Abstract
Background
With respect to patient-centered care, measuring care effects based on patient-relevant outcomes is becoming increasingly important. There is some uncertainty about what outcomes are particularly relevant to patients and who determines their relevance. To determine this, we conducted a scoping review of the international literature with the aim to improve the conceptual clarity regarding (1) the terminology used for supposedly patient-relevant outcomes, (2) the variety of outcomes considered patient-relevant, and (3) justifications for the choice of these specific outcomes.
Methods
We conducted a systematic search in Embase, PubMed (including Medline), Cochrane Central, Scopus, and Google Scholar with a special focus on article titles. Search terms included patient-relevant, patient-important, patient-preferred, and outcome(s), endpoint(s), parameter(s), indicator(s). We limited the search period from January 2000 to July 2019. Full-text articles reporting outcomes that were described as patient-relevant met the inclusion criteria. Two researchers independently analyzed all eligible articles applying quantitative and structuring content analysis.
Results
We identified 155 articles, 44 of which met the inclusion criteria. A content analysis revealed 35 different terms used with regard to patient-relevant outcomes. However, authors predominantly referred to patient-important outcomes (23 articles, 52.3%) and patient-relevant outcomes (17 articles, 38.6%). A structuring content analysis of all extracted outcomes revealed a total of 281 codes, pooled in 32 inductive categories. Among these, the following categories dominated: symptoms, adverse events/complications, survival/mortality, pain. In just 16 of the articles (36.4%), authors provided justifications for the choice of the outcome being based either on patient and/or expert opinions. In another 13 articles (29.5%), no justification was provided.
Conclusion
This scoping review on patient-relevant outcomes was driven by the questions (1) what outcomes are particularly relevant to patients, and (2) who determines their relevance. We found a wide range of supposedly patient-relevant outcomes, with only one third of articles involving patients in the justification of the outcome selection. In view of this conceptual uncertainty it appears difficult to determine or even to compare a particular patient benefit of interventions. A set of generic outcomes relevant to patients would be helpful to contribute to a consistent understanding of patient relevance.
Keywords: Patient-relevant outcome, Patient relevance, Patient preference, Patient-centered care, Patient involvement
Background
Patient-centered care aims to place individuals, their values, preferences, life and health goals at the heart of the care process and to actively involve patients in care decisions [1]. In the sense of shared decision-making, involving patients in decisions implies that patients are adequately informed about existing care options and their potential effects, understand these options, and are given the opportunity to explore what is most relevant to them in order to make a choice based on their personal preferences [2]. In our understanding, this means that for shared decision-making, effect measurements based on parameters that matter to patients are urgently needed. This assumes that studies examine the effects of care that is based on outcomes which are relevant to patients, but so far systematic reviews conclude that such patient-relevant outcomes are underrepresented in recent clinical trials [3–5]. Indeed, this raises the question as to what outcomes are relevant to patients and who determines their relevance.
In Germany, the Institute for Quality and Efficiency in Health Care (IQEHC) officially examines the benefits and harms of medical interventions for patients. To this end, the IQEHC considers parameters to be relevant to patients when they represent how a patient feels, functions or survives; notably mortality, morbidity, and quality of life [6]. However, this understanding of patient relevance is based on a definition of the Biomarkers Definition Working Group on clinical endpoints, which does not contain any information about patient relevance [7]. Similarly to the IQEHC’s understanding of patient-relevant outcomes, the working group on quality of care and patient safety research of the German Network for Health Services Research (DNVF) mentions survival and quality of life as factors that are relevant to patients, but also includes social aspects, such as social reintegration, in its interpretation [8]. Generally, these outcomes are based on the understanding that patient-relevant outcomes reflect the effects of changes in the individual patient’s health status [8].
However, neither the definition provided by the IQEHC nor that provided by the working group of the DNVF offered us a comprehensive explanation as to why the outcomes mentioned are considered to be relevant to patients. Shifting the view from the German to the international context, we aimed to examine which understanding of patient relevance and which outcomes are common to international research and thereby hoped to improve the conceptual clarity of patient relevance. To this end, we conducted a scoping review of the international literature with regard to the following research questions: (1) What terminology is used for supposedly patient-relevant outcomes? (2) What outcomes are considered to be relevant to patients? (3) What explanations are provided to justify the relevance of these specific outcomes for patients?
Methods
We report our scoping review in accordance with the PRISMA extension for scoping reviews (PRISMA-ScR) [9].
Data sources and search strategy
We conducted a systematic literature search in Embase, PubMed (including Medline), Cochrane Central, Scopus, and Google Scholar. Our search strategy considered German and English references published between January 1st, 2000 and July 31st, 2019. Restricting the search period to the past 20 years was considered reasonable to concentrate on more recent research. In order to identify references that clearly focus on the topic of interest, we additionally restricted the search to the article titles. Titles had to include at least one of the following terms: (patient-relevant OR patient-important OR patient-preferred) AND (outcome(s) OR endpoint(s) OR parameter(s) OR indicator(s)). The full search strategies for each database are outlined in Additional file 1.
Study selection
After deleting all duplicates, two of the researchers (Christine Kersting (CK), Malte Kneer (MK)) reviewed all records retrieved from the database search: In the first step, we independently screened the records to limit the search results to English- and German-language articles with full-text availability published in journals. This was reasonable as we aimed to examine whether there is, in fact, a common and consistent understanding of patient relevance in international research. Accordingly, we excluded doctoral theses if not officially published, conference abstracts, commentaries on previously published articles, opinions, debates, or editorials, records on other topics, and those without full-text availability. In the second step, we independently reviewed the full texts of the remaining articles to check whether they met the inclusion criteria for our review. We defined articles as eligible when they reported outcomes that were described by the authors as relevant to patients. In case of disagreements we discussed these until a consensus was achieved.
Data extraction and analysis
In line with the three research questions of this scoping review, we analyzed all eligible articles regarding (1) the terminology used, (2) the outcomes described as patient-relevant, and (3) the justifications for why these outcomes were considered to be of relevance to patients. For the analysis we used both quantitative content analysis and qualitative structuring content analysis [10].
Terminology
All terms that were used to describe patient-relevant outcomes were assessed and extracted in original spelling to collect synonyms; however, paraphrases such as “outcomes that matter to patients” were not considered synonyms. Finally, we applied frequency calculations to quantify the number of different terms used per article and the overall number of different terms identified.
Outcomes
In a second step all outcomes described as relevant to patients were extracted from the articles and structured for the underlying issues (thematically) using inductive categories. The code set was extended continuously as new categories emerged during the full-text analyses. We additionally examined whether specific outcome categories were used more often than others by calculating frequencies and percentages.
Justification
We analyzed whether the articles provided a justification as to why the outcomes described were considered to be relevant to patients. These justifications were categorized inductively. Based on this, we distributed the outcome categories that were identified in the previous step to the justifications provided.
In a subgroup analysis we focused on articles that actively involved patients or experts in the definition of patient-relevant outcomes. We examined whether the outcomes defined in these articles were valid for specific patient groups only and whether these outcomes were different from those described as relevant to patients in articles that did not involve patients or experts. Additionally, we stratified for studies involving patients, studies involving experts, and those involving both, and compared the outcome categories between these groups.
