Abstract
Purpose: Familial Mediterranean fever (FMF) is the most common monogenic auto-inflammatory disease characterized by recurrent attacks of fever and serositis. It is associated with mutation in pyrin inflammasome leading to interleukin-1 (IL-1) over secretion. Although colchicine is the first line treatment in FMF, 5–10% of patients are reported in literature as non-responders. Colchicine is not always well-tolerated due either to its direct toxicity or to co-morbidities that preclude the administration of its proper dosage. For these patients an alternative or additional treatment to colchicine is necessary. This literature review reports the published data regarding the use of IL-1 inhibitors in Familial Mediterranean Fever.
Results: There is no uniform definition of colchicine resistance, but the different studies of treatment with IL-1 inhibitors provide evidence of IL-1 pathogenic role in colchicine-resistant FMF. IL-1 inhibition is an efficacious option for controlling and preventing flares –at least at the short term- in FMF patients who are insufficiently controlled with colchicine alone. Although canakinumab is the only approved drug in Europe for colchicine resistant FMF treatment, experience with anakinra is also substantial. In the absence of comparative studies both treatments seem to be an equal option for the management of these patients. Overall the safety profile of IL-1 inhibitors seems not different in FMF patients than in the other diseases and can be considered as globally safe. The main side effects are local injection site reactions and infections.
Conclusion: IL-1 inhibitors have the potential to improve patient outcome even in FMF patients with co-morbidities or severe complications in whom inflammation control is difficult to achieve with colchicine alone. Nevertheless, current data are limited and further evaluation of long-term efficacy and safety of IL-1 inhibitors are necessary, in order to provide robust evidence in this domain.
Keywords: familial mediterranean fever, anakinra, canakinumab, interleukine-1, colchicine, autoinflammation, amyloidosis
Key Messages
There is no uniform definition of colchicine resistance. A standardized evaluation of adherence to colchicine treatment is mandatory before considering IL-1 inhibitors in FMF patients
Although canakinumab is the only drug approved in Europe for the treatment of colchicine resistant FMF, experience with anakinra is more substantial in the literature.
There are no comparative effectiveness assessment studies for canakinumab vs. anakinra. Both treatments seem to be an option for the management of colchicine resistant or intolerant FMF patients.
The use of anakinra in pre-attack prodromal period (“on-demand treatment”) may be a reasonable approach for alleviating symptoms of an impending attack in patients with insufficient response to the maximum tolerated dosage of colchicine and low risk of amyloidosis.
The use of IL1 inhibitors as a maintenance therapy in patients unresponsive or intolerant to colchicine is globally safe and effective.
Introduction
Familial Mediterranean fever (FMF) is the most frequent monogenic auto-inflammatory disease. FMF is characterized by self-limited episodes fever associated to polyserositis and raised inflammatory markers (1). The disease is mostly seen among particular ethnic groups such as patients with a Middle Eastern ancestry or originating from the Mediterranean basin (2). Autosomal recessive mutations in the MEFV gene are responsible for the symptoms in FMF (3, 4). Although its pathogenesis is not fully understood, pyrin is a crucial player in the regulation of innate immunity and FMF-associated missense mutations induce an uncontrolled IL-1 release (5).
Amyloid deposition and the development of end-stage renal disease are the most severe complications of FMF. Since 1972, colchicine is the cornerstone of treatment for FMF patients. To date, only the daily intake of colchicine has proven its effectiveness on the long-term in preventing or improving inflammatory attacks, but also in decreasing the frequency of secondary amyloidosis (6–8).
Nevertheless, cases of unresponsiveness to colchicine have been reported, although this situation remains rare, probably <10 % of FMF patients (9–11). In addition, colchicine treatment is not always well-tolerated due either to direct colchicine toxicity or to co-morbidities that preclude the administration of the proper colchicine dosage. For these patients an alternative or additional treatment to colchicine is necessary. IL-1 inhibitors are the first candidates given the involvement of IL-1 in pathophysiology of the inflammatory attacks. Four biologic drugs blocking IL-1 are currently available. Of them, anakinra, and canakinumab have been approved for clinical use in Europe, whereas the soluble decoy IL-1-receptor, rilonacept, and the human-engineered monoclonal anti-IL-1, gevokizumab, are not authorized in European countries.
However, the precise indications for initiating IL-1 blocking agents in FMF patients are still unclear and poorly codified. Given the cost of these biological agents and their potential risk of side effects (mainly infections), their use needs still to be defined.
The objective of this article is to review the current knowledge about the use of IL-1 inhibitors in FMF, with the aim of defining the indications and the place of these more recent products in the therapeutic arsenal of the disease.
Methods
Literature Search Strategy
A literature search on the use of IL-1 inhibitors and FMF was conducted from 1947 until 2019 using the Medline, Embase, and Cochrane databases using the following terms: “anakinra,” “canakinumab,” “IL-1 inhibitor,” “Interleukin 1 Receptor Antagonist Protein,” “IL-1 blockade” and “familial Mediterranean fever.” The terms were combined as both key words and MeSH terms. We excluded articles about rilonacept and gevokizumab, as both agents are not authorized in European countries.
Additional articles were retrieved by checking manually the references of the recovered articles and the “related articles” function on Pub-Med (www.pubmed.gov) were also assessed for possible inclusions. Only articles published in English or French before September 2019 have been included to this review.
Data Assessment
All four coauthors read and approved the retrieved articles. We extracted data of the selected articles using predefined scoring forms and classification tables that enabled us to analyze the published data in five different domains: 1/ indications for IL-1 inhibitors in FMF, 2/ efficacy of IL-1 inhibitors in FMF, 3/ comparison of anakinra vs. canakinumab in FMF, 4/ comparison of maintenance vs. on-demand treatment in FMF and 5/ safety of IL-1 inhibitors in FMF.
Results
Sixty one studies or case reports or series concerning 811 patients were identified: 30 case reports or case series with 5 or less patients, 29 case series or open studies with more than 5 patients and 2 randomized studies. Five hundred and seventy one patients (70.4%) originated from the Middle East, 140 (17.2%) from Europe, 99 (12.2%) from international studies or registries and 1 patient from the USA. The retrieved articles are detailed in Table 1.
Table 1.
References of the articles described in the literature review.
