Abstract
The coronavirus disease 2019 (COVID-19) pandemic has in some regions overwhelmed the capacity and staffing needs of healthcare systems, necessitating the provision of resources and staff from different disciplines to aid COVID treatment teams. Stroke centers have multidisciplinary clinical and procedural expertise to support COVID treatment teams. Staff safety and patient safety are essential, as are open lines of communication between stroke center leaders and hospital leadership in a pandemic where policies and procedures can change or evolve rapidly. Support needs to be allocated in a way that allows for the continued operation of a fully capable stroke center, with the ability to adjust if stroke center volume or staff attrition requires.
Keywords: coronavirus, COVID-19, hospital, pandemic, patients
The coronavirus disease 2019 (COVID-19) pandemic has provided a dramatic strain on health care system capacity and staffing, necessitating in some regions the provision of resources and staff from different disciplines to aid in the mission of treating patients with COVID. Stroke centers may be called to aid their hospitals by devoting resources or staff to clinically provide assistance to COVID treatment teams. Ideally, striking a balance between helping the community while maintaining stroke center operation is critical. This document discusses strategies to address1 how stroke center clinical staff can aid pandemic staffing challenges and2 how stroke centers may operationally aid other elements of the healthcare system during the current pandemic and with similar system-wide crises in the future.
Key Underlying Assumptions
It is assumed a stroke center will continue being fully operational with the commensurate staff and resources necessary to strive for attaining recommended diagnostic and interventional metrics while also assuring the safety of stroke center staff and patients.1–7 Additionally, it is expected a comprehensive or hub stroke center would still be able to provide the same quality of remote care to telestroke and other spoke sites.8 Stroke center aid to its institution, or regional partners, should be allocated in a manner that provides the ability to adapt to changing stroke volumes, which appear to have decreased during early phases of the pandemic9 while also having a reserve backup plan in case of staff attrition. Also, given the possibility that stroke clinics could close and that acute patients may avoid emergency rooms (ERs) during a pandemic, it is anticipated that stroke centers would need to allocate staff and resources to do community outreach and engagement activities (ie, telemedicine clinic visits, education reminding people to activate emergency medical services (EMS) for stroke symptoms). It is also important to recognize that patients with mild stroke may not have presented during the pandemic. In many ways, these potentially vulnerable patients are most in need of secondary stroke prevention.
It is likely that most institutions will have some form of a hospital-level multidisciplinary COVID task force, charged with providing temporary pandemic guidance, distributing local institutional data, creating clinical treatment pathways, and providing support to inform system decisions. These local groups may be comprised of key hospital leaders and can interact with larger regional and state bodies to ensure a cohesive and comprehensive response. Frequent and clear communication between such bodies is paramount. It is assumed a stroke program will be in communication loops for local and regional pandemic planning and will have open and ongoing communication with hospital and task force leadership. A final central guiding principle is staff and patient safety with the implementation of effective infection control strategies (Figure 1A).10 Ideally, practice parameters should adhere to guidelines by agencies such as the Centers for Disease Control and Prevention and the World Health Organization with appropriate deference to local operational parameters.
Figure 1.
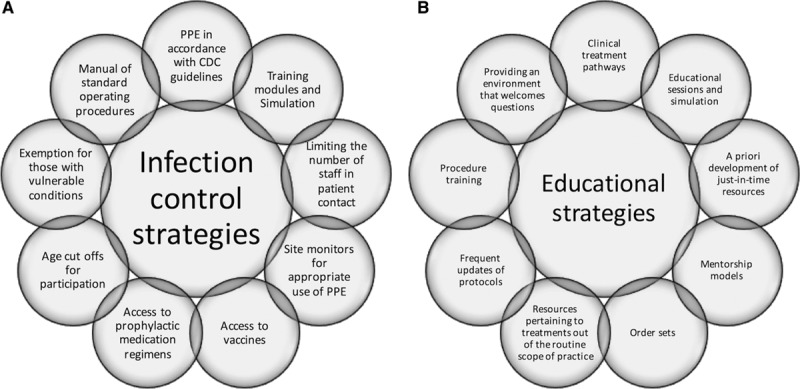
Sample infection control strategies and educational strategies for multidisciplinary coronavirus disease (COVID) treatment teams.
