Abstract
Purpose:
The World Health Organization (WHO) recommends that Southeast Asian countries have ≥1 ophthalmologist per 100,000 persons, equally distributed in urban and rural areas. However, regional patterns of eye care have been poorly characterized. This study investigates the distribution of ophthalmologists in Thailand and provides regional estimates of access to ophthalmologists.
Methods:
We geocoded the work address of ophthalmologists listed in the 2008 directory of the Royal College of Ophthalmologists of Thailand. We determined the number of ophthalmologists per 100,000 persons at the national, provincial, and district levels using data from the 2000 Thai Population Census, and assessed for demographic factors associated with meeting the WHO recommendation of ≥1 ophthalmologist per 100,000 persons.
Results:
In 2008, Thailand had 1.52 ophthalmologists per 100,000 persons; however, only 20 of 76 (26%) provinces and 134 of 926 (14%) districts met the WHO recommendation of ≥1 ophthalmologist per 100,000 persons. District factors associated with not meeting the WHO recommendation included a high proportion of children, a high proportion of elderly, and a high proportion of rural residents.
Conclusion:
Thailand meets the WHO’s goal for access to ophthalmologic care, but the distribution of ophthalmologists is uneven, with less access to ophthalmologic care in rural areas.
Introduction
As part of their Vision 2020 initiative to eliminate avoidable blindness worldwide, the World Health Organization (WHO) recommended that countries in Asia have at least 1 ophthalmologist per 100,000 persons by 2010 and 1 ophthalmologist per 50,000 persons by 2020, with equal distribution for urban and rural populations.1,2 Thailand is an emerging economy with a strong health care system. There are, however, acknowledged shortages of physicians in rural areas of the country, where 65% of the country’s approximately 60 million people reside.3,4 Rural physician shortages are not uncommon; worldwide, the concentration of doctors is higher in cities, where physicians often find higher income, better standard of living, more social recognition, and greater job satisfaction.3 The shortage of rural physicians in Thailand has led to reduced rural access to medical care, an issue which has been directly addressed by the Thai medical system since the 1970s.5 The thrust of this effort to reduce inequitable geographic distribution of physicians has been directed towards primary care; however, in light of the WHO’s recommendations, the distribution of eye-care personnel must be addressed as well. Furthermore, the goals set by the WHO are often implemented at the national rather than regional level; thus while a country may meet the WHO goals at the national level there may be regions of the country with a shortage of ophthalmologists. In this study, we characterize the distribution of ophthalmologic providers within Thailand at the province and district levels and assess factors associated with poor access to ophthalmologic care using the 2010 goal of 1 ophthalmologist per 100,000 persons as a benchmark.
Materials and Methods
We identified the work addresses of all practicing ophthalmologists listed in the 2008 directory of the Royal College of Ophthalmologists of Thailand (RCOPT). Registration with the RCOPT is required to practice ophthalmology in Thailand. The directory contains the information for all practicing ophthalmologists, ophthalmology residents, and ophthalmology fellows in Thailand. Ophthalmologists register after passing their board examination. Addresses are updated every 2–4 years, as determined by a committee of the RCOPT. We are unaware of any practicing ophthalmologists in Thailand who would not be listed in this directory. We geocoded each address with Google Maps (Google, Mountain View, CA). We included all practicing ophthalmologists, fellows, and residents, and excluded ophthalmologists who were retired, abroad, or unable to be located. If the work address could not be located, we geocoded the city-center, district, or home address.
We used population and demographic data for provinces and districts from the 2000 Thai Population and Housing Census.6 We counted the special administrative area of Bangkok as a province, resulting in 76 provinces. There were 50 districts (khet) within Bangkok and 876 districts (amphoe) in other provinces. We did not update the 2000 Census to include any demographic areas newly created since the 2000 census (i.e., Bueng Kan province and Wiang Kao King district were not considered to be separate administrative areas for this analysis). We estimated the 2008 population by updating the 2000 census figures according to population growth estimates for this time period from the World Bank (−4.1% for the population aged 0–14 years, 9.7% for the population aged 15–64 years, and 33.9% for the population aged 65 years and older).7 All other demographic variables were obtained as reported in the 2000 census. The proportion of workers considered to have vulnerable employment was defined as the proportion of workers who were own-account workers (self-employed with no employees working for them) or contributing family workers (family members who work for this type of self-employed person).8
We used geographic information systems software (ArcGIS 10 [ESRI, Redlands, CA]) to create maps and to calculate the proportion of the Thai population living within pre-specified distances from an ophthalmologist. Specifically, we generated basemaps of Thailand using the 1975 Indian Universal Transverse Mercator Zone 47N projection and plotted the location of each geocoded ophthalmologist address.9 We created buffer zones of 10km, 25km, 50km, 100km, 150km, and 200km radii surrounding each ophthalmologist and determined the proportion of the population within each buffer zone using simple areal interpolation,10 which assumes uniform distribution of population within each district.
