Abstract
Background
There is growing evidence for motor impairments in children with autism spectrum disorder (ASD), including poor gross and fine motor performance, poor balance, and incoordination. However, there is limited evidence on the effects of motor interventions for this population.
Objective
In the present study, the effects of a physical therapy intervention using creative yoga on the motor and imitation skills of children with ASD were evaluated.
Design
This study had a pretest-posttest control group design.
Methods
Twenty-four children with ASD aged between 5 and 13 years received 8 weeks of a physical therapist-delivered yoga or academic intervention. Children were tested before and after the intervention using a standardized motor measure, the Bruininks-Oseretsky Test of Motor Performance–2nd Edition (BOT-2). The imitation skills of children using familiar training-specific actions (ie, poses for the yoga group and building actions for the academic group) were also assessed.
Results
After the intervention, children in the yoga group improved gross motor performance on the BOT-2 and displayed fewer imitation/praxis errors when copying training-specific yoga poses. In contrast, children in the academic group improved their fine motor performance on the BOT-2 and performed fewer imitation errors while completing the training-specific building actions.
Limitations
The study limitations include small sample size and lack of long-term follow-up.
Conclusions
Overall, creative interventions, such as yoga, are promising tools for enhancing the motor and imitation skills of children with ASD.
Autism spectrum disorder (ASD) is a neurological disorder characterized by impairments in social communication skills and the presence of restricted and repetitive behaviors.1 Apart from the diagnostic impairments, there is growing evidence for motor impairments in children with ASD such as poor balance and postural control, unsteady gait, and incoordination, as well as poor handwriting and manual dexterity skills.2–7 In fact, the motor performance of children with ASD is at the level of children with typical development (TD) who are one-half their chronological age.5 Motor delays have been reported as early as the first year of life in infants who later develop ASD, and the magnitude of these delays appears to increase with development.8,9 Imitation impairments emerge later in children with ASD and are often considered part of a generalized praxis deficit.10–14 Children with ASD may show spatial errors (eg, incorrect positioning of the moving limb in space), reversal errors (eg, waving with palm facing inward), and body-part-for-tool errors (eg, scissoring motions involving movements of the index and middle fingers) while performing actions on imitation, verbal command, and tool use.10–12 Both motor and imitation impairments could have cascading effects on the social, communication, and cognitive development of children with ASD.2,15–18 For example, children with poor motor skills may avoid playing with their peers and hence lack opportunities to build friendships with them.15,16 Similarly, poor praxis/imitation skills could limit a child’s ability to learn new functional skills, such as dressing and feeding,19,20 or social skills, such as gestures or joint social engagement.17,18 Given the evidence for motor impairments and their broader impact on social communication development, there is a clear need to devise interventions that could offer opportunities to improve both motor skills and their use in developing social communication skills in children with ASD.
Yoga is gaining popularity as a complementary and alternative therapy for multiple reasons. It is cost-effective given the minimal number of supplies required to complete the various tasks. Yoga offers multisystem experiences impacting several developing systems including motor (flexibility, strength, balance),21–23 perceptual (joint proprioception, kinesthesia),24 cardiorespiratory (heart rate variability, respiratory muscle strength),21–23 behavioral (attention, alertness),25 and social communication skills of children (social interactions, speech, and affect).26–28 Additionally, yoga-based activities are easy to learn and modifiable based on the age and level of functioning of the child. Yoga as provided in this study was made fun and creative through the use of songs, stories, games, and props to better contextualize the complex poses and breathing/gaze activities and hereafter will be termed Creative Yoga. Creative Yoga as offered in this study embraced the principles of motor learning such as repetitive task-specific practice of complex movements/postures requiring physical strength, balance, and coordination, clear opportunities for reinforcement and feedback, and, finally, opportunities for trial and error learning and free exploration.29,30 Further, clinical researchers are calling for pediatric physical therapist interventions to not be limited to the motor system alone and instead be more holistic with multisystem goals, as well as cascading effects on other developing systems (eg, social communication, behavioral, cognitive).31,32 However, there is limited preliminary evidence for efficacy of yoga in children with ASD,33 with suggestions for improved imitation and social participation and reduction in maladaptive and negative behaviors.34–37 Children with ASD between 8 and 14 years of age improved imitation of yoga poses and breathing exercises as well as gross motor actions such as jogging and running, and orofacial movements following 10 months of yoga training.34 Similarly, another study reported a decrease in maladaptive behaviors based on the Aberrant Behavior Checklist following 16 weeks of classroom yoga in a group of children with ASD who were compared with a control group of children with ASD receiving usual morning routines.35
Although the current yoga literature is limited in children with ASD, there is evidence from children with TD suggesting the positive effects of yoga on the balance, strength, flexibility, and motor speeds of children.38–42 For example, an intensive 24-week school-based yoga intervention including poses and breathing exercises improved the strength of hand and respiratory muscles in children compared with the control group engaged in regular classroom routines.38 Similarly, a 6-week randomized controlled trial using yoga intervention suggested improvements in the static balance of children with TD between 11 and 14 years of age compared with a no-intervention control group.39 Furthermore, research studies comparing yoga with regular physical activity have suggested better outcomes for children in the yoga group compared with the physical activity group.40,41 A 4-week yoga intervention (involving poses, breathing, relaxation) improved the motor planning and execution of children with TD during a problem-solving task compared with aerobic interventions (involving jogging, jumping, and stretching).41 This perhaps could be attributed to the positive effects of yoga on the motor (eg, motor speed, planning) and behavioral skills (eg, awareness, alertness) of children. Overall, yoga-based interventions could be a promising tool for children with ASD given the evidence from yoga studies involving children with TD and the initial studies conducted in children with ASD.
The primary goal of the current study was to compare the effectiveness of an 8-week physical therapist-delivered yoga intervention or academic intervention in children with ASD between 5 and 13 years of age. The academic intervention included sedentary activities usually practiced within school settings (eg, reading, arts, and crafts). Because of the nature of the activities practiced within each group, we hypothesized that the yoga group would improve their gross motor performance and the academic group would improve their fine motor performance on a standardized motor test. Additionally, we hypothesized that both groups would improve their imitation of familiar, training-specific actions following the intervention.
Methods
Participants
Twenty-four children with ASD between 5 and 13 years of age participated in the study, with 12 children each in the yoga and academic groups (Tab. 1). We estimated our sample size based on our past intervention study involving children with ASD who received similar multisystem, movement-based interventions.43–45 Participants were recruited by distributing fliers in the local schools and through online postings on autism websites. The initial screening process included parents completing the Social Communication Questionnaire46 and/or providing a medical record confirming an ASD diagnosis for their child. If the participating child did not show social communication delays on the Social Communication Questionnaire and the parents failed to provide a medical record, they were excluded. We further confirmed the ASD diagnosis using the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2).47 All 24 children received the diagnosis using ADOS-2, with comparison scores ranging from 5 to 10 indicating moderate to high severity of the disorder (Tab. 1). All participants had delays on the Social Communication Questionnaire and/or parents of participants provided a medical record confirming their child’s diagnosis. Four children were excluded during the screening process because of significant behavioral problems (eg, aggression, nonparticipation, or inattention) and/or communication impairments (eg, inability to follow simple commands during imitative actions). All parents signed the consent form approved by the University of Delaware Review Board before participating in the study. We matched the children in the yoga and the academic group on various criteria including the group demographics (age, sex, and socioeconomic status),48 autism severity (ADOS-2 comparison scores), and level of functioning (intelligence, adaptive functioning, and motor performance) (Tab. 1). Specifically, the Stanford-Binet Intelligence Scales, Fifth Edition,49 were used to assess level of intelligence; the Vineland Adaptive Behavior Scales, Second Edition,50 were used to assess the level of adaptive functioning; and the short form of the Bruininks-Oseretsky Test of Motor Proficiency-2nd Edition (BOT-2)51 was used to assess the level of motor functioning (Tab. 1). On the basis of standard scores on the short form of the BOT-2, children with scores below 30 were considered “well-below average,” those with scores between 30 and 45 were considered “below average,” those with scores between 45 and 55 were considered “average,” and those with scores above 55 were considered “above average.” In the current study, 6 children were “well below average,” 12 children were “below average,” and the remaining 6 children were “average” performers. None of the children performed “above average”; hence, all children had room for improvement in gross/fine motor skill performance at the point of study entry.
