Abstract
CONTEXT:
One of the most important issues in patients with coronary artery disease is their mental health indices such as perceived stress and perception of disease.
AIMS:
The aim of this study was to evaluate the effectiveness of mindfulness-based intervention on the perceived stress and disease perception of patients with acute coronary syndrome.
MATERIALS AND METHODS:
This is a clinical trial, two-group, and three-stage study on 76 patients with acute coronary syndrome who were randomly divided into intervention and control groups. Nine weekly sessions of mindfulness-based training program were administered to the intervention group. The control group received routine services during this period. Data collection was done before, immediately, and 1 month after the intervention, using the Perceived Stress Scale and the Illness Perception Questionnaire. Data were analyzed using descriptive and inferential statistics.
RESULTS:
There was no significant difference between the mean scores of perceived stress and illness perception before intervention. After the intervention and 1 month after it, the mean score of perceived stress in the intervention group was statistically significantly lower than the control group (P < 0.001), and the perception of disease in the intervention group was statistically significantly higher than that of the control group (P < 0.001).
CONCLUSIONS:
It is worthwhile to suggest the mindfulness-based training program to reduce the perceived stress and correct the perception of disease for patients with acute coronary syndrome.
Keywords: Acute coronary syndrome, illness perception, mindfulness, perceived stress
Introduction
Coronary artery disease is the leading cause of premature death and disability in developed countries;[1] it is generally accepted that it is the most common cause of death in the world in the next few years.[2] In Iran, the prevalence of coronary artery disease and its resulting mortality is increasing, accounting for 46% of the causes of death. According to surveys, the prevalence of coronary artery disease in Isfahan is 19.4%.[3]
In most patients with cardiovascular disease, mental disorders are seen as a comorbid condition,[4] which leads to a defective cycle of exacerbation and poor care and treatment outcomes.[5,6] One of the predictors of mental health status of the involved patients is their experience and understanding of stress.[7] The concept of perceived stress refers to the level of stress experienced by the individual as a function of the stressful events and coping strategies faced by them.[8] Some evidence has shown that the perceived stress in cardiac patients is an important predictor of mental well-being in these patients[9] and the higher levels of perceived stress are associated with a higher risk of death in these patients.[10]
In addition to the perceived stress, the researchers nowadays have focused on the crucial role of the perception of disease and its relationship to many outcomes related to the care and treatment in the patients' physical and mental health.[11,12] Although awareness of the cardiovascular risk factors is essential for each individual to help him/her make informed decisions about the continuation of specific behaviors that increase the risk of the disease,[13] what is important is the individual's perception of the danger and the nature of the disease that affects his/her health-related performances. The results of studies have emphasized the dynamic relationship between the perception of disease and the mental health indices, especially in the cardiac patients, even though they identified it as a strong predictor of anxiety and depression in those patients.[14] It has also emphasized its effect on the adherence of treatment and quality of life in these patients.[15,16]
So far, the researchers have taken various steps to improve mental health and influence mental health determinants in patients with chronic diseases, especially heart disease. For example, the findings of the study by Sadeghimoghaddam et al. supported the impact of relaxation and prayer therapy on anxiety and hope in patients with coronary artery disease.[17] According to Zeraatkar et al., considering the high costs of hospital stay and the length of cardiac disease treatment, the psychological intervention have significant impact on improving the patients' quality of life and their mental health.[18]
One of the interventions that has been considered in recent years and has been attempted to influence mental health indices and determinants in chronic patients is the mindfulness-based interventions. These interventions include various meditations, stretch yoga, introductory stress training, body exercises, and several cognitive therapy exercises that show the relationship between mood, thoughts, feelings, and physical sensations, and are a kind of therapies. The following three basic goals are pursued: (a) attention regulation; (b) metacognitive awareness; and (c) decentralization and acceptance of mental states and contents.[19,20]
Some researchers have investigated the effect of mindfulness-based interventions on the different aspects of health in chronic patients. The results suggest that these interventions play a key role in reducing perceived stress[21] and anxiety symptoms in cancer patients[22] and improving stress management in patients with asthma.[23]
One of the areas of increasing use of mindfulness-based interventions is medical centers and specialized heart hospitals. Nowadays, the specialist doctors and nurses working in heart departments speak of the importance of mindfulness exercises alongside a healthy lifestyle to prevent heart disease. Some researches on this group of patients have shown that this intervention improves irregular cardiac activities[24] and may reduce the risk factors for these diseases.[25]
Based on the previous researches and studies, it was found that despite increasing attention to the mental health status of cardiac patients, the focus of studies is not on the predictive and preventable indices of mental health (such as perceived stress and perception of disease). They have focused on the indices of the occurrence of mental disorders (such as depression and anxiety disorders). The literature review also shows that despite the value and importance of mindfulness-based interventions in chronic disease patients, the impact of these interventions, especially on these indices in cardiac disease patients, has not been addressed. The purpose of this research is to investigate the effect of mindfulness-based intervention on the perceived stress and perception of disease in patients with acute coronary syndrome.
