Abstract
This study aimed to investigate the phenomenology of obsessive–compulsive disorder (OCD), addressing specific questions about the nature of obsessions and compulsions, and to contribute to the World Health Organization’s (WHO) revision of OCD diagnostic guidelines. Data from 1001 patients from the Brazilian Research Consortium on Obsessive–Compulsive Spectrum Disorders were used. Patients were evaluated by trained clinicians using validated instruments, including the Dimensional Yalee Brown Obsessive–Compulsive Scale, the University of Sao Paulo Sensory Phenomena Scale, and the Brown Assessment of Beliefs Scale. The aims were to compare the types of sensory phenomena (SP, subjective experiences that precede or accompany compulsions) in OCD patients with and without tic disorders and to determine the frequency of mental compulsions, the co-occurrence of obsessions and compulsions, and the range of insight. SP were common in the whole sample, but patients with tic disorders were more likely to have physical sensations and urges only. Mental compulsions occurred in the majority of OCD patients. It was extremely rare for OCD patients to have obsessions without compulsions. A wide range of insight into OCD beliefs was observed, with a small subset presenting no insight. The data generated from this large sample will help practicing clinicians appreciate the full range of OCD symptoms and confirm prior studies in smaller samples the degree to which insight varies. These findings also support specific revisions to the WHO’s diagnostic guidelines for OCD, such as describing sensory phenomena, mental compulsions and level of insight, so that the world-wide recognition of this disabling disorder is increased.
Keywords: Obsessive–compulsive disorder, Phenomenology, Sensory phenomena, Mental compulsions, Insight
1. Background
The World Health Organization is revising the International Classification of Diseases (ICD). The current version (ICD-10) was approved in 1990. The goal is to enhance scientific validity, clinical utility and global applicability of the diagnostic guidelines (Gureje and Reed, 2012). In that spirit, an international group reviewed guidelines for obsessive–compulsive disorder (OCD) (Simpson et al., 2013), raising questions about how obsessions and compulsions are defined and whether there are valid ways to subtype OCD to facilitate diagnosis, advance pathophysiological studies, and/or help guide treatment planning. To address these questions, we investigated the clinical phenomenology of 1001 patients with OCD from the Brazilian Research Consortium on Obsessive–Compulsive Spectrum Disorders (CTOC). The goal was to refine the clinical phenotype of OCD and determine whether revisions to ICD-10 diagnostic guidelines for OCD are supported by new phenomenological evidence.
How obsessions are defined is central to the clinical recognition of OCD. In ICD-10, obsessions are defined as “ideas, images, or impulses” that enter the individual’s mind again and again. In 2013, DSM-5(2000) replaced the word “impulse” with the word “urge,” primarily to differentiate OCD from impulse control disorders (Leckman et al., 2010). In parallel, a growing literature indicates that OCD patients have sensory phenomena (SP), including urges, defined as physical experiences that precede or accompany compulsions (Ferrão et al., 2012; Miguel et al., 1997). In addition to urges, SP include physical sensations, needing to perform a behavior until it feels “just right,” feelings of incompleteness, and need for energy release (Prado et al., 2008). Initially, SP were thought to be most characteristic of OCD patients with Tourette’s Syndrome (TS) or chronic tic disorder (CTD) (Diniz et al., 2006). However, SP also occur in OCD patients without comorbid tic disorders (Ferrão et al., 2012; Gomes de Alvarenga et al., 2012; Miguel et al., 1997, 2000), especially those with early onset OCD (de Mathis et al., 2009; Rosario-Campos et al., 2001). Together, these findings suggest that the definition of obsessions should be expanded to include SP. Determining the frequency and severity of different types of SP in OCD patients with and without tic disorders would help to address this question.
How compulsions are defined is also important. In ICD-10, compulsions are defined as “stereotyped behaviors that are repeated again and again.” Yet, a study conducted in the United States (U.S.) found that mental compulsions are also common (Foa et al., 1995). As a result, mental compulsions are described in both DSM-IV and DSM-5. In contrast, mental compulsions are not mentioned in ICD-10. Determining the prevalence of mental compulsions in large clinical samples would inform whether ICD-11 guidelines for compulsions should be expanded to include mental compulsions.
Finally, different subtypes for OCD have been proposed (see Simpson and Reddy, in press, for a review). ICD-10 recommends that OCD patients be categorized into those with predominantly obsessional thoughts, predominantly compulsive acts, or a mixed form. The clinical utility of this categorization is unclear: one U.S. study found that most OCD patients have both obsessions and compulsions (Foa et al., 1995). In contrast, DSM categorizes OCD patients based on their degree of insight into their OCD beliefs. Based on data from U.S. studies that insight varies in OCD patients (Foa et al., 1995; Phillips et al., 2012), a dimensional specifier was introduced in DSM-5 (i.e., excellent/good, fair, poor, absent). The rationale was primarily clinical: to ensure that OCD patients with poor/absent insight are not diagnosed as having a psychotic disorder and treated with antipsychotic monotherapy (Leckman et al., 2010). ICD-10 guidelines do not emphasize insight. Data from international studies on the degree of insight in OCD patients are needed.
The CTOC provides a unique dataset in which to investigate these issues. This consortium collected data on OCD patients from seven outpatient clinics across Brazil from 2003 to 2009. Patients were evaluated by trained raters with structured diagnostic interviews and validated clinical measures, including two innovative measures (the Dimensional Yale–Brown Obsessive–Compulsive Scale (D-YBOCS) and Universidade de São Paulo Sensory Phenomena Scale (USP-SP)). Using this database, we asked four questions:1) what types of SP occur in OCD patients with and without tic disorders; 2) how common are mental compulsions; 3) how often do obsessions and compulsions co-occur; and 4) what is the degree of insight in this clinical sample of OCD patients. We also explored whether insight varied with age, age of OCD onset, severity of OCD symptoms, severity of specific OCD symptom dimensions, or current medication status.
2. Methods
2.1. Overview
CTOC methods have been described (Miguel et al., 2008). In brief, patients seeking treatment at participating centers were eligible if they met DSM-IV criteria for OCD as their principal psychiatric diagnosis, were willing to participate in the research, and provided informed consent. Socio-demographic features and medical and family psychiatric history were collected, and patients underwent structured psychiatric evaluation (Structured Clinical Interview for DSM-IV Axis-I Disorders-SCID-I; additional modules for tic and impulse control disorders; the Kiddie Schedule for Affective Disorders and Schizophrenia-K-SADS sections for attention deficit hyperactivity disorder (ADHD) and separation anxiety disorder), and evaluations using validated instruments, including: the Yale–Brown Obsessive–Compulsive Scale (Y-BOCS) and DY-BOCS (for OCD symptoms and severity); the Yale Global Tic Severity Scale (YGTSS), the USP-SPS (for sensory phenomena); and the Brown Assessment of Beliefs Scale (BABS; for insight).