Table 1.
Demographics and Matching Criteria
| Yoga Group | Academic Group | P a | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Matching Criterion | Characteristic | Mean | SE | Range | No. of Participants | Mean | SE | Range | No. of Participants | |
| Demographic information |
Age | 7.77 | 0.5 | 5.5–11 | 7.8 | 0.7 | 5.11–12.5 | .98 | ||
| Sex | 11 boys; 1 girl | 11 boys; 1 girl | 1.00 | |||||||
| Socio-economic status | 56.5 | 2.2 | 40–66 | 52.5 | 2.9 | 29–66 | .3 | |||
| Ethnicity | 7 white; 5 Asian | 9 white; 1 Asian; 1 African American; 1 Hispanic | <.01 | |||||||
| Autism severity | ADOS-2b | 8.4 | 0.5 | 5–10 | 8.7 | 0.5 | 5–10 | .7 | ||
| Level of functioning | Stanford-Binet IQc (cognitive level) | 84.3 | 5.5 | 58–115 | 82.9 | 8.0 | 47–119 | .9 | ||
| VABS-IId (adaptive level) | 81.2 | 4.4 | 57–102 | 75.9 | 5.3 | 39–100 | .5 | |||
| Short form of BOT-2e (motor level) | 37.25 | 2.1 | 24–46 | 39.30 | 3.12 | 20–54 | .6 | |||
a P determined by t test or χ2 test.
bADOS-2 = Autism Diagnostic Observation Schedule, Second Edition.
cStanford-Binet Intelligence Scales, Fifth Edition, intelligence quotient (IQ) scores had a normative mean of 100 and an SD of 15.
dVineland Adaptive Behavior Scales, Second Edition (VABS-II), scores had a normative mean of 100 and an SD of 15.
eBruininks-Oseretsky Test of Motor Proficiency–2nd Edition (BOT-2) scores had a normative mean of 50 and an SD of 10.
Testing Measures
The study lasted 10 weeks, with a pretest session in the first week, 8 weeks of intervention, and a posttest session in the last week of participation. We used 2 testing measures, a standardized motor test administered during the testing sessions and an imitation test administered during the training sessions. An additional third measure was used at the end of the study for the parents to report on the social validity of the intervention. We used several strategies during the study to ensure comprehension and established an adequate communication system with the children. For example, we used pictures to illustrate the steps within each motor activity, simple and brief instructions, and provided 1 practice trial with manual feedback, if needed. Depending on the variable, either a single coder or 2 coders coded the entire dataset after establishing an interrater reliability of greater than 85% and an intrarater reliability of above 90% for a randomly selected 25% of the video dataset. This approach is consistent with our past intervention studies reporting behavioral coding variables.43–45 Coders discussed the coding definitions, coded videos independently, and later computed the correlations between the summated scores they assigned for each condition/domain. After the initial reliability was assessed, the coders met to establish consensus on the codes they disagreed on to establish interrater agreement of > 85%. After establishing interrater reliability of > 85%, the coders coded the dataset 1 more time to establish intrarater reliability of > 90% between the 2 iterations of coding the same set of videos spaced by a period of more than 2 weeks.
Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition (BOT-2)
The BOT-251 was administered in the pretest and posttest session to assess the generalized changes in motor performance following the intervention. The BOT-2 was selected over other measures of motor performance because it has high validity and reliability, and it allowed detailed evaluation of gross motor skills, such as balance and coordination, and fine motor skills, such as precision and integration, following the yoga/academic intervention. We used 2 gross motor and 2 fine motor subtests of the BOT-2, including the bilateral coordination (ability to synchronize upper and lower limbs), balance (postural control in standing and walking), fine motor precision (precise hand and finger control) (FMP), and fine motor integration (ability to integrate visual stimuli during motor control) (FMI) subtests. The testers were doctoral students in the laboratory with a background in occupational therapy/physical therapy. They were blinded to group assignments and interacted with children only during the testing sessions. We are reporting on the raw scores of the BOT-2 subtests. One child in the academic group was excluded from the BOT-2 analysis because of nonparticipation and inability to complete the posttest session.
Training-specific imitation test
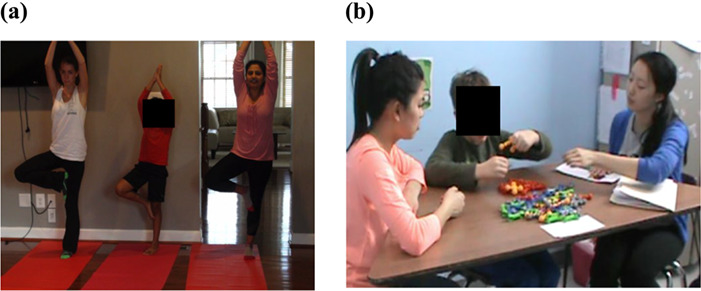
We developed a test using a subset of actions usually practiced within the training sessions to assess the imitation skills of children during the intervention. This test was administered by the trainer during the early, mid, and late training session. Specifically, for the yoga group, the test included sitting, standing, and lying poses involving upper and/or lower extremity (Fig. 1). The scoring for the test was based on imitation error classifications commonly used in the ASD literature11–13 and our past published studies.44,45 We coded the imitation errors performed by the child while executing the essential elements of a pose; for example, for the dog pose, the child was evaluated for 3 elements: hands and feet flat on the floor, knees and elbows straight, and hips bent at an acute angle. For the academic group, the test included actions such as rolling, pinching, pushing, and pulling using building materials such as Play-Doh (Hasbro, Pawtucket, RI, USA), LEGO (The LEGO Group, Billund, Denmark), and ZOOB (Alex Brands, Fairfield, CT, USA) (Fig. 1). For each action, errors ranged from 0 to 2, with higher scores indicating worse performance. A score of 2 indicated the child was unable to complete the action. A score of 1 indicated that the child completed the action but required verbal (repeated instruction), physical (manual hand-on-hand assistance), or visual assistance (repeated demonstration of the action) from trainers. Finally, a score of 0 indicated that the child completed the action independently without any assistance from trainers. We reported on the total percent of errors by summing the errors across all actions and dividing by the total number of errors possible given the number of steps involved (Fig. 1).