Results
Literature search
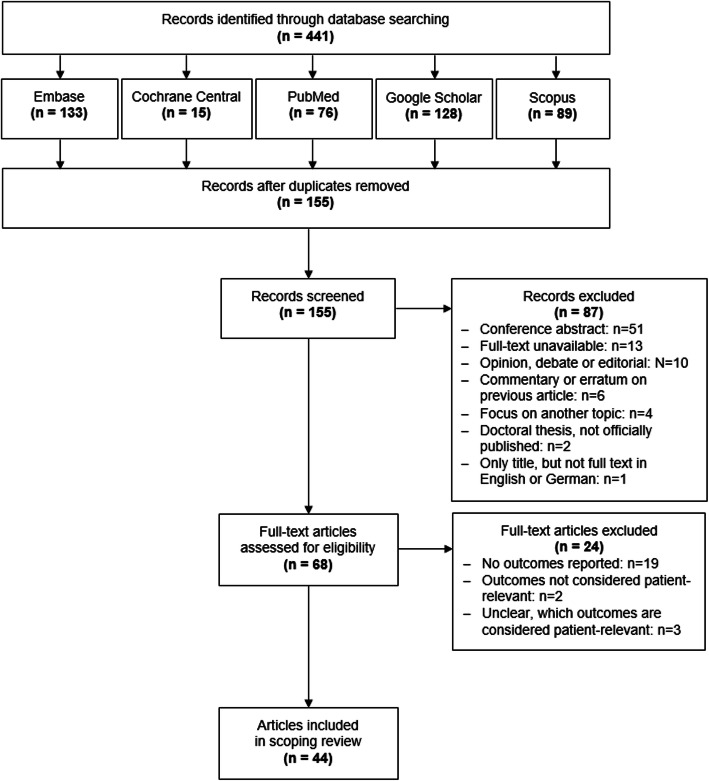
Excluding duplicates, the literature search yielded 155 records (Fig. 1). During the first screening, we excluded 87 records because the full-text papers were unavailable, not written in English or German, focused on another topic, or were conference abstracts, commentaries on previously published articles, opinions, debates, or editorials. Full-text screening of the remaining 68 articles resulted in 44 articles fulfilling the inclusion criteria for this review. Details on all studies are provided in Tables 1, 2, 3 and 4.
Fig. 1.
Flow chart depicting study selection
Table 1.
Characteristics of the 16 articles involving patients and/or experts to justify patient relevance of outcomes
| Authors | Objective/ motivation of article | Type of article/ study | Terms used synonymously | Indicator disease/intervention | Outcomes considered patient-relevant [instrument, if applicable] |
|---|---|---|---|---|---|
| Blome et al. 2009 [11] | Development and validation of a specific version of the German patient benefit index (PBI-S) to be used in the treatment of pruritus (PBI-P) | Mixed methods study involving patients and experts |
5 terms: - patient-relevant benefit - patient-relevant treatment benefit - patient preference - patient-reported benefit - patient-relevant outcome |
Pruritus |
In decreasing order of importance, i.a.: - no longer experience itching - find a clear diagnosis and therapy - have confidence in therapy - be free of pain - no longer have a burning sensation on the skin - be able to sleep better - be less dependent on doctor and clinic visits |
| Blome et al. 2014 [12] | Development and validation of a specific version of the German patient benefit index (PBI-S) to be used in the treatment of lymphedema and lipedema (PBI-L) | Mixed methods study involving patients and experts |
3 terms: - patient-relevant outcome - patient-relevant benefit - patient-relevant treatment benefit |
Lymphedema, lipedema |
In decreasing order of importance, i.a.: - experience less swelling and tension - be free of pain - avoid complications - receive optimal hosiery (e.g., color, fit, prescription quantity) - be less restricted in your ability to move around - have no fear that the disease will become worse - find a clear diagnosis and therapy |
| Cho et al. 2019 [13] | Identification of patients‘and caregivers‘priorities for outcomes in trials on autosomal dominant polycystic kidney disease | Mixed methods study involving patients only |
4 terms: - patient-important outcome - patient-prioritised outcome - patient-centered outcome - patient-reported outcome |
Autosomal dominant polycystic kidney disease |
In decreasing order of importance, i.a.: - kidney function - end-stage kidney disease - survival - cyst size/growth - cyst pain/bleeding - blood pressure - ability to work - cerebral aneurysm/stroke - mobility/physical function - fatigue |
| Daeter et al. 2018 [14] |
1. Share the standard set of outcomes for coronary artery disease developed by Meetbaar Beter 2. Illustrate how the standard set is presented and published Note: Meetbaar Beter aims to improve the quality of cardiovascular care in hospitals in the Netherlands by creating transparency on patient-relevant outcomes (Benchmarking) |
Delphi approach among experts only |
1 term: - patient-relevant outcome |
Coronary artery disease (overall) |
- long-term survival (≤5 years) - 1-year mortality - quality of life [SF-36] - myocardial infarction (≤30 days) |
| Coronary artery bypass grafting |
- 120-day mortality - surgical reexploration (≤30 days) - cerebrovascular accident (≤72 h) - Deep sternal wound infection (≤30 days) - free of myocardial infarction - free of coronary artery reintervention |
||||
| Percutaneous coronary intervention |
- 30-day mortality - urgent coronary artery bypass grafting (≤24 h) - occurrence of target vessel revascularization (≤1 year) |
||||
| Conservative treatment |
- chest pain (≤1 year) - free of major adverse cardiac event |
||||
| Dinglas et al. 2018 [15] | Synthesis of the literature with regard to patient-important outcome for Intensive Care Unit survivors focusing on a research program on acute respiratory failure | Synthesis, Delphi approach among patients only |
1 term: - patient-important outcome |
Acute respiratory failure |
- survival - physical function - muscle and/or nerve function - pulmonary function - cognition - mental health [HADS, IES-R] - pain [EQ-5D pain question] - health-related quality of life [EQ-5D, SF-36] |
| Eiring et al. 2016 [16] |
1. Investigate the relative importance of patient-important outcomes in bipolar disorder 2. Construct a holistic taxonomy of patient-important outcomes |
Mixed methods study involving patients only |
2 terms: - patient-important outcome - patient-relevant outcome |
Bipolar disorder |
In decreasing order of importance, i.a.: - avoid serve depression - avoid serve mania - increase quality of life - better functioning (school/work) - better social functioning |
| Kinter et al. 2009 [17] |
1. Identification of endpoints directly from patients with schizophrenia 2. Evaluation whether patients can express which endpoints matter to them 3. Ranking of the relevant endpoints |
Mixed methods study involving patients only |
5 terms: - patient-relevant endpoint - patient-relevant benefit - patient endpoint - patient preference - patient-centered endpoint |
Schizophrenia |
In decreasing order of importance, i.a.: - clear thinking - minimization of symptoms - social activities - daily activities - supportive physician |
| Konkle et al. 2019 [18] | Review of strengths and limitations of outcome measures used in hemophilia trials from a provider and patient perspective | Review involving patients and experts |
3 terms: - patient-important outcome - patient-relevant outcome - patient-important clinical outcome |
Hemophilia |
- frequency of bleeds - factor activity level - duration of expression - chronic pain - healthcare resource use - mental health |
| Lindsley et al. 2018 [19] | Identification and prioritization of clinical questions and patient-relevant outcomes for research associated with the treatment of age-related macular degeneration | Delphi approach among patients and experts |
1 term: - patient-important outcome |
Age-related macular degeneration |
Highly important to patients: - choroidal neovascularization - development of advanced age-related macular degeneration - retinal hemorrhage - gain of vision - slowing vision loss - serious ocular events |
| Murad et al. 2011 [20] | Assessment of preferences of patients with diabetes on how clinical trials should be conducted with regard to study design (pragmatic versus explanatory) and endpoints (surrogate versus patient-relevant) | Cross-sectional study involving patients only |
2 terms: - patient-important outcome - patient preference |
Diabetes mellitus |
In decreasing order of importance, i.a.: - end-stage renal disease - stroke - myocardial infarction - blindness - HbA1c control - death |
| Nabbout et al. 2018 [21] | Identification of a core set of patient- and caregiver-relevant concepts to be included in future clinical trials on dravet syndrome | Qualitative study, Delphi approach among caregivers and experts |
2 terms: - patient- and caregiver-relevant outcome - patient- and caregiver-relevant endpoint |
Dravet syndrome |
- seizures - expressive communication of the child - receptive communication of the child - daily activities of the caregiver - social functioning of the caregiver |
| Sanderson et al. 2010 [22] | Identification of treatment outcomes important to patients with rheumatoid arthritis receiving anti-tumor necrosis factor therapy | Qualitative study involving patients only |
6 terms: - patient outcome - patient priority treatment outcome - patient priority outcome - patients’ important treatment outcome - patients’ important outcome - patient-important outcome |
Rheumatoid arthritis |
- rheumatoid arthritis under control (symptoms less, rheumatoid arthritis stable, medication effects) - doing things (doing things, able to plan) - emotional health (positive feelings, holistic identity, positive mental changes, better life) - coping with illness (coping with rheumatoid arthritis, coping with health system) - global outcomes (feeling well, return to a normal life, feeling (more) normal) |
| Sung et al. 2014 [23] | Development of a comprehensive conceptual framework representing the relevant dimensions and outcomes important to women with pelvic organ prolapse | Mixed methods study involving patients only |