Materials and Methods
The present study was a pretest-posttest study with a follow-up clinical trial conducted from September 2018 to July 2019.
Setting and sample
The study population comprised patients with acute coronary syndrome who were admitted, being discharged, or discharged (within a week before) in the internal wards of Chamran Medical Center affiliated with Isfahan University of Medical Sciences (IUMS), Iran. They were selected by convenience sampling method. After selecting the participants, they were randomly assigned to two (i.e. intervention and control) groups of 38 people [CONSORT diagram, Figure 1].
Figure 1.
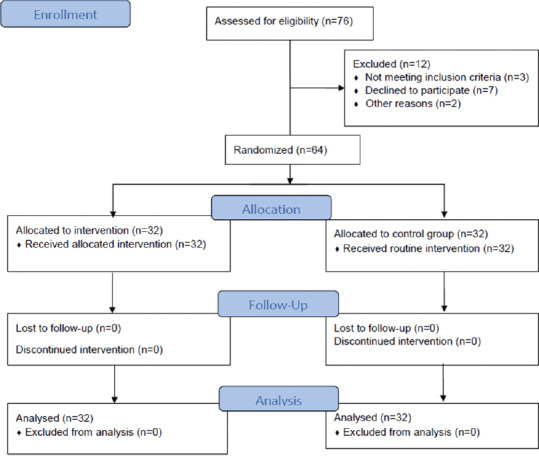
CONSORT followflow diagram of the study
Inclusion criteria
The inclusion criteria for participation in the study were completion of the consent form, ability to attend interventional sessions, minimum reading and writing literacy, age between 35 and 70 years, no attendance in other training and treatment courses over the past year, having coronary artery disease diagnosed (based on clinical and paraclinical diagnosis and file summary), being fully alert as required to attend in the intervention sessions, having ability to complete the research instruments, and living in Isfahan city. Patients who did not have these conditions, had other concomitant diseases, had a medical history of psychiatric diagnosis, or had mental retardation were not included in the study.
Data collection and instruments
Data were collected by a three-part assessment tool, first of which included demographic and personal information questionnaire (i.e. age, gender, marital status, occupation, insurance status, history of hospitalization, education level, financial status, and duration of disease).
Perceived Stress Scale-14
This questionnaire was developed by Cohen et al.[8] and has three 4-, 10-, and 14-item versions to measure perceived general stress over 1 past month. The 14-item scale measures thoughts and feelings about stressful events and the ability of controlling, overcoming, and coping with mental stress and experienced stress through examining responses. Each item is awarded based on a 5-point Likert scale of “never” 0, “almost never” 1, “sometimes” 2, “often” 3, and “most often” 4. Items 4, 5, 6, 7, 9, 10, and 13 are reverse coded. The lowest score is 0 and the highest is 56. In the study by Cohen et al., the internal consistency coefficients for each subscale and overall Perceived Stress Scale (PSS) score ranged from 0.84 to 0.86.[8] In a study by Safaei and Shokri, the Persian version of PSS has been evaluated and Cronbach's alpha coefficients for the total perceived stress score has been reported as 0.76.[26]
Brief Illness Perception Questionnaire
The brief Illness Perception Questionnaire (IPQ) has nine subscales designed by Broadbent et al.[27] to assess the emotional and cognitive visualization of the disease. The number 0 represents the lowest level and the number 10 represents the highest level of perception. The overall score for illness perception indicates a grade based on which the patients perceive their illness as a threatening or benign factor. Cronbach's alpha for this questionnaire was 0.80, and the reliability-retest coefficient of 6 weeks was 0.42–0.75.[27]
Study process and intervention
Before the study process, this trial was registered in the Iranian Registry of Clinical Trials (IRCT) (code: IRCT20160927030002N2). After official arrangements for conducting the intervention, the participants from both groups were asked to participate in a briefing. At this meeting, outlining the aims of the research, it was attempted to gain the necessary motivation and consent of the clients to participate in the research. The clients completed the consent form to participate in the research and were assured that the information presented in the interventional sessions and the results of the questionnaires would be confidential.
