Abstract
INTRODUCTION:
Majority of critical care nurses do not have desirable skills in performing endotracheal tube suctioning (ETS) despite related training taught in the curricula. This study aimed to investigate and compare the effect of education through video and performance feedback (PF) on nurses' skills in performing ETS.
METHODS:
This was a quasi-experimental study. The sample size comprised of all nurses (n = 49) working in the intensive care unit of one of the educational hospital located in one of the western cities of Iran. Nurses were assigned to either one of educational video (EV) and PF groups. Data were collected using a 25-item structured best practices information sheet. Data were analyzed using SPSS software version 20 (SPSS Inc., Chicago, IL, USA).
RESULTS:
After the interventions, no significant difference was found in the total mean score of nurses' practice in ETS between those who received education through EV and those who received through PF (16.3 vs. 15.1) (P > 0.05). Before and after the intervention, a significant improvement was observed in the total mean score and other dimensions of nurses' practice in endotracheal suctioning (P < 0.0001).
CONCLUSIONS:
The results showed that both of methods through feedback and EV are useful in improving nurses' ETS practice. However, further studies are required to examine the effects of such interventions in the long term.
Keywords: Airway care, education, educational video, endotracheal tube suctioning, intensive care unit, nurse, performance feedback
Introduction
Endotracheal tube suctioning (ETS) is a common invasive procedure in hospitalized patients with artificial airway in the critical care unit (ICU), which is mainly performed by nurses.[1,2,3] According to the literature, patients undergoing artificial mechanical ventilation may require 3–4 times of ETS during 24 h.[1,4]
Although suctioning causes pulmonary secretions to remove easily and to keep the airway open, because of discontinuing oxygen intake during suctioning as well as increased oxygen consumption rate this method results in decreased tissue oxygenation and cardiac arrhythmia, tissue injury, laryngeal contraction and bronchitis.[5] Besides, patients may experience moderate to severe pain and may be at increased risk of respiratory infections.[6] It has been estimated that the mortality rate in patients' dependent on mechanical ventilation system following pneumonia is between 20% and 70%.[7] One of the main reasons for such respiratory infections is non-adherence of nurses to accurate principles in endotracheal suctioning.[4]
So, it is necessary for nurses to follow established ETS evidence-based recommendation to execute the suctioning procedure correctly in the ICU. However, unsafe ETS practice of nurses in ICUs is a worldwide problem. It has been shown that nurses do not have adequate knowledge of ETS-related guidelines and perform this procedure based on traditional/routine methods which mainly are not safe, according to some studies.[4,8,9] A study by Rezaee et al. in Iran showed that the quality of nurses' performance in ETS and tracheostomy tube in the ICU was weak in 19.2% cases, moderate in 65.4% cases, and good only in 15.4% cases, and none of them showed an excellent performance.[1] Frota et al. also reported that nurses working in ICU in 16 out of 23 items required for performing ETS had weak performance, and their efficiency in all items was only 51% and their quality of work was poor.[10] These findings indicates the gap exist between the the nurses knowledge and their common practice. Hence, there is need to calls for alternative learning strategies to be put in place for clinical training.
Clinical training is one of the most important component of professional nursing. Since the clinical environment is not predictable, it is deemed more important and sensitive compared with theoretical training.[11] Given traditional training strategies such as lecture have little impact on practice, other approaches, including training through feedback, should be utilized in clinical training.[12] The underlying element of clinical training is feedback. Feedback has been discussed in the writings of Greek physicians as one of the features of medical education. Feedback is a process aimed at making the learners aware of their performance.[13] In a clinical environment, the subjects being learned in theoretical classes are analyzed. The feedback outcome for learners is that enabling them to enhance their learning, recognize their learning errors and correct them. Training through providing feedback can be done in the form of individual or group through oral or written.[14] Kaphle et al. showed that providing performance feedback (PF) results in improving motivation and community health nurses' practice in providing patients counseling.[15]
Training through the multimedia method, particularly through educational video (EV) is a kind of informal training, in which educator does not attend class and is not in the form of face-to-face, but also can be in the form of individual and causes decreased costs. It became integrated as part of traditional and many blended courses and is often the main technique of information provision in online courses.[16,17] In this educational method, video and image relating to training title are provided in the form of the compact disk or web-based contents.[15] Some studies have taken into account the effect of using this method with that of the lecture method as equal. For example, Barzoki et al. compared the effect of education through lecture and multimedia methods on knowledge and performance of nurses working in the cardiac care unit in patients with a temporary pacemaker. They indicated that the score of knowledge and performance of nurses increased significantly in both lecture and multimedia methods after education, whereas there was not a significant difference between the two methods.[13] Yet, the lecture method has lower priority regarding clinical training.