| Bibliography number | First author | Number of FMF patients | Number of patients treated with Anakinra | Number of patients treated with Canakinumab | Number of patients treated with both | Median age | Description of patients with AA amyloidosis |
|---|---|---|---|---|---|---|---|
| Chae et al. (12) | Chae | 1 | 1 | yes | |||
| Vitale et al. (13) | Vitale | 32 | 32 | ||||
| Vitale et al. (14) | Vitale | 6 | 6 | ||||
| Belkhir et al. (15) | Belkhir | 1 | 1 | yes | |||
| Kuijk et al. (16) | Kuijk | 1 | 1 | ||||
| Gattringer et al. (17) | Gattringer | 2 | 2 | ||||
| Roldan et al. (18) | Roldan | 1 | 1 | ||||
| Mitroulis et al. (19) | Mitroulis | 1 | 1 | ||||
| Calligaris et al. (20) | Calligaris | 1 | 1 | ||||
| Moser et al. (21) | Moser | 1 | 1 | yes | |||
| Hennig et al. (22) | Hennig | 1 | 1 | yes | |||
| Bilginer et al. (23) | Bilginer | 1 | 1 | yes | |||
| Petropoulou et al. (24) | Petropoulou | 1 | 1 | ||||
| Meinzer et al. (25) | Meinzer | 1 | 1 | ||||
| Meinzer | 5 | 5 | 12 | ||||
| Meinzer | 1 | 1 | |||||
| Ozen et al. (26) | Ozen | 5 | 5 | 16 | |||
| Alpay et al. (27) | Alpay | 1 | 1 | yes | |||
| Stankovic Stojanovic et al. (28) | Stankovic | 4 | 4 | 27 | yes | ||
| Hacihamdioglu et al. (29) | Hacihamdioglu | 1 | 1 | ||||
| Estublier et al. (30) | Estublier | 1 | 1 | ||||
| Soriano et al. (31) | Soriano | 1 | 1 | ||||
| Ter Haar et al. (32) | Ter Haar | 3 | 3 | ||||
| Celebi et al. (33) | Celebi | 1 | 1 | yes | |||
| Mercan et al. (34) | Mercan | 2 | 2 | ||||
| Brik et al. (35) | Brik | 7 | 7 | 9,5 | |||
| Başaran et al. (36) | Basaran | 4 | 4 | 17 | |||
| Basaran | 4 | 4 | 12 | ||||
| Ugurlu et al. (37) | Ugurlu (poster) | 19 | 19 | yes | |||
| Gül et al. (38) | Gül | 9 | 9 | 22 | |||
| Cetin et al. (39) | Cetin | 12 | 12 | 31 | yes | ||
| Cetin | 8 | 8 | 18 | yes | |||
| Eroglu et al. (40) | Eroglu | 5 | 5 | 13 | yes | ||
| Eroglu | 3 | 3 | 13 | ||||
| Eroglu | 6 | 6 | 13 | ||||
| Sevillano et al. (41) | Sevillano | 1 | 1 | yes | |||
| Alpa et al. (42) | Alpa | 1 | 1 | ||||
| Rossi-Semerano et al. (43) | Rossi | 10 | 10 | 21 | |||
| Rossi | 1 | 1 | 21 | ||||
| Rossi | 3 | 3 | 21 | ||||
| Özçakar et al. (44) | Ozçakar | 3 | 3 | 19 | |||
| Ozçakar | 10 | 10 | 14 | yes | |||
| Sozeri et al. (45) | Sozeri | 1 | 1 | yes | |||
| Kucuksahin et al. (46) | Kucuksahin | 24 | 24 | ||||
| Kucuksahin | 2 | 2 | 29 | yes | |||
| Laskari et al. (47) | Laskari | 9 | 9 | 23 | |||
| Laskari | 5 | 5 | 43 | ||||
| Ben-Zvi et al. (48) | Ben-Zvi | 25 | 25 | ||||
| Georgin-Lavialle et al. (49) | Georgin-Lavialle | 1 | 1 | ||||
| Abbara et al. (50) | Abbara | 1 | 1 | yes | |||
| Ozen et al. (51) | Ozen | 20 | 20 | ||||
| Ozen | 13 | 13 | |||||
| Pecher et al. (52) | Pecher | 13 | 13 | 31 | |||
| Barut et al. (53) | Barut | 16 | 4 | 12 | |||
| Trabulus et al. (54) | Trabulus | 9 | 9 | 33 | yes | ||
| De Benedetti et al. (55) | De Benedetti | 63 | 63 | ||||
| Özçakar et al. (56) | Ozçakar | 1 | 1 | yes | |||
| Ozçakar | 4 | 4 | 23 | yes | |||
| Jesenak et al. (57) | Jesenak | 1 | 1 | ||||
| Yildirim et al. (58) | Yildirim | 3 | 3 | 57 | yes | ||
| Yazilitaş et al. (59) | Yazilitas | 11 | 11 | 14 | yes | ||
| Ergezen et al. (60) | Ergezen (poster) | 48 | 48 | ||||
| Kohler et al. (61) | Köhler | 29 | 29 | yes | |||
| Köhler | 2 | 2 | yes | ||||
| Babaoglu et al. (62) | Babaoglu | 15 | 15 | 34 | |||
| Gülez et al. (63) | Gülez | 12 | 12 | 16, 5 | yes | ||
| Gülez | 3 | 3 | 10 | ||||
| Varan et al. (64) | Varan | 33 | 33 | yes | |||
| Varan | 11 | 11 | yes | ||||
| Varan et al. (65) | Varan | 10 | 10 | yes | |||
| Varan | 7 | 7 | 21 | yes | |||
| Akar et al. (66) | Akar | 133 | 133 | yes | |||
| Akar | 19 | 19 | yes | ||||
| Akar | 18 | 18 | yes | ||||
| Akar | 2 | 2 | yes | ||||
| Berdeli et al. (67) | Berdeli | 22 | 22 | 13, 8 | |||
| Hasbal et al. (68) | Hasbal | 1 | 1 | yes | |||
| Sargin et al. (69) | Sargin | 14 | 14 | 41 | |||
| Eren Akarcan et al. (70) | Eren Arkacan | 9 | 9 | 14, 3 | |||
| Kisla Ekinci et al. (71) | Kisla Ekinci | 14 | 14 | 11 | yes | ||
| Sendogan et al. (72) | Sendogan | 4 | 4 | yes | |||
| TOTAL | 811 | 496 | 234 | 81 |
Anakinra was the main IL-1 inhibitor used (n = 496, 61.2%), rarely prescribed as an “on-demand” treatment (20/496, 4.0%). Two hundred and thirty-four (28.9%) patients were treated with canakinumab and 81(10.0%) with both IL-1 inhibitors, starting in all patients except 2 with anakinra before switching to canakinumab. The Supplementary Figure represents the prescription of IL-1 inhibitors in FMF since the first description in 2006.
We were unable to identify the patients who had been described more than once in the literature: first in case reports, than in case series and/or in retrospective studies. That is the reason why we were unable to assess bias or outcome assessments.
Discussion
Indications for IL1 Inhibition in FMF Patients
Colchicine Resistance
The main indication for the prescription of IL-1 inhibitors is colchicine resistance. However, the meaning of “colchicine resistance” has evolved over the past decade, and a consensus definition remains elusive. The criteria for insufficient response to colchicine are highly variable in the different studies. In many studies, no specific criteria are given to determine whether a patient is resistant or not; the indication to treat with IL-1 inhibition is often made only on the notion of “frequent attacks” despite colchicine treatment. Other studies give a more precise definition of colchicine resistance, but again the different definitions are highly variable. The highest agreement for colchicine resistance is the persistent elevation of acute phase reactants between the attacks (12, 15–20, 23, 24, 26–29, 33, 34, 36, 38–40, 44, 46, 49, 50, 52, 55, 57–59, 61, 63–65, 73). No consensus exists about attack frequency: some authors define colchicine resistance in patients who experience more than 1 typical inflammatory attack per 3 months (38, 53), while others refer to colchicine resistance if there are more than 2 typical attacks per trimester (46) and still others if the patient has monthly attacks (35, 40, 48, 51, 52, 55, 59, 62–65). None of the studies considers that attack frequency may vary with age and therefore the probable necessity to define this parameter differently in adults and children. Some studies take also into consideration the severity of inflammatory episodes in their definition of colchicine resistance (2, 4, 5, 7–11, 17–20, 27, 28, 34, 35, 38, 40, 44, 48, 49, 52, 53, 55, 57, 58, 73) but rarely give a precise definition for this item. Only very few studies include the notions of quality of life assessment or school or work attendance (4, 7–12, 18, 19, 27, 34, 53, 61, 73) into the definition of colchicine resistance, but without defining what is tolerable as absence from work or school or quality of life.
The maximum dosage of colchicine is usually set at 2 mg/day (27, 35, 38, 46, 54, 55, 66), but may change in the different studies, especially in children where doses vary with age in whom the standard dose is sometimes defined as 1.2 mg/m2/day (53). The standard and the most accepted minimal dose before considering resistance in the literature is the “maximum tolerated dose” (74).
The last factor of lack of precision is the difficulty to determine incompliant patients since there is no reliable and practical detection method to estimate active colchicine levels. Only one study had a standardized methodology to verify colchicine compliance by counting the remaining tablets (40). However, compliance with colchicine treatment appears to be low overall (10, 75, 76), which explains why the EULAR recommendations note that lack of compliance should be considered in all patients who do not respond adequately to colchicine (54).