The interventional group received a mindfulness-based program during nine 2-h sessions (one session per week) [Table 1] at the hospital and the control group received no intervention other than routine services. Data collection was done in three stages of before, immediately, and 1 month after the intervention. In order to appreciate the control group's participation, after the follow-up stage, four similar compressed sessions of intervention were held for them.
Table 1.
Mindfulness training program
| Content |
|---|
| Session 1: Recognition of excitements, compositional excitements, describe excitement, enjoy the beauty of nature |
| Session 2: Skill one: Focus on a particular object, skill two: Focus on a single moment, familiarity with the concept of mindfulness at the moment, see the wonders of the present moment |
| Session 3: Skill three: Inner and outer experience, The concept of physical mindfulness, eating raisins, the great taste of mindfulness, enjoy the journey |
| Session 4: What is the excitement? What is the feeling? Recognition of excitements, familiarity with some types of excitement, awareness of feelings and excitements, providing a list of main feelings and subfeelings, listening to unpleasant excitements |
| Session 5: What is the excitement? What is the feeling? recognition of excitements, familiarity with some types of excitement, awareness of feelings and excitements, providing a list of main feelings and subfeelings, listening to unpleasant excitements |
| Session 6: Recognition of thoughts, necessity of training, identifying the difference between thought and feeling, and the concept of thought in mindfulness, Skill five: The fault of thought, Skill six: Record 30 min of thought, keep in your mind that you are different from your thoughts |
| Session 7: Understanding the concepts of body, thought, and feeling mindfulness, skill seven: mindful breathing |
| Session 8: A few key methods for a mindful life, Skill eight: A mindful diet, mindfulness in mindful activities |
Ethical considerations
This study was approved by the Deputy Dean for Research Affairs (grant number 397665) and Ethics Committee (code: IR RESEARCH. REC.1397.491) of IUMS. All participants completed and signed informed consent form, and they were free to discontinue participating in this study whenever they wished.
Data analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows, version 18 (SPSS Inc., Chicago, IL, USA). Data were analyzed using descriptive and inferential statistics. Independent sample t-test, Chi-square test, and Fisher's exact test were used for between-group baseline comparisons. Analysis of covariance was used for between-group comparisons to assess the effect of intervention on PSS and IPQ scores controlling for baseline scores. Assumptions of normality and homogeneity of variance were assessed using Kolmogorov–Smirnov test and Levene's test.
Results
Patients were in the age range of 35–70 years. The age range of the participants in the intervention group was 34–72 years, with a mean of 52.71 and a standard deviation of 10.94; in the control group, it was from 15 to 72 years, with a mean of 52.16 and a standard deviation of 13.56 years. The independent sample t-test showed that the mean age was not statistically significantly different between the two groups (t = 0.17, df = 0.62, P = 0.86).
Other demographic characteristics of the participants were compared between the two groups and their results are reported in Table 2. The results showed that there was no significant difference between the two groups in terms of demographic variables and disease characteristics. Table 3 summarizes the statistics for between-group comparison of PSS and IPQ scores. According to the findings, the mean score of perceived stress immediately and 1 month after the intervention was statistically significantly lower in the intervention group than that of the control group (P < 0.05). In addition, the results showed that the mean score of illness perception immediately and 1 month after the intervention was statistically significantly higher in the intervention group than that of the control group (P < 0.05).
Table 2.