We determined the ratio of ophthalmologists per 100,000 persons (O/P ratio) at the country, province, and district level, assuming a weight of 1.0 for each full-time ophthalmologist and a weight of 0.5 for residents and fellows.11 This weighting system assumed that each resident and fellow provided the equivalent care of half that of a practicing ophthalmologist. We assessed for factors associated with meeting the WHO recommendation of ≥1 ophthalmologist per 100,000 persons using logistic regression. Variables included demographic and socioeconomic factors available through the 2000 Thai Population and Housing Census.6 We created multivariate models using a backwards stepwise selection algorithm, retaining variables with p<0.05. Similar analyses were performed for province-level variables and district-level variables. To summarize the distribution of access to ophthalmologic care in a single number, we calculated a Gini coefficient.12 This metric, which is most often used to summarize income inequality, takes a value between 0 and 1, where 0 indicates perfect equality and 1 perfect inequality. We calculated the Gini coefficient for the weighted number of ophthalmologists per province, using the province-level population as a frequency weight (fastgini command in Stata). In the context of this analysis, the closer the Gini coefficient is to 1, the more unequal the distribution of access to ophthalmologic care. We used Stata 10 for regression analyses (StataCorp LP, College Station, TX). We obtained ethical approval from the University of California, San Francisco Committee on Human Research; all data used are publicly available.
Results
Of the 808 ophthalmologists and 158 ophthalmology residents/fellows in the directory, we successfully geocoded the addresses of 797 ophthalmologists and 158 residents/fellows, including work addresses for 854, city or district coordinates for 82, and home addresses for 19. We excluded the remaining 11 ophthalmologists, of whom 3 were retired, 4 were abroad, and 4 were unable to be located.
Ophthalmologists tended to cluster in Bangkok. In 2008, the population of Thailand was estimated to be 65.7 million people, and the total land area was estimated to be 513,921 km2. Bangkok’s 6.9 million people lived in an area of 1565 km2, meaning that Bangkok made up 10.5% of the population, and 0.3% of the land mass of Thailand. Yet 364 of the 797 geocoded ophthalmologists (45.7%) and 95 of the 158 ophthalmology residents (60.1%) were located in Bangkok, indicating a relative surplus of ophthalmologists there. The Gini coefficient, which was calculated to summarize the inequality in access to ophthalmologic care at the province level, was 0.815. Outside of Bangkok, ophthalmologists appeared to be relatively evenly distributed, with at least 1 ophthalmologist in each of the province capitals (Figure 1). Assuming population was evenly distributed within each district, the proportion of Thai people living within 10km, 25km, 50km, and 100km of an ophthalmologist were 27.2%, 57.1%, 88.2%, and 99.7%, respectively (Figure 2).
Figure 1: Ophthalmologists per person in Thailand.