Each patient’s evaluation lasted about 5 h. Interviews were conducted by psychiatrists or Master level clinicians experienced in OCD. Data were sent to a central data core. Data quality procedures included twice yearly in-person meetings of interviewers from the seven sites and on-line as-needed meetings to clarify data registry. A restricted access website (http://protoc.incubadora.fapesp.br/portal/ctoc/) stored assessment instruments, videos for interview training and inter-rater reliability assessments. A description of all measures, training for reliability and data management is available at Miguel et al. (2008).
2.2. Sample
The sample was comprised of 1001 patients. Half were in treatment at the CTOC centers at the time they participated. The rest came from the community or other mental health services. Demographic and clinical features of this sample are shown in Table 1. Only 4 (0.4%) subjects presented hoarding as the sole symptom dimension, and this was the least severe among all dimensions for the whole sample.
Table 1.
Demographic and clinical characteristics of the sample.
| Characteristic | Total |
|---|---|
| Age in years, mean (SD) | 34.85 (12.99) |
| Age range, in years | 9–82 |
| Younger than 18, No. (%) | 46 (4.6%) |
| Age of onset of OCD symptoms in years, mean (SD)a | 12.56 (7.28) |
| Age range of onset of OCD symptoms in years | 3–54 |
| Age of onset of interference due to OCD symptoms, mean (SD) | 21.76 (10.63) |
| Female, No. (%) | 569 (56.8) |
| Race, No. (%) | |
| White | 832 (83.1) |
| Black/African | 39 (3.9) |
| Asian | 13 (1.3) |
| Mixed (white/black) | 115 (11.5) |
| Other | 2 (0.2) |
| Education in years, mean (SD)b | 14.57 (4.97) |
| Marital Status, No. (%) | |
| Single | 544 (54.3) |
| Married-Partnered (e.g., living together) | 377 (37.7) |
| Divorced-Separated | 66 (6.6) |
| Widowed | 14 (1.4) |
| Employment Status, No. (%) | |
| Working outside the home | 433 (43.3) |
| Retired | 108 (10.8) |
| Student | 179(17.9) |
| Unemployed | 154 (15.4) |
| Working inside the home | 104 (10.4) |
| Other | 23 (2.3) |
| Y-BOCS, mean (SD) | |
| Obsessions | 12.68 (3.94) |
| Compulsions | 12.83 (4.14) |
| Total score | 25.51 (7.51) |
| DY-BOCS, mean (SD) | |
| Aggression | 5.29 (4.98) |
| Sexual, religious | 4.30 (4.90) |
| Symmetryc | 7.34 (4.64) |
| Contamination | 6.22 (5.15) |
| Hoarding | 3.15 (4.08) |
| Miscellaneous | 7.54 (4.70) |
| Total global | 21.15 (6.26) |
| USP-SPS, mean (SD) | 4.88 (4.63) |
| Brown Assessment of Beliefs Scale, mean (SD)d | 6.85 (5.46) |
| Beck Depression Inventory, mean (SD) | 16.50 (11.54) |
| Beck Anxiety Inventory, mean (SD) | 16.02 (11.64) |
| Treatment, No. (%) | |
| Current Medicatione | 563 (56.2) |
| Any history of psychotherapy | 643 (64.2) |
| Comorbid psychiatric disorder, No. (%) | |
| Lifetime | 921 (92.1) |
| Currentf | 837 (83.6) |
| Any mood disorder | 426 (42.6) |
| Any anxiety disorder | 651 (65.0) |
| Any impulse control disorder | 308 (30.8) |
| Any somatoform disorder | 167 (16.7) |
| Attention Deficit Hyperactive Disorder | 127 (12.7) |
| Any eating disorder | 71 (7.1) |
| Any substance or alcohol disorder | 67 (6.7) |
SD = standard deviation; YBOCS = Yale–Brown Obsessive–Compulsive Scale; DY-BOCS = Dimensional Yale–Brown Obsessive–Compulsive Scale; BABS = Brown Assessment of Beliefs Scale; USP-SPS = University of Sao Paulo Sensory Phenomena Scale.
Age of onset of first OCD symptom, may not correspond to the age of onset of distress/interference due to OCD symptoms.
1 (0.01%) missing.
2 (0.02%) missing.
32 (3.2%) missing. All measures are current, unless otherwise specified.
Current medication status includes 397 (39.7%) subjects on selective serotonin reuptake inhibitors, 102 (10.2%) on clomipramine, 27 (2.7%) on selective serotonin and noradrenaline reuptake inhibitors, which could be used in combination with antipsychotics, benzodiazepines and mood stabilizers.
The most frequent current comorbidities, excluding tic disorders, were (%): Generalized Anxiety Disorder (33.8); Major Depressive Disorder (33.2); Social Phobia (32.0); Specific Phobia (30.8); Skin-Picking (15.4); Attention Deficit Hyperactive Disorder (12.7); Dysthimia (11.2); Body Dysmorphic Disorder (11.1) and Post-traumatic Stress Disorder (9.9).
2.3. Assessments
2.3.1. Diagnosis of OCD and tic disorders
The SCID-I (First et al., 2002) was used to determine the presence of Axis I psychiatric diagnoses, including OCD. Tic disorders were also diagnosed according to DSM-IV criteria. CTD was diagnosed when a patient had (a) either vocal or motor tics, (b) tics occurred several times a day, for at least 1 year, without a symptom-free interval longer than 3 months, (c) were time consuming, caused significant distress or functional impairment, (d) started before age 18, (e) were not secondary to substance use or a general medical condition and (f) never met criteria for TS. TS was diagnosed when a patient had (a) both motor and vocal tics at some point, plus (b)–(e) criteria for CTD.
2.3.2. Clinical phenomenology
The Y-BOCS (Goodman et al., 1989) was used to assess severity of obsessions and compulsions by means of 10 questions, 5 addressing obsessions and 5 addressing compulsions in relation to amount of time spent with symptoms, interference, distress, resistance and control over symptoms. Individual scores range from 0 to 4 (total score 0–40), the higher score meaning greater severity.