Baseline demographic and clinical characteristics of the study participants
| Variable | Characteristics | Group control, n (%) | Intervention group, n (%) | χ2 | df | p |
|---|---|---|---|---|---|---|
| Gender | Female | 14 (43.8) | 12 (37.5) | 0.26 | 1 | 0.61a |
| Male | 18 (56.2) | 20 (62.5) | ||||
| Marital status | Married | 27 (84.4) | 28 (87.5) | - | - | 0.50b |
| Single | 5 (15.6) | 4 (12.5) | ||||
| Job | Employee | 28.1 (9) | 3 (9.4) | 6.63 | 4 | 0.14a |
| Worker | 3 (9.4) | 6 (18.7) | ||||
| Free | 3 (9.4) | 7 (21.9) | ||||
| Homemaker | 14 (43.7) | 15 (46.9) | ||||
| Others | 3 (9.4) | 1 (3.1) | ||||
| Supported by insurance | 29 (90.6) | 32 (100) | - | - | 0.12b | |
| History of admission | 3 (9.4) | 6 (18.8) | - | - | 0.2b | |
| Variable | Characteristics | Group control, n (%) | Intervention group, n (%) | Z | p | |
| Level of education | Elementary | 9 (28.1) | 3 (9.4) | 0.78 | 0.44c | |
| Cycle degree | 9 (28.1) | 9 (28.1) | ||||
| Diploma | 7 (21.9) | 7 (21.9) | ||||
| Associate degree | 1 (3.1) | 1 (3.1) | ||||
| Bachelor’s degree and higher | 5 (15.7) | 5 (15.7) | ||||
| Income status | Less than spending | 12 (37.5) | 15 (46.9) | 0.59 | 0.55c | |
| At the expense level | 20 (62.5) | 16 (50) | ||||
| More than spending | 0 | 1 (3.1) | ||||
| Duration of the disease (year) | <1 | 23 (71.9) | 20 (62.5) | 0.93 | 0.35c | |
| 1-3 | 4 (12.5) | 4 (12.5) | ||||
| 4-6 | 3 (9.4) | 3 (9.4) | ||||
| 7-9 | 0 (0) | 1 (3.1) | ||||
| 10 and more | 2(6.2) | 4 (12.5) | ||||
aChi-square test, bFisher’s exact test, cMann-Whitney U-test
Table 3.
Comparison of mean scores of perceived stress and illness perception in the intervention and control groups before, immediately, and 1 month after intervention
| Variable | Time | Group control | Intervention group | Test statistics | p | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t (df) or f(df) | |||
| Perceived stress | Before intervention | 31.02 | 5.74 | 30.83 | 7.86 | t (df)= 0.11(62) | 0.91* |
| Immediately after intervention | 32.06 | 0.61 | 28.01 | 6.97 | f (df)= 17.25 (1) | <0.001** | |
| 1 month after intervention | 33.75 | 3.78 | 23.03 | 7.79 | f (df)= 48.35 (1) | <0.001** | |
| Brief illness perception | Before intervention | 45.47 | 6.95 | 46.63 | 15.08 | t (df)= 0.39(60) | 0.69* |
| Immediately after intervention | 44.56 | 2.94 | 49.41 | 9.01 | f (df)= 9.50 (1) | <0.003** | |
| 1 month after intervention | 46 | 3.80 | 57.75 | 11.55 | f (df)= 32.61 (1) | <0.001** | |
*T-test, **ANCOVA. ANCOVA=Analysis of covariance, SD=Standard deviation
Discussion
The purpose of this research was to investigate the effect of mindfulness-based intervention on the perceived stress and perception of illness in patients with coronary artery disease. The results of the research showed that the mindfulness-based intervention can significantly reduce the perceived stress and this effect has been continued 1 month after the intervention. This finding is in line with that of the studies demonstrating the benefits of mindfulness training to effectively manage perceived stress.[28,29] Our findings are also consistent with the results of the research conducted by Radmehr andYousefvand,[30] supporting the reduction of perceived stress in patients with coronary artery disease, and have been supported by Akbari et al.,[31] who supported the effect of mindfulness training on perceived stress of cancer patients. According to Snippe et al.,[28] mindfulness-based intervention reduces negative affect (i.e. stress sensitivity) and also reduces the extent to which individuals perceive their living situations as stressful.
Furthermore, according to the findings of the study, the intervention was able to significantly modify the perception of the disease both after the intervention and 1 month after it. The findings of the present research on the illness perception are in line with the findings of some studies in the field of other diseases. For example, this finding is similar to the findings of the study conducted by Fowler and Baas in identifying and positively perceiving the disease in order to minimize the perceived consequences of the disease in patients with chronic kidney disease who underwent hemodialysis.[32] We can refer to the findings of a study done by Scharloo et al. in restructuring the perception of the disease, in order to better treat people recently diagnosed with head-and-neck cancer.[33] The findings of the study conducted by Ljótsson et al.[34] confirm the effectiveness of mindfulness-based intervention in reducing the psychological symptoms of patients with irritable bowel syndrome. That is the case also about the findings of a study done by Mohamadi et al.[35] that supported the effectiveness of this intervention in improving the perception of illness in patients with irritable bowel syndrome in Iran.
This study provides evidence in support of the feasibility and effectiveness of mindfulness-based intervention in patients with acute coronary syndrome.
Limitations of the study included reliance on self-report data and absence of a long-term follow-up. Another limitation of the study was that the studied sample was restricted to Isfahan patients only, so caution should be exercised in generalizing its results. Further research is needed to confirm these results and to examine the potential of such interventions.