Given the conducted literature review in national and international studies as well as the experience of the first author as a critical care nurse, nurses use lower standardized methods in performing ETS, which this issue encounters patients' health with serious risks, so it is necessary to make effective interventions to improve critical-care nurses' practice. Besides considering that most of the conducted studies on ETS in Iran have been carried out with a descriptive approach, or merely have been done to improve nurses' knowledge, studies regarding the effect of simulation and evidence-based methods on nurses' clinical practices are needed. Therefore, this study aimed to investigate the effect of two methods of PF and EV on critical-care nurses in performing ETS.
Methods
Study design
This was a quasi-experimental study.
Setting and study population
The study population involved all nurses working in two ICUs of one of Ilam's Educational Hospital in the west of Iran. All of nurses (n = 49) were invited to participate and on agreeing were assigned to either one of EV and PF groups [Figure 1].
Figure 1.
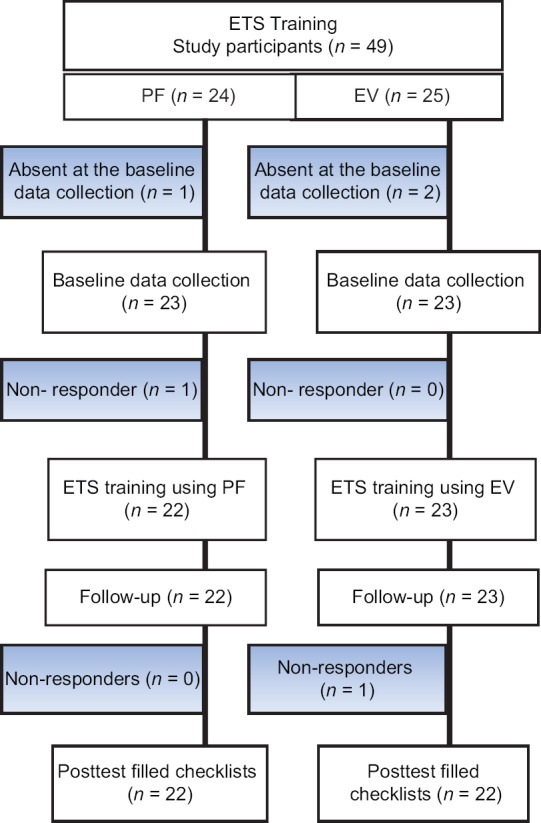
Participants' enrollment for this study
In this study, the inclusion criteria were: (1) having at least a bachelor degree in nursing; (2) informed consent to participate in study; (3) performing direct care of patients with the endotracheal tube; (4) the maximum score obtained of the checklist at the pretest stage to be less than 80% of the total score.
The exclusion criteria included nurses' transfer from the ICU or nurse's unwillingness to collaborate at each stage of the study. The history of prior training on suctioning was not intended as an exclusion criterion, as a person may have been already trained but at the pretest obtained a score of <80% of the checklist total score. Howbeit, none of the nurses had a history of specialized training regarding performing suctioning.
Data collection tools
The instrument used was encompassed of two parts. The first part was related to sociodemographic characteristics which were categorized into age, gender, years of working in critical care, education, and working shift on airway suctioning. The second part was a 25-item structured best practices information sheet related to tracheal suctioning of adults with an artificial airway which was designed by Jansson et al.[18] The checklist comprises of four main parts (practices before ETS event, infection control practices, practices during and post ETS event). The answer to each item was given at two levels: adhere to an item in the recommended procedure (score = 1) and fail to adhere to an item in the recommended procedure (score = 0). The total score of the checklist ranged from 0 to 25.