1 term: - patient-important outcome |
Pelvic organ prolapse |
In decreasing order of importance, i.a.: - alleviation of physical bulge symptoms and associated discomfort - improvement in physical function - improvement in sexual function - improvement in body image perception - improvement in social function |
| Van der Elst et al. 2016 [24] | Better comprehension of the perspective of patients with early rheumatoid arthritis on preferred health and treatment outcomes | Qualitative study involving patients only |
2 terms: - patient-preferred outcome - patient-preferred health and treatment outcome |
Early rheumatoid arthritis |
- aspects of disease control, e.g., prevention or control of joint damage, less medication - physical aspects, e.g., relief of pain and other physical symptoms, improved joint function and mobility - aspects of participation, e.g., performing activities of daily living, engaging in work and/or leisure - mental aspects, e.g., emotional well-being, life enjoyment |
| Wilson et al. 2019 [25] | Synthesis of evidence in all outcome domains identified as important by patients undergoing unicompartmental or total knee replacement and outcome domains commonly used in other studies | Systematic review & meta-analysis involving patients and referring to other studies |
1 term: - patient relevant outcome |
Unicompartmental and total knee replacement in osteoarthritis |
- hospital admission impact: length of operation, length of hospital stay - risk of early complications (myocardial infarction, stroke, venous thromboembolism, deep infection) or early mortality - success of operation: range of movement achieved or kneeling ability, reduction in pain, improvement in function - reoperation or revision rate - rate of recovery: rate of return to work, rate of return to sporting activities |
| Van Veghel et al. 2016 [26] | Presentation and discussion of the patient-relevant outcomes of Meetbaar Beter for coronary artery disease and aortic valve disease, focusing on the surgical procedures coronary artery bypass grafting, percutaneous coronary intervention, aortic valve replacement and transcatheter aortic valve implantation | Database analysis involving experts only |
3 terms: - patient-relevant outcome - patient-relevant health outcome - patient-oriented outcome |
Coronary artery disease (overall) | - readmission due to myocardial infarction (≤30 days) |
| Coronary artery bypass grafting |
- 120-day mortality - quality of life [SF-36] |
||||
| Percutaneous coronary intervention |
- 1-year mortality - Occurrence of target vessel revascularization (≤1 year) |
||||
| Aortic valve replacement |
- 120-day mortality - long-term survival |
||||
| Transcatheter aortic valve implantation |
- 120-day mortality - implantation of a new permanent pacemaker (≤30 days) |
Table 2.
Characteristics of the 12 articles referring to other studies or special classifications to justify patient relevance of outcomes
| Authors | Objective/ motivation of article | Type of article/ study | Terms used synonymously | Indicator disease/intervention | Outcomes considered patient-relevant [instrument, if applicable] |
|---|---|---|---|---|---|
| Adie et al. 2017 [4] | Determination of the proportion of patient-important primary outcomes in surgical randomized controlled trials | Systematic review & meta-analysis |
2 terms: - patient-important outcome - patient-centered outcome |
Surgical interventions |
- mortality/survival - pain - function - quality of life - any morbid event or symptom - patient satisfaction - any intervention to address the previous outcomes |
| Ameur et al. 2017 [27] | Determination whether recently published an ongoing systematic reviews with meta-analyses of therapeutic interventions assess patient-important outcomes | Methodological review |
1 term: - patient-important outcome |
Generic; therapeutic interventions |
- mortality - clinical events - pain - quality of life - therapeutic decision - function |
| Fei et al. 2018 [28] | Examination of the impact of adding ezetimibe to statins on patient-important outcomes in patients at high cardiovascular risk | Narrative systematic review |
1 term: - patient-important outcome |
High cardiovascular risk |
- all-cause mortality - cardiovascular mortality - non-fatal stroke - non-fatal myocardial infarction - adverse events |
| Gaudry et al. 2017 [5] | Investigation whether randomized controlled trials in critically ill patients assess patient-important outcomes | Systematic review |
1 term: - patient-important outcome |
Critical illness |
- mortality - quality of life after Intensive Care Unit discharge - functional, cognitive, and neurological outcomes after Intensive Care Unit discharge |
| Kvitkina et al. 2014 [29] | Description of the feasibility of the early benefit assessment of novel agents on the basis of patient-relevant outcomes by characterizing the outcomes available in the companies dossiers and comparing them to outcomes defined as patient-relevant by the German Institute for Quality and Efficiency in Health Care | Systematic Review |
1 term: - patient-relevant outcome |
Drugs (novel agents) |
- mortality - morbidity - health-related quality of life - adverse events |
| Roos et al. 2000 [30] | Evaluation of patient-relevant outcomes preoperatively and three months after partial meniscectomy | Prospective follow-up study |
1 term: - patient-relevant outcome |
Partial meniscectomy |
- general health status [SF-36] - knee-specific health status: pain, symptoms, activities of daily life, sports and recreation function, knee-related quality of life, functional disability [KOOS, Lysholm Knee Score] |
| Schumacher et al. 2016 [31] | Assessment of current approaches to measure the impact of tuberculosis nucleic acid amplification tests on patient-important outcomes in adults with possibly tuberculosis and/or drug-resistant tuberculosis | Methodological review |
2 terms: - patient-important outcome - patient outcome |
Tuberculosis nucleic acid amplification tests |
- culture conversion - tuberculosis treatment outcomes - infection control/ contact tracing - morbidity - mortality |
| Singh et al. 2017 [32] | Simulation of the long-term effect of novel agents versus chemotherapy-based regimens on progression-free survival, overall survival and health-related quality of life in patients with chronic lymphocytic leukemia | Review & data simulation |
2 terms: - patient-relevant outcome - patient-relevant benefit |
Chronic lymphocytic leukemia |
- progression-free survival - overall survival - quality-adjusted life years - post-progression survival |
| Wieseler et al. 2013 [33] | Determination of the information gain between clinical study reports and publicly available sources for patient-relevant outcomes included in health technology assessments for drugs | Systematic review |
2 terms: - patient-relevant clinical trial outcome - patient-relevant outcome |
Drugs |
- mortality - clinical events - symptoms - health-related quality of life - (serious) adverse events |
| Yordanov et al. 2018 [34] |
1. Evaluation whether the outcomes reported in the summary of finding table of Cochrane reviews could be considered patient-important 2. Evaluation of the quality of evidence for these outcomes |
Methodological review |
1 term - patient-important outcome / PIO |
Generic |
- mortality - other clinical events (e.g., myocardial infarction, stroke) - adverse events - function (e.g., anxiety, depression, disability) - pain - quality of life - therapeutic decisions |
| El Dib et al. 2017 [35] | Review of randomized controlled trials on diagnostic tests with regard to their topic areas, population, setting, study groups, patient-important outcomes, risk of bias, and results | Systematic review |
1 term: - patient-important outcome |
Diagnostic tests |
- mortality - morbidity - symptoms - quality of life - functional status |
| Fayed et al. 2014 [36] |
1. Review to which extent activity and participation outcomes are included in pediatric clinical trials 2. Determination what characteristics are associated with using theses outcomes |
Systematic review |
3 terms: - patient-important outcome - patient-important activity and participation outcome - child and family-important outcome |
Generic; children with chronic conditions |
- body function - activity - participation - environmental factors - personal factors - health condition - general health |
Table 3.