Figure 1.

Training-specific actions included in the imitation test for the yoga and academic groups (Play-Doh [Hasbro, Pawtucket, RI, USA]; LEGO/DUPLO [The LEGO Group, Billund, Denmark]; ZOOB [Alex Brands, Fairfield, CT, USA]).
Exit questionnaire
Parents completed an exit questionnaire at the end of the study to describe their overall experience and acceptance of the intervention. The exit questionnaire served as a measure of social validity and was used to assess whether the parents perceived the intervention to be socially meaningful for their child.52 The exit questionnaire had 6 statements regarding the overall efficacy, satisfaction, and therapeutic effects of the intervention (Tab. 2). The questionnaire was based on a 5-point Likert scale with responses ranging from 1 to 5, with 1 being “do not agree” and 5 being “strongly agree” with the statement.
Table 2.
Parent Responses on the 5-Point Likert Scale of the Exit Questionnairea
| Statement | Yoga Group | Academic Group | ||||
|---|---|---|---|---|---|---|
| Do Not Agree (1 or 2) | Agree (3) | Strongly Agree (4 or 5) | Do Not Agree (1 or 2) | Agree (3) | Strongly Agree (4 or 5) | |
| I found the intervention very useful for my child | 0/11 | 2/11 | 9/11 | 0/11 | 1/11 | 10/11 |
| I am satisfied with the overall intervention | 0/11 | 2/11 | 9/11 | 0/11 | 0/11 | 11/11 |
| I feel the training activities were easy for my child | 1/11 | 5/11 | 5/11 | 0/11 | 1/11 | 10/11 |
| I would recommend the intervention to other parentsb | 0/9 | 2/9 | 7/9 | 0/11 | 0/11 | 11/11 |
| I would continue practicing the activities after the studyb | 1/9 | 1/9 | 7/9 | 0/11 | 1/11 | 10/11 |
| I think the intervention benefited the motor skills of my child | 0/11 | 5/11 | 6/11 | 0/11 | 4/11 | 7/11 |
aData represent the number of parents with the indicated responses.
bTwo parents of children in the yoga group did not respond to this statement.
Training Protocol
The frequency-intensity-time-type principle for this study was as follows: frequency = 4 sessions/wk with 2 expert and 2 parent sessions; intensity = 40 to 45 minutes for expert and 20 to 25 minutes for parent sessions; time = 3 or 4 times/wk for 8 weeks; and type = yoga or academic activities. Expert sessions were delivered by a pediatric physical therapist (also a doctoral student and first author) after receiving significant training from the last author and consultants with Applied Behavioral Analysis or yoga expertise. Furthermore, the expert sessions involved a triadic context, that is, a child with ASD, a trainer, and a model (Suppl. Appendix 1, available at https://academic.oup.com/ptj). The models were university undergraduates who acted as a buddy to the child, modeled positive behaviors such as ready responses, and also copied the activities of the trainer. All models received at least 6 hours of training in the form of instructional manuals and videos as well as discussions with both authors before participating in the intervention sessions. To ensure training fidelity, a coder assessed the trainers’ and the models’ adherence to the training protocol using a checklist including general characteristics such as the environmental set-up and specific characteristics such as repetition and completion of activities (Suppl. Appendix 2, available at https://academic.oup.com/ptj). All the trainers and models adhered to the standard training protocol for the majority of the sessions (yoga group = 95.51% ± 0.41%; academic group = 91.38% ± 0.90%). All the parents were provided with instructional DVDs and manuals to deliver 2 sessions at home each week. Additionally, the trainer provided additional information to the parents regarding the home instructional DVD-based sessions and provided all the necessary materials, such as mats and props, to the yoga group, and art, craft, and building supplies to the academic group. All children completed at least 50% of the total training sessions (yoga group = 71.59% ± 3.73%; academic group = 80.21% ± 4.41%; P = .19), except 1 child in the yoga group who was, therefore, excluded from the final analysis. Eleven children in the yoga group were compared with the 12 children in the academic group.
Children practiced different activities within the yoga and academic groups (Tab. 3). Specifically, for the yoga group, we created a holistic intervention that could address the motor impairments and diagnostic social communication impairments of children with ASD. The training session included traditional yoga activities such as breathing, imitative poses, partner poses, and relaxation as well as context-appropriate social activities to encourage greeting/farewell songs, touch/contact games, and looking games (Tab. 3; see Supplementary Materials). The yoga poses were grouped around meaningful themes such as songs (eg, “Twinkle Twinkle Little Star”), stories (eg, “Goldilocks and the Three Bears”), and games (eg, a musical game). The lyrics for the songs and the stories were significantly modified to make it more generic and appropriate across the age groups. A music graduate student voice recorded all the songs/stories for this study. Additionally, we used various props during the breathing exercises, such as straws and pinwheels, to make the breathing activities clear and engaging for the children. The academic group engaged in several sedentary tabletop activities typically used within academic settings such as reading, arts and crafts, and building supplies such as Play-Doh, LEGO, and ZOOB (Tab. 3). Children would create art, craft, or build creations based on different themes such as the solar system, farm animals, and fruits and vegetables. Yoga facilitated motor skills such as balance, strength, and praxis/planning as well as social skills such as social contact, eye movements, and cooperative play. The academic/tabletop play also promoted fine motor coordination/planning as well as social skills such as social gaze and cooperative play. In both groups, trainers encouraged communication skills including verbal (commenting, responding, singing) and nonverbal gestural use (showing, pointing), and offered reminders for behavioral regulation such as attention and task-related focus. We also implemented common ASD treatment approaches such as the use of visual picture schedules to convey session structure and conditions, repetition and reinforcement when completing the activities, manual/visual feedback as needed, and structured space and materials to facilitate skill learning in the children. The academic intervention group served as a control for various social and therapeutic components mentioned earlier except for the gross motor coordination/posture and relaxation components of yoga.
Table 3.
Training Activities Practiced by Participants in the Yoga and Academic Groups
| Yoga Group | Academic Group |
|---|---|
| Hello: Child sings a song together with the trainer and the model | Hello: Child greets the model and the trainer |
| Breathing: Child practices breathing exercises with or without props (eg, nostril breathing, blowing pinwheels) | Reading: Child reads an age-appropriate book with the trainer and the model while taking turns with them |
| Contact and looking: Child practices social touch (eg, joining hands or feet to form a shape). Child practices eye/head movements toward social and nonsocial stimuli (eg, looking at bouncing ball). | Building: Child builds various creations using building supplies such as Play-Doh,a LEGO,b and ZOOBc (eg, Lego car, Play-Doh snow man) |
| Poses/partner poses: Child practices poses on his or her own and together with the trainer and the model | Arts and crafts: Child makes various creations by coloring/painting/drawing as well as cutting and pasting |
| Relaxation: Child lies down and remains still, with prerecorded verbal imagery playing in the background | Clean up: Child helps the trainer and the model clean up the working station |
| Bye: Child bids farewell by singing a song together with the trainer and the model | Bye: Child bids farewell to the trainer and the model |
aHasbro, Pawtucket, RI, USA.
bThe LEGO Group, Billund, Denmark.
cAlex Brands, Fairfield, CT, USA.
