Abstract
Background:
The evidence to support operative versus non-operative treatment for rotator cuff tears is sparse and inconclusive.
Hypothesis/Purpose:
We assessed pain and functional outcomes in patients undergoing operative versus non-operative treatments for rotator cuff tears.
Study Design:
From 03/2011 to 02/2015, a multi-center cohort of patients with rotator cuff tears undergoing operative and non-operative treatments was recruited.
Methods:
Patients completed a detailed history questionnaire, the Shoulder Pain and Disability Index (SPADI), the American Shoulder and Elbow Surgeons Standardized Form (ASES), and underwent a MRI. In addition to baseline assessments, patients received follow-up questionnaires at 3, 6, 12, and 18 months. Propensity score weighting was used to balance differences in characteristics of operative and non-operative groups.
Results:
Adjusted for propensity score, operative (n=50) and non-operative (n=77) groups had similar characteristics as evidence by small Standardized Mean Differences (SMD) between the groups. Adjusted mean differences in SPADI and ASES scores between the operative and non-operative groups were −22 points (95% CI=−32.1, −11.8) and −22.2 points (95% CI=−32.8, −11.6) at 18 months, respectively. Surgery group had a significantly higher proportion of patients who showed ≥30% (p=0.002) and ≥50% (p<0.0001) improvement in SPADI and ASES scores as compared with non-operative treatment.
Conclusions:
In our prospective cohort study, surgery had significantly better pain and functional outcomes as compared with non-operative treatment for rotator cuff tears. Differences between the two groups in SPADI and ASES scores at the 6–18 month time points met the MCID thresholds. A large randomized controlled trial is needed to answer this question more definitively.
Clinical Relevance:
We present data on operative versus non-operative treatments for rotator cuff tears that can be used in clinical practice by clinicians and patients.
Keywords: rotator cuff tears, arthroscopy, non-operative
Study Design
Level of Evidence: Level IIc (Outcomes Research)
INTRODUCTION
Shoulder pain accounted for 12.6 million ambulatory care visits to physician offices in 2015 in the United States4. Rotator cuff tears are one of the leading causes of shoulder pain and disability and accounted for 272,148 surgeries in 200612, 24. Non-operative treatment and surgery are offered to patients with rotator cuff tears with good outcomes4, 5, 8, 15, 16, 20, 27, 48. However, the evidence-base to support surgical versus non-surgical treatment is quite small and conflicting28, 29, 32, 38, 39. This paucity of evidence is highlighted in the 2012 American Academy of Orthopedic Surgeons (AAOS) Clinical Practice Guidelines43, Cochrane reviews11, 17, a report by the Agency for Healthcare Research and Quality1, and expert reviews2, 9, 35, 36, 41, 47, 53.
In a cohort of patients with rotator cuff tears followed longitudinally, we assessed comparative effectiveness of operative versus non-operative treatment as measured by shoulder pain and function.
MATERIALS AND METHODS
Patient Population
We recruited a cohort of patients with symptomatic rotator cuff tears in a multi-center longitudinal study termed as Rotator Cuff Outcomes Workgroup (ROW). Patients aged 45 and older were recruited from sports/shoulder clinics in 3 academic and 1 community settings between 03/2011 and 02/2015. Exclusion criteria were a current shoulder fracture, prior shoulder surgery (on the index shoulder), and active cervical radiculopathy (elicited as neck pain radiating to the shoulder/arm/hand). Additional details about this cohort has been provided previously21, 22. Patients provided informed consent and the study was approved by our Institutional Review Boards. Patients who met eligibility criteria, completed a baseline assessment, and were recommended either operative or non-operative treatment for rotator cuff tear without crossing over from non-operative treatment to surgery (n=7) were included in this analysis (n=127).
Structured History Questionnaire and Outcome Measures
Patients were asked to complete a structured shoulder and general health questionnaire at enrollment. An abbreviated version of this questionnaire was mailed to patients around each of the follow-up time points. Patients were asked about their demographics, comorbidities, symptoms, smoking/alcohol habits, and patient expectations from treatment in the questionnaires. Patients were asked about manual labor at their current job to get information on daily use of shoulder at work. If patients were not working, they were instructed to provide information on manual labor at their last job. Patients completed the Fear-Avoidance Beliefs questionnaire (FABQ) which was designed by Waddell et al.50 to assess fear-avoidance beliefs about physical activity and work in patients with low back pain. The FABQ physical activity questionnaire (4 items that contribute towards scoring) was slightly modified for our study to say “shoulder” instead of “back” for our study. The scale has 24 possible points with a higher score indicating worse fear-avoidance behavior. The Mental Health Inventory (MHI-5)7, a component of the 36-item Short Form Health Survey51 was used to get information on mental health. MHI-5 scores range from 0 to 100. A score of ≤68 on the MHI-5 is indicative of a probable mood disorder (including depression)26, 49.
