Abstract
The aim of this study is to assess whether the effect of gender on the excessive daytime sleepiness (EDS) is influenced by two confounders (age and hours of sleep per night). A cross-sectional study was conducted at King Abdulaziz Medical City-Riyadh (KAMC-R). A total of 2095 respondents answered a questionnaire that included questions regarding gender, age, hours of sleep per night, and daytime sleepiness using the Epworth Sleepiness Scale (ESS). The prevalence of EDS was 20.5% (females 22.2%, males 19.5%, p-value = 0.136). The EDS did not differ between genders, age groups, or hours of sleep per night (<6 vs. ⩾6 h). However, stratified statistical analysis shows that the prevalence of EDS did differ according to gender (25.3% in females, 19.0% in males, p-value = 0.036) in respondents with shorter hours of sleep per night. EDS was strongly related to female gender and young age (ages ⩽ 29 years) in respondents with short hours of sleep. This study reveals that one out of five of the general Saudi population has EDS. The effect of gender on EDS appeared to be influenced by hours of sleep per night. High EDS strongly related to female gender with short hours of sleep.
Keywords: Epworth Sleepiness Scale, Excessive daytime sleepiness, Hours of sleep per night, Saudi Arabia
1. Introduction
Excessive daytime sleepiness (EDS) is one of the most common features of sleep disorders [1]. EDS should be reserved for patients who complain of compulsory sleepiness, or urge to take naps or tendency to fall asleep, or cannot remain awake when intending to stay awake [2–4]. EDS as a manifestation of disturbed sleep or sleep deprivation has tremendous consequences that affect individuals and society in general [5]. Excessive sleepiness may lead to major morbidity and mortality, lack of production, weak academic achievement, accidents and injuries [6–14].
The Epworth Sleepiness Scale (ESS) is the most commonly used questionnaire for assessing a person’s average level of daytime sleepiness in daily life [2–4,15]. The ESS questionnaire assesses the degree of sleeping in different circumstances, such as a person with excessive sleepiness may fall asleep while watching TV programs, while reading, when chatting with other people, after eating lunch, in public places, or when the car stops for a short time in front of traffic lights while driving [16,17]. The ESS ranges from 0 (no daytime sleepiness) to 24 points (a high level of daytime sleepiness). There are many causes of EDS; the most common sleep disorders causing EDS are sleep breathing disorders [18], narcolepsy [19] and restless legs syndrome (RLS) [20].
The true prevalence of EDS due to different causes is difficult to know. The published studies reported variations in the prevalence among different countries and ethnicity. The reasons for such variations include definition and methodology used to measure EDS; however, the overall prevalence ranged from 15% to 39% [3,4,15,21–26]. The prevalence of EDS (ESS score > 10) in a sample of the Australian adult population was 10.4% for males and 13.6% for females [27]. The prevalence of EDS was 15.9% and 20.8% in Canadian rural populations [3,28], and 14.6% among Turkish rural populations [4]. The prevalence of EDS was found to be 19.8% in a north Irish population [29], 15% and 2.5% among Japanese adults [25,30], 17.8% among the Swedish population [31], 5.5–15.2% among the British [32] and 45% among US Hispanics [33].
Unfortunately, there is a lack of studies on the prevalence of EDS among the general population in Arab countries, including the Kingdom of Saudi Arabia. The prevalence of EDS in Saudi patients with end-stage renal disease has been estimated to be 44% [34] and 39.3% among healthcare employees [22]. However, symptoms of EDS among Saudi adults and its associated factors in the general population still remain unaddressed. The aim of this research is to investigate gender differences in the risk of EDS among a sample of Saudis using ESS for assessment. When no difference in the risk of EDS is seen between both sexes, the roles of two confounders (age and hours of sleep per night) were further studied, which could lead to the gender differences in EDS.