Characteristics of the 3 articles equating patient-relevant outcomes with self-reported outcomes
| Authors | Objective/ motivation of article | Type of article/ study | Terms used synonymously | Indicator disease/ intervention |
Outcomes considered patient-relevant [instrument, if applicable] |
|---|---|---|---|---|---|
| Nilsdotter et al. 2009 [37] |
1. Description of outcomes up to five years after total knee replacement for osteoarthritis from the patients’ perspective 2. Evaluation to what extent patients performed physical activities after total knee replacement 3. Identification of preoperative characteristics predicting postoperative outcomes |
Prospective follow-up study |
2 terms: - patient-relevant outcome - self-reported outcome |
Total knee replacement in osteoarthritis |
- general health status [SF-36] - knee-specific health status: pain, stiffness, physical function [WOMAC] - general comorbidity |
| Nilsdotter, Isaksson 2010 [38] | Prospective evaluation of patient-relevant outcomes seven years after total hip replacement for osteoarthritis focusing on pain and physical function | Prospective cohort study with matched controls without hip complaints |
2 terms: - patient-relevant outcome - patient-reported outcome |
Hybrid total hip replacement and demented total hip replacement for osteoarthritis |
- general health status [SF-36] - knee-specific health status: pain, stiffness, physical function [WOMAC] - postoperative complications - general comorbidity - musculoskeletal comorbidity: need of walking assistance, walking distance, pain, need for analgesics, joint replacement in contralateral hip or in knee, fractures - patient satisfaction |
| Nilsdotter, Lohmander 2003 [39] | Investigation of pre- and postoperative patient-relevant outcomes between hybrid total hip replacement and cemented total hip replacement in patients with osteoarthritis | Prospective cohort study |
2 terms: - patient-relevant outcome - patient-relevant measure |
Total hip replacement for osteoarthritis |
- general health status [SF-36] - knee-specific health status: pain, stiffness, physical function [WOMAC] - postoperative complications - general comorbidity - musculoskeletal comorbidity: need of walking assistance, walking distance, pain, need for analgesics, joint replacement in contralateral hip or in knee, fractures |
Table 4.
Characteristics of the 13 studies not providing any justification for the patient relevance of outcomes
| Authors | Objective/ motivation of article | Type of article/ study | Terms used synonymously | Indicator disease/ intervention |
Outcomes considered patient-relevant [instrument, if applicable] |
|---|---|---|---|---|---|
| Agarwal et al. 2017 [40] | Examination to what extent Cochrane and non-Cochrane reviews report absolute effects for patient-important outcomes in the abstract | Systematic review |
1 term: - patient-important outcome |
Generic |
- mortality - morbidity - symptoms - quality of life - functional status |
| Cao et al. 2014 [41] | Comparison of the efficacy of two commonly used Chinese patent medicines for patients with angina pectoris | Study protocol for a randomized controlled trial |
1 term: - patient-important outcome |
Angina pectoris |
- short of breath - fatigue - palpitations - sweating |
| Cleveringa et al. 2010 [42] |
Determination of the effects of the Diabetes Care Protocol on patient-important outcomes Note: When applying the Diabetes Care Protocol, routine diabetes care is delegated to a nurse, who uses a computerized decision support system to structure diabetes care and set targets |
Cluster-randomized trial |
1 term: - patient-important outcome |
Type 2 diabetes |
- diabetes-specific health status: psychological distress, barriers to activity, disinhibited eating [DHP-18] - general health status [SF-36, EQ-5D] - treatment satisfaction [DTSQ-status] - self-efficacy [DES-SF] |
| Englund et al. 2001 [43] | Evaluation of long-term patient-relevant outcomes after removal of knee meniscus | Retrospective cohort study |
2 terms: - patient-relevant outcome - self-administered outcome measure |
Meniscectomy |
- general health status [SF-36] - knee-specific health status: pain, symptoms, activities of daily life, sports and recreation function, knee-related quality of life [KOOS] |
| Gandhi et al. 2008 [3] | Determination to what extent registered randomized controlled trials among patients with diabetes plan to assess patient-important outcomes | Systematic review |
1 term: - patient-important outcome |
Diabetes |
- mortality - quality of life - major morbid events - minor morbid events - pain - functional status |
| Griffith et al. 2019 [44] | Determination how different disease frameworks impact the prevalence of multimorbidity and its association with patient-important outcomes | Baseline analysis of a population-based cohort study |
2 terms: - patient-important functional outcome - patient-important outcome |
Generic; community-living adults aged 45 to 85 years |
- functional disability [OARS questionnaire] - social participation restriction - self-rated physical health - self-rated mental health |
| Nilsdotter et al. 2003 [45] | Evaluation of long-term patient-relevant outcomes after unilateral total hip replacement for osteoarthritis | Case-control-study |
1 term: - patient relevant outcome |
Unilateral total hip replacement for osteoarthritis |
- general health status [SF-36] - knee-specific health status: pain, stiffness, physical function [WOMAC] - postoperative complications - general comorbidity - musculoskeletal comorbidity: need of walking assistance, walking distance, pain, need for analgesics, joint replacement in contralateral hip or in knee, fractures - patient satisfaction |
| Paradowski et al. 2004 [46] | Assessment of variation in knee pain, function, and quality of life over two years after removal of knee meniscus in patients with and and without radiographic knee osteoarthritis | Prospective follow-up study |
1 term: - patient-relevant outcome |
Meniscectomy | - knee-specific health status: pain, symptoms, activities of daily life, sports and recreation function, knee-related quality of life [KOOS] |
| Porat et al. 2004 [47] |
Identification of the consequences of an anterior cruciate ligament tear 14 years after injury in a cohort of male soccer players regarding radiographic knee osteoarthritis and patient-relevant outcomes |
Prospective cohort study |
1 term: - patient relevant outcome |
Anterior cruciate ligament tear |
- general health status [SF-36] - knee-specific health status: pain, symptoms, activities of daily life, sports and recreation function, knee-related quality of life, functional disability [KOOS, Lysholm Knee Score] |
| Ramar et al. 2017 [48] | Synthesis of the literature with regard to models of care targeting patient-important outcomes for maintenance dialysis patients focusing on hospitalization and mortality | Systematic review & meta-analysis |
2 terms: - patient-important outcome - patient outcome |
Maintenance dialysis care |
- mortality - hospitalization |
| Schnabel et al. 2014 [49] | Comparison of the analgesic efficacy and safety of ultrasound and nerve stimulator guided peripheral nerve catheters for postoperative pain therapy | Retrospective database analysis |
4 terms: - patient-relevant target parameter - patient-related outcome - patient-relevant parameter [German: Patienten-relevanter Parameter] - patient-relevant efficacy parameter [German: Patienten-relevanter Effektivitätsparameter] |
Peripheral nerve catheters for pain therapy |
- postoperative pain - postoperative need for additional opioids - cumulative local anesthetic consumption - puncture-associated complications - postoperative catheter-related complications |
| Stallmach et al. 2015 [50] | Examination of possible improvements in the clinical situation of patients with inflammatory bowel disease in Germany, focusing on patient-relevant endpoints | Secondary data analysis |
1 term: - patient-relevant endpoint |
Inflammatory bowel diseases |
- number of stationary treatments per year (cases) - average residence time - number of operations - inability to work - premature mortality |
| W-Dahl et al. 2005 [51] | Evaluation of the patient-relevant outcomes pain, function, and quality of life during two years in patients operated on for knee osteoarthritis with tibial osteotomy | Prospective follow-up study |
1 term: - patient-relevant outcome |
Tibial osteotomy for uni-compartmental knee osteoarthritis |
- knee-specific health status: pain, symptoms, activities of daily life, sports and recreation function, knee-related quality of life [KOOS] - complications, e.g., delayed healing, deep venous thrombosis |
Regarding the study design, we found a mixture of methodological approaches consisting mainly of reviews (16 of 44, 36.4%) [3–5, 18, 25, 27–29, 31–36, 40, 48] and qualitative or mixed-methods studies including Delphi approaches (12 of 44, 27.3%) [11–17, 19, 21–24]. Whereas the reviews considered studies across different countries, other studies related to a specific country were conducted mainly in Sweden (n = 9) [30, 37–39, 43, 45–47, 51] and Germany (n = 4) [11, 12, 49, 50].