Shoulder pain and function were measured using the Shoulder Pain and Disability Index (SPADI)45, a standardized 13-item questionnaire, and the American Shoulder and Elbow Surgeons Standardized Shoulder Form (ASES)44, an 11-item questionnaire with minor modifications as described elsewhere40. Score ranges for ASES and SPADI are from 0 to 100, with higher scores reflecting worse pain and function.
Strength Testing
Strength testing was performed using a hand-held dynamometer in abduction, external rotation, and internal rotation by trained research assistants. Our detailed protocol for standardized strength testing has been previously described25, 37. Strength testing using a dynamometer has good intra-rater and inter-rater reliability19. We used a ratio of the affected shoulder versus the contralateral shoulder strength in the analysis. There were 2 patients with a strength ratio above 3. These patients were given a value of 3 for the strength ratio to avoid outlying values in the analysis.
Diagnostic Imaging
Shoulder MRI images were read in a blinded fashion by consensus by two shoulder experts. Our detailed protocol for imaging review and good inter-rater and intra-rater reliability for these MRI readings as compared with a reading by a musculoskeletal radiologist has been previously described23. Kappa values ranged from 0.75 to 0.90 for tear presence, tear size, and tear thickness23.
Diagnosis of Rotator Cuff Tear
Our algorithm for diagnosis of rotator cuff tear has been previously described21, 22. A diagnosis of rotator cuff tear was made based on the clinical impression of a sports/shoulder fellowship trained attending physician and evidence of structural deficit on a MRI (when available). If MRI was unavailable (since it was not clinically indicated; n=17), the diagnosis was based on the clinician’s impression. It is important to include patients without MRI in the analysis to avoid a spectrum bias in patients undergoing non-operative treatment who in many cases do not need imaging unless surgery is indicated.
The diagnosis of biceps tendon pathology was based on the physician indicating that the patient had clinical signs and symptoms corresponding to biceps disease (a “yes/no” question).
Non-Operative Treatment and Surgery
Patients pursued either non-operative treatment including physical therapy or rotator cuff surgery after their baseline visit. Treatment decisions were made based on shared decision-making between the physician and the patient. Physical therapy included rotator cuff strengthening, scapular stabilization exercises, and capsular stretching. Surgery was performed by one of the study surgeons and patients underwent post-operative rehabilitation after surgery. Patients were typically in a sling for about 3–6 weeks after surgery. Patients could receive additional interventions such as injections and medications as medically indicated in either arm. There were 11 patients who were recommended surgery but did not have surgery. These patients were included in the non-operative arm of our cohort study.
Longitudinal Follow-Up
Patients were followed at approximately 3, 6, 12, and 18 months after completion of baseline visit. Follow-up was performed via mail and patients received phone or email reminders if they did not return the questionnaires.
Statistical Analysis
Data for this study was entered twice to minimize inaccuracies during data entry. If there was a discrepancy between the two datasets, source documentation was reviewed to resolve them. Baseline SPADI score and 23 individual and composite variables that are related to both the treatment assignment and outcome are included in current analysis. Multiple imputation (MI) with predictive mean matching method was used to impute missing data among all 24 variables. Restricted cubic splines were applied to all continuous variables. Twenty separate datasets were constructed to account for added variability introduced by imputation. A propensity score was estimated for each patient in each imputation data set as the probability of surgery using a multivariable logistic regression3. The final propensity score for each patient was the average of 20 propensity scores calculated from imputed complete datasets. Matching weights were calculated for both surgery and non-operative groups14, 33. The standardized mean difference (SMD) was calculated to estimate the improved balance among covariates achieved by propensity score weight matching. SPADI and ASES scores were measured at baseline, 3, 6, 12, and 18 months post enrollment. Our primary model(s) of SPADI and ASES included treatment, time (modelled as indicator variables), and time by treatment interaction using 11 degrees of freedom. In addition to the fixed effects mentioned above, individual participant ID was included as the random effect and inverse probability weighting (IPW) was used to adjust estimates for the propensity of treatment group membership. Compound symmetry was chosen to model the variance covariance matrix based on AIC criteria relative to auto-regressive and unstructured The primary model, adjusting for propensity score, allows us to estimate the average treatment effect (ATE) at the population level, a measure achieved directly by a randomized study design. Supporting linear mixed effects models were fitted to study differential effects on SPADI and ASES scores over time for smoking, age, alcohol use, baseline SPADI (or ASES), external rotation strength ratio, daily shoulder use at work, trauma, fatty infiltration, number of tendons torn, MHI-5, patient expectations, tear thickness, and treatment (operative versus non-operative). Two-sided alpha level at 0.05 was set as significance level. Statistical analysis was performed using the computing environment R.
RESULTS
There were 77 patients who underwent non-operative treatment and 50 patients who had operative treatment in our cohort. Adjusted for propensity score, operative and non-operative groups had similar characteristics as evidenced by the small Standardized Mean Differences (SMD) between the two groups (Table 1).