2. Methods
A cross-sectional study was conducted among Saudi participants aged 18 or older at Riyadh. The authors confirm that the study was reviewed and approved by the research committee and by the institutional review board at King Abdullah International Medical Research Center (KAIMRC), protocol number SP14/045, before the study began. As per IRB approval, all participants were provided with written information about the study purpose and were informed that the information obtained would be kept confidential and no participant identity would be revealed. Once they agreed verbally to participate, they were enrolled in the study. These participants were gathered from the following sources: blood donors, new employees, hospital employees and visitors of primary clinics. Exclusion criteria were shift work, traveling across time zones during the past 4 weeks, and use of any prescriptions or medications known to affect sleep. Research assistants distributed the questionnaire after participants’ verbal consent and ensured that all the questions were answered. Demographical data (age, gender, education, marital status, job or profession, hours of sleep per day, underlying medical problems and personal habits regarding sleep pattern, coffee and tea drinks, etc.) were collected. In addition, this study assessed the ESS using the validated Arabic version [35]. The validated Arabic version of the ESS includes eight items with an overall range of 0–24 (where 0 stands for no daytime sleepiness and 24 stands for a high level of daytime sleepiness). Participants were asked to rate on a scale of (0–3) how likely they would be to doze off or fall asleep in the eight situations, based on their usual lifestyle in recent times. If a subject had not been in some of the situations recently, he was asked, nonetheless, to estimate how each might affect him. Participants with ESS scores greater than 10 would be classified as having excessive daytime sleepiness or very sleepy [16]. The Pittsburgh Sleep Quality Index (PSQI) was also used to assess sleep quality; a score of 5 or more indicates poor sleep quality [36].
3. Statistical analyses
Data were analyzed using SPSS 22 (SPSS, Inc., Chicago, IL). ESS > 10 represents the presence of EDS. The reliability of the ESS was investigated by Cronbach’s alpha. Pearson Chi-square tests were used to assess the associations between gender, age, hours of sleep per night, coffee intake, tea intake, and obesity across EDS groups (Tables 1 and 2). Respondents were divided into 2 groups: those who reported short (<6) hours of sleep and those who reported longer (⩾6) hours of sleep per night. The Mantel–Haenszel analysis examined the gender differences in the prevalence of EDS among respondents with short hours of sleep per night (Table 3). Furthermore, the effects of age, gender, and hours of sleep jointly were examined. In this regard, gender differences in the prevalence of EDS among young respondents with short hours of sleep per night (Table 4) were investigated. p-Values less than 0.05 are considered to grant sufficient evidence of a significant difference.
Table 1.
EDS and its relation to demographic/clinical characteristics.
| Characteristics | Levels | Overall N = 2095 |
Non-EDS 1666 (79.5%) |
EDS 429(20.5%) |
p-Value | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Gender | Female | 848 | 40.7 | 660 | 77.8 | 188 | 22.2 | 0.136 |
| Male | 1237 | 59.3 | 996 | 80.5 | 241 | 19.5 | ||
| Age group (years) | ⩽29 | 509 | 25.0 | 115 | 22.6 | 394 | 77.4 | 0.554 |
| 30–39 | 481 | 24.0 | 86 | 17.9 | 395 | 82.1 | ||
| 40–49 | 370 | 18.0 | 80 | 21.6 | 290 | 78.4 | ||
| 50–59 | 333 | 16.0 | 67 | 20.1 | 266 | 79.9 | ||
| 60–69 | 253 | 12.0 | 53 | 20.9 | 200 | 79.1 | ||
| ⩾70 | 97 | 5.0 | 18 | 18.6 | 79 | 81.4 | ||
| Marital Status | Single | 389 | 18.7 | 295 | 75.8 | 94 | 24.2 | 0.209 |
| Married | 1481 | 71.4 | 1186 | 80.1 | 295 | 19.9 | ||
| Widow | 118 | 5.7 | 93 | 78.8 | 25 | 21.2 | ||
| Divorced | 87 | 4.2 | 73 | 83.9 | 14 | 16.1 | ||
| Occupation | Employee | 1094 | 52.6 | 874 | 79.9 | 220 | 20.1 | 0.752 |
| Retired | 254 | 12.2 | 202 | 79.5 | 52 | 20.5 | ||
| Not working | 74 | 3.6 | 61 | 82.4 | 13 | 17.6 | ||
| Student | 288 | 13.8 | 221 | 76.7 | 67 | 23.3 | ||
| Housewife | 371 | 17.8 | 297 | 80.1 | 74 | 19.9 | ||
Table 2.