A, Infection control strategies; (B) educational strategies. CDC indicates Centers for Disease Control and Prevention; and PPE, personal protective equipment..
Health System Staffing Challenges With Patient Surge and Staff Attrition
The Problem
Patient volume surge in combination with staff attrition can necessitate the provision of staff from other disciplines to help manage ER, hospitalized or critically ill patients infected with COVID-19. This has extended to neurologists (ie, in Italy, neurologists worked in the ER to manage patients with COVID)11 and could further lead to stroke centers lending staff to help manage patients with COVID or help serve the system in some other capacity.
A Stroke Centers Role
Stroke centers have multidisciplinary clinical and procedural expertise to support institutions in this pandemic, as well as having neurocritical care capabilities in centers having a neurological intensive care unit (NICU). Stroke center staff could help manage patients with COVID in a variety of ways1: being reassigned to a COVID treatment team in the ICU or a COVID unit2; managing overflow patients with COVID in the NICU or on a stroke/neurology service; and3 working on a COVID procedural team. Recruitment of stroke center staff by hospital leadership would ideally be voluntary. However, in times of significant resource strain or pending crisis, there could be mechanisms enacting an all hands on deck reassignment of all staff if a pandemic surge overwhelms a system. Also of importance to note, it is possible smaller stroke centers may not have the ability to offer assistance due to a limited number of staff or beds or due to a concomitant stroke volume surge.
Given the clinical complexities and rapidly changing science with COVID-19, it would be incumbent upon hospitals to have a mechanism providing educational resources and centralized clinical guidance to all providers working with patients with COVID, especially those deployed to units operating out of their usual scope of practice (ie, a stroke ward nurse reassigned to an ICU). Potential strategies to be employed are listed in Figure 1B. It is also advisable that general and unit-specific education regarding infection control procedures be performed, as the risks in the MICU would be different than those of a ward (ie, viral aerosolizing procedures such as noninvasive ventilation and intubation). Not to be underestimated, critical human factor principles would also need to be encouraged at all staff levels to make reassignments successful. Namely, the construction of supportive and nonjudgmental environments where it is ok to ask any question and where staff members can genuinely feel a part of the team. It is possible that any level of stroke center providers could be dedicated to managing patients with COVID, with differing roles and responsibilities outlined below.
Nurses
Stroke center nurses could be reassigned by local nursing leadership to manage patients with COVID in other units (ER, floor, ICU) or could manage COVID overflow patients in the NICU or on the ward. It could be beneficial for a system to identify nurses with unique expertise or past experience, such as a nurse who used to work in the MICU, to work in an overflow COVID ICU. Other nurses with experience similar to an ICU, such as a post-anesthesia care unit, would benefit from being oriented with a team member (buddy system) to assure competence in the COVID ICU environment. Nurses may be especially needed on some COVID units due to visitor restrictions, and the resultant effect that nurses may be spending more time at the bedside providing emotional support to patients since family members are not able to be present. Staffing ratios should be flexed to accommodate this important nursing role. It is also possible nurses could be pulled to work on another non-COVID floor due to staff redistribution or attrition, such as COVID specimen collection, temperature assessment of visitors, or telemedicine contacts. Nurses are often very specialized in tertiary care centers and may be more fluid in community hospitals but the above recommendations apply to all acute hospital settings.
It is possible during an extreme pandemic surge that nursing to patient ratios could be increased from the standard acceptable norms for that unit. Thus, having programmed planning to pull nurses from other service lines, or other sites within a health system, would be advisable. It is recommended that nurses working in areas out of their routine scope of practice, and especially those going from a lower acuity unit to an ICU, have mentorship and resources to aid them in their new roles, such as having clinical pharmacist support for vasopressor infusions and assistance from conurses for select items (ie, zeroing an arterial line).