Table 1:
Baseline Characteristics** of Patients Undergoing Operative and Non-Operative Treatment for Rotator Cuff Tears Before and After Propensity Score Weighting: The ROW Cohort
| BEFORE WEIGHTING | AFTER WEIGHTING | |||||
|---|---|---|---|---|---|---|
| SURGERY (n=50) | NON-OPERATIVE (n=77) | SMD | SURGERY (n=50) | NON-OPERATIVE (n=77) | SMD | |
| DEMOGRAPHICS | ||||||
| SEX | 0.257 | 0.017 | ||||
| Female | 38.0% | 50.6% | 45.6% | 44.7% | ||
| Male | 62.0% | 49.4% | 54.4% | 55.3% | ||
| AGE (YEARS)* | 59.3±8.9 | 63.8±8.3 | 0.534 | 61.5±8.3 | 61.1±8.5 | 0.038 |
| HIGHEST LEVEL OF EDUCATION | 0.019 | 0.101 | ||||
| Less than college | 33.3% | 34.2% | 31.6% | 36.4% | ||
| College or above | 66.7% | 65.8% | 68.4% | 63.6% | ||
| MARITAL STATUS | 0.139 | 0.032 | ||||
| Single/Divorced/Widowed | 22.0% | 28.0% | 27.5% | 26.1% | ||
| Married | 78.0% | 72.0% | 72.5% | 73.9% | ||
| SHOULDER SYMPTOMS AND STRENGTH | ||||||
| SYMPTOM DURATION (MONTHS)* | 22.6±40.6 | 23.9±54.3 | 0.048 | 25.3±46.3 | 27.2±57.7 | 0.035 |
| DOMINANT SHOULDER AFFECTED | 0.041 | 0.023 | ||||
| No | 22.9% | 24.7% | 29.0% | 30.1% | ||
| Yes | 77.1% | 75.3% | 71.0% | 69.9% | ||
| DAILY SHOULDER USE AT WORK | 0.154 | 0.008 | ||||
| Light/No manual labor | 75.5% | 81.8% | 79.9% | 79.6% | ||
| Heavy/Moderate manual labor | 24.5% | 18.2% | 20.1% | 20.4% | ||
| TRAUMATIC TEAR | 0.266 | 0.055 | ||||
| No | 46.0% | 59.2% | 47.9% | 45.2% | ||
| Yes | 54.0% | 40.8% | 52.1% | 54.8% | ||
| SPADI SCORE AT BASELINE* | 55.0±20.5 | 44.2±23.1 | 0.493 | 49.1±20.7 | 49.6±21.6 | 0.025 |
| EXTERNAL ROTATION STRENGTH RATIO*¶ | 0.5±0.3 | 0.8±0.5 | 0.768 | 0.7±0.3 | 0.7±0.3 | 0.105 |
| ISOLATED ABDUCTION STRENGTH RATIO*¶ | 0.9±0.2 | 0.9±0.2 | 0.110 | 0.9±0.2 | 0.9±0.2 | 0.041 |
| COMORBIDITIES AND SOCIAL HISTORY | ||||||
| NUMBER OF COMORBIDITIES | 0.280 | 0.048 | ||||
| ≤1 | 58.0% | 44.2% | 48.9% | 51.3% | ||
| >1 | 42.0% | 55.8% | 51.1% | 48.7% | ||
| SMOKING STATUS | 0.026 | 0.002 | ||||
| Never | 50.0% | 48.7% | 47.2% | 47.3% | ||
| Past/Current | 50.0% | 51.3% | 52.8% | 52.7% | ||
| ALCOHOL USE | 0.389 | 0.015 | ||||
| 2–3 times per month or less | 37.5% | 56.6% | 50.8% | 51.6% | ||
| 1–2 times per week or more | 62.5% | 43.4% | 49.2% | 48.4% | ||
| FEAR AVOIDANCE AND BEHAVIOR (FABQ) PHYSICAL ACTIVITY SCORE | 19.0±4.3 | 16.4±6.1 | 0.495 | 17.9±4.8 | 17.6±4.8 | 0.050 |
| MENTAL HEALTH INVENTORY (MHI-5) SCORE | 80.5±16.9 | 80.3±14.9 | 0.013 | 82.1±14.8 | 81.6±16.0 | 0.035 |
| PATIENT EXPECTATIONS AFTER TREATMENT | 0.762 | 0.067 | ||||