Colchicine Intolerance/Toxicity
Therapeutic oral doses of colchicine in patients without hepatic or renal failure have few side effects and are generally well-tolerated. The most common side-effects are gastrointestinal, including diarrhea, vomiting and nausea. Gastrointestinal toxicity is dose dependent and may improve by diminishing lactose intake (77), or lowering the colchicine dose. Rarer acute adverse effects include myopathy, rhabdomyolysis, and myelosuppression (78). A colchicine neuromyopathy may occur with chronic daily use, particularly in patients whose dose has not been appropriately adjusted for renal disease (79–81). Of note fatalities during therapeutic use have been reported only in patients with chronic renal insufficiency taking unadjusted doses of colchicine or when colchicine has been given intravenously, or combined with CYP3A4 inhibitors (82–84). Due to all these side effects, the intolerance or toxicity of colchicine is therefore a possible indication for the treatment with IL-1 inhibitors.
The main reason for starting IL-1 antagonist in the different studies was the poor digestive tolerance of colchicine (12, 27, 46–48, 85), but in the various studies it was not specified whether means to increase digestive tolerance had been implemented before considering IL-1 inhibition. The second reason for IL-1 inhibition was neuromyopathy (15, 25, 31, 42, 47, 51, 58, 62, 68), occurring exclusively in patients with a risk factor such as renal disease or drug interactions. Myelotoxicity (24, 47) and hepatotoxicity (46, 58) was responsible for the initiation of an IL-1 inhibitor only on a very ad hoc basis. From these studies it appears that the intolerance or toxicity of colchicine is only exceptionally responsible for the need to initiate IL-1 blockade. This is particularly true in children who only exceptionally display co-morbidities that may decrease colchicine tolerance.
In view of the many aspects regarding colchicine treatment, it seems essential to extensively evaluate all these domains before considering colchicine resistance or intolerance. In Table 2, we propose a checklist to help the physician to assess the FMF patient before planning alternative or additional treatment plans to colchicine.
Table 2.
Check list before considering colchicine resistance.
| □ | Verify that the diagnosis of FMF is accurate |
| □ | Verify that reported symptoms are related to inflammation (Check inflammatory markers during symptoms) |
| □ | Eliminate common causes of fever and pain (infection, leukemia, …) |
| □ | Question the patient about personal, social or psychological problems that may be triggers for inflammatory attacks - Propose behavioral approaches for stress management |
| □ | Ensure compliance at full dose for 3–6 months If the maximum dose is not reached, increase gradually the colchicine dosage by 0.5 mg (0.25 mg before the age of 5) every 3 months |
| □ | Ensure colchicine tolerance by - Dietary modifications (limit lactose intake) - Splitting the total daily dose - Associating antidiarrheal and spasmolytic agents to colchicine |
| □ | In patients with a sudden deterioration of FMF despite full compliance of colchicine, look for other causes of inflammation: - Inflammatory rheumatism, vasculitis - Mild myeloid hemopathy (in the elderly) - Chronic peritonitis or peritoneal mesothelioma (in the elderly) |
| □ | Document prospectively the attack recurrence for 3–6 months in order to confirm the number of reported inflammatory episodes |
Severe Complications or Associated Co-morbidities
Secondary amyloidosis
Amyloidosis is characterized by deposition of misfolded insoluble proteins in various organs and tissues. It is a life-threatening progressive disease unless underlying causes are treated early before irreversible organ damage occurs. AA Amyloidosis (AAA) is the most severe complication of FMF (86, 87). There is no cure for amyloidosis but it is preventable by suppression of inflammation. Hence, it is crucial to control inflammation in patient with preexisting AAA (88). As such, IL-1 inhibitors are good candidates in AAA FMF patients suffering from persistent inflammatory symptoms despite the regular use of colchicine at maximal dose.
At present, we were able to identify 160 patients who received IL-1 inhibitors for FMF and AA amyloidosis; they were mainly treated with anakinra compared to canakinumab, due to anakinra's short half-life. The exact number of FMF patients treated for AAA is not available because most series include FMF patients with and without AAA, and the details of data specific to patients with AA amyloidosis were not available, even in supplementary data.
When the data was available (n = 56), the foremost reasons for initiating an IL-1 inhibitor were in decreasing order of frequency: colchicine resistance (n = 24) (21, 22, 27, 28, 33, 39, 40, 44–46, 54, 56, 58, 72), AA amyloidosis and severe renal failure (n = 14) (12, 15, 41, 59, 71, 72), AA amyloidosis onset during the course of FMF (n = 13) (15, 23, 28, 31, 50, 72), colchicine intolerance (n = 7) (12, 15, 46, 58, 68, 72). Unfortunately, the exact reasons were not always specified in AAA patients from FMF series. Altogether, the main reason for IL-1 inhibitor prescription among patients with AAA secondary to FMF was severe kidney failure hindering the adjustment of the colchicine dosage necessary to normalize inflammatory markers. The second main reason was colchicine resistance defined by the persistence of raised inflammatory markers despite the regular daily intake of the maximum tolerated dose of colchicine, which was not always specified.
Anakinra, was mainly prescribed at 100 mg/day except for patients with end stage renal failure who received 100 mg of anakinra 3 times a week, each dialysis day. Canakinumab was mostly prescribed at 150 mg/month and was not chosen in case of end stage renal failure. Considering the recent prescription of IL-1 inhibitors in AAA secondary to FMF, there is not much hindsight to assess tolerance and efficacy in the long term but in the short term, the tolerance and efficacy seem correct. However, it is important to note that in the absence of renal failure, and if AAA reveals FMF, the treatment of choice remains colchicine (9). In case of AAA in FMF patients, colchicine should be tried first, starting at 1 or 1.5 mg/day and increased gradually in steps of 0.5 mg every 3 months during at least 6 months with a close monitoring of inflammatory markers and proteinuria, before starting IL-1 inhibitors. Indeed, in patients who are virgin of any colchicine treatment, the onset of AAA is first and foremost a sign of colchicine absence.
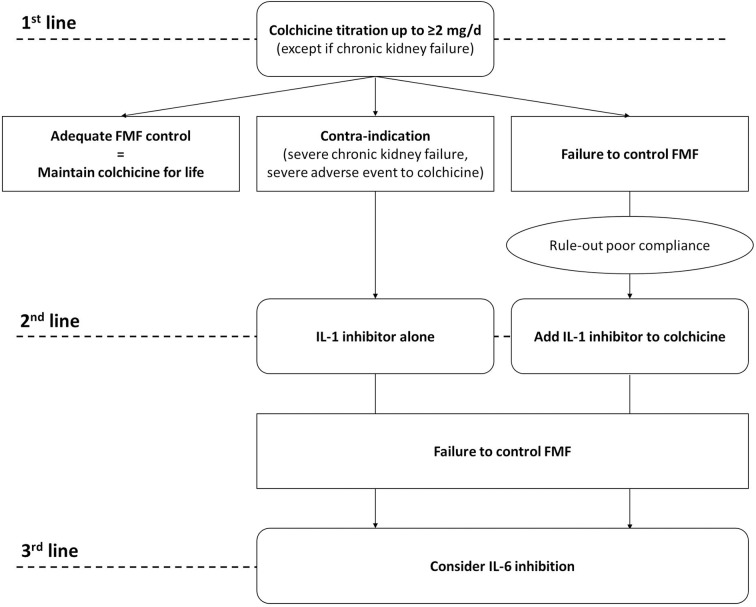
Figure 1 proposes an algorithm for the decision to initiate an IL-1 inhibitor in FMF patients with AAA.
Figure 1.
Proposal of a therapeutic algorithm for AA amyloidosis in patients with FMF.