EDS and clinical/sleep disruption characteristics.
| Characteristics | Overall N = 2095 |
Non-EDS 1666(79.5%) |
EDS 429(20.5%) |
p-Value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Obese | 1094 | 52.2 | 867 | 66.9 | 227 | 67.4 | 0.887 |
| Coffee Intake | 1511 | 72.1 | 1198 | 71.9 | 313 | 73.0 | 0.665 |
| Tea Intake | 1332 | 63.6 | 1055 | 63.3 | 277 | 64.6 | 0.633 |
| Diabetes | 436 | 20.8 | 344 | 20.6 | 92 | 21.4 | 0.717 |
| Hypertension | 711 | 33.9 | 567 | 34.0 | 144 | 33.6 | 0.855 |
| Depression | 91 | 4.3 | 72 | 4.3 | 19 | 4.4 | 0.923 |
| Asthma | 361 | 17.2 | 272 | 16.3 | 89 | 20.7 | 0.031* |
| Less than 6 h of sleep/night | 708 | 33.8 | 554 | 33.3 | 154 | 35.9 | 0.302 |
| Snore | 761 | 36.4 | 583 | 35.0 | 178 | 41.6 | 0.012* |
| Poor sleep quality as per PSQI | 1674 | 83.3 | 1310 | 82.0 | 364 | 88.3 | 0.002* |
| Difficulty falling asleep | 1440 | 68.7 | 1127 | 67.6 | 313 | 73.0 | 0.034* |
| Frequent awakening | 1426 | 68.1 | 1112 | 66.7 | 314 | 73.2 | 0.011* |
| Wake up too early | 1545 | 73.7 | 1220 | 73.2 | 325 | 75.8 | 0.289 |
| Feel tired | 1597 | 76.2 | 1244 | 74.7 | 353 | 82.3 | 0.001* |
| Sleep loss affect your mood | 1107 | 52.8 | 845 | 50.7 | 262 | 61.1 | 0.001* |
The Chi-square statistic is significant at α = 0.05. EDS, excessive daytime sleepiness; PSQI, The Pittsburgh Sleep Quality Index.
Table 3.
EDS by gender among respondents with short hours of sleep per night.
| Gender | No 551(78.2%) |
Yes 154(21.8%) |
p-Value | OR | 95% CI for OR | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Female | 236 | 74.7 | 80 | 25.3 | 0.044 | 1.4 | (1.008–2.065) |
| Male | 315 | 81 | 74 | 19 | |||
Table 4.
EDS by gender for each age group among respondents with short hours of sleep/night.
| Age | Gender | No EDS | EDS | p-Value | OR | 95% CI for OR | ||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| ⩽29 | Female | 43 | 62.3 | 26 | 37.7 | 0.026* | 2.1 | (1.088–4.170) |
| Male | 81 | 77.9 | 23 | 22.1 | ||||
| 30–39 | Female | 30 | 78.9 | 8 | 21.1 | 0.696 | 1.2 | (0.489–2.916) |
| Male | 112 | 81.8 | 25 | 18.2 | ||||
| 40–49 | Female | 32 | 76.2 | 10 | 23.8 | 0.509 | 1.4 | (0.544–3.408) |
| Male | 61 | 81.3 | 14 | 18.7 | ||||
| 50–59 | Female | 40 | 72.7 | 15 | 27.3 | 0.155 | 2.1 | (0.743–6.081) |
| Male | 34 | 85 | 6 | 15 | ||||
| 60–69 | Female | 61 | 82.4 | 13 | 17.6 | 0.636 | 0.7 | (0.171–2.946) |
| Male | 10 | 76.9 | 3 | 23.1 | ||||
| ⩾70 | Female | 25 | 80.6 | 6 | 19.4 | 0.462 | 0.6 | (0.093–3.878) |
| Male | 5 | 71.4 | 2 | 28.6 | ||||
denote significant p-value.
4. Results
A total of 2095 surveys were completed from a total of 2250. The age range was 18–100 years, with a mean age of 42.3 ± 15.5 years, and 59.3% males. Table 1 shows other demographic data. ESS scores ranged from 0 to 24, with a mean of 7.2 ± 4.3 (SD). The ESS was reliable with Cronbach’s alpha of 0.79%. Among the 2095 respondents, EDS was present in 20.5% (95% confidence interval [CI]: 18.75–22.21%). Table 1 shows sample characteristics in relation to EDS. Results show that the presence of EDS was equal for both sexes (22.2% in females vs. 19.5% in males, p-value = 0.136). The age-specific prevalence of EDS was similar in various age groups: 22.6% (ages ⩽ 29 years), 17.9% (ages 30–39 years), 21.6% (ages 40–49 years), 20.1% (ages 50–59 years), 20.9% (ages 60–69 years), and 18.6% (ages ⩾ 70 years). The EDS was not related to marital status or occupation (p-value > 0.05).