| A great improvement | 94.0% | 65.3% | 87.4% | 85.2% | ||
| Moderate/Little/No improvement or worse | 6.0% | 34.7% | 12.6% | 14.8% | ||
| BICEPS TENDONITIS/TENOSYNOVITIS | 0.003 | 0.060 | ||||
| No | 70.0% | 70.1% | 72.1% | 74.7% | ||
| Yes | 30.0% | 29.9% | 27.9% | 25.3% | ||
| TEAR CHARACTERISTICS ON MRI∞ | ||||||
| CROSS-SECTIONAL AREA OF TEAR*# | 14.5±19.3 | 7.9±15.3 | 0.376 | 16.3±22.5 | 17.2±21.7 | 0.039 |
| THICKNESS OF TEAR∏ | 0.841 | 0.005 | ||||
| Partial-thickness | 10.4% | 45.2% | 15.2% | 15.4% | ||
| Full-thickness | 89.6% | 54.8% | 84.8% | 84.6% | ||
| PRESENCE OF FATTY INFILTRATION± | 0.362 | 0.147 | ||||
| No | 54.8% | 71.9% | 51.6% | 58.9% | ||
| Yes | 45.2% | 28.1% | 48.4% | 41.1% | ||
| NUMBER OF TORN TENDONS | 0.224 | 0.083 | ||||
| 1 | 60.4% | 71.0% | 53.0% | 57.1% | s | |
| 2 or 3 | 39.6% | 29% | 47.0% | 42.9% | ||
| TENDON RETRACTION | 0.414 | 0.032 | ||||
| Stage I or not applicable¶ | 60.4% | 79.0% | 60.5% | 58.9% | ||
| Stage II or more | 39.6% | 21.0% | 39.5% | 41.1% | ||
SMD=Standardized Mean Difference
n for missing before imputation: Daily shoulder use at work=1; Alcohol use=3; Education level=3; Smoking status=3; Traumatic tear=6; Patient expectations=2; Duration of symptoms=5; Dominant shoulder affected=6; Marital status=2; External rotation strength ratio=8; Isolated abduction strength ratio=10; MHI-5=2; FABQ=5; SPADI score at baseline=7; cross-sectional are of tear=27
X ± Standard Deviation for continuous variables
After multiple imputation for missing values
Strength ratio is measured as affected shoulder versus unaffected shoulder
MRI information available for 110 patients; fatty infiltration and muscle atrophy were determined from CT scan in 2 patients a CT scan who were included in the analysis but not in the table above
Tear size determined by sum of supraspinatus and infraspinatus tears in longitudinal or transverse planes for full-thickness tears only
If any of the tendons had a full-thickness tear, the tear was classified as full-thickness
Fatty infiltration reported for muscle most severely affected
Since tear was partial-thickness
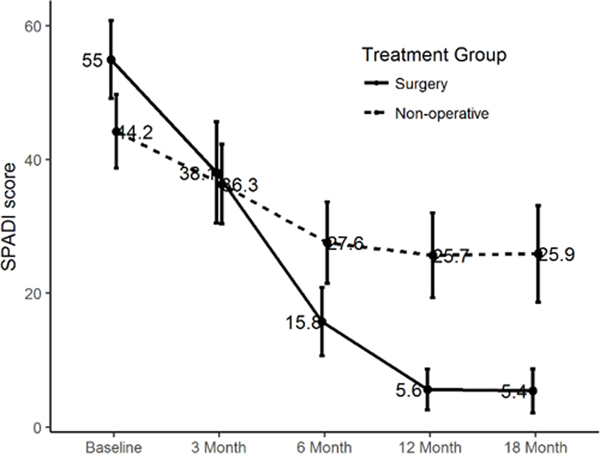
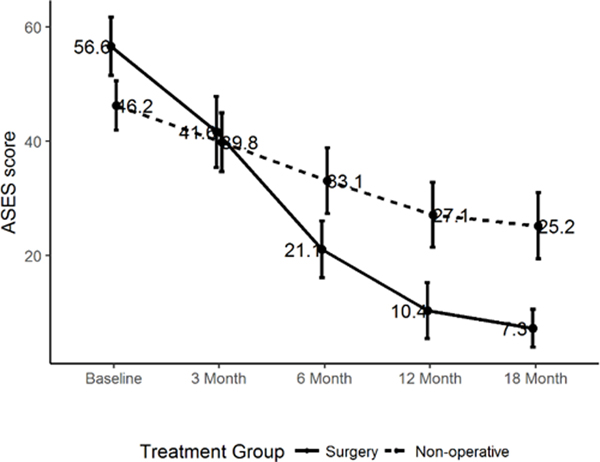
The observed SPADI (5.6; 95%CI=2.6, 8.7 for surgery and 25.7; 95%CI=19.4, 32.0 for non-operative; Figure 1a), and ASES (10.4; s95%CI=5.5, 15.2 for surgery and 27.1; 95%CI=21.4, 32.8 for non-operative; Figure 1b) scores plateaued by 12 months of follow-up in our cohort.