The checklist validity and reliability
The validity and reliability of the checklist have already been confirmed by Rezaee et al.[1] Before the data collection, the face and content validity of the checklist was determined by ten experts with technical–scientific knowledge regarding the issue (nursing professors, anesthesiologists, and ICU head nurses). Then experts' suggested comments which consisted of minor changes, were involved in the checklist. The reliability of the questionnaire was evaluated using the test–retest method. Fifteen nurses (who were different from those enrolled in the study) were asked to perform ETS on moulage, and this action was repeated next week. The correlation coefficient between the two stages was 0.78.
Moreover, an EV on standard suctioning which its content was in consonance with the standard checklist of ETS was designed and sent to some faculty members of the school of nursing and midwifery and anesthesiologists for determining and judging its relation to the study objectives. After observing the video by professionals, some minor changes were recommended, which again, some stages were repeated and taking video was made again.
Intervention
At the first stage, the researcher as an observer had observed the nurses' ETS practices of intubated patients at all shifts (morning, evening, and night) even on holidays based on the checklist. Next, the nurses ETS practices was recorded in the checklist. Furthermore, the checklists were coded to review each nurse for only once and prevent wrong information being recorded.
Since the performance score of none of the nurses at the pretest was not more than 80% of checklist total score, all nurses (n = 49) were invited to participate and assigned to each of PF and EV groups. To reduce the likelihood of exchange of educational contents between the groups, the nurses at the ICU No. 1 were trained using PF and the nurses at ICU No. 2 received ETS training using EV. For selecting a valid multimedia content for EV group, current ETS EVs in the web were reviewed. Since none of the EVs met all the checklist items, the research team decided to design the video content.
Hence, an 8-min and 22nd EV at the University Clinical Skills Center was formulated by the research team, and corresponding professionals confirmed its content. Following that, the EV through a WhatsApp group was given to nurses in the EV group. Nurses were urged to refrain from sending video content outside the group until the end of the study. In the PF group, the intervention was performed by the first author of this study based on the latest endotracheal suctioning-related guidelines and checklist's items. Given the number of nurses and different working shifts, education at the patients' bedside was carried out individually for nurses in the PF group. In this group, the researcher observed the practice of nurse during performing ETS, and if the nurse performed any of the endotracheal suctioning stages incorrectly, the feedback was immediately provided, and the nurse's performance was corrected. This feedback for each nurse was done two times and at two different working shifts. After the end of the training, participants were followed up for 4 weeks, and no training was provided. Subsequently, the researcher referred again to the same wards and reviewed the endotracheal suctioning performance of the same nurses according to standard checklist and as an observer and without informing the staff.
Ethical considerations
Written consent was obtained from the authorities of the hospital before the start of the study. Besides, before conducting the study, study objectives were explained to the nurses, and informed consent was obtained from them. Nurses were informed that their information was kept confidential. They were ensured that participation in the study is entirely optional. This study was approved in Ethics committee of Ilam University of Medical Sciences (Reference No: IR. MEDILAM. REC.1398.005).
Data analysis
Data were analyzed using SPSS software version 20 (SPSS Inc., Chicago, IL, USA). Descriptive statistics such as percent, mean, and standard deviation (SD) were used to summarize demographic and educational characteristics of the study participants. Chi-square test was used to examine gender, education status, and working shift differences of participants in the groups. Kolmogorov–Smirnov test was applied to evaluate data normality in both groups; also, Levene's test was used to assess the equality of variance.
After confirming the normality of data, ANCOVA test was used to compare the mean difference between groups. The paired t-test was used to compare the means of groups before and after the intervention. P < 0.05 was considered as statistically significant.
Results
A total of 49 participants were studied, of whom 2 and 3 participants from the PF and EV groups were excluded due to absenteeism in the data collection or ETS training sessions, respectively. Finally, the data of 44 particpants consisting of 22 nurses in each of groups were analyzed. The mean ± SD of age of participants in PF and EV groups was 31.82 ± 8.29 and 33.14 ± 7.27, respectively. Moreover, the mean ± SD of work experience of nurses in PF and EV groups was 4.73 ± 3.77 and 7.14 ± 6.14 years, respectively. A significant difference was not observed between the two groups in terms of age and work experience (P > 0.05). Furthermore, none of nurses was taught any training on ETS after graduation. Other demographic and work-related characteristics of participants are depicted in Table 1.