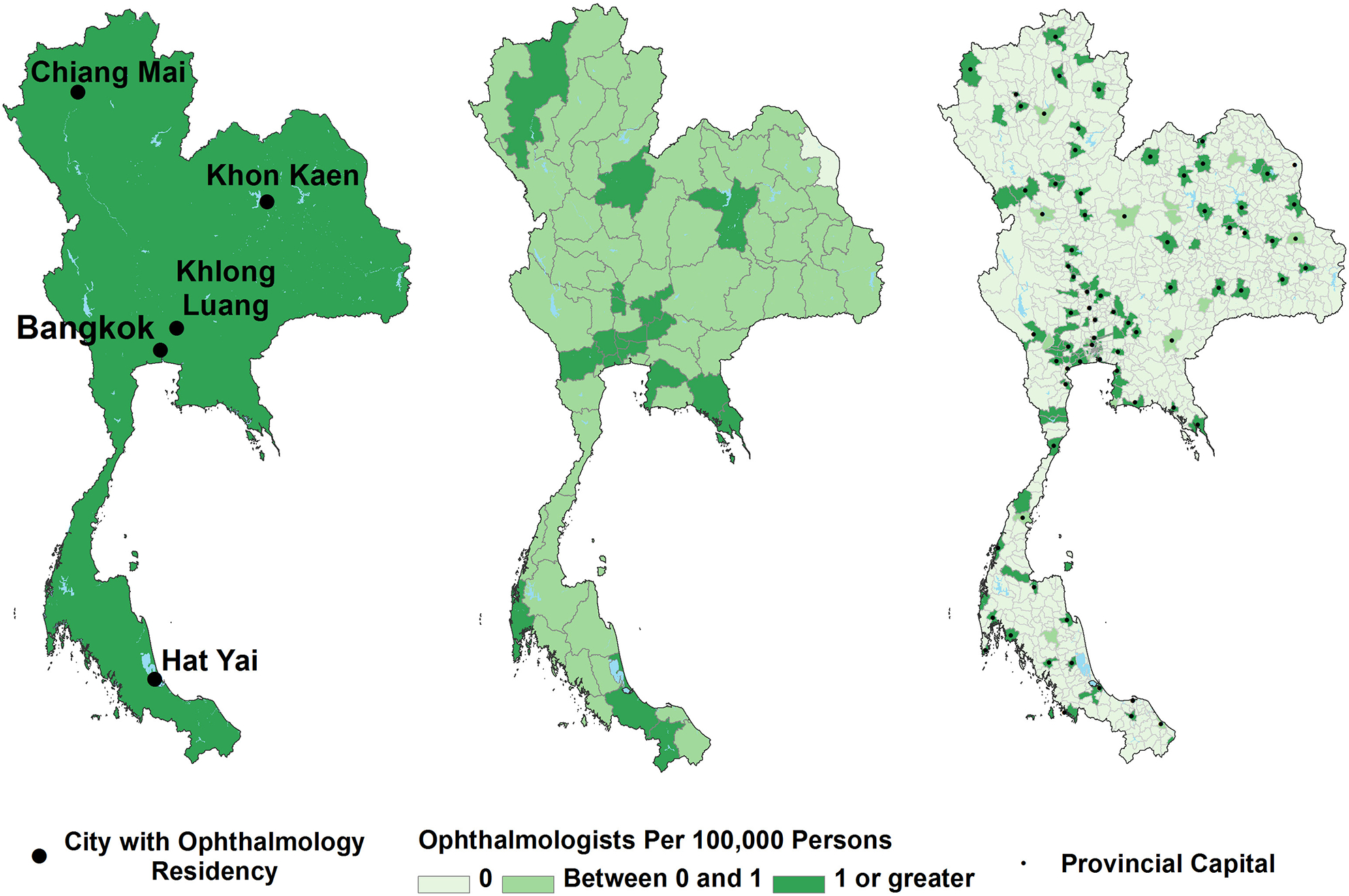
Ratios are represented at the national, provincial, and district levels.
Figure 2. Location of ophthalmologists in Thailand.