Table 2 presents the respondents’ clinical and sleep disruption in relation to EDS. The percent of EDS was significantly higher than the percent of non-EDS among respondents with asthma (20.7% EDS vs. 16.3% non-EDS, p-value = 0.031). The percent of EDS was higher than the percent of non-EDS among respondents who do snore (41.6% EDS vs. 35.0% non-EDS, p-value = 0.012). Among respondents with poor quality of sleep as per the PSQI, the percent of EDS was significantly higher than the percent of non-EDS (88.3% EDS vs. 82.0% non-EDS, p-value = 0.002). Among those who had difficulty falling asleep, the EDS was significantly higher than non-EDS (73.0% EDS vs. 67.6% non-EDS, p-value = 0.034). The percent of EDS in respondents with frequent nighttime awakenings was higher than the percent of non-EDS (73.2% EDS vs. 66.7% non-EDS, p-value = 0.011). The percent of EDS and non-EDS differed in respondents that reported feeling tired during the day (82.3% EDS vs. 74.7% non-EDS, p-value = 0.001) and in respondents that reported sleep loss affected their mood (61.1% EDS vs. 50.7% non-EDS, p-value 0.001). The EDS was not related to coffee or tea consumption, diabetes, depression, hypertension, or waking up too early (p-values > 0.05). The bivariate analyses found that the percent of EDS and non-EDS was similar in those who reported short (<6) hours of sleep per night (35.9% EDS vs. 33.3% non-EDS, p-value = 0.302).
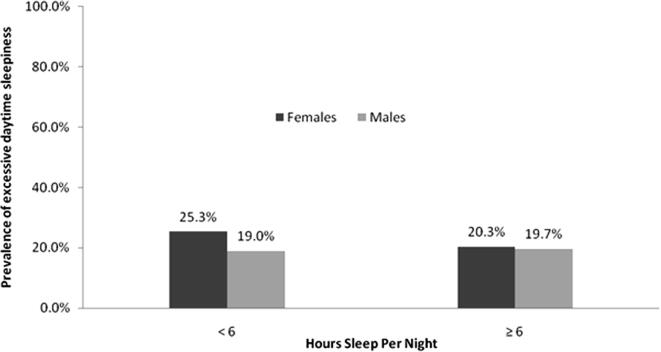
After adjustments for potential confounders, such as gender and short hours of sleep per night, Mantel–Haenszel test showed that female respondents were 1.4 times more likely than male respondents to have EDS (adjusted odds ratio [aOR] = 1.4; confidence interval [CI] = 1.008–2.065) (Table 3). Fig. 1 shows the effects of gender on EDS among respondents who reported short hours of sleep per night. Furthermore, the EDS among females was significantly higher than males (25.3% vs. 19%, p-value = 0.044).
Fig. 1.
EDS and gender by hours of sleep per night.
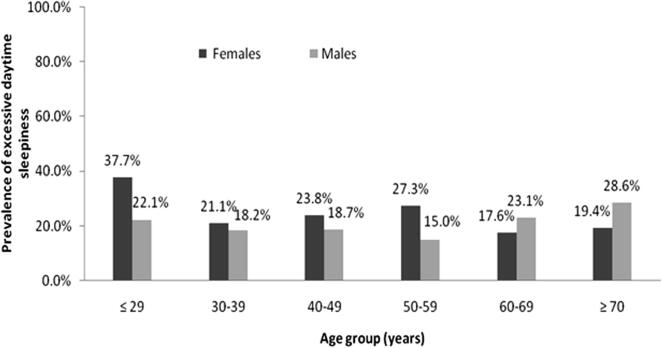
Additionally, the effects of age, gender, and short hours of sleep per night jointly were examined. Considering respondents with short hours of sleep, the reported EDS for males and females within each age group is shown in Table 4. According to the results, young females (ages ⩽ 29 years) had higher EDS than young males (37.7% vs. 22.1%, p-value = 0.026). Furthermore, in respondents with short hours of sleep per night, females were twice more likely to have EDS compared with young males (aOR 2.1; 95% CI = 1.088–4.170). However, the prevalence of EDS for males and females was similar within middle-aged (ages 30–59 years) and the elderly groups (ages ⩾ 70 - years). Fig. 2 demonstrates the effect of female and young age group on EDS among respondents with short hours of sleep per night.