Nurse Practitioners and Physician Associates
It is possible stroke program nurse practitioners and physician associates could provide direct patient care in a variety of settings and perhaps alongside pulled staff from other disciplines (ie, surgery, pediatrics). Preferably, stroke center staff, and those from other disciplines, would be placed on teams with some form of direct mentorship from that treatment areas practitioners (ie, in the MICU would work with MICU staff). Given restrictions on hospital visitation during this pandemic, team members could also just only round with a COVID team, without having direct patient contact, and serve by providing direct communication to family members of admitted patients. These advanced providers could likely also benefit from educational sessions and resources pertaining to the pathophysiology of COVID infections, treatments, and procedures out of their usual scope of practice, as well as being provided standardized treatment protocols and order sets specific for patients with COVID.
Neuro-Intensivists, Neuro-Hospitalists, and Stroke/Vascular Neurologists
NICU faculty may be asked to manage a medical intensive care unit (MICU) off-load COVID team or manage overflow medical patients with COVID in the critical care or ward setting. In the NICU, leadership would provide oversight for COVID infection control processes which are of paramount importance to protect staff and other non-COVID critically ill brain-injured patients. When felt to be needed, NICU faculty would identify educational resources for NICU team members about the management of COVID specific complications (ie, refractory hypoxia treatment with nitrous oxide or pulmonary vasodilator infusions) as well as education regarding therapeutics. NICU leaders should work with MICU and hospital leadership to optimize patient flow, bed triage and bed flow, tight bed control flow, and fragmentation of care. NICUs managing overflow patients with COVID should have close and frequent communication with the hospital COVID task force. When feasible, having representation on the task force could have several advantages. It would facilitate communication to the broader NICU nursing and faculty pool of providers, would enable important contributions from a representative overflow unit, would provide up-to-date information in a pandemic where new knowledge is regularly being learned about COVID and COVID management, could provide another avenue for stroke center issues to be addressed, and would enable real-time participation in the creation of institutional policies and procedures.
Stroke center directors should be in close communication with hospital leadership regarding system changes in the pandemic which could influence the stroke program. When approached for voluntary redeployment, stroke division directors should consider prioritization of the faculty to sustain the rotation of coverage for stroke codes and overseeing the stroke unit—that is, a rotation that allows for at least one vascular neurologist and a backup provider at all times in the case of staff drop out for exposure or illness, with adequate time for quarantining before reentering the hospital between rotations.
Clinically, neuro-hospitalists and vascular neurologists could be invited to manage an internal medicine COVID treatment team overseeing noncritically ill patients with COVID. In cases of severe surge, there may be a request to help with critical care services. In such an instance, adequate, rapid, just-in-time training should be made available, ideally with proportionate mentorship/oversight from critical care colleagues, and a graded responsibility that matches physician comfort and training. On occasions where hospitals execute internal disaster plans calling for the aid of all medical staff to help manage critically ill patients with COVID, placing some out of their typical scope of practice, it is hoped state or local authorities would implement temporary liability protections or that hospitals will provide the requisite liability coverage for these providers. Overflow of noncritically ill patients with COVID onto a stroke or neurology floor may also occur. Like for NICU faculty, stroke service medical directors and faculty would be the leaders of their teams, responsible for staff education, infection control, and the overall management of patients with COVID on their service.
Finally, NICU leaders, stroke center medical directors, and neuro-hospitalist leaders should be in close communication to discuss relevant protocols and procedures in light of current and projected capacity trends over the course of the pandemic. If a center becomes overwhelmed with patients with COVID, thus losing a critical number of ICU beds, these leaders would be integral for identifying how a stroke center could decrease its use of ICU beds and could also alter protocols to optimize patient care and staff safety. Additionally, under the auspices of temporary guidance for stroke centers, by which full compliance is a goal, rather than an expectation,1 these leaders could work with nursing leadership to identify specific patient populations who could be cared for in a stepdown unit or general floor, presuming specific provisions were made to ensure patient safety.