Associated co-morbidities
Unresponsiveness to colchicine—even if taken properly—may be due to associated inflammatory diseases. Most reports concern FMF associated ankylosing spondylitis with a good response to IL-1 inhibitors (29, 40, 46, 49, 63, 64) even if older studies showed also efficacy with TNF blocking agents (89, 90).
Other inflammatory conditions associated to FMF, such as Behçet's disease (23, 40), inflammatory bowel disease (27, 28, 33, 64), protracted febrile myositis (25, 30, 34, 40, 63), hidradenitis suppurativa (50) and Henloch-Schönlein purpura (25) also responded well to IL-1 inhibitors.
Finally, IL-1 inhibitors were described to be effective among FMF children with failure to thrive (36, 45) or children with an important need of corticosteroids (70); unfortunately the inflammatory status between attacks was not specified in these children.
In the light of these studies, patients with FMF previously well-controlled with colchicine alone, need a careful assessment for inflammatory comorbidities appearing later in the course of the disease. Indeed, the therapeutic implication of distinguishing this subgroup from the “true” colchicine resistance may be major: one can hypothesize that IL-1 inhibitors may be tapered and possibly withdrawn once the associated disease is controlled.
Efficacy
To evaluate the efficacy of IL-1 inhibitors, phase 2 studies (in which the patient is his own control) and placebo-controlled studies provide the best information.
At our knowledge only one randomized, double-blind, placebo-controlled trial with anakinra in FMF patients who were colchicine resistant was published (48). In this study 25 patients were enrolled and randomized (12 in the treatment group and 13 in the placebo group). All the patients received maximum tolerated doses of colchicine during the whole study period. Seven patients discontinued the study, all of whom were from the placebo group, due to treatment failure or to side effects. Complete response was achieved in 7 patients of the treatment group whereas the 5 remaining patients had a partial response. For all the patients of the treatment group, anakinra improved furthermore life quality. In this specific study, anakinra combined to colchicine also decreased he number of joints attacks. These findings may support a role for dual therapy with colchicine especially in patients with FMF articular complications.
For canakinumab a first open-label pilot trial was conducted in 7 children who experienced at least 1 investigator-confirmed FMF attack per month (35). The median 28-day time-adjusted attack rate decreased from 2.7 to 0.3 in this study and the proportion of days that participants were experiencing an attack decreased from 24.2 to 3.6%. Furthermore, serum acute phase reactants levels normalized during the treatment period and health-related quality of life improved in all patients.
A second small open-label pilot trial with canakinumab in patients with monthly attacks, showed that monthly injections prevented attacks in 8/9 patients and reduced the frequency of attacks in the remaining patient (38). Furthermore, serum acute phase reactants levels (C-reactive protein and serum amyloid A protein) remained low throughout the treatment period in all the patients. Significant improvement was also observed in both physical and mental component scores.
These preliminary results in colchicine resistant FMF patients could be confirmed in a placebo-controlled phase 3 study with an injection every 4 weeks, in which 61% of 31 patients treated with canakinumab (150 mg or 2 mg/kg in children) vs. 6% of 32 patients in the placebo group had a complete response and did not experience any flare of the disease for 40 weeks while treated (55). This proportion increased to 71% of patients if the blinded dose in non-complete responders was increased to 300 mg (or 4 mg/kg in children) every 4 weeks. A dosing interval of every 8 weeks was enough to maintain complete disease control in 46% of patients with colchicine resistant FMF. In patients who did not have a complete control of the disease, the mean attack frequency decreased from more than 30 to <2 per year and remaining attacks seemed less severe.
Overall these studies provided evidence of the pathogenic role of IL-1 in colchicine-resistant familial Mediterranean fever. They also showed that IL-1 inhibition is an efficacious option for controlling and preventing flares –at least at the short term- in these patients.
Anakinra vs. Canakinumab
Although canakinumab is the only drug approved in Europe for the treatment of colchicine resistant FMF, in literature, experience with anakinra is also significant. Up to now, there are no comparative effectiveness assessment studies for canakinumab vs. anakinra. The preference of one treatment over the other can therefore be based only on indirect data. Significant reasons to prescribe anakinra rather than canakinumab are the price and/or reimbursement conditions of the drugs, explaining probably partially why the experience in the literature with anakinra is more substantial than with canakinumab. By analyzing studies in which patients have switched from one treatment to another, it seems that the main reason for switching is the ease of administration of canakinumab and/or the loss of compliance to anakinra after longer periods of use (36, 43, 56, 61, 64, 66, 72). A second reason for switching from anakinra to canakinumab is the occurrence of injection site reactions or other side effects with anakinra (such as urticaria or the rise of liver enzymes) which seem less prominent when taking canakinumab (40, 42, 43).
Interestingly the loss of efficacy of the first line IL-1 inhibitor can also be a reason for switching from one IL-1 inhibitor to the other. An inadequate or partial response has principally be described with anakinra (mainly after an initial good response and a secondary recurrence of symptoms), followed by a better response with canakinumab (29, 36, 40, 43, 47, 57, 64, 66, 72). However, in none of these reports the adherence to daily injections has been assessed. Moreover, that the worsening of the clinical picture with IL-1 antagonist could be secondary to other potential non-FMF conditions was only exceptionally discussed. An inadequate response with canakinumab has also been described in 2 reports (36, 66); both reports relate that canakinumab treatment was changed to anakinra for clinical and/or laboratory worsening, with a good response. These observations raise the question of whether the efficacy of IL-1 inhibitors is sustainable over the long term.
At present and in the absence of comparative studies both treatments seem to be an equal option for the management of colchicine resistant or intolerant FMF patients.
Maintenance Therapy vs. on Demand Treatment
The particularity of FMF is that the disease evolves by flare-ups. Usually, the only treatment offered are NSAIDs (naproxen, diclofenac, indomethacin, etc) that may alleviate symptoms during attacks but which are rarely completely effective (91). It therefore seems quite logical to offer intermittent treatment with IL-1 inhibitors to patients who continue to have attacks despite proper colchicine treatment. Paradoxically, this attitude has been little investigated. We identified simply 3 publications, concerning 20 patients treated with anakinra only during flares of the disease (19, 43, 92). The most interesting data is described in a retrospective study of Babaoglu and co-authors who investigated retrospectively The Gazi FMF cohort (92). The cohort is made up of 689 FMF patients of whom 78 patients were treated with IL-1 inhibitors among those 15 were treated with an on-demand anakinra protocol. Patient reporting attack severity, duration, frequency, absenteeism were significantly improved when receiving an on demand treatment with anakinra. Furthermore, prophylactic on-demand use of anakinra in patients with prominent triggers seemed also successful. All the patients continued the maximum tolerated dosage of colchicine and none had persistent inflammation before starting the on-demand protocol. The authors conclude that the use of anakinra during the prodromal period would be a reasonable approach for halting or alleviating symptoms of an impending attack allowing patients to diminish the loss of workdays and to improve the quality of life. Another advantage of this approach would be reducing cost and adverse effects of continued use of IL-1 inhibitors in selected patients with marked prodromes or triggers and low risk of amyloidosis.
Safety
In the different studies, the safety of LL-1 inhibition seemed generally good, at least at the short term. Only one case series reported a death following a treatment with canakinumab (59). The patient had end stage renal disease and severe multiorgan amyloidosis and died due to sepsis and peritonitis 1 year after cessation of IL-1 inhibition treatment. One opportunistic infection (fungal pneumonia) was reported in one patient receiving canakinumab (66). No malignancies were reported in any of the studies or case series.
The main reported side effect were local injection site reactions (17, 20, 25, 36, 40, 42, 43, 46, 48, 55, 57, 66, 69). Nevertheless, this side effect seems far more frequent in patients treated with anakinra than with canakinumab. Figure 2 shows an illustrative example of such a local site reaction. Up to now severe (43, 60, 66) or mild anaphylactic reactions (16, 40) were described only with anakinra.