Figure 1a:
Observed SPADI Scores with 95% Confidence Intervals of Operative and Non-Operative Treatments over 18 Months of Follow-Up
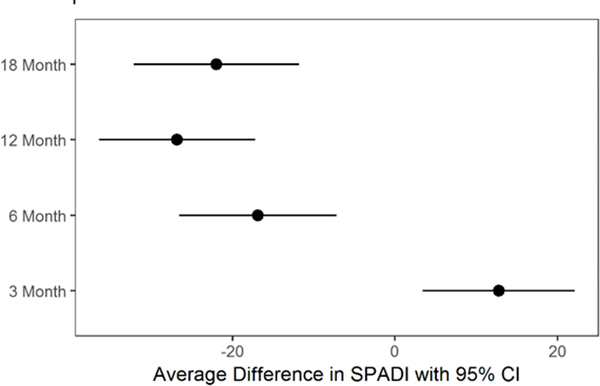
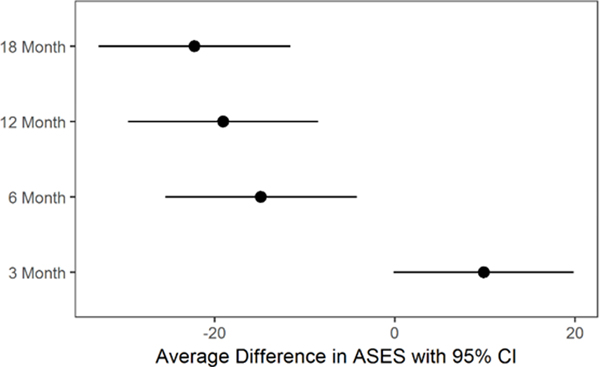
Adjusted for propensity score, the estimated difference in SPADI score between the operative and non-operative groups was −22 points (95% CI=−32.1, −11.8;; Table 2a and Figure 2a) at 18 months. Similarly, the estimated adjusted difference in ASES score between the operative and non-operative groups was −22.2 points (95% CI=−32.8, −11.6; Table 2b and Figure 2b) at 18 months. In a sensitivity analysis adjusting for smoking, age, alcohol use, baseline SPADI (or ASES), external rotation strength ratio, daily shoulder use at work, trauma, fatty infiltration, number of tendons torn, MHI-5, patient expectations, and thickness of tear, receiving operative treatment versus non-operative treatment showed a differential effect over time, with visits at 6, 12, and 18 months for the operative group having lower SPADI and ASES scores than 3 months visit (p<0.01).
Table 2a:
Predicted and Propensity Score Adjusted Differences in SPADI Score between Operative and Non-Operative Treatments at Follow-Up Time Points
| Follow-Up Time Point | Estimated Difference in SPADI Score (95% Confidence Intervals) |
|---|---|
| 3 Month | 13 (3.4, 22.1) |
| 6 Month | −17 (−26.6, −7.2) |
| 12 Month | −27 (−36.4, −17.2) |
| 18 Month | −22 (−32.1, −11.8) |
SPADI=Shoulder Pain and Disability Index
Figure 1b:
Observed ASES Scores with 95% Confidence Intervals of Operative and Non-Operative Treatments over 18 Months of Follow-Up
Table 2b:
Predicted and Propensity Score Adjusted Differences in ASES Score between Operative and Non-Operative Treatments at Follow-Up Time Points
| Follow-Up Time Point | Estimated Difference in ASES Score (95% Confidence Intervals) |
|---|---|
| 3 Month | 9.9 (−0.1, 19.9) |
| 6 Month | −14.8 (−25.5, −4.2) |
| 12 Month | −19.0 (−29.6, −8.5) |
| 18 Month | −22.2 (−32.8, −11.6) |
ASES=American Shoulder and Elbow Surgeons
In an analysis of ≥30% improvement from baseline in SPADI and ASES scores, a significantly higher proportion of patients undergoing surgery improved versus non-operative treatment (90% versus 57%; p=0.002 for SPADI, and 88% versus 61%; p=0.002 for ASES; Tables 3a and 3b). Similarly, when a ≥50% improvement from baseline threshold in SPADI and ASES scores was used, a significantly higher proportion of patients undergoing surgery improved versus non-operative treatment (86% versus 44%; p<0.0001 for SPADI, and 84% versus 45%; p<0.0001 for ASES; Tables 3a and 3b).
Table 3a:
Percent Improvement in SPADI Score between Operative and Non-Operative Treatments During 18 Months of Follow-Up. n for missing for SPADI=7 (9%) for non-operative
| IMPROVEMENT IN SPADI SCORE FROM BASELINE | SURGERY n (%) | NON-OPERATIVE n (%) | p-Value (Surgery versus Non-Operative) |
|---|---|---|---|
| <30% | 5 (10%) | 26 (34%) | 0.002 |
| ≥30% | 45 (90%) | 44 (57%) |
| IMPROVEMENT IN SPADI SCORE FROM BASELINE | SURGERY n (%) | NON-OPERATIVE n (%) | p-Value (Surgery versus Non-Operative) |
|---|---|---|---|
| <50% | 7 (14%) | 36 (47%) | <0.0001 |
| ≥50% | 43 (86%) | 34 (44%) |
n for missing for SPADI=7 (9%) for non-operative
Table 3b:
Percent Improvement in ASES Score between Operative and Non-Operative Treatments During 18 Months of Follow-Up. n for missing for ASES=1 (2%) for surgery and 3 (4%) for non-operative
| IMPROVEMENT IN ASES SCORE FROM BASELINE | SURGERY n (%) | NON-OPERATIVE n (%) | p-Value (Surgery versus Non-Operative) |
|---|---|---|---|
| <30% | 5 (10%) | 27 (35%) | 0.002 |
| ≥30% | 44 (88%) | 47 (61%) |
| IMPROVEMENT IN ASES SCORE FROM BASELINE | SURGERY n (%) | NON-OPERATIVE n (%) | p-Value (Surgery versus Non-Operative) |
|---|---|---|---|
| <50% | 7 (14%) | 39 (51%) | <0.0001 |
| ≥50% | 42 (84%) | 35 (45%) |
n for missing for ASES=1 (2%) for surgery and 3 (4%) for non-operative
DISCUSSION
We assessed comparative-effectiveness of operative versus non-operative treatment for rotator cuff tears in a well-characterized cohort of patients recruited from academic and community settings. Our results show that over an 18-month follow-up period, patients undergoing surgery had significantly improved pain and functional outcomes as measured by SPADI and ASES as compared with those receiving non-operative treatment. The difference between the groups is sustained over the duration of the study after the first 3 months. When assessed as a 30% or 50% change in SPADI or ASES scores from baseline, patients undergoing surgery had a significantly higher proportion of patients meeting these outcomes improvement benchmarks.