As the use of mindfulness-based training intervention was associated with a decrease in perceived stress and a positive perception of disease in patients with coronary artery disease, it is suggested that nurses and other health professionals be able to use this technique so that they can communicate more effectively with these patients in order to take steps to improve their mental health.
Conclusions
Considering the mindfulness-based training intervention, it may be worthwhile to suggest launching this training program in respective units to reduce the perceived stress and correct the perception of disease for patients with acute coronary syndrome.
Financial support and sponsorship
This study was financially supported by IUMS, Isfahan, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study was approved by the Research Committee of IUMS (code: IR RESEARCH. REC.1397.491). The authors express their gratitude to the Research Deputy of the IUMS. The authors also thank all the study participants who made this study possible through their cooperation and support.
References
- 1.Kahungu L. Contemporary themes in health care Incidence and Management of Coronary Heart Disease in the United Kingdom GRIN Verlag. 2018 [Google Scholar]
- 2.Lemos DJ, Omland T. Chronic coronary artery disease: A companion to Braunwald's heart disease E-Book. Philadelphia: Elsevier Health Sciences; 2017. [Google Scholar]
- 3.Momeni T, Musarezaie A, Moeini M, Esfahani NH. The effect of spiritual care program on ischemic heart disease patients, anxiety, hospitalized in CCU: A clinical trial. J Res Behav Sci. 2013;6:554–64. [Google Scholar]
- 4.De Hert M, Detraux J, Vancampfort D. The intriguing relationship between coronary heart disease and mental disorders. Dialogues Clin Neurosci. 2018;20:31–40. doi: 10.31887/DCNS.2018.20.1/mdehert. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akbari M, Mousavi MS, Shirani F, Massoumi G, Shafeie M, Niknejad R, Khourasani P, Alavi M, Ghadami A. Sharing the power through promoting heart health literacy: A participatory action research in Iran. ARYA Atheroscler. 2019;15:146–51. doi: 10.22122/arya.v15i3.1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: A meta-analysis. J Am Coll Cardiol. 2010;56:38–46. doi: 10.1016/j.jacc.2010.03.034. [DOI] [PubMed] [Google Scholar]
- 7.Pimple P, Lima BB, Hammadah M, Wilmot K, Ramadan R, Levantsevych O, et al. Psychological distress and subsequent cardiovascular events in individuals with coronary artery disease. J Am Heart Assoc. 2019;8:e011866. doi: 10.1161/JAHA.118.011866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 9.Kamoei K, Meschi F. The relationship between perceived stress and coping styles with psychological well-being in cardiac patients. Int J Med Res Health Sci. 2016;5:707–11. [Google Scholar]
- 10.Arnold SV, Smolderen KG, Buchanan DM, Li Y, Spertus JA. Perceived stress in myocardial infarction: Long-term mortality and health status outcomes. J Am Coll Cardiol. 2012;60:1756–63. doi: 10.1016/j.jacc.2012.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sadeghi M, Alavi M, Mohammadi M, Roohafza H, Mahmoodi A, Visentin D, et al. Perceptions of illness as predictive factors for perceived stress in patients participating in a cardiac rehabilitation program. Nurs Health Sci. 2019;21:508–14. doi: 10.1111/nhs.12635. [DOI] [PubMed] [Google Scholar]
- 12.van Erp SJ, Brakenhoff LK, Vollmann M, van der Heijde D, Veenendaal RA, Fidder HH, et al. Illness perceptions and outcomes in patients with inflammatory bowel disease: Is coping a mediator? Int J Behav Med. 2017;24:205–14. doi: 10.1007/s12529-016-9599-y. [DOI] [PubMed] [Google Scholar]
- 13.Winham DM, Jones KM. Knowledge of young African American adults about heart disease: A cross-sectional survey. BMC Public Health. 2011;11:248. doi: 10.1186/1471-2458-11-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgan K, Villiers-Tuthill A, Barker M, McGee H. The contribution of illness perception to psychological distress in heart failure patients. BMC Psychol. 2014;2:50. doi: 10.1186/s40359-014-0050-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sarrafzadegan N, Rabiei K, Alavi M, Abedi H, Zarfeshani S. How can the results of a qualitative process evaluation be applied in management, improvement and modification of a preventive community trial? The IHHP Study. Arch Public Health. 2011;69:9. doi: 10.1186/0778-7367-69-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tkhostov A, Nelyubina A. Illness perceptions in patients with coronary heart disease and their doctors. Procedia Soc Behav Sci. 2013;86:574–7. [Google Scholar]