The DY-BOCS (Rosario-Campos et al., 2006) was used to evaluate OCD symptoms according to six dimensions: (1) aggression, (2) sexual/religious, (3) symmetry/ordering/arranging, (4) contamination/cleaning, (5) hoarding and (6) miscellaneous. Obsessions, avoidant behaviors, mental and behavioral compulsions are investigated within each dimension. Individual dimension scores range from 0 to 15. A global score ranging from 0 to 30 addresses time (0–5), distress (0–5), interference (0–5) and impairment (0–15) in the past week, the higher score meaning greater severity.
The USP-SPS (Rosario et al., 2009) evaluated the presence and severity of SP. It is a semi-structured scale with two parts. The first assesses the occurrence of different types of SP and their respective age at onset. The second measures the severity of current and past SP. For each SP, severity is measured by three ordinal scales with six anchor points that focus on the frequency (0–5), amount of distress (0–5) and interference with functioning (0–5), making a severity score for each type of SP range from 0 to 15. For the present analyses only current scores were used. Types of SP include: 1) Physical sensations (tactile and/or muscle-joint), defined as uncomfortable sensations localized in a specific region of the body (skin, muscles, or joints), which precede or occur along with repetitive behaviors; 2) “Just right” perceptions, triggered by tactile, visual, or auditory sensations, including the need for things to feel, look or sound “just right”; 3) Feelings of incompleteness (i.e., inner feeling or perception of discomfort that makes the patient do things indefinitely, or until feeling ‘complete’); 4) Energy release (i.e., generalized inner tension or energy that builds up and needs to be released by an action) and 5) Urge only (i.e., “have to do it” perception related to the repetitive behavior).
The BABS (Eisen et al., 1998) evaluates six aspects of insight in the past week: conviction, perception of others’ views of the belief, fixity of the belief, attempts to disprove it, whether the individual recognizes a psychiatric/psychological cause for the belief, and the presence of ideas of reference. The score ranges from 0 to 24; higher scores correspond to poorer insight. BABS scores have been categorized into excellent (0–3), good (4–7), fair (8–12), poor (13–17 or ≥ 18 + score < 4 in the conviction question, where 4 = 100% conviction), or absent (≥18 score 4 in the conviction question) (Phillips et al., 2012).
2.4. Analyses
Statistical analyses were performed using the SPSS18. The OCD + TS, OCD + CTD and OCD without tics groups were compared using the Kruskal–Wallis Test for continuous variables (current age, age at OCD onset, Y-BOCS, DY-BOCS and USP-SPS scores) and the Chi-square test for categorical variables (sex, proportion of different SP). Post-hoc analyses were performed with the nonparametric relative contrast effects test for the continuous variables and Chi-square tests for the categorical variables with the Bonferroni correction.
Descriptive analyses were performed for the distribution of BABS scores and the distribution of the Y-BOCS subscores of distress associated with obsessions and compulsions. Mann–Whitney and Wilcoxon Tests were employed to investigate the relationship between current medication status and global BABS scores. The Spearman test was used to investigate the correlation between the global BABS score and: (1) current age, (2) age at OCD onset, (4) Y-BOCS scores, (5) DY-BOCS scores and (6) duration of illness. Statistical significance was set at 0.05.
3. Results
3.1. Q1: What SP occur in OCD with and without tic disorders?
Ninety OCD patients (9.0%) met DSM-IV lifetime criteria for TS, 154 (15.4%) met criteria for CTD, and 757 (75.6%) had no tic disorder. There were no significant differences between these groups regarding age (mean (SD): OCD + TS = 32.01 (12.26); OCD + CTD = 33.27 (12.51); OCD without tics = 35.5 (13.12), p = 0.073), age at OCD onset (mean (SD):OCD + TS 11.06 (5.88); OCD + CTD = 11.93 (7.65); OCD without tics = 12.86 (7.33), p = 0.072), or OCD severity (mean Y-BOCS (SD):OCD + TS = 25.74 (7.89); OCD + CTD = 26.12 (7.70); OCD without tics = 25.35 (7.43), p = 0.739). There was a difference in the proportion of males (OCD + TS = 49%; OCD + CTD = 52%; OCD without tics 41%, p = 0.019 [overall chi square], with post-hoc tests finding OCD + CTD patients significantly more likely to be male than OCD patients without tics).
The types of SP endorsed by OCD + TS, OCD + CTD OCD without tics are shown in and Table 2. Most OCD patients endorsed SP (60.4%), but there was a significant difference between groups (p-value < 0.001), with post-hoc tests finding that OCD + TS and OCD + CTD endorsed SP significantly more frequently than OCD patients without tics. Significant differences also existed between groups in the proportion endorsing physical sensations (p-value < 0.001) and urge only (p-value = 0.021); post-hoc tests revealed that OCD + TS or OCD + CTD endorsed both significantly more often than OCD patients without tics. The global severity of SP was higher in the OCD + TS [mean (SD) = 6.90 (4.55)] and OCD + CTD groups [mean (SD) = 5.02 (4.22)] than in the OCD without tics group [mean (SD) = 4.61 (4.66)] (p < 0.001); post-hoc tests revealed that the severity of SP was significantly higher in the OCD + TS than in the OCD + CTD and OCD without tics groups.
Table 2.
Types of sensory phenomena in OCD patients with Tourette’s Syndrome, OCD patients with chronic tic disorder and OCD patients without tics.
| Sensory phenomena | OCD + TS | OCD + CTD | OCD | p-Value* |
|---|---|---|---|---|
| N = 90 | N = 154 | N = 757 | ||
| Any Sensory Phenomena, N (%) | 76 (84.4)A | 117 (76.0)A | 457 (60.4)B | <0.001 |
| Physical sensations, N (%) | 58 (64.4)A | s78 (50.6)A | 232 (30.6)B | <0.001 |
| Just-right sensations, N (%) | 63 (70.0) | 94 (61.0) | 362 (47.8) | 0.654 |
| Feelings of incompleteness, N (%) | 19(21.1) | 36 (23.4) | 117 (15.5) | 0.504 |
| Energy release, N (%) | 23 (25.6) | 31 (20.1) | 84(11.1) | 0.133 |
| Urge only, N (%) | 38 (42.2)A | 48 (31.2)A | 154 (20.3)B | 0.021 |
Abbreviations: OCD = Obsessive–Compulsive disorder; TS = Tourette’s Syndrome; CTD = chronic tic disorder.
Chi-square test;
post-hoc tests with Bonferroni correction: (A different from B in post-hoc tests).