Our study was designed to be a cohort study. Given the non-randomized nature of a cohort study, it has inherent indication bias in patients that receive operative versus non-operative treatment30. We used propensity score methodology as has been previously described18, 30 to control for confounding by indication. This method accounts for differences in the likelihood of patients with certain characteristics to receive surgery versus non-operative treatment, and weights each patient in the cohort to balance the two groups. The gold standard study design for minimizing bias is a randomized controlled trial. Thus, even though we have used advanced methodology in this comparative-effectiveness study to adjust for indication bias, our results should be interpreted with caution.
There is substantial literature on pain and functional improvements after operative and non-operative treatment4–6, 10, 15, 16, 20, 27, 34, 42, 48. Surgical studies generally report favorable outcomes but do not have a comparison non-operative group4–6, 10, 15, 16, 20, 27, 34, 42, 48. Similarly, studies on non-operative treatments show improved symptoms and function over 12–24 weeks but do not have a surgical comparison group. There are three published small randomized trials on operative versus non-operative treatments for rotator cuff tears28, 32, 38. Moosmayer et al.38 had clinically relevant study entry criteria such as exclusion of subscapularis tendon tears and prior shoulder tendon surgery, and inclusion of only full-thickness tears. The trial showed a statistically significant improvement in the surgery versus the non-operative group as measured by the shoulder Constant score13 (13 point difference) and the visual analogue pain scale (1.7 cm difference). Recently, results from two and five year follow-up of this cohort were presented39. The difference in Constant scores between the surgery and non-operative groups in an intention to treat analysis was 2.6 (95% confidence intervals=−3.1, 8.3) at 2 years and 5.3 points (95% confidence intervals=−0.05, 10.7) at 5 years of follow-up. Thus, differences between the two groups were not statistically significant. Kukkonen et al.28 randomized 173 patients with supraspinatus tears into three groups: physiotherapy; physiotherapy and acromioplasty, and; rotator cuff repair, acromioplasty, and physiotherapy. They reported no statistically significant differences in Constant scores at 12 months of follow-up across the three groups. After two years of follow-up, results again, showed no difference in clinical outcome between the three groups29. Lambers Heerspink et al.32 randomized 56 patients with degenerative full-thickness tears and at 12 months of follow-up reported no significant difference in Constant-Murley score between the surgery group and conservative care group. Although differences in VAS pain and disability scores between the two groups were statistically significant, these differences were small and unlikely to meet clinical significance. In our study, surgery had significantly superior outcomes as compared with non-operative treatment at all follow-up time points except for 3 months. At the 3 month time point patients who had surgery are still recovering from the operation, and hence it is not surprising that they have not improved. The differences in SPADI scores at time points from 6–18 months between the operative and non-operative groups were greater than the reported Minimal Clinically Important Difference (MCID) of 8–13.2 points for SPADI31, 46, 54. ASES has a MCID of 6.2–13.9 points52, and differences between the two groups also cross this threshold between 6–18 months.
Limitations of our study include a relatively small sample size, missing MRI information in 17 patients, and unavailability of complete data at all of the outcome time points. We were also limited by a cohort study design as opposed to a randomized controlled trial.
In our prospective cohort study, surgery had significantly better pain and functional outcomes as compared with non-operative treatment for rotator cuff tears. Differences between the two groups in SPADI and ASES scores at the 6–18 month time points met the MCID thresholds. Thus, pain and functional differences observed between the two groups in our study meet statistical significance and are clinically meaningful. An analysis with 30% and 50% improvement in SPADI and ASES scores from baseline also yielded similar results with surgery significantly superior to non-operative treatment. Although we present data from a well-designed cohort study and use advanced methodology, a large randomized controlled trial is needed to answer this question more definitively.