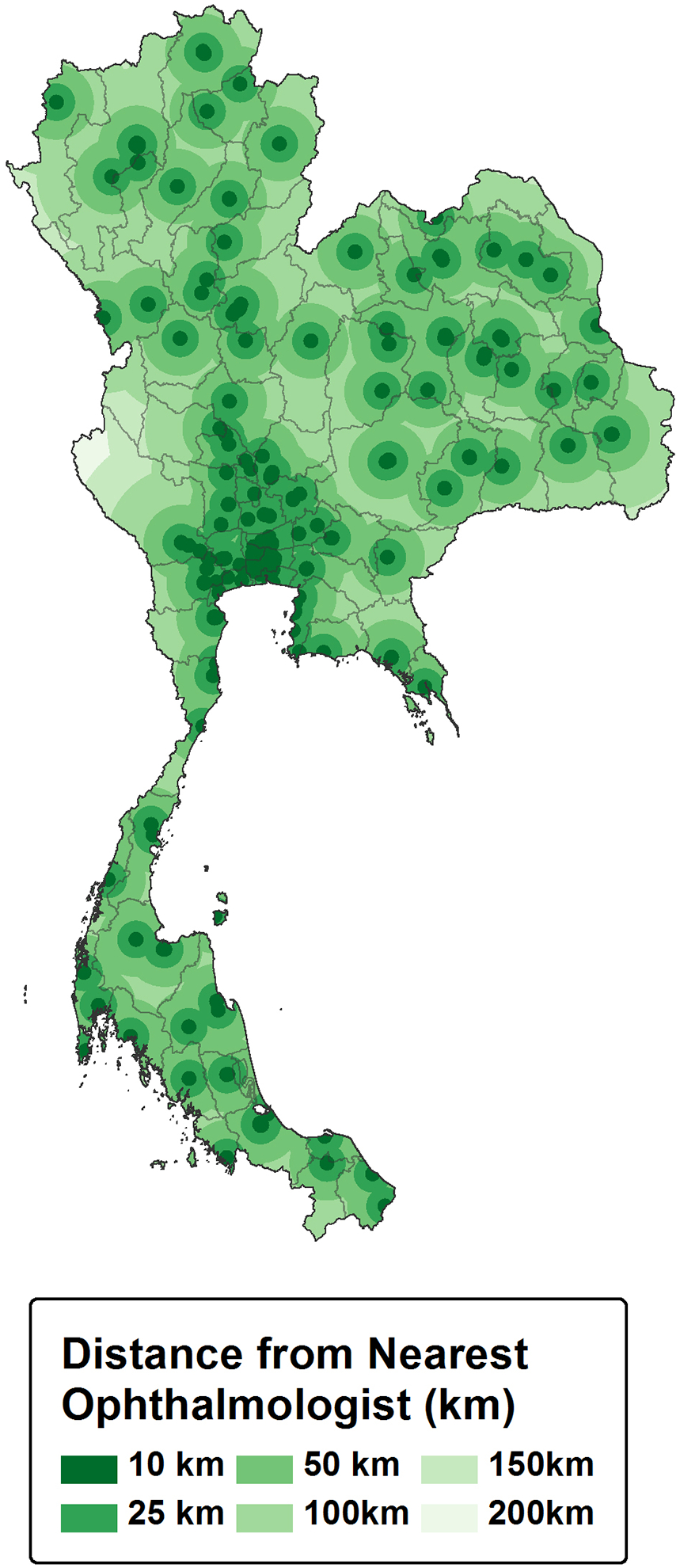
Rings surrounding ophthalmologists represent the linear distance to the nearest ophthalmologist.
In 2008, there were 1.52 ophthalmologists per 100,000 people (O/P ratio) in Thailand. The O/P ratio for provinces ranged from 0.12 to 5.96 (median 0.58, interquartile range [IQR] 0.36 to 1.07; mean 0.87 ± 0.90) and for districts ranged from 0 to 71.6 (median 0, IQR 0 to 0; mean 0.65 ± 3.40). The highest concentration of ophthalmologists was found in the special administrative area of Bangkok (O/P ratio = 5.96), with the next highest concentration in the adjacent province of Pathum Thani (O/P ratio = 2.80). There were 9 ophthalmology residency programs listed in the 2008 directory, with 5 of these located in Bangkok. The concentration of ophthalmologists was significantly higher in the 5 provinces with an ophthalmology residency program compared to the 71 without a program (median O/P ratio 2.7 vs 0.6; P=0.004, Wilcoxon rank sum test).
Of the 76 provinces, 20 met the WHO recommendation for 2010 of having at least 1 ophthalmologist per 100,000 persons (26.3% of provinces, accounting for 31.6% of Thailand’s estimated 65.7 million people), and 56 (73.7%) did not. Of 926 districts, 134 had at least 1 ophthalmologist per 100,000 persons (14.5% of districts, accounting for 30.3% of the national population), 26 had between 0 and 1 ophthalmologist per 100,000 persons (2.8% of districts, accounting for 5.9% of the population), and 766 had no ophthalmologists (82.7% of districts, accounting for 63.8% of the population). Figure 1 shows the provinces and districts of Thailand that met the WHO recommendation of at least 1 ophthalmologist per 100,000 persons.
We also summarized access to ophthalmologists in terms of the WHO’s recommendations for 2020 of 1 ophthalmologist per 50,000 persons. Of the 76 provinces, 10 had at least 1 ophthalmologist per 50,000 persons (13.2% of provinces, accounting for 23.3% of Thailand’s national population), and of the 926 districts, 71 had at least 1 ophthalmologist per 50,000 persons (7.6% of districts, accounting for 16.5% of the national population).