Interventionalists
Stroke interventionalists may be invited to provide technical assistance on COVID procedure teams performing procedures such as basic and advanced vascular access. This could be of distinct importance if a hospital’s COVID volume necessitated the creation of COVID treatment teams consisting of clinicians from other disciplines who routinely do not perform critical care procedures.
Operational Challenges in a Pandemic or Other Time of Crisis
The Problem
In some regions, the COVID-19 pandemic surge has led to a crisis of diminished hospital bed capacity. This follows and is perhaps accentuated by prepandemic ED and hospital overcrowding issues.12 Some districts considered enacting prehospital and inpatient critical care triage protocols determining medical futility adapted from the Maryland framework for the allocation of scarce life-sustaining medical resources in a catastrophic medical emergency.13 To handle the surge, many systems created inpatient COVID units on other floors and other units in nontraditional spaces (ie, hospital meeting rooms, clinic offices). Challenges may also be encountered in maintaining health system operations, pandemic data surveillance and reporting, local and regional communication, scalability, and preparedness projections. Other national or regional disasters have posed similar problems to health care systems.
A Stroke Centers Role
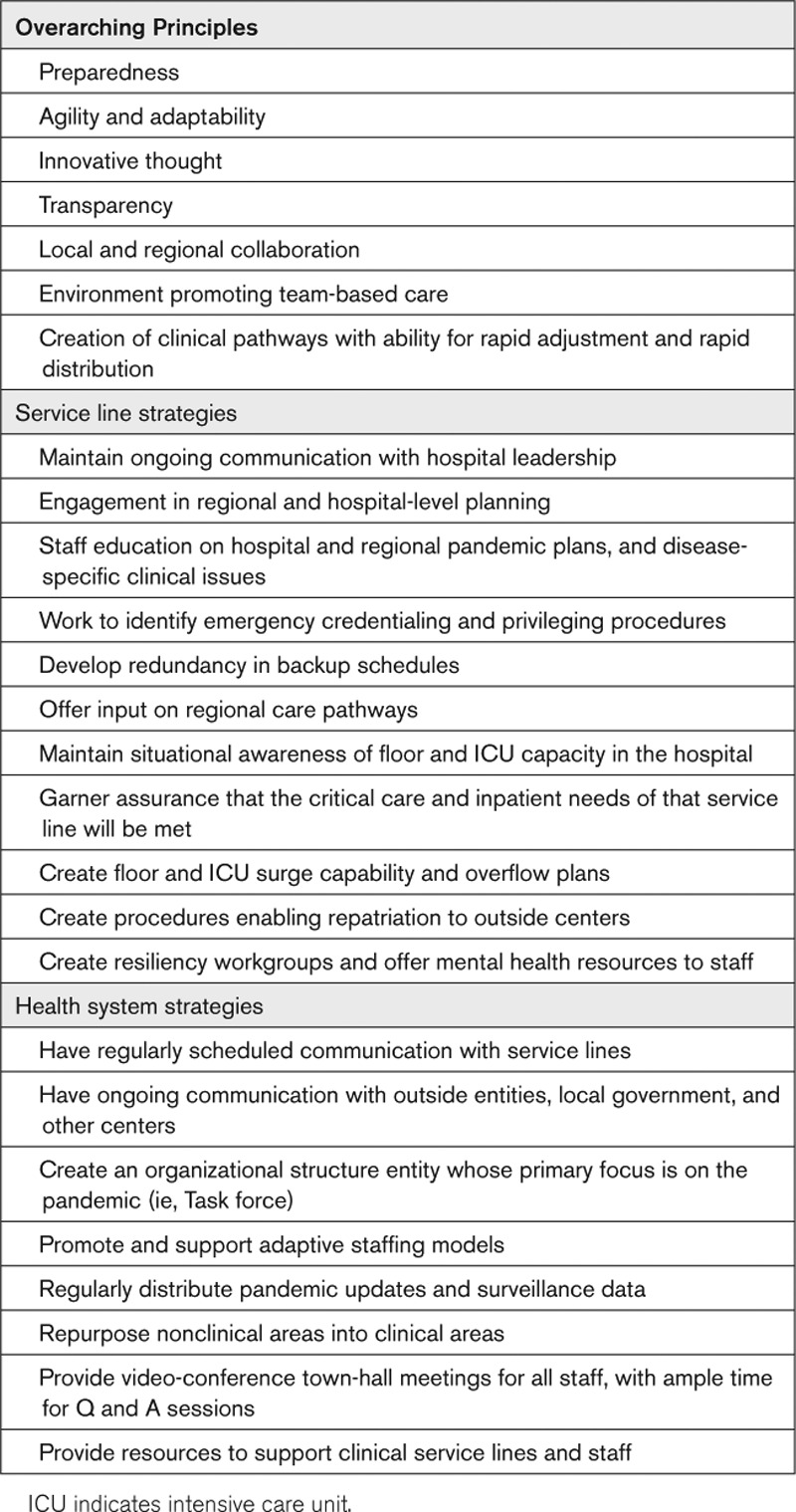
Within a health care system, many service lines (ie, stroke, trauma, cardiac critical care) could be called to provide aid to their institutions during a pandemic, with core principles and strategies for optimally utilizing a service line resources listed in the Table.14,15 Stroke centers have clinical and nonclinical resources that may provide aid in a pandemic or similar crisis. First, a cohort of stroke center beds could be converted into COVID units or COVID overflow beds. If resources permit, stroke center equipment could be devoted to helping equip overflow units in nontraditional patient care areas. In such cases, there should be flexibility to add, reduce, or reallocate stroke capacity and equipment as needed during an evolving crisis.