3.2. Q2: How common are mental compulsions?
Five hundred and sixty-eight patients (56.7%) endorsed mental compulsions. All patients with mental compulsions endorsed behavioral compulsions. Mental compulsions were most common for the symmetry/ordering/arranging [n = 282 (28.2%); e.g., organizing objects mentally; checking list of tasks mentally], aggression [n = 270 (27.0%); e.g., thinking “good” thoughts to remove “bad” (aggressive) thoughts], and the sexual/religious dimensions [n = 247 (24.7%); e.g., thinking good thoughts after the thoughts that offended God; saying prayers repeatedly to relieve distress caused by sexual thoughts], and less common for the contamination [n = 166 (16.6%); e.g., imagining washing hands when washing impossible in real life] and miscellaneous dimensions [n = 132 (13.2%); e.g., checking mentally for body signals]. Mental compulsions were least common for the hoarding dimension [n = 83(8.3%); e.g., imagining accumulating objects].
3.3. Q3: How frequently do obsessions and compulsions co-occur?
According to the DY-BOCS, 991 (99%) patients endorsed both obsessions and compulsions. Five (0.5%) patients had obsessions only and five (0.5%) patients had compulsions only; all of the latter endorsed SP preceding their compulsions, including just-right perceptions (n = 3), energy release (n = 3), urge only (n = 3), and incompleteness (n = 1). Most patients stated that their obsessions were associated with at least moderate distress (proportion endorsing distress: none 1.6%, mild 6.9%, moderate 25.5%, severe 48.3%, incapacitating 17.8%). Most also reported that they would feel at least moderate distress if they could not do their compulsions (proportion endorsing distress: none 1.7%, mild 10%, moderate 19.6%, severe 46.3%, incapacitating 22%).
3.4. Q4: What is the degree of insight in OCD patients seeking treatment?
The degree of insight varied across the sample, as shown in Fig. 1. Based on prior methods for categorizing insight (Phillips et al., 2012), 31% of the sample had excellent (score 0–3), 25% good (score 4–7), 26% fair (score 8–12), 11% poor (score 13–17 or >18 + score 0–3 in the conviction question), and 3% absent insight (score > 18 + score 4 in the conviction question). Using the BABS item that assesses the degree to which a patient is convinced their OCD belief is true, a similar distribution was observed: 28% were completely convinced their beliefs were not true, 17% thought their beliefs were probably not true; 20% thought the beliefs could or could not be true; 16% were very convinced the beliefs were true; and 16% were completely convinced that the beliefs were true. The median total BABS scores did not significantly differ between those currently receiving medication (n = 563) and those not receiving medication (n = 438; Mann–Whitney Test, p-value = 0.797; Wilcoxon Test (Fig. 2)). Of those on medication, 88.6% were receiving either clomipramine or a selective serotonin reuptake inhibitor.
Fig. 1.
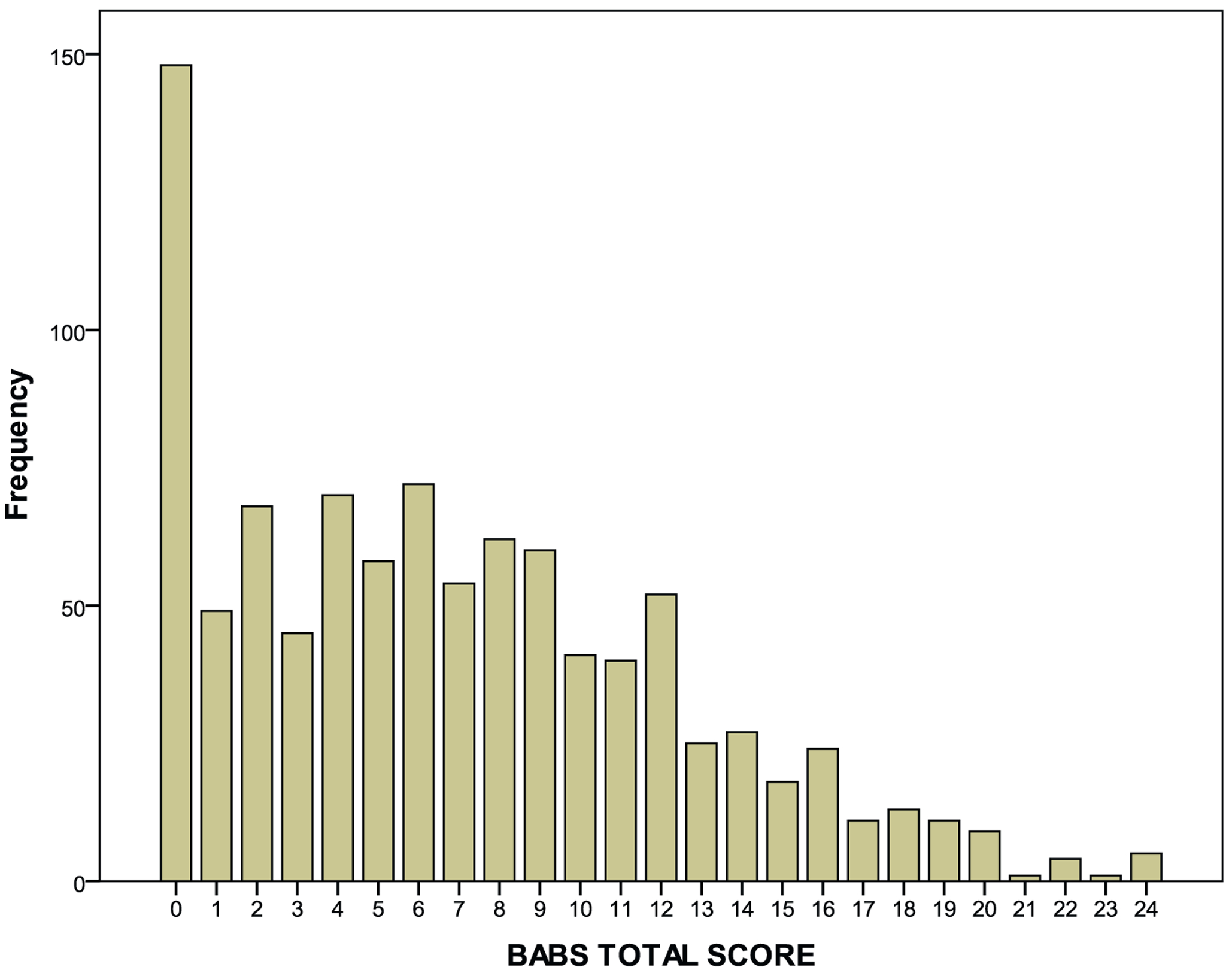
Distribution of total Brown Assessment of Beliefs Scale (BABS) scores.1
1Missing data correspond to 3.3% of the sample (n=33).