We assessed for predictors of meeting the WHO recommendation for ophthalmologist supply using several socioeconomic and demographic variables that were available from the 2000 Thai census at the province- and district-level (Table 1). In province-level bivariate logistic regression analyses, having an O/P ratio ≥ 1 was associated with several measures of higher socioeconomic status (Table 2). In the multivariate province-level models, the only variable that retained statistical significance was the proportion of workers classified as having vulnerable employment (OR 0.39 [95%CI 0.25–0.62] per additional 10% of workforce classified as vulnerable). Of note, the vulnerable employment rate was highly correlated with the proportion of the population living in rural areas (Pearson’s r=0.74, p<0.001). Similar multivariate analyses using the district-level data (Table 3) found that an O/P ratio ≥ 1 was less common in districts with a high proportion of children (OR 0.76 [95%CI 0.69–0.83] per additional 1% of children aged <15 years), a high proportion of elderly (OR 0.86 [95%CI 0.77–0.96] per additional 1% of persons aged 65 and older) and a high proportion of people living in rural areas (OR 0.82 [95%CI 0.74–0.92] per additional 10% of rural population).
Table 1.
Demographic and socioeconomic characteristics of provinces and districts in Thailand stratified by access to ophthalmologic care
| Median (Interquartile Range) | ||||
|---|---|---|---|---|
| Province | District | |||
| Variable | ≥1 ophthalmologist per 100,000 persons N= 20 | <1 ophthalmologist per 100,000 persons N= 56 | ≥1 ophthalmologist per 100,000 persons N= 134 | <1 ophthalmologist per 100,000 persons N= 792 |
| Population (thousands) | 677.0 (281.3–1006.1) | 648.9 (489.8–1030.4) | 136.4 (88.8–175.9) | 47.5 (30.8–75.1) |
| Population density (persons/km2) | 181.3 (91.2–447.1) | 121.1 (77.3–158.2) | 378.4 (173.9–2897.5) | 119.7 (73.5–171.4) |
| % population in rural areas (%) | 70.0% (59.5–75.3%) | 81.7% (77.6–85.1%) | 61.7% (12.3–74.8%) | 86.9% (78.2–93.8%) |
| % population < 14 years old (%) | 20.0% (18.3–21.5%) | 23.0% (20.6–24.9%) | 19.1% (16.4–21.3%) | 23.6% (20.8–25.6%) |
| % population ≥ 65 years old (%) | 7.9% (6.3–9.1%) | 8.0% (6.6–9.5%) | 7.2% (5.9–9.2%) | 7.7% (6.5–9.5%) |
| Years of education, adults (mean)* | 7.0 (6.7–7.7) | 6.3 (6.0–6.7) | ||
| % with vulnerable employment (%)† | 51.3% (32.2–55.4%) | 69.8% (59.7–81.8%) | ||
| Average household size (persons) | 3.6 (3.5–3.8) | 3.8 (3.6–4.1) | ||
| % households headed by females (%) | 29.7 (25.1–32.5%) | 24.1% (21.9–26.8%) | ||
| % houses made of nonpermanent materials (%) | 7.3% (4.9–8.2%) | 7.3% (5.9–9.3%) | ||
| % households with safe water (%) | 96.5% (93.6–97.5%) | 92.7% (89.4–96.3%) | ||
| % households with gas/electricity (%) | 89.3% (84.6–94.2%) | 62.9% (35.1–84.9%) | ||
Average years of education attainment of population > 15 years of age
Vulnerable work status refers to the proportion of workers who work as business owners without employees,, or without pay for family members
Table 2:
Province-level associations between demographic/socioeconomic factors and access to ophthalmologic care
| Presence of ≥1 ophthalmologist per 100,000 persons | ||||
|---|---|---|---|---|
| Bivariate | Multivariate | |||
| Variable | OR (95%CI) | p-value | OR (95%CI) | p-value |
| Population density (per 100 persons/km2) | 1.35 (1.00–1.83) | 0.048 | ||
| % population in rural areas (per 10%) | 0.37 (0.20–0.68) | 0.001 | ||
| % population < 14 years old (per 1%) | 0.72 (0.58–0.89) | 0.003 | ||
| % population ≥ 65 years old (per 1%) | 0.98 (0.74–1.29) | 0.87 | ||
| Average years of education, adults (per year)* | 6.49 (2.22–18.9) | 0.001 | ||
| % with vulnerable employment (per 10%)† | 0.39 (0.25–0.62) | <0.001 | 0.39 (0.25–0.62) | <0.001 |
| Average household size | 0.09 (0.01–0.65) | 0.02 | ||
| % households headed by females (per 10%) | 7.61 (2.17–26.7) | 0.002 | ||
| % houses made of nonpermanent materials (per 10%) | 0.36 (0.06–2.05) | 0.25 | ||
| % households with safe water (per 10%) | 4.25 (1.14–15.8) | 0.03 | ||