Table.
Stroke centers often have robust research infrastructure adept at conducting clinical trials. In the setting of a pandemic such as COVID-19, this research infrastructure can be redeployed to rapidly prop up new treatment trials based on the current priority. This is a reasonable trade-off as prepandemic trials may be put on hold for enrollment, particularly acute stroke trials due to the reprioritization of emergency providers and resources. These staff could also aid the local COVID task force by acquiring daily hospital dashboards and reportable data (ICU capacity, ventilator availability, total COVID volume) which could be reported.
A stroke center also has familiarity and overlapping patient care responsibilities with a multitude of different service lines and other outside hospitals, potentially poising stroke center representatives to assist in facilitating system communication in a pandemic (Figure 2). The open lines of communication with other hospitals in a region are also crucial during a pandemic for facilitating state or regional stroke system surveillance, with the capability of formulating rerouting plans if another stroke center needs to close. Thus, a stroke center could also serve to help another health system with over-stretched capacity or significantly high staff attrition. Stroke centers often perform regular outreach to local and regional EMS networks and provide regular continuing education for EMS providers regarding prehospital stroke care. In the setting of a pandemic, these relationships could be channeled to offload busy local EMS medical directors, and by assisting education, clinical care, and wellness for EMS providers managing infected patients on the front lines.
Figure 2.
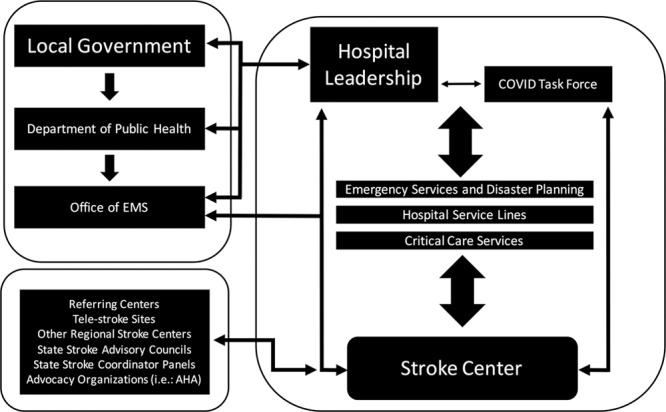
Communication pathways during a pandemic for a comprehensive or tertiary care stroke center.
AHA indicates American Heart Association; COVID, coronavirus disease; and EMS, emergency medical services.