Fig. 2.
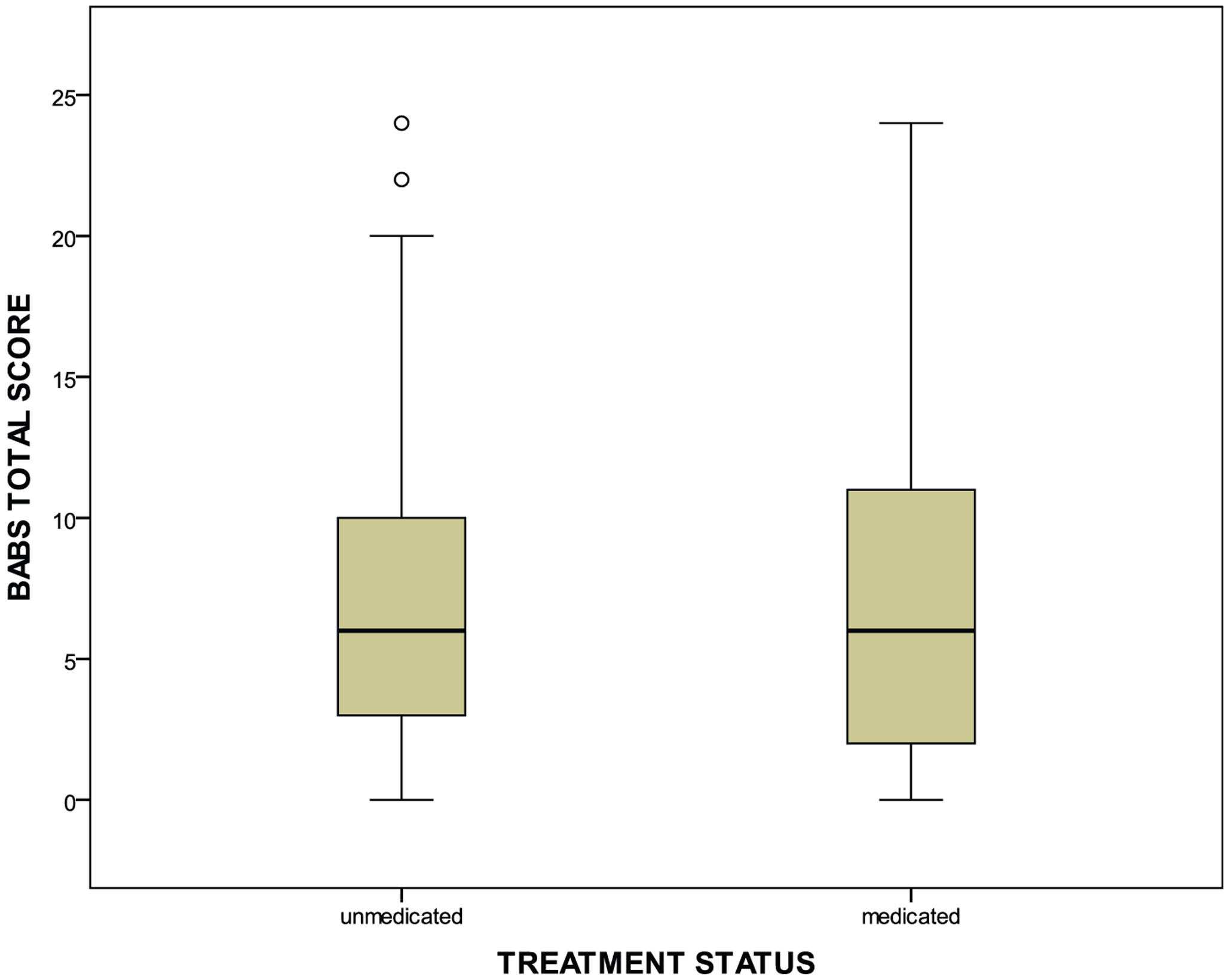
Distribution of total Brown Assessment of Beliefs Scale (BABS) scores in relation to medication status.a
aWilcoxon test (non-parametric). The median of the total BABS score of the whole sample was used as the reference for the comparison of each group with the whole sample. The two circles refer to outliers.
Poorer insight was correlated with: earlier age at OCD onset (rho = −0.076, p-value = 0.020), greater OCD severity (rho = 0.295, p-value < 0.001), greater severity of individual symptom dimensions (aggression: rho = 0.089, p-value = 0.006; sexual/religious: rho = 0.096, p-value = 0.003; symmetry: rho = 0.153, p < 0.001; contamination: rho 0.177, p-value < 0.001; hoarding: rho =0.156, p-value < 0.001; miscellaneous: rho = 0.192, p-value = 0.001) and longer duration of illness (rho = 0.11, p-value = 0.001). Insight was also analyzed as a dichotomous variable. Compared to patients with excellent + good insight (56% of the sample), patients with fair + poor + no insight (40%) presented higher scores in all symptom dimensions (analyses not shown).
4. Discussion
We used data from 1001 patients with OCD to address questions about the clinical phenotype of OCD that are relevant to the recognition of OCD by practicing clinicians and to how the WHO might revise OCD diagnostic guidelines for ICD-11. In this large OCD sample, SP were common despite the comorbidity with tics. However, patients with tic disorders were more likely to have SP that consisted of physical sensations and urge only. Mental compulsions occurred in the majority of the sample, and the occurrence of obsessions in the absence of compulsions was extremely rare. Finally, patients in this sample had a wide range of insight into the rationality of their OCD beliefs, with a small subset presenting no insight. These findings confirm and extend prior studies and support revisions to the WHO’s OCD guidelines.