| % households with gas/electricity (per 10%) | 1.86 (1.27–2.74) | 0.002 | ||
Average years of education attainment of population > 15 years of age
Vulnerable work status refers to the proportion of workers who work as business owners without employees, or without pay for family members
Table 3:
District-level associations between demographic/socioeconomic factors and access to ophthalmologic care
| Presence of ≥1 ophthalmologist per 100,000 persons | ||||
|---|---|---|---|---|
| Variable | Bivariate | Multivariate | ||
| OR (95%CI) | p-value | OR (95%CI) | p-value | |
| Population density (per 100 persons/km2) | 1.04 (1.03–1.06) | <0.001 | ||
| % population in rural areas (per 10%) | 0.64 (0.60–0.69) | <0.001 | 0.82 (0.74–0.92) | <0.001 |
| % population < 14 years old (per 1%) | 0.69 (0.65–0.74) | <0.001 | 0.76 (0.69–0.83) | <0.001 |
| % population ≥ 65 years old (per 1%) | 0.91 (0.83–0.99) | 0.02 | 0.86 (0.77–0.96) | 0.006 |
Discussion
In 2008, the spatial distribution of ophthalmologists in Thailand was fairly uniform, with at least 1 ophthalmologist in each province capital, and with most Thais living a reasonable distance from an ophthalmologist. At the country level, Thailand had 1.52 ophthalmologists per 100,000 people, which surpassed the 2010 WHO target of 1 ophthalmologist per 100,000 people. However, access to ophthalmologic care was not evenly distributed throughout the country. The concentration of ophthalmologists was highest in Bangkok, with 6 ophthalmologists per 100,000 persons. This concentration is similar to the national concentration of ophthalmologists in the United States, where there are approximately 6.2 ophthalmologists per 100,000 persons.13 However, the majority of provinces and districts did not meet the WHO recommendation of ≥1 ophthalmologist per 100,000 people. Demographic factors indicative of lower socioeconomic status and rural residence were associated with not meeting this WHO target. Looking toward the future, Thailand does not appear to currently meet the WHO’s 2020 goal of 1 ophthalmologist per 50,000 people at the national level, nor for the vast majority of the provinces. This indicates an opportunity for public health planners to increase access to ophthalmologists over the next decade.
The majority of Thais lived within 25km of an ophthalmologist, and 88% lived within 50km of an ophthalmologist. Thus, the vast majority of Thai people live relatively close to an ophthalmologist’s office, even in areas outside of Bangkok. However, this calculation does not adequately describe access to care, since it does not describe both the supply and demand of ophthalmologists. A provider to population ratio, such as the O/P ratio, provides a better reflection of access to ophthalmologic care. We found considerable variation in the O/P ratio in Thailand, with Bangkok and surrounding areas having a higher concentration of ophthalmologists than the more distant provinces.
This study demonstrates the importance of assessing access to care on a sub-national scale. While the O/P ratio exceeded the 2010 WHO recommendation at the national level, almost three-quarters of the Thai population live in a province with an O/P ratio <1. Provinces with more vulnerable workers were less likely to have an O/P ratio ≥ 1. Vulnerable employment refers to self-employed workers who have no employees, and family members who work with these self-employed individuals. These types of workers were much more common in rural areas, where many farmers would likely be classified as having vulnerable employment. These observations were consistent with the district-level analyses, which found that districts with high populations of children and elderly, and a high proportion of rural residents, were less likely to meet the WHO recommendation of an O/P ratio ≥ 1. It is not surprising that rural areas have poorer access to eye care. Nonetheless, identification of areas with poorer access to ophthalmologic care is an important step to address the national eye health of Thailand, especially given a rapidly aging population with an increasing demand for cataract surgery and other ophthalmic services.