Terminology
Based on the 44 articles included in this review, we identified 35 different terms for patient-relevant outcomes (Table 5). Of these 35 terms, the two most frequently used terms were patient-important outcome (identified in 23 articles, 52.3%) and patient-relevant outcome (identified in 17 articles, 38.6%).
Table 5.
Terms used for supposedly patient-relevant outcomes (n = 44 articles)
| Term, identified in the (international) literature | Number of articles using this term (%) |
|---|---|
| Patient-important outcome | 23 (52.3) |
| Patient-relevant outcome | 17 (38.6) |
| Patient-relevant benefit | 4 (9.1) |
| Patient preference | 3 (6.8) |
| Patient outcome | 3 (6.8) |
| Patient-relevant endpoint | 2 (4.5) |
| Patient-centred outcome | 2 (4.5) |
| Patient-reported outcome | 2 (4.5) |
| Patient-relevant treatment benefit | 2 (4.5) |
| Patient endpoint | 1 (2.3) |
| Patient-prioritised outcome | 1 (2.3) |
| Patient-preferred outcome | 1 (2.3) |
| Patient-preferred health and treatment outcome | 1 (2.3) |
| Patient-reported benefit | 1 (2.3) |
| Patient-relevant health outcome | 1 (2.3) |
| Patient-oriented outcome | 1 (2.3) |
| Patient-relevant clinical trial outcome | 1 (2.3) |
| Self-reported outcome | 1 (2.3) |
| Patient-relevant measure | 1 (2.3) |
| Self-administered outcome measure | 1 (2.3) |
| Patient-relevant target parameter | 1 (2.3) |
| Patient-relevant parameter | 1 (2.3) |
| Patient-relevant efficacy parameter | 1 (2.3) |
| Patient-important activity and participation outcome | 1 (2.3) |
| Patient-important functional outcome | 1 (2.3) |
| Patient-important clinical outcome | 1 (2.3) |
| Child and family-important outcome | 1 (2.3) |
| Patient- and caregiver-relevant outcome | 1 (2.3) |
| Patient- and caregiver-relevant endpoint | 1 (2.3) |
| Patient-related outcome | 1 (2.3) |
| Patient-centered endpoint | 1 (2.3) |
| Patients’ important outcome | 1 (2.3) |
| Patients’ important treatment outcome | 1 (2.3) |
| Patient priority outcome | 1 (2.3) |
| Patient priority treatment outcome | 1 (2.3) |
In 21 articles (47.7%) one term was used consistently for supposedly patient-relevant outcomes; in 14 articles (31.8%) two terms were used, and in the remaining nine articles (20.5%) up to six different terms were used to describe the outcomes. We were not able to identify different patterns in terminology across countries. The terms identified per article are demonstrated in Tables 1, 2, 3 and 4.
Outcomes
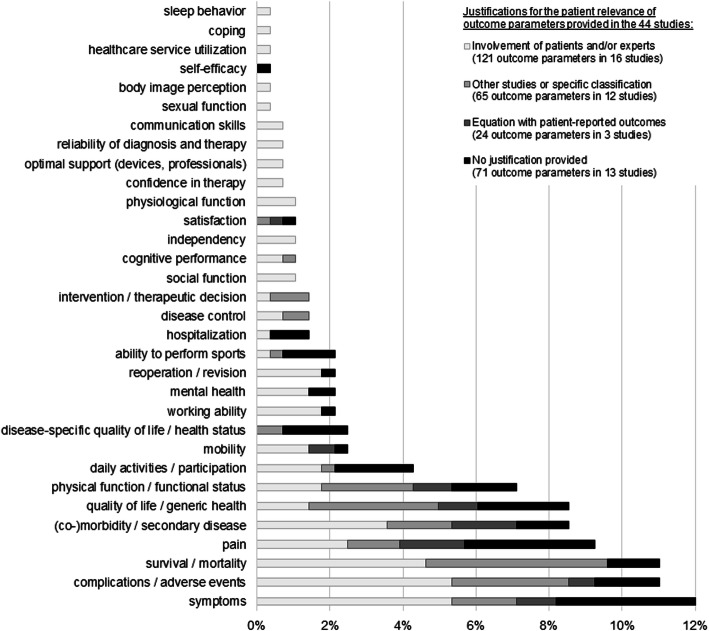
A structuring content analysis of the outcomes extracted from the 44 articles resulted in 281 codes, from which 32 inductive categories were composed. Irrespective of the different shadings per bar, Fig. 2 illustrates these 32 categories in ascending order of frequency (. The most strongly represented categories were: symptoms (n = 34 codes, 12.1%), adverse events/complications (n = 31 codes, 11.0%), survival/mortality (n = 31 codes, 11.0%), pain (n = 26 codes, 9.3%), generic quality of life/health status (n = 24 codes, 8.5%), (co)morbidity/secondary diseases (n = 24 codes, 8.5%), and physical function/functional status (n = 20 codes, 7.1%). The outcomes extracted per article are listed in Tables 1, 2, 3 and 4.
Fig. 2.
Distribution of the 281 codes representing patient-relevant outcomes in 32 inductive categories (bars) with the distribution for each category grouped by the four justifications provided for the patient relevance of outcomes (shading); the percentages on the x-axis refer to 281
Justification
In about one third (n = 13, 29.5%) of the 44 articles analyzed, no reason was provided why the outcomes reported were considered to be relevant to patients (Table 4). However, in other studies we found different explanations justifying the selection of patient-relevant outcomes that refer mainly to three core issues:
Involvement of patients and/or experts was apparent in 16 out of 44 articles (36.4%) (Table 1). To explain their choice of outcomes authors referred either to patients only (n = 9) [13, 15–17, 20, 22–25] or to experts only (n = 2) [14, 26] or to both patients’ and experts’ opinion (n = 5) [11, 12, 18, 19, 21]. One study on early childhood disease included caregivers instead of patients [21], another one on critical disease included caregivers in addition to patients [13]. Sample sizes differed largely from smaller qualitative studies including 10 to 30 patients recruited in the health care setting [21, 22, 24] to a cross-sectional study in a random sample of about 2000 individuals invited by mail [20].
Referral to other studies [4, 5, 27–34] or special classification [35, 36] was used as another source of supposedly patient-relevant outcomes (Table 2). These articles (n = 12, 27.3%) referred their choice of outcomes mainly to reviews [4, 5, 27, 28, 34] or to a specific classification such as the International Classification of Functioning, Disability and Health [36].
A few articles considered patient-reported outcomes equivalent to patient-reported outcomes (n = 3, 6.8%; Table 3). In one of these articles authors argued that patient-relevant outcomes rely exclusively on the information provided by patients themselves [39].
The different shading of the bars in Fig. 2 illustrates the allocation of the outcomes extracted from the studies considering justifications of patient relevance provided by the authors. It shows that more popular outcome categories were justified on the basis of different explanations, whereas more seldom categories and those based on social aspects were commonly traced back to patients and/or experts.
Subgroup analysis of articles involving patients and/or experts
All articles that had actively involved patients and/or experts focused on a specific disease (Table 1), but outcomes considered patient-relevant showed a widespread distribution with regard to the 32 inductive categories identified, referring to as many as 29 different categories. However, these studies did not include outcomes related to satisfaction, self-efficacy, or disease-specific quality of life/health status (Fig. 2). Interestingly, we found that 12 of the 32 inductive categories were only used in articles with patient and/or expert involvement such as physiological functioning, ability to fulfil social functions, independency, reliability of diagnosis and therapy, and confidence in therapy. However, outcomes most commonly described as patient-relevant, such as symptoms, adverse events/complications, survival/mortality, and (co)morbidity/secondary disease were identical to those most commonly described as patient-relevant in the other 28 articles not involving patients and/or experts (Fig. 2).