Supplementary Material
Figure 2a:
Predicted mean differences with 95% confidence intervals in SPADI Scores between Operative and Non-Operative Treatments over 18 Months of Follow-Up
Figure 2b:
Predicted mean differences with 95% confidence intervals in ASES Scores between Operative and Non-Operative Treatments over 18 Months of Follow-Up
What is known about the subject
Rotator cuff tears are the most common cause of shoulder pain and treated operatively or non-operatively
Operative and non-operative treatments have good outcomes
What this study adds to existing knowledge:
We provide data on comparative-effectiveness of operative versus non-operative treatments for rotator cuff tears in a well-designed cohort study
Acknowledgements:
We thank the entire ROW team for their efforts. We also thank our clinical staff at the Orthopedic and Arthritis Center at Brigham and Women’s Hospital, Shoulder Service at Massachusetts General Hospital, and clinical staff at Vanderbilt Orthopaedic Institute for their efforts and cooperation.
Footnotes
Investigation performed at: Vanderbilt University Medical Center
References
- 1.Agency for Healthcare Research and Quality (AHRQ). Comparative effectiveness of non-operative and operative treatments for rotator cuff tears. Effective Health Care: AHRQ; 2008. [PubMed] [Google Scholar]
- 2.Ainsworth R, Lewis JS. Exercise therapy for the conservative management of full thickness tears of the rotator cuff: a systematic review. Br J Sports Med. 2007;41(4):200–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res. 2011;46(3):399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartolozzi A, Andreychik D, Ahmad S. Determinants of outcome in the treatment of rotator cuff disease. Clin Orthop Relat Res. 1994(308):90–97. [PubMed] [Google Scholar]
- 5.Baysal D, Balyk R, Otto D, Luciak-Corea C, Beaupre L. Functional outcome and health-related quality of life after surgical repair of full-thickness rotator cuff tear using a mini-open technique. Am J Sports Med. 2005;33(9):1346–1355. [DOI] [PubMed] [Google Scholar]
- 6.Bennett WF. Arthroscopic repair of massive rotator cuff tears: a prospective cohort with 2- to 4-year follow-up. Arthroscopy. 2003;19(4):380–390. [DOI] [PubMed] [Google Scholar]
- 7.Berwick DM, Murphy JM, Goldman PA, Ware JE Jr.,, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29(2):169–176. [DOI] [PubMed] [Google Scholar]
- 8.Bokor DJ, Hawkins RJ, Huckell GH, Angelo RL, Schickendantz MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res. 1993(294):103–110. [PubMed] [Google Scholar]
- 9.Clement ND, Nie YX, McBirnie JM. Management of degenerative rotator cuff tears: a review and treatment strategy. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Joint Surg Am. 2001;83-A(1):71–77. [DOI] [PubMed] [Google Scholar]
- 11.Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN. Surgery for rotator cuff disease. Cochrane Database Syst Rev. 2008(1):CD005619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94(3):227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987(214):160–164. [PubMed] [Google Scholar]
- 14.Dunn WR, Kuhn JE, Sanders R, et al. Symptoms of pain do not correlate with rotator cuff tear severity: a cross-sectional study of 393 patients with a symptomatic atraumatic full-thickness rotator cuff tear. J Bone Joint Surg Am. 2014;96(10):793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A(2):219–224. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg BA, Nowinski RJ, Matsen FA 3rd., Outcome of nonoperative management of full-thickness rotator cuff tears. Clin Orthop Relat Res. 2001(382):99–107. [DOI] [PubMed] [Google Scholar]
- 17.Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003(2):CD004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haukoos JS, Lewis RJ. The Propensity Score. JAMA. 2015;314(15):1637–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hayes K, Walton JR, Szomor ZL, Murrell GA. Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg. 2002;11(1):33–39. [DOI] [PubMed] [Google Scholar]
- 20.Itoi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop Relat Res. 1992(275):165–173. [PubMed] [Google Scholar]
- 21.Jain NB, Ayers GD, Fan R, et al. Predictors of Pain and Functional Outcomes After the Nonoperative Treatment of Rotator Cuff Tears. Orthop J Sports Med. 2018;6(8):2325967118788531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jain NB, Ayers GD, Fan R, et al. Predictors of pain and functional outcomes after operative treatment for rotator cuff tears. J Shoulder Elbow Surg. 2018;27(8):1393–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jain NB, Collins J, Newman JS, Katz JN, Losina E, Higgins LD. Reliability of Magnetic Resonance Imaging Assessment of Rotator Cuff: The ROW Study. PM R. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jain NB, Higgins LD, Losina E, Collins J, Blazar PE, Katz JN. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord. 2014;15(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jain NB, Wilcox RB 3rd,, Katz JN, Higgins LD. Clinical examination of the rotator cuff. PM R. 2013;5(1):45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly MJ, Dunstan FD, Lloyd K, Fone DL. Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: a comparison of five different methods. BMC Psychiatry. 2008;8:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuhn JE, Dunn WR, Sanders R, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013;22(10):1371–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kukkonen J, Joukainen A, Lehtinen J, et al. Treatment of non-traumatic rotator cuff tears: A randomised controlled trial with one-year clinical results. Bone Joint J. 2014;96-B(1):75–81. [DOI] [PubMed] [Google Scholar]