Historically, obsessions have been defined as thoughts, images, or impulses that are intrusive and distressing. However, “sensory phenomena” (including physical sensations, “just right” perceptions, feelings of incompleteness, need for energy release, and urges) (Rosario et al., 2009) have also been described in OCD patients (Leckman et al., 1994; Miguel et al., 2000). Most recently, Ferrão et al. (2012) reported that 65% of OCD patients in this Brazilian sample had at least one type of SP preceding their compulsions. In another study of 813 patients from this same consortium (Gomes de Alvarenga et al., 2012), OCD patients with tics had a higher rate of SP than OCD patients without tics (80% versus 67%), but the rate of SP was very high in both groups. To contribute to this literature, we investigated for the first time whether the specific types of SP differed according to comorbidity with tics, and found that OCD patients with TS or CTD were significantly more likely to have physical sensations and urge only than OCD patients without tics. At the same time, 20% of OCD patients without tics also reported urges preceding their compulsions, and the most common type of SP in all groups were the “just right” sensations. The severity of SP was greatest in OCD + TS patients, adding to evidence for a continuum between OCD + TS, OCD + CTD and OCD without tics (Diniz et al., 2006), which could correspond to varying degrees of overlapping neural circuits involved in their pathophysiology (Marsh et al., 2009). Overall, these data do not show that the type of SP differentiates OCD patients with and without tics, consistent with a prior study (Leckman et al., 1994). On the other hand, from the clinical practice perspective, these data do support describing SP in OCD diagnostic guidelines, since they are common, could be an important target of treatment, and should trigger an evaluation for tic disorders in the patient and family members. Despite the lack of specific controlled trials, we would expect SP to be successfully managed in the psychological treatment of OCD in a similar way to tic disorders, by adding to exposure and response prevention the components of habit reversal training, such as awareness and competing response training (McGuire et al., 2014).
The majority of the sample endorsed mental compulsions. In a field trial for DSM-IV that evaluated 431 OCD patients in the U.S.,79.5% had mental compulsions, as measured by the Y-BOCS checklist (Foa et al., 1995). That we found a lower rate (56.7%) could be due to the fact that we used the DY-BOCS, which asks about mental compulsions inside each symptom dimension. In contrast, the DSM-IV field trial added five specific items to the Y-BOCS checklist to capture mental compulsions (i.e., special words, images or numbers re-created mentally; special prayers repeated in a set manner; mental counting, mental list-making; and mental reviewing). Regardless, both studies demonstrate that mental compulsions are common and that they almost always occur alongside behavioral compulsions: none in our study and only 0.2% in the DSM-IV field trial had mental compulsions without behavioral compulsions. These data support describing mental compulsions in WHO diagnostic guidelines for OCD. Once recognized, mental compulsions also constitute important treatment targets.
Our data confirm that obsessions without compulsions or vice-versa are rare in OCD patients seeking treatment. In our study, 99% of patients endorsed both obsessions and compulsions: only 0.5% had only obsessions and 0.5% had only compulsions. Moreover, of the five patients endorsing only compulsions, all reported sensory phenomena preceding the compulsions. Likewise, in the DSM-IV field trial (Foa et al., 1995), 96% of patients had both obsessions and compulsions, only 2% had predominantly obsessions and only 2% had predominantly compulsions. Together, these data demonstrate that the patient who reports only obsessions or compulsions warrants further investigation to determine whether mental compulsions or SP are present (supporting OCD diagnosis) or whether the diagnosis of OCD should be reconsidered. These data also support the practice of using the co-occurrence of obsessions and compulsions to differentiate OCD from other disorders with repetitive thoughts (e.g., worries of generalized anxiety disorder, ruminations of major depressive disorder) or repetitive behaviors (e.g., trichotillomania, skin-picking). Whether the underlying brain mechanisms (e.g., of obsessions versus compulsions and of obsessions versus ruminations) are also differentiated remains an important area of study.
Although our data confirm that obsessions and compulsions usually co-occur in OCD, they cannot resolve the direction of the relationship: whether obsessions trigger compulsions as some OCD models assert (Salkovskis, 1985, 1999) or compulsive behaviors lead to obsessions as others assert (Robbins et al., 2012). Given this uncertainty, we support the proposed plan for ICD-11 (Simpson et al., 2013), which is to describe the strong relationship between these symptoms but to use language that does not presume a direction of causality.
Our data confirm and extend prior findings that insight varies in OCD. Consistent with the DSM-IV field trial (Foa et al., 1995) and prior studies in smaller samples (Phillips et al., 2012), we found that about half of OCD patients had good or excellent insight, about one-third had fair to poor insight, and a small subset had no insight. Interestingly, the distribution of insight did not differ between those on or off medication. Degree of insight was also not associated with age. However, the majority of patients in this sample were adults (range 9–82, with only 25% aged 25 or younger); other studies have found that children with OCD often exhibit poor insight (Storch et al., 2008).
Insight was weakly correlated in our sample with both earlier age of OCD onset and duration of the illness, consistent with some prior studies (Ravi Kishore et al., 2004). Different from previous studies (Alonso et al., 2008; Shimshoni et al., 2011), but consistent with others (Catapano et al., 2010; Eisen et al., 2001) we observed a positive correlation between lower levels of insight and higher OCD severity. This finding raises the question if the degree of insight should be considered an additional indicator of severity rather than a specifier. On the other hand, an insight specifier may have clinical utility if it increased awareness about how insight varies in this disorder (e.g., so that OCD patients with poor/absent insight are not erroneously diagnosed with a primary psychotic disorder and prescribed antipsychotic monotherapy). An insight specifier might also prove useful in treatment planning. Although insight improves alongside OCD symptoms with successful treatment (Eisen et al., 2001), poor insight patients are underrepresented in clinical trials because they are less likely to seek or adhere to treatment (Santana et al., 2013). Thus, patients with poor insight may need help to engage with treatment. Yet, the ability of clinicians across diverse settings and in different cultures to reliably use such an insight specifier is unknown. The global applicability of the concept of insight needs more study.
Several study limitations are worth noting. First, evaluations occurred only at one point in time. Second, 75% of the sample was 25 or older, making our findings most relevant to adult patients. Third, data about current treatment status was limited: medication doses and length of treatment were not recorded, and there was no information on whether patients received cognitive-behavioral therapy. Fourth, patients were recruited at tertiary services specialized in OCD, and may present higher severity compared to other clinical and epidemiological populations. Fifth, some variables (e.g., age at OCD onset, past psychiatric symptoms, prior pharmacological treatments) were assessed retrospectively and subject to recall bias. Sixth, despite the clinical importance of avoidant behaviors in OCD, their frequency and correlates were not captured by the assessment instruments used. Reports on the frequency of avoidance and the socio-demographical and clinical factors associated with its occurrence (including the diverse OCD symptom dimensions) are urgently needed to obtain a more complete phenomenological picture of the disorder. Finally, the high level of education of the sample may limit the generalization of the results to the broad OCD population and the worldwide applicability of these findings needs additional study.