Fig. 2.
EDS by gender for each age group among respondents with short hours of sleep/night.
5. Discussion
This study discussed EDS and its relationship to gender, age groups, and hours of sleep per night among a sample of Saudi Arabian adult population. No similar study has estimated gender, age, and hours of sleep per night in relationship to EDS in the Saudi general population. In this sample, EDS (ESS > 10) is present in 20.5% of participants (95% CI: 18.75–22.21%). Although this may appear as a high prevalence, it is comparable with other reported studies from other countries. Pahwa et al. reported prevalence of 20.8% among the rural Canadian population [28], 19.8% among the north Irish population [29], 17.8% among the Swedish population [31], and 45% among US Hispanics [33]. However, it is much higher than other reported studies [4,12,15,37,38].
There are conflicting reports regarding the prevalence of EDS in relationship to gender. This study did not show a statistically significant difference in EDS among males (19.5%) and females (22.2%), p-value = 0.136. This is similar to the studies reported by Pahwa et al. among the Canadian population [28], among the Australian adult population [27], and the American population, as reported by Bixler et al. [39]. However, these studies neglected to assess the joint effect of gender and hours of sleep per night on EDS. Other studies reported more EDS among males compared with females [40,41]; however, many other studies reported more EDS among females than males [38,42–44].
Also similar to the Australian study [2], this study shows that the prevalence of EDS does not vary significantly across various age groups or hours of sleep per night. Vashum et al. noted that the prevalence of EDS was roughly equivalent among various age groups [2]. A major limitation of these studies is that the relationship between EDS and gender was not described by age groups or hours of sleep per night. Importantly, gender differences in EDS were observed when respondents with short hours of sleep per night (less than 6 h) were considered. Furthermore, the major differences appeared between males and females in the young age group and in respondents with short hours of sleep per night. The results show the EDS was more common among young Saudi females than young Saudi males (aOR = 2.1). It is likely that this finding is related to lifestyle, physical activity, and health behavior of both genders; however, this study was not designed in particular to study these factors. Future epidemiological studies are needed to investigate the roles of lifestyle, physical activity, and health behavior in relation to EDS among the young age group. The stratified analysis found that the EDS in this population did not increase significantly in middle-aged or elderly male respondents with short hours of sleep per night. Similar to the study by Pahwa et al. [28], the present study did not show any significant association with hypertension. Also, the present study did not find any association between smoking and EDS, similar when compared with the Australian study [27]. This study has a few major limitations. One is that the ESS reported in this study is subjective and depends on self-reporting by the participant, creating the possibility of over- or under-reporting the symptoms, including other associated factors. Secondly, it is a cross-sectional study and was not designed to examine the cause of EDS; therefore, no inference can be made regarding causality, such as insomnia, sleep apnea, sleep patterns, or other parasomnias. No objective measurement was used, such as MSLT. The final major limitation of this study was that it utilized a convenient sample that may not be representative of the Saudi population. Despite these limitations, it is the first study to assess EDS among Saudis. Also, self-reported data about sleep have been shown to be comparable with laboratory data [45]. A major advantage of this study compared with other studies is that the association of EDS and sleep quality as measured by the PSQI was examined, which showed that the patients with EDS have poor sleep quality, and it also assesses the daytime effect of EDS. In addition, this study investigated the roles of some confounding factors that lead to gender differences in the risk of EDS.
6. Conclusions
The present study did not observe any gender differences in the risk of EDS. However, this study described the prevalence of EDS by gender with respect to short hours of sleep and young age group. An argument was developed through this study that EDS could vary significantly by gender when considering short hours of sleep per night, which has not been fully addressed in previous studies. The study revealed that EDS was not affected by various age groups. Nonetheless, the prevalence of EDS was significantly higher in young Saudi females than young Saudi males in respondents with short hours of sleep per night.
Acknowledgements
The authors extend their deep and sincere appreciation to King Abdullah International Medical Research Center and King Abdulaziz City for Science and Technology (KACST) for funding the study.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jegh.2015.05.005.