Stratifying articles involving patients and/or experts (n = 16) by the manner of involvement showed that survival/mortality was mentioned especially in studies involving experts only. On the other hand, outcomes identified only in studies involving patients and/or experts (i.e. physiological functioning, reliability of diagnosis and therapy, or confidence in therapy) were traced back to those studies involving either patients only or both patients and experts.
Discussion
In this scoping review, we analyzed the international literature of the last 20 years with regard to patient relevance. We found a large variety of terms used as well as numerous supposedly patient-relevant outcomes. No more than one third of the articles referred to the patients’, the caregivers’ or the experts’ opinions to explain the relevance of the outcomes reported. All in all, we were not able to identify a consistent concept or understanding of patient-relevant outcomes. Table 6 summarizes the main findings and implications for future research.
Table 6.
Summary of findings and implications for future research
| Research question | Findings | Implications for future research |
|---|---|---|
| What terminology is used for supposedly patient-relevant outcomes? |
- large variety of terms found in the international literature - inconsistency of terms across and within papers - possible confusion between patient-relevant and patient-reported |
- consistent concept of patient relevance is needed - standard set of patient-relevant outcomes is needed - patients must be involved when defining what is relevant to them - consistency regarding patient relevance will improve the comparability of study results and enable patients to make informed choices |
| What outcomes are considered to be relevant to patients? |
- wide range of outcomes found - commonly disease-specific outcomes - social dimensions underrepresented |
|
| What explanations are provided to justify the relevance of these specific outcomes for patients? |
- one third of studies without any explanation - another third refers to the opinion of patients, experts, or caregivers as patient representatives - outcomes exclusively defined by experts do not necessarily represent patients’ preferences |
According to our analysis, the reasons for the identified ambiguity appear to be heterogeneous. Some articles did not differentiate between patient-reported and patient-relevant outcomes [37–39]. Other articles emphasized a potential overlap of the terms, but noted that not every outcome which can be reported by patients necessarily has to be relevant for them [16, 18, 23, 24, 41]. Two articles on chronically ill children expanded the terminology from patients to the family to underline the social context and impact [21, 36]. In both studies, the target group was involved in the definition of relevant outcomes. Indeed, such patient- or target group-driven approaches are not common practice yet: two thirds of the articles we analyzed referred to previous articles [4, 5, 27–34] or did not even provide a justification as to why the reported outcomes were considered to be relevant to patients [3, 40–51]. With respect to both of these justifications, Murad et al. (2011) pointed out that neither outcomes considered patient-relevant in other studies nor those described as relevant to patients from a researchers’ perspective necessarily represent what really matters to patients [20]. In addition, our subgroup analysis on studies involving patients and/or experts suggested that outcomes defined solely by experts in sense of health care professionals might not necessarily represent the patients’ perspectives as well. Transferring this to practice implies that patient-driven approaches are required: Patients or representatives need to be asked when defining what is relevant for them. Referring to the patients’ or – in the case of young children or critical care – the caregivers’ opinions, such patient-driven approaches were identified in 14 articles included in our scoping review, but were limited to specific diseases such as cardiovascular disorders [11–13, 15–25]. For these particular patients, adverse events like myocardial infarction or stroke might be important outcomes but may not necessarily be applicable to other patient groups as specific diseases are commonly associated with very specific needs and preferences that cannot be generalized.
The number of outcomes identified in the context of patient relevance with 32 inductive categories certainly exceeded our expectations. However, outcomes representing social dimensions including the ability to perform daily activities or to fulfil social functions were apparently underrepresented, especially in studies not involving patients and experts. The variety of outcome measures as well as the lack of a consistent concept with regard to outcomes representing patient relevance limit the comparability of study results and make it difficult to determine the particular patient benefit of different interventions. This problem is also known from patient-centered care: Based on a systematic review and concept analysis of 417 articles, Scholl et al. (2014) found that models on patient-centeredness lack conceptual clarity, resulting in heterogeneous terminology and inconsistent outcome measures [52]. Even in the context of patient-relevant outcomes, this criticism was already voiced years ago, for example by Cleveringa et al. (2010) [42].
Meanwhile, promising initiatives like the European Qualitative research project on Patient-preferred outcomes in Early Rheumatoid Arthritis [53] or the International Consortium for Health Outcomes Measurement (ICHOM) [54] address this problem by defining core sets of outcomes that matter to patients. With a stronger focus on the operationalization of patient-relevant outcomes, a working group at the German Center for Health Services Research in Dermatology developed and validated a questionnaire assessing patient-relevant treatment benefits. This so-called Patient Benefit Index is available for different diseases, e.g. for the treatment of pruritus, lymphedema, and lipedema [11, 12]. While such initiatives usually focus on individual diseases, the ICHOM has also started to develop outcome sets across diseases (e.g., overall adult health, older persons, overall pediatric health) [55]. Providing validated instruments for each outcome set, the ICHOM may have the potential to standardize outcome measurement in (clinical) trials, even though the initiative originally aimed to standardize the assessment of routine care data across countries to improve the quality of healthcare for common diseases worldwide.
Based on this scoping review we aimed to improve the conceptual clarity on patient relevance. Since the results do not allow us to derive a clear concept, in a next step we plan to close this gap by conducting a study among patients, health care professionals, and researchers. Unlike the approaches described above, we not only aim to identify a core set of generic rather than disease-specific patient-relevant outcomes, but also to contribute to a clear definition and understanding thereof. Based on the findings of this review, patients and health care professionals will be involved to define outcomes that are relevant to patients across diseases and important components of an adequate definition. Researchers will additionally ensure that the concept is feasible for research purposes. Our overarching long-term objective is to increase the comparability of study results with regard to patient relevance.
Limitations
A key strength of this scoping review is the systematic approach: The terms and outcomes were systematically and independently extracted by two researchers. Also, the literature search was not limited to fixed term sequences, but considered combinations of terms, e.g. “patient-relevant” and “outcome” instead of “patient-relevant outcome”. Due to this approach, articles with titles including a statement or question like “Are outcomes reported patient-relevant?” were also covered. Nevertheless, the search strategy focused only on the titles of articles. Thus, it cannot be excluded that we missed relevant articles. This is further aggravated by the fact that the terminology used in the literature lacks consistency. For example, we did not consider search terms like “patient-centered outcomes” as we aimed to focus on outcomes that are relevant to patients, but these terms might have been used as synonyms in some articles as well. Finally, the restriction to full-text availability might represent another limitation. However, the abstracts alone did not provide sufficient information regarding supposedly patient-relevant outcomes and outcome justification.
Conclusions
Returning to the initial question what outcomes are particularly relevant to patients and who determines their relevance, we conclude that recent studies use a variety of outcomes without asking patients what really matters to them. We were unable to identify either a sound definition or a consistent outcome set of patient-relevant outcomes, not even in the few studies that actively involved patients. In our opinion, consensus on a consistent terminology and set of generic patient-relevant outcomes is needed to adequately operationalize patient-centered care, increase the comparability of study results, and thereby enable patients to make choices regarding therapy in the context of shared decision-making.
Supplementary information
Additional file 1. Full electronic search strategy for Embase, PubMed, Cochrane Central, Scopus, and Google Scholar.
Acknowledgements
We thank Dorothea Kesztyüs, MPH, Institute of General Medicine, Ulm University, for conducting the literature search in Embase.