Data Analysis
For the BOT-2, we conducted a repeated-measures analysis of variance (ANOVA) with testing session (pretest, posttest) and subtest type (bilateral coordination, balance, FMP, FMI) as the within-participants factors, and group (yoga group, academic group) as the between-participants factor. For the training-specific imitation test, we conducted separate 1-way repeated-measures ANOVA for the yoga and the academic group with training session (early, mid, late) as the within-participants factor. For the exit questionnaire, we report a count for the number of parents who responded with 1 or 2 (do not agree), 3 (agree), and 4 or 5 (strongly agree) for each of the statements. Finally, we determined the Pearson correlations of several child-specific variables, such as age, ADOS-2 comparison and total scores, and intelligence quotient (IQ) levels, with the intervention effectiveness and dosage. Specifically, for intervention effectiveness, we conducted correlations for only those variables that significantly improved after the intervention. For the yoga group, we used the change in BOT-2 bilateral coordination as well as imitation scores from early to mid/late sessions. For the academic group we used the change in BOT-2 FMI, BOT-2 FMP, and imitation scores from early/mid to late session. For the intervention dosage, we correlated child-specific variables with the proportion of sessions completed by each child. To be clear, dosage was defined as follows: (number of sessions completed/32) × 100, with 32 sessions provided in total, 16 by physical therapists and 16 by parents. We checked our data for parametric assumptions using the Mauchly Test of Sphericity, and Greenhouse-Geisser corrections were applied in case of violations. The significance was set at P ≤ .05, and further analysis was conducted using post hoc dependent t tests with Bonferroni corrections applied for multiple comparisons. We are also reporting on the effect sizes using the Cohen d, with d ≥ 0.2 indicating a small effect, d ≥ 0.5 indicating a medium effect, and d ≥ 0.8 indicating a large effect.
Role of the Funding Source
The first author’s effort on this project was partially supported by the University Graduate Fellowship from the Office of Graduate and Professional Development at the University of Delaware, and the last author’s effort on this project and manuscript was supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health (NIH) (grant no. U54-GM104941) (Principal investigator: S. Binder-Macleod). The funders played no role in the design, conduct, or reporting of this study.
Results
Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition
The repeated-measures ANOVA for BOT-2 revealed a significant main effect of testing session (F1,20 = 17.18; P < .01; partial η2 = 0.46) and subtest type (F3,60 = 57.84; P < .01; partial η2 = 0.74), a 2-way subtest type × group interaction (F3,60 = 2.85; P = .05; partial η2 = 0.13), and 3-way testing session × subtest type × group interaction (F3,60 = 2.95; P = .04; partial η2 = 0.13). We further analyzed the 3-way interaction, testing session × subtest type × group using post hoc t tests. The post hoc tests indicated that the yoga group improved their performance for the gross motor subtest, bilateral coordination subtest in the posttest compared with the pretest session (P < .006 after Bonferroni correction; d = 0.56 [medium effect]) (Fig. 2A) with no changes for any of the other subtests. The academic group showed statistical improvements in both the fine motor subtests (ie, FMI and FMP) in the posttest compared with the pretest session with no changes on the gross motor subtests (P = .03; d = 0.30 and 0.32 [small effects]) (Fig. 2B).
Figure 2.
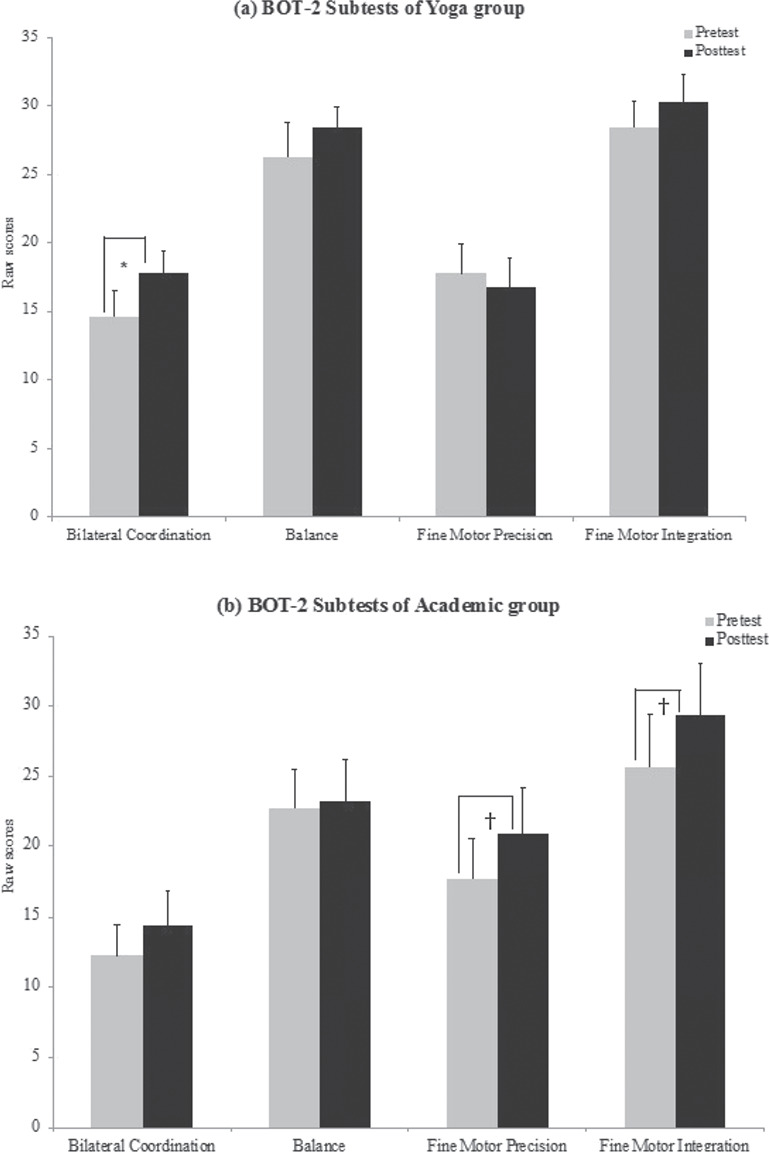
Raw scores for the Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition (BOT-2) subtests during the pretest and posttest sessions for the yoga group (A) and the academic group (B). *P = .006. †P = .03.
Training-specific Imitation Test
The 1-way repeated-measures ANOVA for the yoga and academic groups indicated a significant main effect of training (yoga group: F2,20 = 10.32; P < .01; partial η2 = 0.51; academic group: F2,22 = 5.12; P = .03; partial η2 = 0.32). The post hoc tests indicated that the yoga group reduced the total percentage of imitation errors in the mid and late training session compared with the early training session (P < .02 after Bonferroni correction; d = 0.96 and 1.48 [large effects]) (Fig. 3). Similarly, the academic group reduced the total percentage of imitation errors in the late session compared with the early session (P < .02 after Bonferroni correction; d = 0.83 [large effect]) and a statistical trend for reduced errors in the late compared with the mid training session (P = .03; d = 0.81) (Fig. 3).
Figure 3.