Figure 2.

Example of an injection site reaction with anakinra.
The second most reported side effects were infectious complications, in a probably equivalent manner regardless of the type of IL-1 inhibitor used. The infections concerned chiefly the upper and lower respiratory tract (28, 35, 38, 48, 55) and were sometimes considered to be severe (12, 17, 39, 40, 56, 59, 66). Cutaneous infections (55, 63, 66) or viral infections of the herpes simplex group (54, 66) were also reported.
Anakinra seems to be more often responsible for cases of leucopenia (28, 37, 40, 62, 66), whereas headache (considered occasionally to be severe) seems to be observed more frequently with canakinumab (25, 38, 48, 55, 57).
Overall the safety profile of IL-1 inhibitors seems not different in FMF patients than in the other diseases including cryopyrin associated periodic syndrome, rheumatoid arthritis, adult-onset Still's disease and systemic-onset juvenile idiopathic arthritis. However, longer studies on FMF and post-marketing real-life experience are needed to verify the persistence of the relatively good IL-1 inhibitor tolerance on the long term.
Conclusion
The results from the present review suggest that IL-1 inhibitors are good candidates for colchicine resistant and/or intolerant FMF patients. IL-1 inhibitors have the potential to improve patient outcome even in patients with co-morbidities or severe complications in whom inflammation control is difficult to achieve with colchicine alone. Nevertheless, current data are limited and further evaluation of long-term efficacy and safety of IL-1 inhibitors are necessary, in order to provide robust evidence in this domain.
Author Contributions
VH conceived and wrote the review. CV and AF performed the literature search. VH and SG-L approved and validated the selected articles and checked the data assessment. All authors agreed to the final version of the manuscript.
Conflict of Interest
VH and SG-L have received counseling fees or for travel expenses from Novartis and SOBI, manufacturer of canakinumab and anakinra, respectively, but not for this work. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Versailles Hospital for editing assistance.
Glossary
Abbreviations
- AAA
amyloid type A protein amyloidosis formerly known as secondary amyloidosis
- FMF
familial Mediterranean Fever
- IL-1
interleukine 1
- MEFV gene
mediterranean fever gene
- NSAIDs
non-steroidal anti-inflammatory drugs
- TNF
tumor necrosis factor.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2020.00971/full#supplementary-material
References
- 1.Ben-Chetrit E, Levy M. Familial Mediterranean fever. Lancet. (1998) 351:659–64. 10.1016/S0140-6736(97)09408-7 [DOI] [PubMed] [Google Scholar]
- 2.Papadopoulos VP, Giaglis S, Mitroulis I, Ritis K. The population genetics of familial mediterranean fever: a meta-analysis study. Ann Hum Genet. (2008) 72:752–61. 10.1111/j.1469-1809.2008.00471.x [DOI] [PubMed] [Google Scholar]
- 3.French FMF Consortium . A candidate gene for familial Mediterranean fever. Nat Genet. (1997) 17:25–31. 10.1038/ng0997-25 [DOI] [PubMed] [Google Scholar]
- 4.The International FMF Consortium . Ancient missense mutations in a new member of the RoRet gene family are likely to cause familial Mediterranean fever. Cell. (1997) 90:797–807. 10.1016/S0092-8674(00)80539-5 [DOI] [PubMed] [Google Scholar]
- 5.Park YH, Wood G, Kastner DL, Chae JJ. Pyrin inflammasome activation and RhoA signaling in the autoinflammatory diseases FMF and HIDS. Nat Immunol. (2016) 17:914–21. 10.1038/ni.3457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dinarello CA, Wolff SM, Goldfinger SE, Dale DC, Alling DW. Colchicine therapy for familial mediterranean fever. A double-blind trial. N Engl J Med. (1974) 291:934–7. 10.1056/NEJM197410312911804 [DOI] [PubMed] [Google Scholar]
- 7.Zemer D, Pras M, Sohar E, Modan M, Cabili S, Gafni J. Colchicine in the prevention and treatment of the amyloidosis of familial Mediterranean fever. N Engl J Med. (1986) 314:1001–5. 10.1056/NEJM198604173141601 [DOI] [PubMed] [Google Scholar]
- 8.Cabili S, Zemer D, Pras M, Aviram A, Sohar E, Gafni J. The prevention of amyloidosis in familial Mediterranean fever with colchicine. Proc Eur Dial Transpl Assoc Eur Ren Assoc. (1985) 21:709–11. [PubMed] [Google Scholar]
- 9.Ozen S, Demirkaya E, Erer B, Livneh A, Ben-Chetrit E, Giancane G, et al. EULAR recommendations for the management of familial Mediterranean fever. Ann Rheum Dis. (2016) 75:644–51. 10.1136/annrheumdis-2015-208690 [DOI] [PubMed] [Google Scholar]
- 10.Corsia A, Georgin-Lavialle S, Hentgen V, Hachulla E, Grateau G, Faye A, et al. A survey of resistance to colchicine treatment for French patients with familial Mediterranean fever. Orphanet J Rare Dis. (2017) 12:54. 10.1186/s13023-017-0609-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ozen S, Kone-Paut I, Gül A. Colchicine resistance and intolerance in familial mediterranean fever: Definition, causes, and alternative treatments. Semin Arthritis Rheum. (2017) 47:115–20. 10.1016/j.semarthrit.2017.03.006 [DOI] [PubMed] [Google Scholar]
- 12.Chae JJ, Wood G, Masters SL, Richard K, Park G, Smith BJ, et al. The B30.2 domain of pyrin, the familial Mediterranean fever protein, interacts directly with caspase-1 to modulate IL-1beta production. Proc Natl Acad Sci USA. (2006) 103:9982–7. 10.1073/pnas.0602081103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vitale A, Orlando I, Lopalco G, Emmi G, Cattalini M, Frediani B, et al. Demographic, clinical and therapeutic findings in a monocentric cohort of adult patients with suspected PFAPA syndrome. Clin Exp Rheumatol. (2016) 34:77–81. [PubMed] [Google Scholar]
- 14.Vitale A, Insalaco A, Sfriso P, Lopalco G, Emmi G, Cattalini M, et al. A snapshot on the on-label and off-label use of the Interleukin-1 inhibitors in italy among rheumatologists and pediatric rheumatologists: a nationwide multi-center retrospective observational study. Front Pharmacol. (2016) 7:380. 10.3389/fphar.2016.00380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Belkhir R, Moulonguet-Doleris L, Hachulla E, Prinseau J, Baglin A, Hanslik T. Treatment of familial Mediterranean fever with anakinra. Ann Intern Med. (2007) 146:825–6. 10.7326/0003-4819-146-11-200706050-00023 [DOI] [PubMed] [Google Scholar]