Table 1.
Sociodemographic characteristics of participants
| Variable | Group | Mode | Frequency (%) | P |
|---|---|---|---|---|
| Gender | EV | Male | 7 (31.8) | 0.368 |
| Female | 15 (68.3) | |||
| PF | Male | 5 (22.7) | ||
| Female | 17 (77.3) | |||
| Education status | EV | Bachelor | 18 (81.8) | 0.507 |
| Master | 3 (13.6) | |||
| PhD | 1 (4.5) | |||
| PF | Bachelor | 19 (86.4) | ||
| Master | 1 (4.5) | |||
| PhD | 2 (9.1) | |||
| Working shift | EV | Morning | 14 (63.7) | 0.415 |
| Evening | 5 (22.7) | |||
| Night | 3 (13.6) | |||
| PF | Morning | 10 (45.4) | ||
| Evening | 6 (27.3) | |||
| Night | 6 (27.3) |
PF=Performance feedback, EV=Educational video
At the beginning of the study, the ETS score in both groups was considered as a control variable (covariate). In light of the results, the total mean score of the nurses' practice in ETS among those who had received training through EV was higher than those in PF group (16.3 vs. 15.1), but this difference was not statistically significant, according to ANCOVA test [F (2, 41) =7.67, P = 073, Table 2].
Table 2.
The comparison of nurses ‘performance in endotracheal tube suctioning in both groups before and after the intervention
| Suctioning stages | Variables (source) | Df | Mean square | F | Significant (P) |
|---|---|---|---|---|---|
| Prior to the ETS event | Before the intervention | 1 | 1.28 | 1.95 | 0.17 |
| After the intervention | 1 | 10.94 | 16.65 | <0.0001 | |
| Infection-control event | Before the intervention | 1 | 9.43 | 0.000 | 0.99 |
| After the intervention | 1 | 5.96 | 9.45 | 0.04 | |
| During the ETS event | Before the intervention | 1 | 4.23 | 6.67 | 0.013 |
| After the intervention | 1 | 1.02 | 1.63 | <0.01 | |
| Post-ETS event | Before the intervention | 1 | 1.175 | 3.02 | 0.08 |
| After the intervention | 1 | 0.25 | 0.66 | 0.41 | |
| Total score | Before the intervention | 1 | 14.01 | 7.02 | 0.011 |
| After the intervention | 1 | 0.226 | 0.113 | 0.738 |
ETS=Endotracheal tube suctioning
Moreover, the mean score of nurses practices before ETS event (checklist items 1 to 7) in the PF group was significantly higher than those in EV group (3.23 vs. 2.27) [F (2, 41) = 8.6, P < 0.001, Table 2]. The mean score of nurses' practice in infection control practice (checklist items 8–12) between those who were trained through EV was significantly higher than those in PF group (4 vs. 3.2) (F [2, 41] = 5.2, P = 0.04) [Table 2].
The results also showed that the mean score of nurses' practice during the ETSs event (checklist items 13–18) in EV group was significantly higher than those who did receive training through PF (4.91 vs. 3.59) (F [2, 41] = 16.4, P < 0.01). Furthermore, nurses' post-ETS practices (checklist items 19–25) before and after the intervention in both groups depicted that there is no statistically significant difference between the mean score of groups (F [2, 41] = 1.63, P = 0.41) [Table 2].
Table 3 shows the mean score of nurses' practice in ETS before and after the intervention in PF and EV groups. The results demonstrated a significant increase in the score of nurses' practice in all dimensions of the checklist and total score after the intervention compared with before the intervention.
Table 3.