Finally, for pandemics or other disasters, stroke centers have high fidelity equipment at their disposal which could aid operations. Telestroke technology platforms could be utilized by other specialties wanting to do remote consults in the ER during the pandemic and could also facilitate telecritical care and teleneurocritical care evaluations between smaller hospitals and tertiary care centers for complex critically ill or patients with COVID. For other disasters, there have been instances of mobile stroke units being deployed to a satellite hospital and serving as that sites computed tomography scan. It is also conceivable that a mobile stroke unit could be deployed to a local or national disaster with emergency preparedness physicians, with the computed tomography serving to triage trauma patients.
Conclusions
Stroke centers have clinical and procedural expertise, as well as resources to help in the COVID pandemic. These trying times and their unique challenges also provide an epoch of opportunity to provide assistance to colleagues and overall can enhance collegiality in addition to increasing familiarity with other provider’s roles and responsibilities. This interdisciplinary collaboration, although supporting members and patients, can improve future care models and post-pandemic operational procedures. Maintenance of staff safety and stroke care efficacy and quality for our patients are both crucial. Frequent and effective patient safety is essential, as is open and ongoing communication between front-line providers, stroke center leaders, and hospital leadership. The strategies provided above and early preparation now will aid in future emergencies. In addition, there needs to be continuing focus on staff wellness and team performance such that stroke providers can rise to this challenge with our other colleagues to provide excellent stroke-specific care and assistance to other specialized areas.
Acknowledgments
Dr Wira contributed to conceptualization, drafting, and critical revision of the article. Remaining authors contributed to drafting or critical revision of the article.
Sources of Funding
None.
Disclosures
Dr Southerland reports research support (Diffusion Pharmaceuticals, American Heart Association/American Stroke Association, National Institutes of Health [NIH], National Science Foundation, Coulter Translational Research Fund), intellectual property (nonremunerative: US Patent Application No. 14/910,890, US Provisional Patent Application No. 62/620,096) and he is a legal Expert Review (Stroke and Vascular Neurology). Dr Sheth reports research grants (NIH R01NS110721, RO3NS112859, RO1NS075209, UO1NS113445, U01NS106513, RO1NR01833, U24NS107215, U24NS107136) and funding from the AHA, Novartis, Biogen, Bard, Hyperfine, and is a consultant for Zoll, Astrocyte. Dr Sheth has also equity ownership (Alva). Dr Goyal is a consultant for Medtronic, Stryker, Microvention, GE Healthcare, Mentice. The other authors report no conflicts.
Nonstandard Abbreviations and Acronyms
- COVID-19
- coronavirus disease 2019
- ER
- emergency room
- NICU
- neurological intensive care unit
This manuscript was sent to Marc Fisher, Senior Consulting Editor, for review by expert referees, editorial decision, and final disposition.
For Sources of Funding and Disclosures, see page xxx.
Dr Wira contributed to conceptualization, drafting, and critical revision of the article. Remaining authors contributed to drafting or critical revision of the article.