Abbreviations
- DES-SF
Diabetes Empowerment Scale-Short Form
- DHP-18
Diabetes Health Profile (18 questions)
- DNVF
German Network for Health Services Research
- DTSQ-status
Diabetes Treatment Satisfaction Questionnaire
- EQ-5D
European Quality of Life questionnaire - 5 Dimensions
- HADS
Hospital Anxiety and Depression Scale
- IES-R
Impact of Event Scale-Revised
- IQEHC
Institute for Quality and Efficiency in Health Care
- KOOS
Knee Injury and Osteoarthritis Outcome Score
- LOST-IT
LOST to follow-up Information in Trials
- OARS questionnaire
Older American Resources and Services questionnaire
- SF-36
Short Form-36 Health Survey
- WOMAC
Western Ontario and McMaster Universities Osteoarthritis Index
Authors’ contributions
AB and CK developed the idea and concept for the study. CK conducted the literature search and prepared the search results for analysis. The literature was analyzed by CK and MK under the supervision of AB. CK drafted the first version of the manuscript, which was critically reviewed by AB. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Christine Kersting, Email: Christine.Kersting@uni-wh.de.
Malte Kneer, Email: Malte.Kneer@uni-wh.de.
Anne Barzel, Email: Anne.Barzel@uni-ulm.de.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12913-020-05442-9.
References
- 1.American Geriatrics Society Expert Panel on Person-Centered Care Person-centered care: a definition and essential elements. J Am Geriatr Soc. 2016;64:15–18. doi: 10.1111/jgs.13866. [DOI] [PubMed] [Google Scholar]
- 2.Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–1367. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gandhi GY, Murad MH, Fujiyoshi A, Mullan RJ, Flynn DN, Elamin MB, et al. Patient-important outcomes in registered diabetes trials. JAMA. 2008;299:2543–2549. doi: 10.1001/jama.299.21.2543. [DOI] [PubMed] [Google Scholar]
- 4.Adie S, Harris IA, Naylor JM, Mittal R. Are outcomes reported in surgical randomized trials patient-important? A systematic review and meta-analysis. Can J Surg. 2017;60:86–93. doi: 10.1503/cjs.010616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaudry S, Messika J, Ricard J-D, Guillo S, Pasquet B, Dubief E, et al. Patient-important outcomes in randomized controlled trials in critically ill patients: a systematic review. Ann Intensive Care. 2017;7:28. doi: 10.1186/s13613-017-0243-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen . Allgemeine Methoden. 2017. [Google Scholar]
- 7.Biomarkers Definitions Working Group Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69:89–95. doi: 10.1067/mcp.2001.113989. [DOI] [PubMed] [Google Scholar]
- 8.Geraedts M, Drösler SE, Döbler K, Eberlein-Gonska M, Heller G, Kuske S, et al. Memorandum III, part 3: quality of care and patient safety methods. Gesundheitswesen. 2017;79:e95–e124. doi: 10.1055/s-0043-112431. [DOI] [PubMed] [Google Scholar]
- 9.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 10.Mayring P. Qualitative content analysis: theoretical foundation, basic procedures and software solution. 2014. [Google Scholar]
- 11.Blome C, Augustin M, Siepmann D, Phan NQ, Rustenbach SJ, Stander S. Measuring patient-relevant benefits in pruritus treatment: development and validation of a specific outcomes tool. Br J Dermatol. 2009;161:1143–1148. doi: 10.1111/j.1365-2133.2009.09328.x. [DOI] [PubMed] [Google Scholar]
- 12.Blome C, Augustin M, Heyer K, Knofel J, Cornelsen H, Purwins S, Herberger K. Evaluation of patient-relevant outcomes of lymphedema and lipedema treatment: development and validation of a new benefit tool. Eur J Vasc Endovasc Surg. 2014;47:100–107. doi: 10.1016/j.ejvs.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Cho Y, Sautenet B, Gutman T, Rangan G, Craig JC, Ong AC, et al. Identifying patient-important outcomes in polycystic kidney disease: an international nominal group technique study. Nephrology (Carlton). 2019. 10.1111/nep.13566. [DOI] [PubMed]
- 14.Daeter EJ, Timmermans MJC, Hirsch A, Lipsic E, Houterman S, van Veghel D, van Boven WJ. Defining and measuring a standard set of patient-relevant outcomes in coronary artery disease. Am J Cardiol. 2018;121:1477–1488. doi: 10.1016/j.amjcard.2018.02.037. [DOI] [PubMed] [Google Scholar]
- 15.Dinglas VD, Faraone LN, Needham DM. Understanding patient-important outcomes after critical illness: a synthesis of recent qualitative, empirical, and consensus-related studies. Curr Opin Crit Care. 2018;24:401–409. doi: 10.1097/MCC.0000000000000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eiring O, Nylenna M, Nytroen K. Patient-important outcomes in the long-term treatment of bipolar disorder: a mixed-methods approach investigating relative preferences and a proposed taxonomy. Patient. 2016;9:91–102. doi: 10.1007/s40271-015-0128-x. [DOI] [PubMed] [Google Scholar]
- 17.Kinter ET, Schmeding A, Rudolph I, dos Reis S, Bridges JFP. Identifying patient-relevant endpoints among individuals with schizophrenia: An application of patient-centered health technology assessment. Int J Technol Assess Health Care. 2009;25:35–41. doi: 10.1017/S0266462309090059. [DOI] [PubMed] [Google Scholar]
- 18.Konkle BA, Skinner M, Iorio A. Hemophilia trials in the twenty-first century: defining patient important outcomes. Res Pract Thromb Haemost. 2019;3:184–192. doi: 10.1002/rth2.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lindsley KB, Hutfless S, Hawkins BS, Blim JF, Roberts D, Olsen TW, et al. Evaluation of clinical questions and patient-important outcomes associated with the treatment of age-related macular degeneration. JAMA Ophthalmol. 2018;136:1217–1225. doi: 10.1001/jamaophthalmol.2018.3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murad MH, Shah ND, van Houten HK, Ziegenfuss JY, Deming JR, Beebe TJ, et al. Individuals with diabetes preferred that future trials use patient-important outcomes and provide pragmatic inferences. J Clin Epidemiol. 2011;64:743–748. doi: 10.1016/j.jclinepi.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 21.Nabbout R, Auvin S, Chiron C, Irwin J, Mistry A, Bonner N, et al. Development and content validation of a preliminary core set of patient- and caregiver-relevant outcomes for inclusion in a potential composite endpoint for Dravet syndrome. Epilepsy Behav. 2018;78:232–242. doi: 10.1016/j.yebeh.2017.08.029. [DOI] [PubMed] [Google Scholar]
- 22.Sanderson T, Morris M, Calnan M, Richards P, Hewlett S. What outcomes from pharmacologic treatments are important to people with rheumatoid arthritis? Creating the basis of a patient core set. Arthritis Care Res (Hoboken) 2010;62:640–646. doi: 10.1002/acr.20034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sung VW, Rogers RG, Barber MD, Clark MA. Conceptual framework for patient-important treatment outcomes for pelvic organ prolapse. Neurourol Urodyn. 2014;33:414–419. doi: 10.1002/nau.22397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van der Elst K, Meyfroidt S, De Cock D, De Groef A, Binnard E, Moons P, et al. Unraveling patient-preferred health and treatment outcomes in early rheumatoid arthritis: a longitudinal qualitative study. Arthritis Care Res (Hoboken) 2016;68:1278–1287. doi: 10.1002/acr.22824. [DOI] [PubMed] [Google Scholar]
- 25.Wilson HA, Middleton R, Abram SGF, Smith S, Alvand A, Jackson WF, et al. Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ. 2019;364:l352. doi: 10.1136/bmj.l352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Veghel D, Marteijn M, de Mol B. First results of a national initiative to enable quality improvement of cardiovascular care by transparently reporting on patient-relevant outcomes. Eur J Cardiothorac Surg. 2016;49:1660–1669. doi: 10.1093/ejcts/ezw034. [DOI] [PubMed] [Google Scholar]