The comparison of the mean score of nurses’ practice in endotracheal tube suctioning before and after the intervention in both groups
| Suctioning stages | Groups | |||||
|---|---|---|---|---|---|---|
| PF (mean±SD) | P | EV (mean±SD) | P | |||
| Before the intervention | After the intervention | Before the intervention | After the intervention | |||
| Prior to the ETS event | 0.59±0.59 | 2.32±1.06 | <0.0001 | 0.82±0.79 | 2.27±0.45 | <0.0001 |
| Infection-control event | 1.41±0.66 | 3.23±1.06 | <0.0001 | 1.86±0.77 | 4.00±0.30 | <0.0001 |
| During the ETS event | 1.45±0.74 | 3.59±0.59 | <0.0001 | 2.68±0.94 | 4.91±0.52 | <0.0001 |
| Post-ETS event | 1.40±0.73 | 5.09±0.81 | <0.0001 | 2.68±0.88 | 5.18±0.39 | <0.0001 |
| Total score | 4.86±1.24 | 15.14±1.98 | <0.0001 | 8.23±2.34 | 16.36±0.79 | <0.0001 |
ETS=Endotracheal tube suctioning, PF=Performance feedback, EV=Educational video, SD=Standard deviation
Discussion
This study aimed to investigate the effect of two different educational methods on nurses' practice during ETS. To the best of our knowledge, this is the first study that evaluated the effect of PF and EV methods on nurses' practice in ETS in Iran. The results showed that both methods of PF and EV lead to a significant improvement in nurses' practice in performing ETS.
In this study, in practices before ETS event, those who received training through PF had a better performance than nurses in EV group. Day et al. reported that PF is useful in nurses' knowledge and skills during performing ETS, which is in line with our findings.[6] Abu-Hanna et al. also evaluated the effect of providing PF at ward rounds on guideline adherence in nurses and ICU physicians and stated that the percentage of ventilation time in excess of the guideline's recommendation decreased significantly because of the feedback.[19] It appears that the effect of feedback on guideline adherence depends on actual usage of feedback and the inspection of the outcome over time. The previous studies have cited various factors in improving feedback effect, including giving feedback at the right time and non-judgmental practice. Kaye et al. suggested that feedback information is effective in improving clinical practice when it provides feedback close to the time of decision-making. They also commented on other aspects involving the person giving the feedback and the recipient, including differences in gender, age, and educational or cultural background.[14]
The results also suggested that the score of nurses' practice in infection-control practices as well as during the ETS event was higher in nurses in EV group than those in PF group. Keulers et al. conducted a study on patients with Carpel tunnel syndrome in the Netherlands and showed that those who receive education through multimedia content has higher knowledge than those who receive through face-to-face.[20] Furthermore, Varaei et al. evaluated the effect of multimedia education program on knowledge and practice of nurses about safe injection and demonstrated that the implementation of multimedia education program increased knowledge and improved the practice of nurses.[21]
In our study, there was no significant difference between the score of nurses' in practices post-ETS event and the total score of checklist in the two groups. According to the conducted literature review, we did not find any other study that compared the effect of education through multimedia and PF methods. Yet, some studies reported the effect of education through multimedia and lecture method as equal. For example, Barzoki et al. compared the effect of education through lecture and multimedia on knowledge, attitude, and practice of nurses working in cardiac care and revealed no difference between the effectiveness of education through two methods of lecture and multimedia.[13]
Based on our findings, nurses' overall practice in performing ETS in both group of PF and EV improved approximately alike. PF is an important component of education during nurses' care. Giving feedback about clinical practice and its outcomes are essential to develop both confidence and competence at all stages of nurses careers, yet are not embedded in continuum education and routine wards rounds.[22] Useful feedback should be an integral part of nurses' clinical practice. Considering a more immediate formal feedback strategy that focuses on goal-oriented behavior can be effective in improving nurses' clinical practice.[23] Education through multimedia also has been widely used in recent years in clinical education. Studies have shown that education through video is more appropriate in terms of time, place, and even economic for learners, which makes the use of this method more than ever, and its role in ongoing education and lifelong learning to be addressed.[24]
The results of this study can be a useful guide for nurses, managers, as well as planers of continuum education. Since ETS is one of the essential measures in intubated patients our fndings showed the nurses' practice of ETS was poor in the pre-test step. So, providing clinical guidelines in the form of EV and also the implementation of such guidelines by providing ongoing feedback can be useful in improving nurses' practice. Besides, precise monitoring and evaluation of nurses' practice can be useful in the durability of the effect of these methods.