In summary, the new data generated from this very large sample of OCD patients indicates that the clinical phenotype of OCD can be further refined and supports the revision of the WHO’s diagnostic guidelines for OCD. Specifically, the data support broadening the conceptualization of obsessions, to include sensory phenomena, and of compulsions, to include mental compulsions. As obsessions and compulsions co-occurred in 99% of this sample, the clinical utility of subtyping OCD by those with predominant obsessions or compulsions is not supported. Finally, insight in this treatment-seeking sample of OCD patients varied from excellent to absent, supporting reconsideration of the boundary between OCD and psychotic disorders in diagnostic guidelines.
Acknowledgments
We thank the members of the Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders who participated in the process of data collection: Aline S. Sampaio, Amanda Galvão de Almeida, Ana Gabriela Hounie, Ana Teresa A. Ramos-Cerqueira, Andréa L. Raffin, Angélica P. Lopes, Anna Guerra Toniolo, Aristides Volpato Cordioli, Antonio Carlos Lopes, Armando Rezende, Carina C. D’Alcante, Carolina Valério, Christina H. Gonzales, Cristina Belotto da Silva, Cristiana Machado, Daisy Pontual, Daniela Braga, Dante Marino Malavazzi, Elenita Domingues, Eduardo Alliende Perin, Elisabeth Meyer da Silva, Érica Vasques Trench Helen Copque, Fernanda Pasquotto de Souza, Helena Bins, Helena Silva Prado, Ilduara Sidrim, Ivanil Aparecido de Morais, Juliana Oliveira, Kátia Niederauer, Kátia Petribú, Lucas Lovato, Luciana Gropo, Luis Evandro Lima Filho, Marcelo Basso, Marcelo Camargo Batistuzzo, Maria Eugenia de Mathis, Marinês Alves Joaquim, Manuela C. Borges, Melissa Chagas Assunção, Moacir Pires, Pedro Alvarenga, Patrícia Veloso, Priscila Chacon, Priscylla Jennie Rabelo, Ricardo Cezar Torresan, Rosana Savio Mastrorosa, Samantha Nunes Santos, Sandro Iego, Sonia Borcato, Tatiane Cristina Ribeiro.
We thank the support from the New York State Office of Mental Hygiene and faculty and staff from the Anxiety Disorders Clinic at the New York State Psychiatric Institute, who provided comments on an earlier draft of the manuscript.
Role of the funding source
The following funding sources supported the research reported in this manuscript:
1. Fundação de Amparo à Pesquisa do Estado de São Paulo (Sao Paulo State Research Support Agency)
Grants #
1999/12205-7
2005/55628-8
2011/21357-9
2011/51485-9
2. Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ, National Brazilian Council for Scientific and Technological Development)
Grant # 420122/2005-2
3. New York State Office of Mental Hygiene
4. National Institute of Mental Health, grant #K24MH09155
Footnotes
Conflicts of interest in the last 36 months
Dr. Shavitt has received travel grants from Lundbeck S.A. to participate in the European College of Neuropsycopharmacology Meeting and International College of Obsessive–Compulsive Disorders Meeting in October/2012 and October/2013 and receives research grants from Fundação de Amparo à Pesquisa do Estado de Sao Paulo (FAPESP, State agency, #2011/51485–9) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ, Federal agency, #307742/2012–1). Dr. De Mathis receives a research grant from Fundação de Amparo à Pesquisa do Estado de Sao Paulo (FAPESP, #2013/04203–3). Dr. Ferrão has received honoraria as a speaker for GSK, Pfizer and Abbott. Dr. Fontenelle receives grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ, # 303846/2008–9), Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ, State Agency, E-26/ 103.252/2011) and Instituto D’Or de Pesquisa e Ensino (private agency). Dr. Diniz receives a research grant from Fundação de Amparo à Pesquisa do Estado de Sao Paulo (FAPESP, state agency, #2011/00968–0). Dr. Costa receives a research grant from Fundação de Amparo à Pesquisa do Estado de Sao Paulo (FAPESP, state agency, de Amparo a #2012/14070–8). Dr. Rosario has received honoraria as speaker and part of the advisory board for Novartis and Shire. Dr. Hoexter receives a research grant from Fundação de Amparo à Pesquisa do Estado de Sao Paulo (FAPESP, state agency, #2013/16864–4). Dr. Miguel receives research grants from Fundação de Amparo à Pesquisa do Estado de Sao Paulo (FAPESP, #2011/21357–9) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ, #573974/2008–0). Dr. Simpson has received research funds for clinical trials from Janssen Pharmaceuticals (2006–2012), Transcept Pharmaceuticals (2011–2013), has consulted for Quintiles, Inc. (September, 2012), and receives royalties from Cambridge University Press and UpToDate, Inc. Dr. Simpson’s work on this project was supported by the National Institute of Mental Health grant #K24MH09155 and by the New York State Office of Mental Hygiene. All other authors declare that they have no conflicts of interest.