References
- 1.AHA/ASA Stroke Council Leadership. Temporary emergency guidance to US stroke centers during the coronavirus disease 2019 (COVID-19) pandemic: on Behalf of the American Heart Association/American Stroke Association Stroke Council Leadership Stroke. 2020; 51:1910–1912. doi: 10.1161/STROKEAHA.120.030023 [DOI] [PubMed] [Google Scholar]
- 2.Smith MS, Bonomo J, Knight WA, 4th, Prestigiacomo CJ, Richards CT, Ramser E, Adeoye O, Bertsch S, Shirani P, Vagal A, et al. Endovascular therapy for patients with acute ischemic stroke during the COVID-19 pandemic: a proposed algorithm. Stroke. 2020; 51:1902–1909. doi: 10.1161/STROKEAHA.120.029863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen TN, Abdalkader M, Jovin TG, Nogueira RG, Jadhav AP, Haussen DC, Hassan AE, Novakovic R, Sheth SA, Ortega-Gutierrez S, et al. Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the society of vascular and interventional neurology Stroke. 2020; 51:1896–1901. doi: 10.1161/STROKEAHA.120.030100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodríguez-Pardo J, Fuentes B, Alonso de Leciñana M, Campollo J, Calleja Castano P, Carneado Ruiz J, Egido Herrero J, García Leal R, Gil Núñez A, Gómez Cerezo JF, et al. Acute stroke care during the COVID-19 pandemic. Ictus Madrid Program recommendations Neurologia. 2020; 35:258–263. doi: 10.1016/j.nrl.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qureshi AI, Abd-Allah F, Alsenani F, Aytac E, Borhani-Haghighi A, Ciccone A, Gomez CR, Gurkas E, Hsu CY, Jani V, et al. Management of acute ischemic stroke in patients with COVID-19 infection: report of an international panel Int J Stroke. 20201747493020923234 doi: 10.1177/1747493020923234 [DOI] [PubMed] [Google Scholar]
- 6.Dafer RM, Osteraas ND, Biller J. Acute stroke care in the coronavirus disease 2019 pandemic J Stroke Cerebrovasc Dis. 2020; 29:104881 doi: 10.1016/j.jstrokecerebrovasdis.2020.104881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fraser JF, Arthur AS, Chen M, Levitt M, Mocco J, Albuquerque FC, Ansari SA, Dabus G, Jayaraman MV, Mack WJ, et al. Society of NeuroInterventional Surgery recommendations for the care of emergent neurointerventional patients in the setting of COVID-19 J Neurointerv Surg. 2020; 12:539–541. doi: 10.1136/neurintsurg-2020-016098 [DOI] [PubMed] [Google Scholar]
- 8.Leira EC, Russman AN, Biller J, Brown DL, Bushnell CD, Caso V, Chamorro A, Creutzfeldt CJ, Cruz-Flores S, Elkind MSV, et al. Preserving stroke care during the COVID-19 pandemic: potential issues and solutions Neurology. 2020. 10.1212/WNL.0000000000009713. Available at: https://n.neurology.org/content/early/2020/05/07/WNL.0000000000009713. Accessed May 9, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of covid-19 on stroke evaluation in the United States N Engl J Med. 202010.1056/NEJMc2014816 doi: 10.1056/NEJMc2014816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khosravani H, Rajendram P, Notario L, Chapman MG, Menon BK. Protected code stroke: hyperacute stroke management during the coronavirus disease 2019 (COVID-19) pandemic Stroke. 2020; 51:1891–1895. doi: 10.1161/STROKEAHA.120.029838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, Colombi D, Zaino D, Michieletti E, Guidetti D. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era Eur Neurol. 20201–3. doi: 10.1159/000507666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salehi L, Phalpher P, Valani R, Meaney C, Amin Q, Ferrari K, Mercuri M. Emergency department boarding: a descriptive analysis and measurement of impact on outcomes CJEM. 2018; 20:929–937. doi: 10.1017/cem.2018.18 [DOI] [PubMed] [Google Scholar]
- 13.Daugherty Biddison EL, Faden R, Gwon HS, Mareiniss DP, Regenberg AC, Schoch-Spana M, Schwartz J, Toner ES. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters Chest. 2019; 155:848–854. doi: 10.1016/j.chest.2018.09.025 [DOI] [PubMed] [Google Scholar]
- 14.American College of Surgeons Committee on Trauma. Quality programs of the American college of surgeons, Maintaining trauma center access and care during the COVID-19 pandemic: guided document for trauma medical directors. Available at: https://www.facs.org/-/media/files/quality-programs/trauma/acs_cot_statement_on_maintaining_trauma_center_access.ashx, Accessed May 18, 2020.
- 15.Katz JN, Sinha SS, Alviar CL, Dudzinski DM, Gage A, Brusca SB, Casey Flanagan M, Welch T, Geller BJ, Elliott Miller P, et al. Disruptive modifications to cardiac critical care delivery during the Covid-19 pandemic: an international perspective J Am Coll Cardiol. 2020S0735-1097(20)35002-6 doi: 10.1016/j.jacc.2 [DOI] [PMC free article] [PubMed] [Google Scholar]