Conflict of interest
None declared.
References
- [1].Slater G, Steier J. Excessive daytime sleepiness in sleep disorders. J Thorac Dis. 2012 Dec;4(6):608–16. doi: 10.3978/j.issn.2072-1439.2012.10.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Vashum KP, McEvoy MA, Hancock SJ, Islam MR, Peel R, Attia JR, et al. Prevalence of and associations with excessive daytime sleepiness in an Australian older population. Asia Pac J Public Health. 2013 Oct 4; doi: 10.1177/1010539513497783. [DOI] [PubMed] [Google Scholar]
- [3].Gjevre JA, Pahwa P, Karunanayake C, Hagel L, Rennie D, Lawson J, et al. Excessive daytime sleepiness among rural residents in Saskatchewan. Can Respir J. 2014 Jul-Aug;21(4):227–33. doi: 10.1155/2014/921541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gunes Z, Sahbaz M, Tugrul E, Gunes H. Prevalence and risk factors for excessive daytime of sleepiness in rural western Anatolia (Turkey): the role of obesity and metabolic syndrome. Southeast Asian J Trop Med Public Health. 2012 May;43(3):747–55. [PubMed] [Google Scholar]
- [5].Bonnet MH, Arand DL. We are chronically sleep deprived. Sleep. 1995 Dec;18(10):908–11. doi: 10.1093/sleep/18.10.908. [DOI] [PubMed] [Google Scholar]
- [6].Lopes JM, Dantas FG, Medeiros JL. Excessive daytime sleepiness in the elderly: association with cardiovascular risk, obesity and depression. Rev Bras Epidemiol. 2013 Dec;16(4):872–9. doi: 10.1590/s1415-790x2013000400007. [DOI] [PubMed] [Google Scholar]
- [7].Bourjeily G, El Sabbagh R, Sawan P, Raker C, Wang C, Hott B, et al. Epworth sleepiness scale scores and adverse pregnancy outcomes. Sleep Breath. 2013 Feb 19; doi: 10.1007/s11325-013-0820-9. [DOI] [PubMed] [Google Scholar]
- [8].Blachier M, Dauvilliers Y, Jaussent I, Helmer C, Ritchie K, Jouven X, et al. Excessive daytime sleepiness and vascular events: the three city study. Ann Neurol. 2012 May;71(5):661–7. doi: 10.1002/ana.22656. [DOI] [PubMed] [Google Scholar]
- [9].Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, Mayes SD, Tsaoussoglou M, Rodriguez-Munoz A, et al. Learning, attention/hyperactivity, and conduct problems as sequelae of excessive daytime sleepiness in a general population study of young children. Sleep. 2012 May;35(5):627–32. doi: 10.5665/sleep.1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chasens ER, Korytkowski M, Sereika SM, Burke LE. Effect of poor sleep quality and excessive daytime sleepiness on factors associated with diabetes self-management. Diab Educ. 2013 Jan-Feb;39(1):74–82. doi: 10.1177/0145721712467683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Grimm W, Hildebrandt O, Nell C, Koehler U. Excessive daytime sleepiness and central sleep apnea in patients with stable heart failure. Int J Cardiol. 2014 Aug 17; doi: 10.1016/j.ijcard.2014.08.069. [DOI] [PubMed] [Google Scholar]
- [12].Lee CH, Ng WY, Hau W, Ho HH, Tai BC, Chan MY, et al. Excessive daytime sleepiness is associated with longer culprit lesion and adverse outcomes in patients with coronary artery disease. J Clin Sleep Med. 2013;9(12):1267–72. doi: 10.5664/jcsm.3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Singh R, Undevia NS, Schuman C, Attarian H. Excessive daytime sleepiness among attending physicians: a pilot survey study at an academic institution. Sleep Med. 2011 Sep;12(8):808–10. doi: 10.1016/j.sleep.2011.04.003. [DOI] [PubMed] [Google Scholar]