Limitations
Our study has some limitations. First, this study conducted in only two ICU of an educational hospital in the studied city, and samples' informal communication control in groups was not possible about the likelihood of exchange educational contents. Moreover, some participants may have noticed that the study on ETS is performing in their workplace and have deliberately changed their performance or have sought another source on how to undertake ETS accurately. Posttest stage carried out only 4 weeks after the end of the education. These limitations may have affected the results of the study. It is suggested that in future studies, the combined effect of such methods to be evaluated in improving nurses' clinical practice such as ETS. It is also recommended that clinical guidelines content be given to nurses in the form of multimedia and then their behavior to be observed using PF, and be amended in case of need. Besides, further studies are required to ascertain of the extent to which the effect of these educations is durable on nurses' practice in an extended period of time.
Conclusions
The results of this study have raised concerns about nurses' practice in performing ETS, which ought to be of great interest by nursing managers and ICU staff, especially nurses. Our results indicated that none of the critical care nurses (even those with long work experience) had a desirable performance in performing ETS in the pretest stage, meaning that evidence-based performance based on guidelines even among critical care nurses has underlying flaws. The results also demonstrated that both methods of PF and EV are useful in improving nurses' practice in performing ETS. However, these results require more prolonged supervision and more precise design. It is suggested that mid-career training be provided on ETS care principles using approaches used in this study for all critical care nurses irrespective of their work experience.
Financial support and sponsorship
This study is financially supported by Ilam University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This is a report of a database from thesis entitled “the effect of PF and EV on endotracheal-suctioning practices of critical care nurses” approved by Ilam University of Medical Sciences. The authors wish to acknowledge all of the nurses, whose contribution enabled the production of this article. This study was approved in Ethics committee of Ilam University of Medical Sciences (Reference No: IR. MEDILAM. REC.1398.005).
References
- 1.Rezaee HH, Sabzevari S, Sharafkhani R, Golzari Z. Study of nurses performance on standardized endotracheal and tracheostomy tube suctioning in intensive care unit in Kerman hospitals 2013-2014. J Iran Soc Anaesthesiol Intensive Care. 2015;37:11–9. [Google Scholar]
- 2.Meijiao L, Qiao Z, Xiaohua W. CT findings of pulmonary infection in patients with endotracheal intubation and mechanical ventilation. Radiol Infect Dis. 2017;4:1–6. [Google Scholar]
- 3.Pedersen C, Rosendahl-Nielsen M, Hjermind J, Egerod I. Endotracheal suctioning of the adult intubated patient--what is the evidence? Intensive Crit Care Nurs. 2009;25:21–30. doi: 10.1016/j.iccn.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Mazaheri A, Jawadi MS, Mohammadi R, Swadopour M, Kazemzadeh R. Nursing staff performance in chest care in patients undergoing mechanical ventilation. J Health Care. 2013;13:51–6. [Google Scholar]
- 5.Mohammadi N, Parviz S, Pairavi H. The effect of tracheal tube suction retraining on changes in blood oxygen saturation and heart rate in patients admitted to the intensive care unit. J Cardiovasc Nurs. 2013;1:232–45. [Google Scholar]
- 6.Day T, Iles N, Griffiths P. Effect of performance feedback on tracheal suctioning knowledge and skills: Randomized controlled trial. J Adv Nurs. 2009;65:1423–31. doi: 10.1111/j.1365-2648.2009.04997.x. [DOI] [PubMed] [Google Scholar]
- 7.Li G, Cook DJ, Thabane L, Friedrich JO, Crozier TM, Muscedere J, et al. Risk factors for mortality in patients admitted to intensive care units with pneumonia. Respir Res. 2016;17:80. doi: 10.1186/s12931-016-0397-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amirzade N, KHorsandi F, Feizi A, Baghaei R. Evaluating the application of safe suction criteria by nurses working in intensive care unit in Urmia. J Urmia Nurs Midwifery Fac. 2015;11:98–112. [Google Scholar]
