition of the Akt pathway using inhibitors such as triciribine and MK2206, alone or in combination with the currently evolving standard of care, provides potential treatment options for COVID-19 patients with ARDS. Based on the preclinical observations from non-COVID-19 lung disease research, Akt suppression is expected to increase Tregs in the lungs of COVID-19 patients, in turn, suppressing inflammation and fibroproliferation, promoting the resolution of injury, and preventing vascular pruning in the lungs as a result of SARS-CoV-2 infection. This, however, needs further experimental validation in a suitable preclinical COVID-19 model such as the non-human primates before clinical trials are conducted in COVID-19 patients.
GRANTS
This work was supported in part by National Heart, Lung, and Blood Institute Grant R01HL103952 and National Center for Advancing Translational Sciences Grant UL1TR002378.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author.
AUTHOR CONTRIBUTIONS
P.R.S prepared figure; drafted manuscript; edited and revised manuscript; and approved final version of manuscript.
REFERENCES
- 1.Abdalla M, Goc A, Segar L, Somanath PR. Akt1 mediates α-smooth muscle actin expression and myofibroblast differentiation via myocardin and serum response factor. J Biol Chem 288: 33483–33493, 2013. doi: 10.1074/jbc.M113.504290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abdalla M, Sabbineni H, Prakash R, Ergul A, Fagan SC, Somanath PR. The Akt inhibitor, triciribine, ameliorates chronic hypoxia-induced vascular pruning and TGFβ-induced pulmonary fibrosis. Br J Pharmacol 172: 4173–4188, 2015. doi: 10.1111/bph.13203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Artham S, Verma A, Alwhaibi A, Adil MS, Manicassamy S, Munn DH, Somanath PR. Delayed Akt suppression in the lipopolysaccharide-induced acute lung injury promotes resolution that is associated with enhanced effector regulatory T cells. Am J Physiol Lung Cell Mol Physiol 318: L750–L761, 2020. doi: 10.1152/ajplung.00251.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cao X, Yang F, Shi T, Yuan M, Xin Z, Xie R, Li S, Li H, Yang JK. Angiotensin-converting enzyme 2/angiotensin-(1-7)/Mas axis activates Akt signaling to ameliorate hepatic steatosis. Sci Rep 6: 21592, 2016. doi: 10.1038/srep21592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunn EF, Connor JH. HijAkt: the PI3K/Akt pathway in virus replication and pathogenesis. Prog Mol Biol Transl Sci 106: 223–250, 2012. doi: 10.1016/B978-0-12-396456-4.00002-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garibaldi BT, D’Alessio FR, Mock JR, Files DC, Chau E, Eto Y, Drummond MB, Aggarwal NR, Sidhaye V, King LS. Regulatory T cells reduce acute lung injury fibroproliferation by decreasing fibrocyte recruitment. Am J Respir Cell Mol Biol 48: 35–43, 2013. doi: 10.1165/rcmb.2012-0198OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guignabert C, de Man F, Lombès M. ACE2 as therapy for pulmonary arterial hypertension: the good outweighs the bad. Eur Respir J 51: 1800848, 2018. doi: 10.1183/13993003.00848-2018. [DOI] [PubMed] [Google Scholar]
- 8.Hawkins PT, Stephens LR. PI3K signalling in inflammation. Biochim Biophys Acta 1851: 882–897, 2015. doi: 10.1016/j.bbalip.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181: 271–280.e8, 2020. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497–506, 2020. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jia H. Pulmonary angiotensin-converting enzyme 2 (ACE2) and inflammatory lung disease. Shock 46: 239–248, 2016. doi: 10.1097/SHK.0000000000000633. [DOI] [PubMed] [Google Scholar]
- 12.Jiang X, Rayner S, Luo MH. Does SARS-CoV-2 has a longer incubation period than SARS and MERS? J Med Virol 92: 476–478, 2020. doi: 10.1002/jmv.25708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kerr BA, Ma L, West XZ, Ding L, Malinin NL, Weber ME, Tischenko M, Goc A, Somanath PR, Penn MS, Podrez EA, Byzova TV. Interference with akt signaling protects against myocardial infarction and death by limiting the consequences of oxidative stress. Sci Signal 6: ra67, 2013. doi: 10.1126/scisignal.2003948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li G, He X, Zhang L, Ran Q, Wang J, Xiong A, Wu D, Chen F, Sun J, Chang C. Assessing ACE2 expression patterns in lung tissues in the pathogenesis of COVID-19. J Autoimmun. In press. doi: 10.1016/j.jaut.2020.102463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin S, Wu H, Wang C, Xiao Z, Xu F. Regulatory T cells and acute lung injury: cytokines, uncontrolled inflammation, and therapeutic implications. Front Immunol 9: 1545, 2018. doi: 10.3389/fimmu.2018.01545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma L, Kerr BA, Naga Prasad SV, Byzova TV, Somanath PR. Differential effects of Akt1 signaling on short- versus long-term consequences of myocardial infarction and reperfusion injury. Lab Invest 94: 1083–1091, 2014. doi: 10.1038/labinvest.2014.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep 20: 12, 2018. doi: 10.1007/s11906-018-0812-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma MD, Shinde R, McGaha TL, Huang L, Holmgaard RB, Wolchok JD, Mautino MR, Celis E, Sharpe AH, Francisco LM, Powell JD, Yagita H, Mellor AL, Blazar BR, Munn DH. The PTEN pathway in Tregs is a critical driver of the suppressive tumor microenvironment. Sci Adv 1: e1500845, 2015. doi: 10.1126/sciadv.1500845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh AK, Gupta R, Misra A. Comorbidities in COVID-19: outcomes in hypertensive cohort and controversies with renin angiotensin system blockers. Diabetes Metab Syndr 14: 283–287, 2020. doi: 10.1016/j.dsx.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soares JA, Leite FG, Andrade LG, Torres AA, De Sousa LP, Barcelos LS, Teixeira MM, Ferreira PC, Kroon EG, Souto-Padrón T, Bonjardim CA. Activation of the PI3K/Akt pathway early during vaccinia and cowpox virus infections is required for both host survival and viral replication. J Virol 83: 6883–6899, 2009. doi: 10.1128/JVI.00245-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thompson BT, Chambers RC, Liu KD. Acute respiratory distress syndrome. N Engl J Med 377: 1904–1905, 2017. doi: 10.1056/NEJMra1608077. [DOI] [PubMed] [Google Scholar]
- 22.Umbrello M, Formenti P, Bolgiaghi L, Chiumello D. Current concepts of ARDS: a narrative review. Int J Mol Sci 18: 64, 2016. doi: 10.3390/ijms18010064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell 181: 281–292.e6, 2020. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323: 1239, 2020. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 25.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395: 1054–1062, 2020. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