- 17.Sadeghimoghaddam S, Alavi M, Mehrabi T, Bankpoor-Fard A. The effect of two methods of relaxation and prayer therapy on anxiety and hope in patients with coronary artery disease: A Quasi-experimental study. Iran J Nurs Midwifery Res. 2019;24:102–7. doi: 10.4103/ijnmr.IJNMR_60_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zeraatkar M, Boogar RI, Talepasand S, Amin A. The effectiveness of healthy lifestyle promotion intervention on quality of life in patients with congestive heart failure via cognitive-behavioral procedure. SSU J 201623. 2016;23:1094–107. [Google Scholar]
- 19.Crane R. Mindfulness-Based Cognitive Therapy: Distinctive Features. New York: Taylor and Francis; 2017. [Google Scholar]
- 20.Segal ZV, Teasdale J. Mindfulness-Based Cognitive Therapy for Depression. New York: Guilford Publications; 2018. [Google Scholar]
- 21.Zainal NZ, Booth S, Huppert FA. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: A meta-analysis. Psychooncology. 2013;22:1457–65. doi: 10.1002/pon.3171. [DOI] [PubMed] [Google Scholar]
- 22.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65:571–81. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- 23.Kimura T, Yokoyama A, Kohno N, Nakamura H, Eboshida A. Perceived stress, severity of asthma, and quality of life in young adults with asthma. Allergol Int. 2009;58:71–9. doi: 10.2332/allergolint.O-07-531. [DOI] [PubMed] [Google Scholar]
- 24.Gao J, Fan J, Wu BW, Zhang Z, Chang C, Hung YS, et al. Entrainment of chaotic activities in brain and heart during MBSR mindfulness training. Neurosci Lett. 2016;616:218–23. doi: 10.1016/j.neulet.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 25.Spijkerman MP, Pots WT, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clin Psychol Rev. 2016;45:102–14. doi: 10.1016/j.cpr.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Safaei M, Shokri O. Assessing Stress in Cancer Patients: Factorial Validity of the Perceived Stress Scale in Iran. 2014 [Google Scholar]
- 27.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 28.Snippe E, Dziak JJ, Lanza ST, Nyklíček I, Wichers M. The shape of change in perceived stress, negative affect, and stress sensitivity during mindfulness-based stress reduction. Mindfulness. 2017;8:728–36. doi: 10.1007/s12671-016-0650-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lengacher CA, Shelton MM, Reich RR, Barta MK, Johnson-Mallard V, Moscoso MS, et al. Mindfulness based stress reduction (MBSR (BC)) in breast cancer: Evaluating fear of recurrence (FOR) as a mediator of psychological and physical symptoms in a randomized control trial (RCT) J Behav Med. 2014;37:185–95. doi: 10.1007/s10865-012-9473-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Radmehr P, Yousefvand L. he investigating rate of mindfulness-based cognitive therapy in reduces perceived stress and increase life expectancy in women suffering coronary artery disease. Iran J Health Educ Health Promot. 2017;5:164–72. [Google Scholar]
- 31.Akbari M, Nafisi N, Jamshidifar Z. Effectiveness of mindfulness training in decreasing the perceived stress among the patients suffering from breast cancer. J Thought Behav Clin Psychol. 2013;7:7–16. [Google Scholar]
- 32.Fowler C, Baas LS. Illness representations in patients with chronic kidney disease on maintenance hemodialysis. Nephrol Nurs J. 2006;33:173. [PubMed] [Google Scholar]
- 33.Scharloo M, Baatenburg de Jong RJ, Langeveld TP, van Velzen-Verkaik E, Doorn-op den Akker MM, Kaptein AA. Quality of life and illness perceptions in patients with recently diagnosed head and neck cancer. Head Neck. 2005;27:857–63. doi: 10.1002/hed.20251. [DOI] [PubMed] [Google Scholar]
- 34.Ljótsson B, Andréewitch S, Hedman E, Rück C, Andersson G, Lindefors N. Exposure and mindfulness based therapy for irritable bowel syndrome – An open pilot study. J Behav Ther Exp Psychiatry. 2010;41:185–90. doi: 10.1016/j.jbtep.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 35.Mohamadi J, Mir Drikvand F, Azizi A. Efficacy of mindfulness on anxiety and depression in patients with irritable bowel syndrome. J Mazandaran Univ Med Sci. 2015;25:52–61. [Google Scholar]