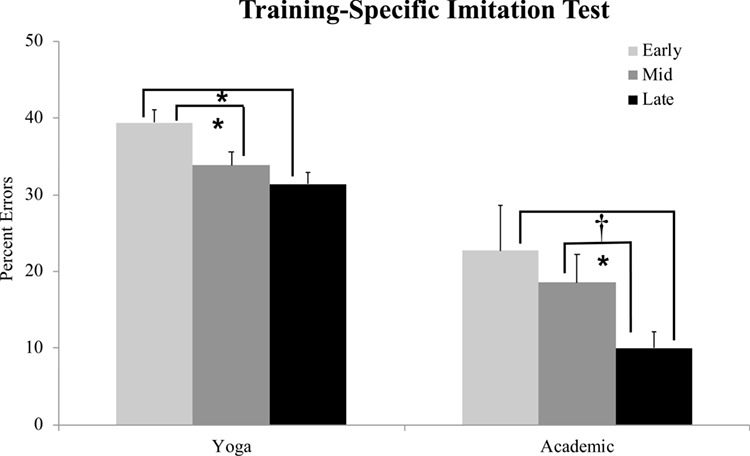
Percentage of imitation errors during the early, mid, and late training sessions for the yoga group and the academic group. *P ≤ .003. †P = .03.
Exit Questionnaire
The exit questionnaire was completed by 11 parents in each group, because 1 parent in the academic group did not fill out the questionnaire and 1 child in the yoga group was excluded from the final analysis because the training intensity was < 50% (Tab. 2). Most of the parents from both groups strongly agreed (score of 4 or 5) that the intervention was useful, that they would continue practicing similar activities, and that they would recommend it to other parents. However, between the 2 groups, there were relatively fewer parents in the yoga group who responded “strongly agree,” especially regarding the ease of training activities for their child. This could be because yoga-related activities were novel and not often practiced whereas the academic activities were similar to those practiced at school or home. Furthermore, it is possible that parents in the academic group perceived the training activities, such as reading books and coloring/drawing, to have a positive impact on the child’s school performance and, hence, to be more useful for the child than the yoga activities.
Correlations Between Intervention Dosage and Effectiveness and Child-specific Factors
Pearson correlations determined for each group indicated that children’s IQ levels strongly correlated with the intervention outcome variables (the BOT-2 and the imitation scores). For changes in BOT-2 scores, children’s IQ levels positively correlated with improvements in the BOT-2 FMI scores of the academic group (r = 0.71; P = .02), but not for the yoga group (r = −0.35; P = .29). This meant that the children with higher IQ within the academic group showed more fine motor improvements following the intervention than those with lower IQ. For changes in imitation scores, children’s IQ levels negatively correlated with training-related improvements in the imitation performance for the yoga group (r = −0.69; P = .02) but not for the academic group (r = −0.50; P = .1). In short, in the yoga group, children with lower IQ showed greater improvements in pose imitation following training. None of the other child-specific factors (ie, age, autism severity) correlated with the intervention effectiveness variables or with the intervention dosages.
Discussion
Generalized Effects on the Motor Skills of Children with ASD
The yoga group demonstrated generalized improvements for a standardized measure, bilateral coordination subtest of BOT-2 administered before and after the intervention. The current evidence for yoga is limited in the ASD population,33 but the literature in children with TD suggests a positive impact of yoga on several motor domains such as strength, endurance, speed, flexibility, and coordination.21–23,38–42 In general, improved motor functioning following yoga has been attributed to improved musculoskeletal health such as increased capillary formation in muscle tissue, alternate recruitment of motor neurons to avoid muscular fatigue, elongation of elastic connective and muscle tissue, and improved perception of performed movements.22,42 Specifically, improvements in joint proprioception, that is, the ability to sense joint position, could result in better coordination between moving body segments. In another study, 4 weeks of yoga training enhanced the joint proprioception in a group of individuals who had visual impairments and were between 10 and 19 years of age.24 Similarly, in our study, continuous practice of different poses/postures in lying, sitting, and standing could have improved the proprioceptive input from the joints and enhanced children’s awareness of their body movements. Although, the medium effect sizes observed for motor coordination are promising, it is possible that relatively longer training durations could result in greater generalized changes in the motor functioning/musculoskeletal health of children. We would like to add that our yoga sessions included a mix of traditional yoga elements such as poses and breathing as well as nontraditional versus elements such as looking and contact games. Therefore, it is difficult to tease apart the effects of traditional vs nontraditional yoga elements on the motor coordination of children. However, the selective improvement of children in the gross motor subtest of BOT-2 could be a direct result of the poses and the partner poses practiced during the training sessions, because these were the only activities requiring significant whole-body movements.
Surprisingly, the yoga group did not show any improvements in the balance subtest, which could be attributed to the differences in the training and the testing activities. To be clear, the BOT-2 balance subtest uses a mix of static (eg, standing on 1 leg) and dynamic activities (eg, walking heel-to-toe), whereas the majority of the yoga training focused on the static balance of children (eg, holding a tree pose) for the majority of the training period. Moreover, the balance subtest involves children holding a posture with and without visual input; however, during the training period, children practiced holding the poses with the help of visual input. Thus, it is possible that the changes in balance due to the yoga intervention did not generalize to a standardized measure of balance.
The academic group showed improvements in the fine motor subtests of BOT-2 (ie, FMP and FMI). The academic group practiced activities typically included within the school settings of children with ASD, for example, reading, building, and arts and crafts to promoting social interactions, engagement, and creativity. All these activities required isolated and controlled finger and hand movements as well as eye-hand coordination while grasping (crayons, scissors, blocks) and manipulating the objects (rolling, folding, cutting, pressing). Therefore, it is not surprising that the academic group improved on the FMI and FMP subtests of BOT-2. On the other hand, the smaller effect sizes in the academic group could possibly indicate smaller scope for improvement in this domain as children were already receiving occupational therapy/special education experiences that improved their fine motor performance within school settings. It is estimated that children spend about 30% to 60% of their school time completing fine motor activites.53 Nevertheless, therapies centered around arts (drawing, coloring), crafts (cutting, folding paper), and building (LEGO, Play-Doh) would be beneficial for children with ASD demonstrating fine motor impairments.53–55
Training-specific Effects on the Imitation Skills of Children With ASD
Both groups improved their imitation skills for training-specific actions, that is, poses for the yoga group and building actions for the academic group. The improvements in the imitation skills of children following the intervention are not surprising because both the interventions were primarily delivered within an imitation context. Social monitoring skills, that is, visually monitoring the actions of social partners, are extremely important for strong imitation performance.17–19 Children with ASD often have reduced eye contact and monitoring of others’ actions,56 which impacts their ability to observe and copy actions of others. During both yoga and academic tabletop play, the children had to observe and copy the actions of the trainer and model. Hence, the training activities may have improved the social monitoring and turn-taking abilities of children resulting in improved imitation of the familiar and novel actions following the training. Children’s motor coordination skills are also closely related to their imitation performance.2,11,17,19 In this study, children in both groups improved their motor coordination (gross or fine motor) skills following the intervention on the BOT-2. We believe that their motor improvements could have translated to improved imitation skills. There is limited evidence on the effects of yoga on imitation skills of children with ASD, with only 1 study reporting better imitation of yoga poses, breathing exercises, vocalizations, and orofacial movements as well as increased eye contact with social partners following an intensive 10- to 20-month yoga intervention.34 Therefore, the current results are encouraging in that creative movement interventions such as yoga could improve the imitation skills of children with ASD for familiar and unfamiliar actions.