- 16.Kuijk LM, Govers AMAP, Frenkel J, Hofhuis WJD. Effective treatment of a colchicine-resistant familial Mediterranean fever patient with anakinra. Ann Rheum Dis. (2007) 66:1545–6. 10.1136/ard.2007.071498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gattringer R, Lagler H, Gattringer KB, Knapp S, Burgmann H, Winkler S, et al. Anakinra in two adolescent female patients suffering from colchicine-resistant familial Mediterranean fever: effective but risky. Eur J Clin Invest. (2007) 37:912–4. 10.1111/j.1365-2362.2007.01868.x [DOI] [PubMed] [Google Scholar]
- 18.Roldan R, Ruiz AM, Miranda MD, Collantes E. Anakinra: new therapeutic approach in children with Familial Mediterranean Fever resistant to colchicine. Joint Bone Spine. (2008) 75:504–5. 10.1016/j.jbspin.2008.04.001 [DOI] [PubMed] [Google Scholar]
- 19.Mitroulis I, Papadopoulos VP, Konstantinidis T, Ritis K. Anakinra suppresses familial Mediterranean fever crises in a colchicine-resistant patient. Neth J Med. (2008) 66:489–91. [PubMed] [Google Scholar]
- 20.Calligaris L, Marchetti F, Tommasini A, Ventura A. The efficacy of anakinra in an adolescent with colchicine-resistant familial Mediterranean fever. Eur J Pediatr. (2008) 167:695–6. 10.1007/s00431-007-0547-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moser C, Pohl G, Haslinger I, Knapp S, Rowczenio D, Russel T, et al. Successful treatment of familial Mediterranean fever with Anakinra and outcome after renal transplantation. Nephrol Dial Transpl. (2009) 24:676–8. 10.1093/ndt/gfn646 [DOI] [PubMed] [Google Scholar]
- 22.Hennig S, Bayegan K, Uffmann M, Thalhammer F, Winkler S. Pneumonia in a patient with familial Mediterranean fever successfully treated with anakinra—case report and review. Rheumatol Int. (2012) 32:1801–4. 10.1007/s00296-010-1429-y [DOI] [PubMed] [Google Scholar]
- 23.Bilginer Y, Ayaz NA, Ozen S. Anti-IL-1 treatment for secondary amyloidosis in an adolescent with FMF and Behçet's disease. Clin Rheumatol. (2010) 29:209–10. 10.1007/s10067-009-1279-8 [DOI] [PubMed] [Google Scholar]
- 24.Petropoulou AD, Robin M, Socié G, Galicier L. Transmission of familial Mediterranean fever mutation after bone marrow transplantation and successful treatment with anakinra. Transplantation. (2010) 90:102–3. 10.1097/TP.0b013e3181d84cc3 [DOI] [PubMed] [Google Scholar]
- 25.Meinzer U, Quartier P, Alexandra JF, Hentgen V, Retornaz F, Koné-Paut I. Interleukin-1 targeting drugs in familial Mediterranean fever: a case series and a review of the literature. Semin Arthritis Rheum. (2011) 41:265–71. 10.1016/j.semarthrit.2010.11.003 [DOI] [PubMed] [Google Scholar]
- 26.Ozen S, Bilginer Y, Aktay Ayaz N, Calguneri M. Anti-interleukin 1 treatment for patients with familial Mediterranean fever resistant to colchicine. J Rheumatol. (2011) 38:516–8. 10.3899/jrheum.100718 [DOI] [PubMed] [Google Scholar]
- 27.Alpay N, Sumnu A, Calişkan Y, Yazici H, Türkmen A, Gül A. Efficacy of anakinra treatment in a patient with colchicine-resistant familial Mediterranean fever. Rheumatol Int. (2012) 32:3277–9. 10.1007/s00296-010-1474-6 [DOI] [PubMed] [Google Scholar]
- 28.Stankovic Stojanovic K, Delmas Y, Torres PU, Peltier J, Pelle G, Jéru I, et al. Dramatic beneficial effect of interleukin-1 inhibitor treatment in patients with familial Mediterranean fever complicated with amyloidosis and renal failure. Nephrol Dial Transplant. (2012) 27:1898–901. 10.1093/ndt/gfr528 [DOI] [PubMed] [Google Scholar]
- 29.Hacihamdioglu DO, Ozen S. Canakinumab induces remission in a patient with resistant familial Mediterranean fever. Rheumatology. (2012) 51:1041. 10.1093/rheumatology/kes021 [DOI] [PubMed] [Google Scholar]
- 30.Estublier C, Stankovic Stojanovic K, Bergerot JF, Broussolle C, Sève P. Myositis in a patient with familial Mediterranean fever and spondyloarthritis successfully treated with anakinra. Joint Bone Spine. (2013) 80:645–9. 10.1016/j.jbspin.2013.03.004 [DOI] [PubMed] [Google Scholar]
- 31.Soriano A, Verecchia E, Afeltra A, Landolfi R, Manna R. IL-1β biological treatment of familial Mediterranean fever. Clin Rev Allergy Immunol. (2013) 45:117–30. 10.1007/s12016-013-8358-y [DOI] [PubMed] [Google Scholar]
- 32.Ter Haar N, Lachmann H, Özen S, Woo P, Uziel Y, Modesto C, et al. Treatment of autoinflammatory diseases: results from the Eurofever Registry and a literature review. Ann Rheum Dis. (2013) 72:678–85. 10.1136/annrheumdis-2011-201268 [DOI] [PubMed] [Google Scholar]
- 33.Celebi ZK, Kucuksahin O, Sengul S, Tuzuner A, Keven K. Colchicine-resistant familial Mediterranean fever in a renal transplantation patient: successful treatment with anakinra. Clin Kidney J. (2014) 7:219–20. 10.1093/ckj/sft164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mercan R, Turan A, Bitik B, Tufan A, Haznedaroglu S, Goker B. Rapid resolution of protracted febrile myalgia syndrome with anakinra: report of two cases. Mod Rheumatol. (2016) 26:458–9. 10.3109/14397595.2014.882221 [DOI] [PubMed] [Google Scholar]
- 35.Brik R, Butbul-Aviel Y, Lubin S, Ben Dayan E, Rachmilewitz-Minei T, Tseng L, et al. Canakinumab for the treatment of children with colchicine-resistant familial Mediterranean fever: a 6-month open-label, single-arm pilot study. Arthritis Rheumatol. (2014) 66:3241–3. 10.1002/art.38777 [DOI] [PubMed] [Google Scholar]
- 36.Başaran Ö, Uncu N, Çelikel BA, Taktak A, Gür G, Cakar N. Interleukin-1 targeting treatment in familial Mediterranean fever: an experience of pediatric patients. Mod Rheumatol Jpn Rheum Assoc. (2015) 25:621–4. 10.3109/14397595.2014.987437 [DOI] [PubMed] [Google Scholar]
- 37.Ugurlu S, Seyahi E, Hatemi G, Hacioglu A, Ozcan H, Akkoc F, et al. Canakinumab therapy in patients with Familial Mediterranean Fever. Pediatr Rheumatol. (2015) 13:O45. 10.1186/1546-0096-13-S1-O4528362189 [DOI] [Google Scholar]
- 38.Gül A, Ozdogan H, Erer B, Ugurlu S, Kasapcopur O, Davis N, et al. Efficacy and safety of canakinumab in adolescents and adults with colchicine-resistant familial Mediterranean fever. Arthritis Res Ther. (2015) 17:243. 10.1186/s13075-015-0765-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cetin P, Sari I, Sozeri B, Cam O, Birlik M, Akkoc N, et al. Efficacy of interleukin-1 targeting treatments in patients with familial mediterranean Fever. Inflammation. (2015) 38:27–31. 10.1007/s10753-014-0004-1 [DOI] [PubMed] [Google Scholar]
- 40.Eroglu FK, Beşbaş N, Topaloglu R, Ozen S. Treatment of colchicine-resistant Familial Mediterranean fever in children and adolescents. Rheumatol Int. (2015) 35:1733–7. 10.1007/s00296-015-3293-2 [DOI] [PubMed] [Google Scholar]