Since 2001, Thailand has extended government subsidized health coverage to all citizens, with cost sharing that is limited to 30 Baht per healthcare visit (< $1.00USD/per visit). Since the inception of this “30 Baht” program, it is estimated that more than 13.6 million formerly uninsured Thais have gained health insurance coverage.14 Under the 30 Baht program, people are allowed to visit an ophthalmologist within their home province or else receive a special referral to visit an ophthalmologist outside of their home province. This program may have increased the demand for ophthalmologic care, since many more people are now able to afford the visit to an ophthalmologist. It should be noted, however, that transportation to the medical visit is not covered by the program, which could effectively reduce access for the poorest individuals. There are additional programs in place to increase access to ophthalmic care to rural residents. For example, hospitals sponsor mobile clinics and cataract campaigns, although the coverage for these programs can be sporadic.
There were 9 residency programs listed in the 2008 directory, with programs distributed throughout the country. Having a residency program in the province was associated with a higher concentration of ophthalmologists, likely because residency programs require a large number of ophthalmologists to provide training. In addition, the ophthalmology residents themselves provide eye care, thereby increasing the concentration of ophthalmologists. It is also likely that ophthalmologists graduating from a residency program will tend to settle near the program at which they trained, further accentuating the imbalance in supply of ophthalmologists. If this is true, then establishing residency programs in areas of relative ophthalmologist shortage could help alleviate this imbalance.
We calculated the Gini coefficient to estimate the inequality in access to ophthalmologic care in Thailand. This number was relatively high (0.815), suggesting inequality in the distribution of ophthalmologists—most likely because of the disproportionately high proportion of ophthalmologists working in Bangkok. The Gini coefficient has been used previously to monitor access to physicians over time, and could be useful as a way to monitor for progress in the access to ophthalmologic care, both in Thailand and elsewhere.15
We acknowledge several limitations with this study. First, we relied on physician to population ratios based on administrative regions (e.g., provinces). Such ratios can provide a misleading picture of access to physicians if patients seek care outside of their home region16,17. This should be less of a problem in Thailand, however, since the government’s “30 Baht” health insurance scheme dictates that patients seek higher levels of care through referral hospitals within the province.14, 18 Thai patients are thus less likely to seek care outside of their home province, suggesting that the O/P ratios in this study provide a reliable indicator of access to ophthalmologic care. Second, we focused solely on ophthalmologists listed in the directory of the national ophthalmologic society. Although this should capture most if not all ophthalmologists, it did not provide an opportunity to determine access to specific services such as cataract surgery or subspecialty care. For example, we may have overestimated access to ophthalmologic surgery if not all ophthalmologists listed in the directory performed cataract surgery. Alternately, we could have underestimated access to eye care in general, since we did not include other eye care providers such as optometrists. However, optometrists do not provide the surgical services that ophthalmologists do and are not common in Thailand.19 Third, we assumed that all ophthalmologists listed in the directory worked full time, and that all resident ophthalmologists provided the equivalent of one-half an ophthalmologist. Different assumptions may have altered the provider-to-population ratios reported in this study. Fourth, this study discusses the geographical proximity and availability of providers, but does not fully address patient-related barriers to service utilization such as affordability and acceptability of care, or health perceptions and beliefs.20 Finally, this analysis uses ophthalmologist data from 2008, and projects the 2008 population from the 2000 Thai census. We used this dated information because both sources provided detailed information at the district level, whereas the currently available data from each of these sources contains only province-level statistics. We acknowledge that this analysis provides a snapshot of the year 2008, and that the situation may have changed in the past 5 years.
In conclusion, we found that the number of ophthalmologists in Thailand currently surpasses the number currently recommended by the WHO. Thailand needs to increase its number of ophthalmologists in order to meet the 2020 goal of 1 ophthalmologist per 50,000 persons. Although most Thais live within a reasonable distance from the nearest ophthalmologist, there was a relative shortage of ophthalmologists in rural areas; increasing the number of ophthalmologists in these areas would bring the country in closer alignment with the WHO’s recommendations for the year 2020. This information will be of use to national and provincial health authorities in Thailand and is a helpful example for other countries in southeast Asia.
Financial Support:
This work was made possible in part, by NIH-NEI EY02162 - Core Grant for Vision Research and an unrestricted grant from Research to Prevent Blindness.