Furthermore, the current treatment approaches for imitation, such as reciprocal imitation training and video modeling, primarily target social imitation (eg, greeting) and object imitation (eg, brushing teeth) in children with ASD. Specifically, reciprocal imitation training is an adult- or peer-delivered intervention in a naturalistic and socially interactive environment to promote the spontaneous imitation of children with ASD.57,58 On the other hand, video modeling includes watching the video clips of target behaviors along with opportunities to copy the televised behaviors.59,60 Although both approaches are successful in improving imitation skills of children with ASD, they do not focus on motor imitation or practice of motor skills. Overall, our study adds to the current body of knowledge on movement-based interventions, along with its potential to improve the fine/gross motor imitation skills of children with ASD.
Effects of Child-specific Factors on Intervention Effectiveness and Dosage
We found that IQ negatively correlated with change in imitation scores in the yoga group, which suggested that children with lower IQ and lower motor performance (perhaps with more scope for improvement) also showed greater improvements in spite of a relatively short 8-week intervention. On the other hand, for the academic group, IQ was positively correlated with changes in BOT-2 FMI scores. Perhaps fine motor skills were at a higher level in the case of children with higher IQ enough to produce short-term improvements within an 8-week period. However, for children with lower IQ, greater fine motor practice was required to significantly impact performance. None of the other child-specific variables, such as age range and the degree of autism severity, correlated with the dosage and the overall effectiveness of the intervention. Overall, these results should be treated with caution given the small sample size of our study. We recommend that future studies continue to investigate the associations between the functioning of children with ASD (IQ, severity) and intervention efficacy and dosage.
Limitations and Future Directions
Our sample size was relatively small, with a wider age range of children and a mix of high- and low-functioning children with ASD resulting in a relatively heterogeneous study sample. However, we ensured homogeneity between the 2 intervention groups by matching the children on various demographic, cognitive, motor, and adaptive behaviors. We also excluded children with severe behavioral challenges and nonparticipation, which could limit the generalizability of this intervention. Secondly, our training duration (8 weeks of intervention) was relatively shorter but intensive, with 4 sessions (2 expert and 2 parent) being delivered each week. There was some variability in terms of the number of parent sessions provided to each child. Furthermore, the training sessions involved an adult model instead of a peer model; however, it was difficult to recruit age-matched peers in each instance because many children with ASD lacked consistent friendships. We were unable to conduct long-term follow-ups after the completion of the study and hence are unable to comment on the long-term maintenance of study effects or generalization to other settings. Although we value the medium and large effects on imitation and motor performance seen in the yoga group, we also advise clinicians and therapists to cautiously interpret the study results because of the aforementioned limitations. In terms of future directions, we suggest conducting larger randomized controlled trials in children with wide-ranging autism-specific symptomology. Furthermore, we suggest using both standardized and training-specific outcome measures, masked assessors, as well as short-term and long-term follow-ups to evaluate the maintenance of training effects. Finally, we recommend that future studies explore the associations between factors such as age, autism severity, and cognitive levels and the intervention dosage and effectiveness of yoga in children with ASD.
Recommendations for Clinicians and Researchers
Given the rising evidence for motor impairments in children with ASD and its strong association with social communication and behavioral impairments,15,16 motor interventions such as yoga could be beneficial for children with ASD. In this section, we have provided some recommendations for clinicians and researchers regarding the use of yoga in children with ASD. First, in terms of intervention dosage, it is usually recommended to practice yoga 2 to 3 times per week for shorter periods (20–30 minutes) in young preschoolers and longer periods (30–60 minutes) in school-age children.61 Second, a yoga session should include activities such as breathing exercises, attentional focus/gaze control along with chanting/singing, yoga poses done face to face in parallel or with a partner, relaxation poses, as well as a period of reflection/thankfulness (see exemplar video content under Supplementary Materials).21–23,37,61
Poses could change week to week with gradual progression from simple to complex whole-body movements. The time spent within each activity could be varied based on the child’s interest and attentional capacities. For example, a child with attention deficits/disruptive behaviors could benefit from breathing and relaxation exercises whereas a child with motor impairments will benefit more from individual and partner poses. Third, the intervention should be socially embedded and inherently engaging for children. For example, in the current study, we used a triadic context involving a trainer, a model, and a child to promote natural communication such as turn-taking, spontaneous and responsive conversations, and gestural hand use. In addition, we used engaging themes involving stories, songs, and musical games to make the sessions fun and inherently motivating for children. Finally, the training set-up should include appropriate props for better contextual understanding as well as appropriate communication strategies to interact with children with ASD32,37 (eg, picture schedules to facilitate transitions between activities, predictable and familiar environment/trainers across sessions, adequate breaks, use of prompts, and establishment of an appropriate communication system with the children).
Conclusion
The current study explored the effects of a physical therapist-delivered yoga intervention on the motor and imitation skills of children with ASD between 5 and 13 years of age. Our findings show that an 8-week yoga intervention leads to generalized and training-specific improvements in gross motor and imitation skills of children. To elaborate, generalized improvements refer to improvements in the standardized BOT-2 as these activities were not practiced during the intervention and were administered by a novel tester, who interacted with the children only during the testing sessions. Training-specific improvements refer to improvements in the imitation skills for actions practiced throughout the intervention with a familiar trainer. Furthermore, reports from the exit questionnaire indicated that the parents viewed both interventions as useful and beneficial for their child. Overall, given the growing evidence for the presence of motor impairments and physical inactivity in children with ASD and its strong association with their social communication and behavioral impairments, we believe that physical therapists have a significant role in addressing the gross motor/physical activity impairments of children with ASD and physical therapist-delivered creative movement interventions utilizing music and yoga should be an essential part of the standard of care for children with ASD.
Appendix 1
Training setup indicating the triadic context during the yoga session (a) and the academic session 740 (b).
Appendix 2
Fidelity Checklist
| Checklist Criterion | Characteristic |
|---|---|
| General characteristics | 1. Environmental setup: the trainer sets up the room, such as appropriate lighting and limited distractions within the child’s vicinity |
| 2. Incremental prompts: the trainer provides incremental prompts to the child if he or she is unable to perform the activity (ie, visual, verbal, and physical hands-on-hands assistance) |
|
| 3. Eye contact: the trainer encourages the child to maintain eye contact during social interactions | |
| 4. Social interactions: the trainer encourages the child to indulge in spontaneous and responsive verbalizations | |
| 5. Social praise: both the trainer and the model provide verbal and gestural praise to the child throughout the session | |
| 6. Picture board: the trainer uses the picture board to explain the training activities and transition between activities | |
| 7. Asking for help: the trainer and the model ask the child to help throughout the session (eg, “Can you help laying down the mats?”) | |
| Specific characteristics | 1. Ready position: the trainer ensures that the child is ready for the activity (eg, cross-legged sitting for breathing in the yoga group or tabletop sitting for reading in the comparison group) |
| 2. Activity instructions: the trainer provides appropriate instructions before starting any activity (eg, “Today we are going to do poses on a story theme.”) | |
| 3. Repetition: the trainer repeats each activity twice to ensure learning | |
| 4. Activity completion: the trainer ensures that the child completes the critical elements within each activity |
M. Kaur, PT, PhD, Department of Physical Therapy, MGH Institute of Health Professions, Charlestown, Massachusetts
A. Bhat, PT, PhD, Department of Physical Therapy, Biomechanics and Movement Sciences Program, University of Delaware, 540 S College Avenue, Newark, DE 19713 (USA) and Department of Psychological and Brain Sciences, Behavioral Neuroscience program, University of Delaware
Author Contributions and Acknowledgments
Concept/idea/research design: M. Kaur, A. Bhat
Writing: M. Kaur, A. Bhat
Data collection: M. Kaur, A. Bhat
Data analysis: M. Kaur, A. Bhat
Project management: M. Kaur, A. Bhat
Fund procurement: M. Kaur, A. Bhat
Providing participants: A. Bhat
Providing facilities/equipment: A. Bhat
Providing institutional liaisons: A. Bhat
Clerical/secretarial support: M. Kaur, A. Bhat
Acknowledgments
The authors thank the study participants and undergraduate student Kristen Arborio and graduate student Sara Izadi for assistance with data collections. The authors also thank consultant Yana Kofman, PT, DPT, at The Yoga Way Clinic, Morristown, NJ, for her initial recommendations on yoga activities for children with ASD. Ms Kofman is a registered yoga teacher who has been trained in Yoga for the Special Child.