- 27.Ameur H, Ravaud P, Fayard F, Riveros C, Dechartres A. Systematic reviews of therapeutic interventions frequently consider patient-important outcomes. J Clin Epidemiol. 2017;84:70–77. doi: 10.1016/j.jclinepi.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 28.Fei Y, Guyatt GH, Alexander PE, El Dib R, Siemieniuk RAC, Vandvik PO, et al. Addition of Ezetimibe to statins for patients at high cardiovascular risk: systematic review of patient-important outcomes. J Eval Clin Pract. 2018;1:222–231. doi: 10.1111/jep.12663. [DOI] [PubMed] [Google Scholar]
- 29.Kvitkina T, ten Haaf A, Reken S, McGauran N, Wieseler B. Patient-relevant outcomes and surrogates in the early benefit assessment of drugs: first experiences. Zeitschrift für Evidenz Fortbildung und Qualität im Gesundheitswesen. 2014;108:528–538. doi: 10.1016/j.zefq.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 30.Roos EM, Roos HP, Ryd L, Lohmander LS. Substantial disability 3 months after arthroscopic partial meniscectomy: a prospective study of patient-relevant outcomes. Arthroscopy. 2000;16:619–626. doi: 10.1053/jars.2000.4818. [DOI] [PubMed] [Google Scholar]
- 31.Schumacher SG, Sohn H, Qin ZZ, Gore G, Davis JL, Denkinger CM, Pai M. Impact of molecular diagnostics for tuberculosis on patient-important outcomes: a systematic review of study methodologies. PLoS One. 2016;11:e0151073. doi: 10.1371/journal.pone.0151073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singh M, Mealing S, Baculea S, Cote S, Whelan J. Impact of novel agents on patient-relevant outcomes in patients with previously untreated chronic lymphocytic leukemia who are not eligible for fludarabine-based therapy. J Med Econ. 2017;20:1066–1073. doi: 10.1080/13696998.2017.1357563. [DOI] [PubMed] [Google Scholar]
- 33.Wieseler B, Wolfram N, McGauran N, Kerekes MF, Vervolgyi V, Kohlepp P, et al. Completeness of reporting of patient-relevant clinical trial outcomes: comparison of unpublished clinical study reports with publicly availablel data. PLoS Med. 2013;10:e1001526. 10.1371/journal.pmed.1001526. [DOI] [PMC free article] [PubMed]
- 34.Yordanov Y, Dechartres A, Ravaud P. Patient-important outcomes in systematic reviews: poor quality of evidence. PLoS One. 2018;13:e0195460. doi: 10.1371/journal.pone.0195460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El Dib R, Tikkinen KAO, Akl EA, Gomaa HA, Mustafa RA, Agarwal A, et al. Systematic survey of randomized trials evaluating the impact of alternative diagnostic strategies on patient-important outcomes. J Clin Epidemiol. 2017;84:61–69. doi: 10.1016/j.jclinepi.2016.12.009. [DOI] [PubMed] [Google Scholar]
- 36.Fayed N, de Camargo OK, Elahi I, Dubey A, Fernandes RM, Houtrow A, Cohen E. Patient-important activity and participation outcomes in clinical trials involving children with chronic conditions. Qual Life Res. 2014;23:751–757. doi: 10.1007/s11136-013-0483-9. [DOI] [PubMed] [Google Scholar]
- 37.Nilsdotter A-K, Toksvig-Larsen S, Roos EM. A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthr Cartil. 2009;17:601–606. doi: 10.1016/j.joca.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 38.Nilsdotter A-K, Isaksson F. Patient relevant outcome 7 years after total hip replacement for OA - a prospective study. BMC Musculoskelet Disord. 2010;11:47. doi: 10.1186/1471-2474-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nilsdotter AK, Lohmander LS. Patient relevant outcomes after total hip replacement. A comparison between different surgical techniques. Health Qual Life Outcomes. 2003;1:21. doi: 10.1186/1477-7525-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Agarwal A, Johnston BC, Vernooij RWM, Carrasco-Labra A, Brignardello-Petersen R, Neumann I, et al. Authors seldom report the most patient-important outcomes and absolute effect measures in systematic review abstracts. J Clin Epidemiol. 2017:3–12. 10.1016/j.jclinepi.2016.08.004. [DOI] [PubMed]
- 41.Cao H, Zhai J, Mu W, Lei X, Cao H, Liu C, Shang H. Use of comparative effectiveness research for similar Chinese patent medicine for angina pectoris of coronary heart disease: a new approach based on patient-important outcomes. Trials. 2014;15:84. doi: 10.1186/1745-6215-15-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cleveringa FGW, Minkman MH, Gorter KJ, van den Donk M, Rutten GE. Diabetes care protocol: effects on patient-important outcomes. A cluster randomized, non-inferiority trial in primary care. Diabet Med. 2010;27:442–450. doi: 10.1111/j.1464-5491.2010.02968.x. [DOI] [PubMed] [Google Scholar]
- 43.Englund M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford) 2001;40:631–639. doi: 10.1093/rheumatology/40.6.631. [DOI] [PubMed] [Google Scholar]
- 44.Griffith LE, Gilsing A, Mangin D, Patterson C, van den Heuvel E, Sohel N, et al. Multimorbidity frameworks impact prevalence and relationships with patient-important outcomes. J Am Geriatr Soc. 2019. 10.1111/jgs.15921. [DOI] [PubMed]
- 45.Nilsdotter A-K, Petersson IF, Roos EM, Lohmander LS. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Ann Rheum Dis. 2003;62:923–930. doi: 10.1136/ard.62.10.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paradowski PT, Englund M, Roos EM, Lohmander LS. Similar group mean scores, but large individual variations, in patient-relevant outcomes over 2 years in meniscectomized subjects with and without radiographic knee osteoarthritis. Health Qual Life Outcomes. 2004;2:38. doi: 10.1186/1477-7525-2-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ramar P, Ahmed AT, Wang Z, Chawla SS, Suarez MLG, Hickson LJ, et al. Effects of different models of Dialysis care on patient-important outcomes: a systematic review and meta-analysis. Popul Health Manag. 2017;6:495–505. doi: 10.1089/pop.2016.0157. [DOI] [PubMed] [Google Scholar]
- 49.Schnabel A, Middendorf B, Boschin MG, Gottschalk A, van Aken H, Zahn PK, Pogatzki-Zahn EM. Differences of analgesic efficacy and complication rates between ultrasound and nervestimulator guided peripheral nerve catheters: database analysis on patient-relevant target parameters. Der Anästhesist. 2014;63:825–831. doi: 10.1007/s00101-014-2379-7. [DOI] [PubMed] [Google Scholar]
- 50.Stallmach A, Dennler U, Marschall U, Schmidt C. Patient-relevant endpoints in inflammatory bowel diseases - have changes occurred in Germany over the past twelve years? J Crohns Colitis. 2015;9:390–397. doi: 10.1093/ecco-jcc/jjv041. [DOI] [PubMed] [Google Scholar]
- 51.W-Dahl A, Toksvig-Larsen S, Roos EM. A 2-year prospective study of patient-relevant outcomes in patients operated on for knee osteoarthritis with tibial osteotomy. BMC Musculoskelet Disord. 2005;6:18. doi: 10.1186/1471-2474-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scholl I, Zill JM, Harter M, Dirmaier J. An integrative model of patient-centeredness - a systematic review and concept analysis. PLoS One. 2014;9:e107828. doi: 10.1371/journal.pone.0107828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van der Elst K, Bremander A, de Groef A, Larsson I, Mathijssen EGE, Vriezekolk JE, et al. European qualitative research project on patient-preferred outcomes in early rheumatoid arthritis (EQPERA): rationale, design and methods of a multinational, multicentre, multilingual, longitudinal qualitative study. BMJ Open. 2019;9:e023606. doi: 10.1136/bmjopen-2018-023606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.International Consortium for Health Outcome Measurement. ICHOM. https://www.ichom.org/. Accessed 4 June 2020.
- 55.International Consortium for Health Outcome Measurement. ICHOM Standard Sets. https://www.ichom.org/standard-sets/. Accessed 4 June 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Full electronic search strategy for Embase, PubMed, Cochrane Central, Scopus, and Google Scholar.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.