- [14].Wu S, Wang R, Ma X, Zhao Y, Yan X, He J. Excessive daytime sleepiness assessed by the Epworth Sleepiness Scale and its association with health related quality of life: a population-based study in China. BMC Public Health. 2012;12:849. doi: 10.1186/1471-2458-12-849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Johns M, Hocking B. Daytime sleepiness and sleep habits of Australian workers. Sleep. 1997 Oct;20(10):844–9. doi: 10.1093/sleep/20.10.844. [DOI] [PubMed] [Google Scholar]
- [16].Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991 Dec;14(6):540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- [17].Johns MW. Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep. 1994 Dec;17(8):703–10. doi: 10.1093/sleep/17.8.703. [DOI] [PubMed] [Google Scholar]
- [18].Castiglioni P, Lombardi C, Di Rienzo M, Lugaresi E, Montagna P, Cortelli P, et al. What are the causes of excessive daytime sleepiness in patients with sleep-disordered breathing? Eur Respir J. 2008 Aug;32(2):526–7. doi: 10.1183/09031936.00043308. [DOI] [PubMed] [Google Scholar]
- [19].Gerhardstein R, Day R, Rosenthal L. Narcolepsy and other causes of excessive daytime sleepiness. Respir Care Clin N Am. 1999 Sep;5(3):427–46. [viii-ix] [PubMed] [Google Scholar]
- [20].Mignot E. Excessive daytime sleepiness: population and etiology versus nosology. Sleep Med Rev. 2008 Apr;12(2):87–94. doi: 10.1016/j.smrv.2007.12.006. [DOI] [PubMed] [Google Scholar]
- [21].Cleator J, Abbott J, Judd P, Wilding JP, Sutton CJ. Correlations between night eating, sleep quality, and excessive daytime sleepiness in a severely obese UK population. Sleep Med. 2013 Nov;14(11):1151–6. doi: 10.1016/j.sleep.2013.04.026. [DOI] [PubMed] [Google Scholar]
- [22].Wali SO, Krayem AB, Samman YS, Mirdad S, Alshimemeri AA, Almobaireek A. Sleep disorders in Saudi health care workers. Ann Saudi Med. 1999 Sep-Oct;19(5):406–9. doi: 10.5144/0256-4947.1999.406. [DOI] [PubMed] [Google Scholar]
- [23].Aloe F, Pedroso A, Tavares SM. Epworth Sleepiness Scale outcome in 616 Brazilian medical students. Arq Neuropsiquiatr. 1997 Jun;55(2):220–6. doi: 10.1590/s0004-282x1997000200009. [DOI] [PubMed] [Google Scholar]
- [24].Haddock CK, Poston WS, Jitnarin N, Jahnke SA. Excessive daytime sleepiness in firefighters in the central United States. J Occup Environ Med. 2013 Apr;55(4):416–23. doi: 10.1097/jom.0b013e31827cbb0b. [DOI] [PubMed] [Google Scholar]
- [25].Liu X, Uchiyama M, Kim K, Okawa M, Shibui K, Kudo Y, et al. Sleep loss and daytime sleepiness in the general adult population of Japan. Psychiatry Res. 2000 Feb 14;93(1):1–11. doi: 10.1016/s0165-1781(99)00119-5. [DOI] [PubMed] [Google Scholar]
- [26].Joo S, Shin C, Kim J, Yi H, Ahn Y, Park M, et al. Prevalence and correlates of excessive daytime sleepiness in high school students in Korea. Psychiatry Clin Neurosci. 2005 Aug;59(4):433–40. doi: 10.1111/j.1440-1819.2005.01396.x. [DOI] [PubMed] [Google Scholar]
- [27].Hayley AC, Williams LJ, Kennedy GA, Berk M, Brennan SL, Pasco JA. Prevalence of excessive daytime sleepiness in a sample of the Australian adult population. Sleep Med. 2014 Mar;15(3):348–54. doi: 10.1016/j.sleep.2013.11.783. [DOI] [PubMed] [Google Scholar]
- [28].Pahwa P, Karunanayake CP, Hagel L, Gjevre JA, Rennie D, Lawson J, et al. Prevalence of high Epworth Sleepiness Scale scores in a rural population. Can Respir J. 2012 Mar-Apr;19(2):e10–4. doi: 10.1155/2012/287309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Nugent AM, Gleadhill I, McCrum E, Patterson CC, Evans A, MacMahon J. Sleep complaints and risk factors for excessive daytime sleepiness in adult males in Northern Ireland. J Sleep Res. 2001 Mar;10(1):69–74. doi: 10.1046/j.1365-2869.2001.00226.x. [DOI] [PubMed] [Google Scholar]