Funding
A. Bhat was supported by the Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health (NIH) (grant no. U54-GM104941) (Principal investigator: S. Binder-Macleod). M. Kaur was supported by the University Graduate Fellowship from the Office of Graduate and Professional Development, University of Delaware.
Disclosure
The authors completed the ICJME Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
This manuscript was written in partial fulfillment of M. Kaur’s dissertation requirements for Doctor of Philosophy in Biomechanics and Movement Sciences (“Creative Yoga Intervention for Children with Autism Spectrum Disorder,” University of Delaware, 2016).
Ethics Approval
This study was approved by the University of Delaware Institutional Review Board. All parents signed the consent form approved by the University of Delaware Review Board before participating in the study.
References
- 1. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Arlington, VA, USA: American Psychiatric Association; 2013. [Google Scholar]
- 2. Bhat AN, Landa RJ, Galloway JC. Current perspectives on motor functioning in infants, children, and adults with autism spectrum disorders. Phys Ther. 2011;91:1116–1129. [DOI] [PubMed] [Google Scholar]
- 3. Chukoskie L, Townsend J, Westerfield M. Motor skill in autism spectrum disorders: a subcortical view. Int Rev Neurobiol. 2013;113:207–249. [DOI] [PubMed] [Google Scholar]
- 4. Kaur M, Srinivasan SM, Bhat AN. Comparing motor performance, praxis, coordination, and interpersonal synchrony between children with and without autism spectrum disorder (ASD). Res Dev Disabil. 2017;72:79–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Staples KL, Reid G. Fundamental movement skills and autism spectrum disorders. J Autism Dev Disord. 2010;40:209–217. [DOI] [PubMed] [Google Scholar]
- 6. Mari M, Castiello U, Marks D, Marraffa C, Prior M. The reach-to-grasp movement in children with autism spectrum disorder. Philos Trans R Soc Lond B Biol Sci. 2003;358:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rinehart NJ, Tonge BJ, Iansek R et al. Gait function in newly diagnosed children with autism: cerebellar and basal ganglia related motor disorder. Dev Med Child Neurol. 2006;48:819–824. [DOI] [PubMed] [Google Scholar]
- 8. Kaur M, Srinivasan SM, Bhat AN. Atypical object exploration in infants at-risk for autism during the first year of life. Front Psychol. 2015;6:798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lloyd M, MacDonald M, Lord C. Motor skills of toddlers with autism spectrum disorders. Autism. 2013;17:133–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Williams JH, Whiten A, Singh T. A systematic review of action imitation in autistic spectrum disorder. J Autism Dev Disord. 2004;34:285–299. [DOI] [PubMed] [Google Scholar]
- 11. Mostofsky SH, Dubey P, Jerath VK, Jansiewicz EM, Goldberg MC, Denckla MB. Developmental dyspraxia is not limited to imitation in children with autism spectrum disorders. J Int Neuropsychol Soc. 2006;12:314–326. [DOI] [PubMed] [Google Scholar]
- 12. Dewey D, Cantell M, Crawford SG. Motor and gestural performance in children with autism spectrum disorders, developmental coordination disorder, and/or attention deficit hyperactivity disorder. J Int Neuropsychol Soc. 2007;13:246–256. [DOI] [PubMed] [Google Scholar]
- 13. Vanvuchelen M, Roeyers H, De Weerdt W. Nature of motor imitation problems in school-aged boys with autism: a motor or a cognitive problem? Autism. 2007;11:225–240. [DOI] [PubMed] [Google Scholar]
- 14. Rogers SJ, Bennetto L, McEvoy R, Pennington BF. Imitation and pantomime in high-functioning adolescents with autism spectrum disorders. Child Dev. 1996;67:2060–2073. [PubMed] [Google Scholar]
- 15. MacDonald M, Lord C, Ulrich DA. The relationship of motor skills and social communicative skills in school-aged children with autism spectrum disorder. Adapt Phys Activ Q. 2013;30:271–282. [DOI] [PubMed] [Google Scholar]
- 16. Radonovich K, Fournier KA, Hass CJ. Relationship between postural control and restricted, repetitive behaviors in autism spectrum disorders. Front Integr Neurosci. 2013;7:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dziuk MA, Larson JC, Apostu A, Mahone EM, Denckla MB, Mostofsky SH. Dyspraxia in autism: association with motor, social, and communicative deficits. Dev Med Child Neurol. 2007;49:734–739. [DOI] [PubMed] [Google Scholar]
- 18. Dadgar H, Rad JA, Soleymani Z, Khorammi A, McCleery J, Maroufizadeh S. The relationship between motor, imitation, and early social communication skills in children with autism. Iran J Psychiatry. 2017;12:236–240. [PMC free article] [PubMed] [Google Scholar]
- 19. McDuffie A, Turner L, Stone W, Yoder P, Wolery M, Ulman T. Developmental correlates of different types of motor imitation in young children with autism spectrum disorders. J Autism Dev Disord. 2007;37:401–412. [DOI] [PubMed] [Google Scholar]
- 20. Ingersoll B, Meyer K. Examination of correlates of different imitative functions in young children with autism spectrum disorders. Res Autism Spectr Disord. 2011;5:1078–1085. [Google Scholar]
- 21. Birdee GS, Yeh GY, Wayne PM, Phillips RS, Davis RB, Gardiner P. Clinical applications of yoga for the pediatric population: a systematic review. Acad Pediatr. 2009;9:212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Galantino ML, Galbavy R, Quinn L. Therapeutic effects of yoga for children: a systematic review of the literature. Pediatr Phys Ther. 2008;20:66–80. [DOI] [PubMed] [Google Scholar]
- 23. Serwacki M, Cook-Cottone C. Yoga in the schools: a systematic review of the literature. Int J Yoga Therap. 2012;22:101–109. [PubMed] [Google Scholar]
- 24. Mohanty S, Pradhan B, Nagathna R. The effect of yoga practice on proprioception in congenitally blind students. Br J Vis Impair. 2014;32:124–135. [Google Scholar]
- 25. Jensen PS, Kenny DT. The effects of yoga on the attention and behavior of boys with attention-deficit/hyperactivity disorder (ADHD). J Atten Disord. 2004;7:205–216. [DOI] [PubMed] [Google Scholar]
- 26. Harrison LJ, Manocha R, Rubia K. Sahaja yoga meditation as a family treatment programme for children with attention deficit-hyperactivity disorder. Clin Child Psychol Psychiatry. 2004;9:479–497. [Google Scholar]
- 27. Beauchemin J, Hutchins TL, Patterson F. Mindfulness meditation may lessen anxiety, promote social skills, and improve academic performance among adolescents with learning disabilities. Complement Health Pract Rev. 2008;13:34–45. [Google Scholar]