- 41.Sevillano ÁM, Hernandez E, Gonzalez E, Mateo I, Gutierrez E, Morales E, et al. Anakinra induce la remisión completa del síndrome nefrótico en un paciente con fiebre mediterránea familiar y amiloidosis. Nefrología. (2016) 36:63–6. 10.1016/j.nefro.2015.06.026 [DOI] [PubMed] [Google Scholar]
- 42.Alpa M, Roccatello D. Canakinumab as rescue therapy in familial Mediterranean fever refractory to conventional treatment. Drug Des Devel Ther. (2015) 9:1983–7. 10.2147/DDDT.S69117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rossi-Semerano L, Fautrel B, Wendling D, Hachulla E, Galeotti C, Semerano L, et al. Tolerance and efficacy of off-label anti-interleukin-1 treatments in France: a nationwide survey. Orphanet J Rare Dis. (2015) 10:19. 10.1186/s13023-015-0228-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Özçakar ZB, Özdel S, Yilmaz S, Kurt-Sükür ED, Ekim M, Yalçinkaya F. Anti-IL-1 treatment in familial Mediterranean fever and related amyloidosis. Clin Rheumatol. (2016) 35:441–6. 10.1007/s10067-014-2772-2 [DOI] [PubMed] [Google Scholar]
- 45.Sozeri B, Kasapcopur O. Biological agents in familial Mediterranean fever focusing on colchicine resistance and amyloidosis. Curr Med Chem. (2015) 22:1986–91. 10.2174/0929867322666150311152300 [DOI] [PubMed] [Google Scholar]
- 46.Kucuksahin O, Yildizgoren MT, Ilgen U, Ates A, Kinikli G, Turgay M, et al. Anti-interleukin-1 treatment in 26 patients with refractory familial mediterranean fever. Mod Rheumatol. (2017) 27:350–5. 10.1080/14397595.2016.1194510 [DOI] [PubMed] [Google Scholar]
- 47.Laskari K, Boura P, Dalekos GN, Garyfallos A, Karokis D, Pikazis D, et al. Longterm beneficial effect of canakinumab in colchicine-resistant familial Mediterranean fever. J Rheumatol. (2017) 44:102–9. 10.3899/jrheum.160518 [DOI] [PubMed] [Google Scholar]
- 48.Ben-Zvi I, Kukuy O, Giat E, Pras E, Feld O, Kivity S, et al. Anakinra for colchicine-resistant familial Mediterranean fever: a randomized, double-blind, placebo-controlled trial. Arthritis Rheumatol. (2017) 69:854–62. 10.1002/art.39995 [DOI] [PubMed] [Google Scholar]
- 49.Georgin-Lavialle S, Stankovic Stojanovic K, Bachmeyer C, Sellam J, Abbara S, Awad F, et al. Spondyloarthritis associated with familial Mediterranean fever: successful treatment with anakinra. Rheumatol Oxf Engl. (2017) 56:167–9. 10.1093/rheumatology/kew290 [DOI] [PubMed] [Google Scholar]
- 50.Abbara S, Georgin-Lavialle S, Stankovic Stojanovic K, Bachmeyer C, Senet P, Buob D, et al. Association of hidradenitis suppurativa and familial Mediterranean fever: a case series of 6 patients. Jt Bone Spine Rev Rhum. (2017) 84:159–62. 10.1016/j.jbspin.2016.02.021 [DOI] [PubMed] [Google Scholar]
- 51.Ozen S, Kuemmerle-Deschner JB, Cimaz R, Livneh A, Quartier P, Kone-Paut I, et al. International retrospective chart review of treatment patterns in severe familial mediterranean fever, tumor necrosis factor receptor-associated periodic syndrome, and mevalonate kinase deficiency/hyperimmunoglobulinemia D syndrome. Arthritis Care Res. (2017) 69:578–86. 10.1002/acr.23120 [DOI] [PubMed] [Google Scholar]
- 52.Pecher AC, Igney-Oertel A, Kanz L, Henes J. Treatment of familial Mediterranean fever with anakinra in patients unresponsive to colchicine. Scand J Rheumatol. (2017) 46:407–9. 10.1080/03009742.2016.1245780 [DOI] [PubMed] [Google Scholar]
- 53.Barut K, Sahin S, Adrovic A, Sinoplu AB, Yucel G, Pamuk G, et al. Familial Mediterranean fever in childhood: a single-center experience. Rheumatol Int. (2018) 38:67–74. 10.1007/s00296-017-3796-0 [DOI] [PubMed] [Google Scholar]
- 54.Trabulus S, Korkmaz M, Kaya E, Seyahi N. Canakinumab treatment in kidney transplant recipients with AA amyloidosis due to familial Mediterranean fever. Clin Transplant. (2018) 32:e13345. 10.1111/ctr.13345 [DOI] [PubMed] [Google Scholar]
- 55.De Benedetti F, Gattorno M, Anton J, Ben-Chetrit E, Frenkel J, Hoffman HM, et al. Canakinumab for the treatment of autoinflammatory recurrent fever syndromes. N Engl J Med. (2018) 378:1908–19. 10.1056/NEJMoa1706314 [DOI] [PubMed] [Google Scholar]
- 56.Özçakar ZB, Keven K, Çakar N, Yalçinkaya F. Transplantation within the era of anti-IL-1 therapy: case series of five patients with familial Mediterranean fever-related amyloidosis. Transpl Int. (2018) 31:1181–4. 10.1111/tri.13312 [DOI] [PubMed] [Google Scholar]
- 57.Jesenak M, Hrubiskova K, Kapustova L, Kostkova M, Banovcin P. Canakinumab as monotherapy for treatment of familial Mediterranean fever - first report in Central and Eastern Europe region. Bratisl Lek Listy. (2018) 119:198–200. 10.4149/BLL_2018_036 [DOI] [PubMed] [Google Scholar]
- 58.Yildirim T, Yilmaz R, Uzerk Kibar M, Erdem Y. Canakinumab treatment in renal transplant recipients with familial Mediterranean fever. J Nephrol. (2018) 31:453–5. 10.1007/s40620-018-0475-5 [DOI] [PubMed] [Google Scholar]
- 59.Yazilitaş F, Aydog Ö, Özlü SG, Çakici EK, Güngör T, Eroglu FK, et al. Canakinumab treatment in children with familial Mediterranean fever: report from a single center. Rheumatol Int. (2018) 38:879–85. 10.1007/s00296-018-3993-5 [DOI] [PubMed] [Google Scholar]
- 60.Ergezen B, Ugurlu S, Ozdogan H. THU0611 anakinra treatment in patients with familial Mediterranean fever: a single-centre experience. Annals Rheumat Dis. (2018) 77:504–5. 10.1136/annrheumdis-2018-eular [DOI] [PubMed] [Google Scholar]
- 61.Kohler BM, Lorenz HM, Blank N. IL1-blocking therapy in colchicine-resistant familial Mediterranean fever. Eur J Rheumatol. (2018) 5:230–4. 10.5152/eurjrheum.2018.18036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Babaoglu H, Varan O, Kucuk H, Atas N, Satis H, Salman R, et al. Effectiveness of canakinumab in colchicine- and anakinra-resistant or -intolerant adult familial Mediterranean fever patients: a single-center real-life study. JCR J Clin Rheumatol. (2018) 1:7–13. [DOI] [PubMed] [Google Scholar]
- 63.Gülez N, Makay B, Sözeri B. Long-term effectiveness and safety of canakinumab in pediatric familial Mediterranean fever patients. Mod Rheumatol. (2018) 30:166–71. 10.1080/14397595.2018.1559488 [DOI] [PubMed] [Google Scholar]
- 64.Varan Ö, Kucuk H, Babaoglu H, Guven SC, Ozturk MA, Haznedaroglu S, et al. Efficacy and safety of interleukin-1 inhibitors in familial Mediterranean fever patients complicated with amyloidosis. Mod Rheumatol. (2019) 29:363–6. 10.1080/14397595.2018.1457469 [DOI] [PubMed] [Google Scholar]
- 65.Varan O, Kucuk H, Babaoglu H, Atas N, Salman RB, Satis H, et al. Effect of interleukin-1 antagonists on the quality of life in familial Mediterranean fever patients. Clin Rheumatol. (2019) 38:1125–30. 10.1007/s10067-018-4384-8 [DOI] [PubMed] [Google Scholar]