- 9.Ghorbanpoor A, Jouybari L, Vakili MA, Sanagoo A, Kavosi A. Knowledge and practices of nurses in intensive care units on endotracheal suctioning. J Nurs Edu. 2018;7:9–17. [Google Scholar]
- 10.Frota O, Loureiro MD, Ferreira AM. Open system endotracheal suctioning: Practices of intensive care nursing professionals. Esc Anna Nery. 2014;18:296–302. [Google Scholar]
- 11.Mwakanyanga ET, Masika GM, Tarimo EA. Intensive care nurses' knowledge and practice on endotracheal suctioning of the intubated patient: A quantitative cross-sectional observational study. PLoS One. 2018;13:e0201743. doi: 10.1371/journal.pone.0201743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ziarat MH, Hashemi M, Fakharzadeh L, Nasagi AN, Khazni S. Assessment of efficacy of oral feedback on trainee's satisfaction in nursing education. J Nurs Edu. 2019;7:11–20. [Google Scholar]
- 13.Barzoki EK, Bakhshandeh H, Nikpajouh A, Elahi E, Haghjoo M. Comparison of the effect of education through lecture and multimedia methods on knowledge, attitude, and performance of cardiac care. J Cardiovasc Nurs J. 2016;4:6–13. [Google Scholar]
- 14.Kaye A, Okanlawon O, Urman R. Clinical performance feedback and quality improvement opportunities for perioperative physicians. Adv Med Educ Pract. 2014;5:115–23. doi: 10.2147/AMEP.S62165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaphle S, Matheke-Fischer M, Lesh N. Effect of performance feedback on community health workers' motivation and performance in Madhya Pradesh, India: A randomized controlled trial. JMIR Public Health Surveill. 2016;2:e169. doi: 10.2196/publichealth.3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brame CJ. Effective educational videos: Principles and guidelines for maximizing student learning from video content. CBE Life Sci Educ Wint. 2016;15:1–6. doi: 10.1187/cbe.16-03-0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Islami Vaghar M. The impact of an educational program on blood and blood products transfusion on nurses' level of knowledge and performance. J Med Life. 2018;11:238–42. doi: 10.25122/jml-2018-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jansson M, Ala-Kokko T, Ylipalosaari P, Kyngäs H. Evaluation of endotracheal-suctioning practices of critical-care nurses an observational correlation study. J Nurs Edu Pract. 2013;3:99–105. [Google Scholar]
- 19.Abu-Hanna A, Eslami S, Schultz MJ, de Jonge E, de Keizer NF. Analyzing effects of providing performance feedback at ward rounds on guideline adherence the importance of feedback usage analysis and statistical control charts. Stud Health Technol Inform. 2010;160:826–30. [PubMed] [Google Scholar]
- 20.Keulers BJ, Welters CF, Spauwen PH, Houpt P. Can face-to-face patient education be replaced by computer-based patient education? A randomised trial. Patient Educ Couns. 2007;67:176–82. doi: 10.1016/j.pec.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 21.Varaei S, Mamashli L, Ghiyasvandian SH, Bahrani N. The Effect of multimedia education program on knowledge and practice of nurses about safe injection. Iran J Nurs. 2016;29:68–77. [Google Scholar]
- 22.Gilder E, Parke RL, Jull A. Endotracheal suction in intensive care: A point prevalence study of current practice in New Zealand and Australia. Aust Crit Care. 2019;32:112–5. doi: 10.1016/j.aucc.2018.03.001. Australian and New Zealand Intensive Care Society Clinical Trials Group and The George Institute for Global Health. [DOI] [PubMed] [Google Scholar]
- 23.Kim J, Gu MO, Chang H. Effects of an evidence-based practice education program using multifaceted interventions: A quasi-experimental stud with undergraduate nursing students. BMC Med Edu. 2019;19:1–10. doi: 10.1186/s12909-019-1501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tang B, Coret A, Qureshi A, Barron H, Ayala AP, Law M. Online lectures in undergraduate medical education: Scoping review. JMIR Med Educ. 2018;4:e11. doi: 10.2196/mededu.9091. [DOI] [PMC free article] [PubMed] [Google Scholar]