References
- Alonso P, Menchón JM, Segalàs C, Jaurrieta N, Jiménez-Murcia S, Cardoner N, et al. Clinical implications of insight assessment in Obsessive–Compulsive disorder. Compr Psychiatry 2008;49:305–12. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5). 5th ed Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Catapano F, Perris F, Fabrazzo M, Cioffi V, Giacco D, De Santis V, et al. Obsessive–Compulsive disorder with poor insight: a three-year prospective study. Prog Neuropsychopharmacol Biol Psychiatry 2010;34:323–30. [DOI] [PubMed] [Google Scholar]
- de Mathis MA, Diniz JB, Shavitt RG, Torres AR, Ferrão YA, Fossaluza V, et al. Early onset Obsessive–Compulsive disorder with and without tics. CNS Spectr 2009;14:362–70. [DOI] [PubMed] [Google Scholar]
- Diniz JB, Rosario-Campos MC, Hounie AG, Curi M, Shavitt RG, Lopes AC, et al. Chronic tics and Tourette syndrome in patients with Obsessive–Compulsive disorder. J Psychiatr Res 2006;40:487–93. [DOI] [PubMed] [Google Scholar]
- Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, Rasmussen SA. The brown assessment of beliefs scale: reliability and validity. Am J Psychiatry 1998;155:102–8. [DOI] [PubMed] [Google Scholar]
- Eisen JL, Rasmussen SA, Phillips KA, Price LH, Davidson J, Lydiard RB, et al. Insight and treatment outcome in Obsessive–Compulsive disorder. Compr Psychiatry 2001;42:494–7. [DOI] [PubMed] [Google Scholar]
- Ferrão YA, Shavitt RG, Prado H, Fontenelle LF, Malavazzi DM, de Mathis MA, et al. Sensory phenomena associated with repetitive behaviors in Obsessive–Compulsive disorder: an exploratory study of 1001 patients. Psychiatry Res 2012;197:253–8. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P). New York: Biometrics Research: New York State Psychiatric Institute; 2002. [Google Scholar]
- Foa EB, Kozak MJ, Goodman WK, Hollander E, Jenike MA, Rasmussen SA. DSM-IV field trial: Obsessive–Compulsive disorder. Am J Psychiatry 1995;152:90–6. [DOI] [PubMed] [Google Scholar]
- Gomes de Alvarenga P, de Mathis MA, Dominguez Alves AC, do Rosário MC, Fossaluza V, Hounie AG, et al. Clinical features of tic-related Obsessive–Compulsive disorder: results from a large multicenter study. CNS Spectr 2012;17:87–93. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale–Brown obsessive compulsive scale. I. Development, use, and reliability. Arch Gen Psychiatry 1989;46:1006–11. [DOI] [PubMed] [Google Scholar]
- Gureje O, Reed G. Revising the classifications of mental disorders: do we really need to bother? Int Rev Psychiatry 2012;24:511–3. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Denys D, Simpson HB, Mataix-Cols D, Hollander E, Saxena S, et al. Obsessive–Compulsive disorder: a review of the diagnostic criteria and possible subtypes and dimensional specifiers for DSM-V. Depress Anxiety 2010;27:507–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leckman JF, Grice DE, Barr LC, de Vries AL, Martin C, Cohen DJ, et al. Tic-related vs. non-tic-related obsessive compulsive disorder. Anxiety 1994;1:208–15. [PubMed] [Google Scholar]
- Marsh R, Maia TV, Peterson BS. Functional disturbances within frontostriatal circuits across multiple childhood psychopathologies. Am J Psychiatry 2009;166:664–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire JF, Piacentini J, Brennan EA, Lewin AB, Murphy TK, Small BJ, et al. A meta-analysis of behavior therapy for Tourette Syndrome. J Psychiatr Res 2014;50: 106–12. [DOI] [PubMed] [Google Scholar]
- Miguel EC, Baer L, Coffey BJ, Rauch SL, Savage CR, O’Sullivan RL, et al. Phenomenological differences appearing with repetitive behaviours in Obsessive–Compulsive disorder and Gilles de la Tourette’s syndrome. Br J Psychiatry 1997;170:140–5. [DOI] [PubMed] [Google Scholar]
- Miguel EC, do Rosário-Campos MC, Prado HS, do Valle R, Rauch SL, Coffey BJ, et al. Sensory phenomena in Obsessive–Compulsive disorder and Tourette’s disorder. J Clin Psychiatry 2000;61:150–6. quiz 157. [DOI] [PubMed] [Google Scholar]
- Miguel EC, Ferrão YA, Rosário MC, Mathis MA, Torres AR, Fontenelle LF, et al. The Brazilian Research Consortium on Obsessive–Compulsive Spectrum Disorders: recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Rev Bras Psiquiatr 2008;30:185–96. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Pinto A, Hart AS, Coles ME, Eisen JL, Menard W, et al. A comparison of insight in body dysmorphic disorder and Obsessive–Compulsive disorder. J Psychiatr Res 2012;46:1293–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prado HS, Rosário MC, Lee J, Hounie AG, Shavitt RG, Miguel EC. Sensory phenomena in Obsessive–Compulsive disorder and tic disorders: a review of the literature. CNS Spectr 2008;13:425–32. [DOI] [PubMed] [Google Scholar]
- Ravi Kishore V, Samar R, Janardhan Reddy YC, Chandrasekhar CR, Thennarasu K. Clinical characteristics and treatment response in poor and good insight Obsessive–Compulsive disorder. Eur Psychiatry 2004;19:202–8. [DOI] [PubMed] [Google Scholar]
- Robbins TW, Gillan CM, Smith DG, de Wit S, Ersche KD. Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends Cogn Sci 2012;16:81–91. [DOI] [PubMed] [Google Scholar]
- Rosario MC, Prado HS, Borcato S, Diniz JB, Shavitt RG, Hounie AG, et al. Validation of the University of São Paulo Sensory Phenomena Scale: initial psychometric properties. CNS Spectr 2009;14:315–23. [DOI] [PubMed] [Google Scholar]
- Rosario-Campos MC, Leckman JF, Mercadante MT, Shavitt RG, Prado HS, Sada P, et al. Adults with early-onset Obsessive–Compulsive disorder. Am J Psychiatry 2001;158:1899–903. [DOI] [PubMed] [Google Scholar]
- Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, Findley D, et al. The Dimensional Yale–Brown Obsessive–Compulsive Scale (DY-BOCS): an instrument for assessing Obsessive–Compulsive symptom dimensions. Mol Psychiatry 2006;11:495–504. [DOI] [PubMed] [Google Scholar]
- Salkovskis PM. Obsessional-compulsive problems: a cognitive-behavioural analysis. Behav Res Ther 1985;23:571–83. [DOI] [PubMed] [Google Scholar]
- Salkovskis PM. Understanding and treating Obsessive–Compulsive disorder. BehavRes Ther 1999;37(Suppl. 1):S29–52. [PubMed] [Google Scholar]
- Santana L, Fontenelle JM, Yücel M, Fontenelle LF. Rates and correlates of non-adherence to treatment in Obsessive–Compulsive disorder. J Psychiatr Pract 2013;19:42–53. [DOI] [PubMed] [Google Scholar]
- Shimshoni Y, Reuven O, Dar R, Hermesh H. Insight in Obsessive–Compulsive disorder: a comparative study of insight measures in an Israeli clinical sample. J Behav Ther Exp Psychiatry 2011;42:389–96. [DOI] [PubMed] [Google Scholar]
- Simpson HB, Reddy J. Obsessive–Compulsive disorder for ICD-11: proposed revisions to the diagnostic guidelines. Rev Bras Psiquiatr [in press]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Milsom VA, Merlo LJ, Larson M, Geffken GR, Jacob ML, et al. Insight in pediatric Obsessive–Compulsive disorder: associations with clinical presentation. Psychiatry Res 2008;160:212–20. [DOI] [PubMed] [Google Scholar]