- 66.Akar S, Cetin P, Kalyoncu U, Karadag O, Sari I, Cinar M, et al. Nationwide Experience with off-label use of Interleukin-1 targeting treatment in familial mediterranean fever patients. Arthritis Care Res. (2018) 70:1090–4. 10.1002/acr.23446 [DOI] [PubMed] [Google Scholar]
- 67.Berdeli A, Senol Ö, Talay G. Treatment of familial Mediterranean fever with canakinumab in patients who are unresponsive to colchicine. Eur J Rheumatol. (2019) 6:82–5. 10.5152/eurjrheum.2019.18190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hasbal NB, Koc Y, Sevinc M, Unsal A, Basturk T. A familial Mediterranean fever patient with double homozygous mutations treated with anakinra after kidney transplantation. Nefrologia. (2019) 10.1016/j.nefro.2019.03.012. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 69.Sargin G, Kose R, Senturk T. Anti-interleukin-1 treatment among patients with familial Mediterranean fever resistant to colchicine treatment. Retrospective analysis. São Paulo Med J. (2019) 137:39–44. 10.1590/1516-3180.2018.0311101218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Eren Akarcan S, Dogantan S, Edeer Karaca N, Aksu G, Kutukculer N. Successful management of colchicine resistant familial Mediterranean fever patients with a standardized canakinumab treatment protocol: a case series and literature review. Rheumatol Int. (2019) 40:161–8. 10.1007/s00296-019-04366-w [DOI] [PubMed] [Google Scholar]
- 71.Kisla Ekinci RM, Balci S, Dogruel D, Altintas DU, Yilmaz M. Canakinumab in children with familial Mediterranean fever: a single-center, retrospective analysis. Pediatr Drugs. (2019) 21:389–95. 10.1007/s40272-019-00354-6 [DOI] [PubMed] [Google Scholar]
- 72.Sendogan DO, Saritas H, Kumru G, Eyupoglu S, Sadioglu RE, Tuzuner A, et al. Outcomes of canakinumab treatment in recipients of kidney transplant with familial Mediterranean fever: a case series. Transplant Proc. (2019) 51:2292–4. 10.1016/j.transproceed.2019.03.049 [DOI] [PubMed] [Google Scholar]
- 73.Berdeli A, Mir S, Nalbantoglu S, Kutukculer N, Sozeri B, Kabasakal Y, et al. Comprehensive analysis of a large-scale screen for MEFV gene mutations: do they truly provide a “heterozygote advantage” in Turkey? Genet Test Mol Biomark. (2011) 15:475–82. 10.1089/gtmb.2010.0146 [DOI] [PubMed] [Google Scholar]
- 74.Erden A, Batu ED, Sari A, Sönmez HE, Armagan B, Demir S, et al. Which definition should be used to determine colchicine resistance among patients with familial Mediterranean fever? Clin Exp Rheumatol. (2018) 36:97–102. [PubMed] [Google Scholar]
- 75.Ben-Chetrit E, Aamar S. About colchicine compliance, resistance and virulence. Clin Exp Rheumatol. (2009) 27:S1–3. [PubMed] [Google Scholar]
- 76.Melikoglu MA, Senel K. Non-response to colchicine in familial Mediterranean fever should be identified accurately. Int J Rheum Dis. (2017) 20:2118–21. 10.1111/1756-185X.12374 [DOI] [PubMed] [Google Scholar]
- 77.Fradkin A, Yahav J, Zemer D, Jonas A. Colchicine-induced lactose malabsorption in patients with familial Mediterranean fever. Isr J Med Sci. (1995) 31:616–20. [PubMed] [Google Scholar]
- 78.Stamp LK. Safety profile of anti-gout agents: an update. Curr Opin Rheumatol. (2014) 26:162–8. 10.1097/BOR.0000000000000031 [DOI] [PubMed] [Google Scholar]
- 79.Kuncl RW, Duncan G, Watson D, Alderson K, Rogawski MA, Peper M. Colchicine myopathy and neuropathy. N Engl J Med. (1987) 316:1562–8. 10.1056/NEJM198706183162502 [DOI] [PubMed] [Google Scholar]
- 80.Altiparmak MR, Pamuk ON, Pamuk GE, Hamuryudan V, Ataman R, Serdengecti K. Colchicine neuromyopathy: a report of six cases. Clin Exp Rheumatol. (2002) 20:S13–6. 10.1034/j.1399-0012.2002.01129.x [DOI] [PubMed] [Google Scholar]
- 81.Medani S, Wall C. Colchicine toxicity in renal patients - Are we paying attention? Clin Nephrol. (2016) 86:100–5. 10.5414/CN108343 [DOI] [PubMed] [Google Scholar]
- 82.Mullins M, Cannarozzi AA, Bailey TC, Ranganathan P. Unrecognized fatalities related to colchicine in hospitalized patients. Clin Toxicol. (2011) 49:648–52. 10.3109/15563650.2011.589844 [DOI] [PubMed] [Google Scholar]
- 83.Montseny JJ, Meyrier A, Gherardi RK. Colchicine toxicity in patients with chronic renal failure. Nephrol Dial Transplant. (1996) 11:2055–8. 10.1093/oxfordjournals.ndt.a027096 [DOI] [PubMed] [Google Scholar]
- 84.Hung IFN, Wu AKL, Cheng VCC, Tang BSF, To KW, Yeung CK, et al. Fatal interaction between clarithromycin and colchicine in patients with renal insufficiency: a retrospective study. Clin Infect Dis. (2005) 41:291–300. 10.1086/431592 [DOI] [PubMed] [Google Scholar]
- 85.Soriano A, Manna R. Familial Mediterranean fever: new phenotypes. Autoimmun Rev. (2012) 12:31–7. 10.1016/j.autrev.2012.07.019 [DOI] [PubMed] [Google Scholar]
- 86.Heller H, Sohar E, Sherf L. Familial Mediterranean fever. AMA Arch Intern Med. (1958) 102:50–71. 10.1001/archinte.1958.00260190052007 [DOI] [PubMed] [Google Scholar]
- 87.Heller H, Sohar E, Pras M. Ethnic distribution and amyloidosis in familial Mediterranean fever (FMF). Pathol Microbiol Basel. (1961) 24:718–23. 10.1159/000161188 [DOI] [PubMed] [Google Scholar]
- 88.Lachmann HJ, Goodman HJB, Gilbertson JA, Gallimore JR, Sabin CA, Gillmore JD, et al. Natural history and outcome in systemic AA amyloidosis. N Engl J Med. (2007) 356:2361–71. 10.1056/NEJMoa070265 [DOI] [PubMed] [Google Scholar]
- 89.Bilgen SA, Kilic L, Akdogan A, Kiraz S, Kalyoncu U, Karadag O, et al. Effects of anti-tumor necrosis factor agents for familial mediterranean fever patients with chronic arthritis and/or sacroiliitis who were resistant to colchicine treatment. J Clin Rheumatol. (2011) 17:358–62. 10.1097/RHU.0b013e31823682f5 [DOI] [PubMed] [Google Scholar]
- 90.Seyahi E, Ozdogan H, Celik S, Ugurlu S, Yazici H. Treatment options in colchicine resistant familial Mediterranean fever patients: thalidomide and etanercept as adjunctive agents. Clin Exp Rheumatol. (2006) 24:S99–103. [PubMed] [Google Scholar]
- 91.Ozturk MA, Kanbay M, Kasapoglu B, Onat AM, Guz G, Furst DE, et al. Therapeutic approach to familial Mediterranean fever: a review update. Clin Exp Rheumatol. (2011) 29:S77–86. [PubMed] [Google Scholar]
- 92.Babaoglu H, Varan O, Kucuk H, Atas N, Satis H, Salman R, et al. On demand use of anakinra for attacks of familial Mediterranean fever (FMF). Clin Rheumatol. (2019) 38:577–81. 10.1007/s10067-018-4230-z [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.