- [30].Kaneita Y, Ohida T, Uchiyama M, Takemura S, Kawahara K, Yokoyama E, et al. Excessive daytime sleepiness among the Japanese general population. J Epidemiol. 2005 Jan;15(1):1–8. doi: 10.2188/jea.15.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Abstracts of the 18th Congress of the European Sleep Research Society, 12–16 September 2006, Innsbruck, Austria. J Sleep Res. 2006 Sep;15(Suppl. 1):1–253. doi: 10.1111/j.1365-2869.2006.00540_1.x. [DOI] [PubMed] [Google Scholar]
- [32].Ohayon MM, Caulet M, Philip P, Guilleminault C, Priest RG. How sleep and mental disorders are related to complaints of daytime sleepiness. Arch Intern Med. 1997 Dec 8–22;157(22):2645–52. [PubMed] [Google Scholar]
- [33].Shafazand S, Wallace DM, Vargas SS, Del Toro Y, Dib S, Abreu AR, et al. Sleep disordered breathing, insomnia symptoms, and sleep quality in a clinical cohort of U.S. Hispanics in south Florida. J Clin Sleep Med. 2012 Oct 15;8(5):507–14. doi: 10.5664/jcsm.2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Al-Jahdali H. Prevalence of sleep apnea and excessive day time sleepiness in patients with end-stage renal disease on dialysis. Saudi J Kidney Dis Transpl. 2012 Mar;23(2):251–61. [PubMed] [Google Scholar]
- [35].Ahmed AE, Fatani A, Al-Harbi A, Al-Shimemeri A, Ali YZ, et al. Validation of the arabic version of the Epworth Sleepiness Scale. J Epidemiol Global Health. 2014 doi: 10.1016/j.jegh.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989 May;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- [37].Joo S, Baik I, Yi H, Jung K, Kim J, Shin C. Prevalence of excessive daytime sleepiness and associated factors in the adult population of Korea. Sleep Med. 2009 Feb;10(2):182–8. doi: 10.1016/j.sleep.2008.03.017. [DOI] [PubMed] [Google Scholar]
- [38].Tsuno N, Jaussent I, Dauvilliers Y, Touchon J, Ritchie K, Besset A. Determinants of excessive daytime sleepiness in a French community-dwelling elderly population. J Sleep Res. 2007 Dec;16(4):364–71. doi: 10.1111/j.1365-2869.2007.00606.x. [DOI] [PubMed] [Google Scholar]
- [39].Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A. Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab. 2005 Aug;90(8):4510–5. doi: 10.1210/jc.2005-0035. [DOI] [PubMed] [Google Scholar]
- [40].Yukawa K, Inoue Y, Yagyu H, Hasegawa T, Komada Y, Namba K, et al. Gender differences in the clinical characteristics among Japanese patients with obstructive sleep apnea syndrome. Chest. 2009 Feb;135(2):337–43. doi: 10.1378/chest.08-1414. [DOI] [PubMed] [Google Scholar]
- [41].Pallesen S, Nordhus IH, Omvik S, Sivertsen B, Tell GS, Bjorvatn B. Prevalence and risk factors of subjective sleepiness in the general adult population. Sleep. 2007 May;30(5):619–24. doi: 10.1093/sleep/30.5.619. [DOI] [PubMed] [Google Scholar]
- [42].Basta M, Lin HM, Pejovic S, Sarrigiannidis A, Bixler E, Vgontzas AN. Lack of regular exercise, depression, and degree of apnea are predictors of excessive daytime sleepiness in patients with sleep apnea: sex differences. J Clin Sleep Med. 2008 Feb 15;4(1):19–25. doi: 10.1016/j.sleep.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Hublin C, Kaprio J, Partinen M, Heikkila K, Koskenvuo M. Daytime sleepiness in an adult, Finnish population. J Intern Med. 1996 May;239(5):417–23. doi: 10.1046/j.1365-2796.1996.475826000.x. [DOI] [PubMed] [Google Scholar]
- [44].Doi Y, Minowa M. Gender differences in excessive daytime sleepiness among Japanese workers. Soc Sci Med. 2003 Feb;56(4):883–94. doi: 10.1016/s0277-9536(02)00089-8. [DOI] [PubMed] [Google Scholar]
- [45].Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992 Aug;15(4):376–81. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jegh.2015.05.005.