- 28. Narasimhan L, Nagarathna R, Nagendra HR. Effect of integrated yogic practices on positive and negative emotions in healthy adults. Int J Yoga. 2011;4:13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shumway-Cook A, Woollacott M. Motor Control: Translating Research in Clinical Practice. 3rd ed. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 30. Schmidt RA, Wrisberg CA. Motor Learning and Performance. Champaign, IL, USA: Human Kinetics; 2000. [Google Scholar]
- 31. Lobo MA, Harbourne RT, Dusing SC, McCoy SW. Grounding early intervention: physical therapy cannot just be about motor skills anymore. Phys Ther. 2013;93:94–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Srinivasan S, Bhat A. Music and movement interventions for children with autism Spectrum disorders: embodied interventions for multisystem development. Front Integr Neurosci. 2013;7:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gwynette MF, Warren NJ, Warthen J et al. Yoga as an intervention for patients with autism spectrum disorder: a review of the evidence and future directions. Autism Open Access. 2015;5:2. [Google Scholar]
- 34. Radhakrishna S. Application of integrated yoga therapy to increase imitation skills in children with autism spectrum disorder. Int J Yoga. 2010;3:26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Koenig KP, Buckley-Reen A, Garg S. Efficacy of the get ready to learn yoga program among children with autism spectrum disorders: a pretest–posttest control group design. Am J Occup Ther. 2012;66:538–546. [DOI] [PubMed] [Google Scholar]
- 36. Rosenblatt LE, Gorantla S, Torres JA et al. Relaxation response–based yoga improves functioning in young children with autism: a pilot study. J Altern Complement Med. 2011;17:1029–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kenny M. Integrated movement therapy™: yoga-based therapy as a viable and effective intervention for autism spectrum and related disorders. Int J Yoga Therap. 2002;12:71–79. [Google Scholar]
- 38. Mandanmohan JL, Udupa K, Bhavanani AB. Effect of yoga training on handgrip, respiratory pressures and pulmonary function. Indian J Physiol Pharmacol. 2003;47:387–392. [PubMed] [Google Scholar]
- 39. Hotkar JM. Yoga for agility and balance of slum school students. Yoga-mimamsa. 2009;41:264–270. [Google Scholar]
- 40. Manjunath NK, Telles S. Improved performance in the Tower of London test following yoga. Indian J Physiol Pharmacol. 2001;45:351–354. [PubMed] [Google Scholar]
- 41. D'souza C, Avadhany S. Effects of yoga training and detraining on physical performance measures in prepubertal children: a randomized trial. Indian J Physiol Pharmacol. 2014;58:61–68. [PubMed] [Google Scholar]
- 42. Tran MD, Holly RG, Lashbrook J, Amsterdam EA. Effects of hatha yoga practice on the health-related aspects of physical fitness. Prev Cardiol. 2001;4:165–170. [DOI] [PubMed] [Google Scholar]
- 43. Srinivasan SM, Eigsti I-M, Gifford T, Bhat AN. The effects of embodied rhythm and robotic interventions on the verbalization patterns of children with autism spectrum disorder (ASD). Res Autism Spectr Disord. 2016;27:54–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Srinivasan SM, Lynch KA, Bubela DJ, Gifford TD, Bhat AN. Effect of interactions between a child and a robot on the imitation and praxis performance of typically developing children and a child with autism: a preliminary study. Percept Mot Skills. 2013;116:885–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Srinivasan SM, Kaur M, Park IK, Gifford TD, Marsh KL, Bhat AN. The effects of rhythm and robotic interventions on the imitation/praxis, interpersonal synchrony, and motor performance of children with autism spectrum disorder (ASD): a pilot randomized controlled trial. Autism Res Treat. 2015;2015:736516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rutter M, Bailey A, Lord C. Social Communication Questionnaire. Los Angeles, CA, USA: Western Psychological Services; 2003. [Google Scholar]
- 47. Lord C, Rutter M, DiLavore PC et al. Autism Diagnostic Observation Schedule. Second ed. Torrance, CA, USA: Western Psychological Services; 2012. [Google Scholar]
- 48. Hollingshead AB. Four Factor Index of Social Status. New Haven, CT, USA: Yale University, Department of Psychology; 1975. [Google Scholar]
- 49. Roid GH. Stanford-Binet Intelligence Scales. Fifth ed. Itasca, IL: Riverside Publishing; 2003. [Google Scholar]
- 50. Sparrow SS, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales, Second Edition. Toronto, Canada: Pearson; 2005. [Google Scholar]
- 51. Bruininks RH, Bruininks BD. Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition. Minneapolis, MN, USA: NCS Pearson; 2005. [Google Scholar]
- 52. Schwartz IS, Baer DM. Social validity assessments: Is current practice state of the art? J Appl Behav Anal. 1991;24:189–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. McHale K, Cermak SA. Fine motor activities in elementary school: Preliminary findings and provisional implications for children with fine motor problems. Am J Occup Ther. 1992;46:898–903. [DOI] [PubMed] [Google Scholar]
- 54. Case-Smith J. Effects of occupational therapy services on fine motor and functional performance in preschool children. Am J Occup Ther. 2000;54:372–380. [DOI] [PubMed] [Google Scholar]
- 55. Reid, Chiu T, Sinclair G, Wehrmann S, Naseer Z. Outcomes of an occupational therapy school-based consultation service for students with fine motor difficulties. Can J Occup Ther. 2006;73:215–224. [DOI] [PubMed] [Google Scholar]
- 56. Dawson G, Toth K, Abbott R et al. Early social attention impairments in autism: social orienting, joint attention, and attention to distress. Dev Psychol. 2004;40:271–283. [DOI] [PubMed] [Google Scholar]
- 57. Ingersoll B. Brief report: Pilot randomized controlled trial of reciprocal imitation training for teaching elicited and spontaneous imitation to children with autism. J Autism Dev Disord. 2010;40:1154–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Walton KM, Ingersoll BR. Evaluation of a sibling-mediated imitation intervention for young children with autism. J Posit Behav Interv. 2012;14:241–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bellini S, Akullian J. A meta-analysis of video modeling and video self-modeling interventions for children and adolescents with autism spectrum disorders. Exceptional Children. 2007;73:264–287. [Google Scholar]
- 60. Charlop-Christy MH, Daneshvar S. Using video modeling to teach perspective taking to children with autism. J Posit Behav Interv. 2003;5:12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kaley-Isley LC, Peterson J, Fischer C, Peterson E. Yoga as a complementary therapy for children and adolescents: A guide for clinicians. Psychiatry (Edgemont). 2010;7:20–32. [PMC free article] [PubMed] [Google Scholar]