- 29.Kukkonen J, Joukainen A, Lehtinen J, et al. Treatment of Nontraumatic Rotator Cuff Tears: A Randomized Controlled Trial with Two Years of Clinical and Imaging Follow-up. J Bone Joint Surg Am. 2015;97(21):1729–1737. [DOI] [PubMed] [Google Scholar]
- 30.Kyriacou DN, Lewis RJ. Confounding by Indication in Clinical Research. JAMA. 2016;316(17):1818–1819. [DOI] [PubMed] [Google Scholar]
- 31.L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am. 1997;79(5):738–748. [PubMed] [Google Scholar]
- 32.Lambers Heerspink FO, van Raay JJ, Koorevaar RC, et al. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elbow Surg. 2015;24(8):1274–1281. [DOI] [PubMed] [Google Scholar]
- 33.Li L, Greene T. A weighting analogue to pair matching in propensity score analysis. Int J Biostat. 2013;9(2):215–234. [DOI] [PubMed] [Google Scholar]
- 34.MacDonald P, McRae S, Leiter J, Mascarenhas R, Lapner P. Arthroscopic rotator cuff repair with and without acromioplasty in the treatment of full-thickness rotator cuff tears: a multicenter, randomized controlled trial. J Bone Joint Surg Am. 2011;93(21):1953–1960. [DOI] [PubMed] [Google Scholar]
- 35.Marx RG, Koulouvaris P, Chu SK, Levy BA. Indications for surgery in clinical outcome studies of rotator cuff repair. Clin Orthop Relat Res. 2009;467(2):450–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matsen FA 3rd., Clinical practice. Rotator-cuff failure. N Engl J Med. 2008;358(20):2138–2147.18480206 [Google Scholar]
- 37.Miller JE, Higgins LD, Dong Y, et al. Association of Strength Measurement with Rotator Cuff Tear in Patients with Shoulder Pain: The Rotator Cuff Outcomes Workgroup Study. Am J Phys Med Rehabil. 2016;95(1):47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moosmayer S, Lund G, Seljom U, et al. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: A randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br. 2010;92(1):83–91. [DOI] [PubMed] [Google Scholar]
- 39.Moosmayer S, Lund G, Seljom US, et al. Tendon Repair Compared with Physiotherapy in the Treatment of Rotator Cuff Tears: A Randomized Controlled Study in 103 Cases with a Five-Year Follow-up. J Bone Joint Surg Am. 2014;96(18):1504–1514. [DOI] [PubMed] [Google Scholar]
- 40.Nho SJ, Brown BS, Lyman S, Adler RS, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg. 2009;18(1):13–20. [DOI] [PubMed] [Google Scholar]
- 41.Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res. 2007;455:52–63. [DOI] [PubMed] [Google Scholar]
- 42.Park JY, Chung KT, Yoo MJ. A serial comparison of arthroscopic repairs for partial- and full-thickness rotator cuff tears. Arthroscopy. 2004;20(7):705–711. [DOI] [PubMed] [Google Scholar]
- 43.Pedowitz RA, Yamaguchi K, Ahmad CS, et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on: optimizing the management of rotator cuff problems. J Bone Joint Surg Am. 2012;94(2):163–167. [PubMed] [Google Scholar]
- 44.Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347–352. [DOI] [PubMed] [Google Scholar]
- 45.Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res. 1991;4(4):143–149. [PubMed] [Google Scholar]
- 46.Schmitt JS, Di Fabio RP. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J Clin Epidemiol. 2004;57(10):1008–1018. [DOI] [PubMed] [Google Scholar]
- 47.Seida JC, LeBlanc C, Schouten JR, et al. Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med. 2010;153(4):246–255. [DOI] [PubMed] [Google Scholar]
- 48.Tashjian RZ, Henn RF, Kang L, Green A. Effect of medical comorbidity on self-assessed pain, function, and general health status after rotator cuff repair. J Bone Joint Surg Am. 2006;88(3):536–540. [DOI] [PubMed] [Google Scholar]
- 49.Thorsen SV, Rugulies R, Hjarsbech PU, Bjorner JB. The predictive value of mental health for long-term sickness absence: the Major Depression Inventory (MDI) and the Mental Health Inventory (MHI-5) compared. BMC Med Res Methodol. 2013;13:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. [DOI] [PubMed] [Google Scholar]
- 51.Ware JE Jr.,, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 52.Werner BC, Chang B, Nguyen JT, Dines DM, Gulotta LV. What Change in American Shoulder and Elbow Surgeons Score Represents a Clinically Important Change After Shoulder Arthroplasty? Clin Orthop Relat Res. 2016;474(12):2672–2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Williams GR Jr.,, Rockwood CA Jr., Bigliani LU, Iannotti JP, Stanwood W. Rotator cuff tears: why do we repair them? J Bone Joint Surg Am. 2004;86-A(12):2764–2776. [PubMed] [Google Scholar]
- 54.Williams JW Jr.,, Holleman DR Jr.,, Simel DL. Measuring shoulder function with the Shoulder Pain and Disability Index. J Rheumatol. 1995;22(4):727–732. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.