Footnotes
None of the authors have any proprietary interests or conflicts of interest related to this submission.
This submission has not been published anywhere previously and is not simultaneously being considered for any other publication.
References
- 1.World Health Organization. Global initiative for the elimination of avoidable blindness. 1997; http://whqlibdoc.who.int/hq/1997/WHO_PBL_97.61_Rev.1.pdf. Accessed June 10, 2012.
- 2.World Health Organization. Global Initiative for the Elimination of Avoidable Blindness : action plan 2006–2011. 2007; vi, 89 p. Available at: http://whqlibdoc.who.int/publications/2007/9789241595889_eng.pdf. Accessed April 15, 2013.
- 3.Wibulpolprasert S, Pengpaibon P. Integrated strategies to tackle the inequitable distribution of doctors in Thailand: four decades of experience. Human Resources for Health. 2003;1; http://www.ncbi.nlm.nih.gov/pubmed/14641940. Accessed April 15, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suwannakiji T, Sirikanokwilai N, Wibulpolprasert S. Supply projection for physicians in Thailand over the next 25 years. Human Resources Development Journal. 1998; 2; http://www.who.int/hrh/en/HRDJ_2_2_04.pdf. Accessed June 10, 2012. [Google Scholar]
- 5.Wibulpolprasert S Thailand health profile 1999–2000. Bangkok: 2002. [Google Scholar]
- 6.National Statistical Office Thailand. Population and Housing Census 2000; http://web.nso.go.th/pop2000/pop_e2000.htm. Accessed October 1, 2011.
- 7.The World Bank. Thailand: World Development Indicators. 2011; http://api.worldbank.org/datafiles/THA_Country_MetaData_en_EXCEL.xls. Accessed May 28, 2012.
- 8.International Labour Office. Guide to the new Millennium Development Goals Employment Indicators: including the fill set of Decent Work Indicators. Geneva: International Labour Office; 2009. [Google Scholar]
- 9.WHO Multicentre Growth Reference Study Group. Reliability of anthropometric measurements in the WHO Multicentre Growth Reference Study. Acta Paediatr Suppl. 2006;450:38–46. [DOI] [PubMed] [Google Scholar]
- 10.Goodchild MF, Lam NS. Areal Interpolation: A Variant of the Traditional Spatial Problem. Geo-Processing. 1980;1:297–312. [Google Scholar]
- 11.Guagliardo MF, Ronzio CR, Cheung I, Chacko E, Joseph JG. Physician accessibility: an urban case study of pediatric providers. Health & place. 2004;10(3):273–283. [DOI] [PubMed] [Google Scholar]
- 12.Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33(5):545–557. [DOI] [PubMed] [Google Scholar]
- 13.Weiner JP. Prepaid group practice staffing and U.S. physician supply: lessons for workforce policy. Health Aff (Millwood). 2004;Suppl Web Exclusives:W4–43–59. [DOI] [PubMed] [Google Scholar]
- 14.Damrongplasit K, Melnick GA. Early results from Thailand’s 30 Baht Health Reform: something to smile about. Health Aff (Millwood). 2009;28(3):w457–466. [DOI] [PubMed] [Google Scholar]
- 15.Kobayashi Y, Takaki H. Geographic distribution of physicians in Japan. Lancet. 1992;340(8832):1391–1393. [DOI] [PubMed] [Google Scholar]
- 16.Newhouse JP. Geographic access to physician services. Annual review of public health. 1990;11:207–230. [DOI] [PubMed] [Google Scholar]
- 17.Kindig DA, Movassaghi H. The adequacy of physician supply in small rural counties. Health Aff (Millwood). 1989;8(2):63–76. [DOI] [PubMed] [Google Scholar]
- 18.Hughes D, Leethongdee S. Universal coverage in the land of smiles: lessons from Thailand’s 30 Baht health reforms. Health Aff (Millwood). 2007;26(4):999–1008. [DOI] [PubMed] [Google Scholar]
- 19.Tonkerdmonkon D, Yen L. Review of Optometry Status in Thailand: Supply and Demand. 2001; http://www.thaioptometry.org/OHCRTV4.pdf. Accessed April 15, 2013.
- 20.Jacobs B, Ir P, Bigdeli M, Annear PL, Van Damme W. Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2012;27(4):288–300. [DOI] [PubMed] [Google Scholar]


