Abstract
Since it first emerged in December 2019, coronavirus disease 2019 (COVID-19) has spread rapidly worldwide. During the pandemic of an emerging infectious disease, it is very important to prevent nosocomial outbreaks and operate hospitals safely to maintain their functions. In this article, we present the strategies for safe hospital operations based on the experiences of the Republic of Korea early in the COVID-19 pandemic. Each hospital should maintain multiple layers of defenses to prevent even small cracks in the hospital’s quarantine system.
Keywords: COVID-19, SARS-CoV-2, Infection control, Health personnel, Hospital planning
During the 2015 Middle East respiratory syndrome (MERS) outbreak in South Korea, most cases were hospital-acquired infections, and 21% of them occurred among healthcare personnel (HCP) (Choi et al., 2016). Based on the experience gained during the 2015 MERS outbreak, the health authorities and individual hospitals in South Korea implemented enhanced responses to the coronavirus disease 2019 (COVID-19) pandemic. With the implementation of a reinforced hospital action plan, nosocomial transmission of COVID-19 was quite limited (Supplementary Material Figure S1) (Korea Ministry of Health and Welfare and Centers for Disease Control and Prevention, 2020). Only 1.4% of COVID-19 cases occurred in acute care hospitals, whereas more than 6% of cases occurred in long-term care facilities and psychiatric long-term care hospitals (Korea Ministry of Health and Welfare and Centers for Disease Control and Prevention, 2020). It is necessary to support and strengthen the infection control systems of long-term care facilities, which may be places of unexpected outbreaks with higher case fatality rates (McMichael et al., 2020).
According to a report from the International Council of Nurses, at least 90 000 HCP worldwide are believed to have been infected with COVID-19 (Nebehay, 2020). HCP comprised about 6% of the 3.5 million cases of COVID-19 in the world, as of May 6, 2020. In South Korea, HCP accounted for 2.4% of the total patients with COVID-19, significantly lower than the rates in other countries (9.1–29.0%) (Supplementary Material Figure S2) (Korea Ministry of Health and Welfare and Centers for Disease Control and Prevention, 2020; COVID-19 Response Team of Centers for Disease Control and Prevention, 2020; Wang et al., 2020). It was possible to lower the infection rate in HCP by reducing the workload through the efficient distribution of medical resources and providing sufficient personal protective equipment (PPE).
The outbreak of COVID-19 in hospitals will not only lead to missed opportunities of treat chronic diseases in patients with high-risk conditions, but will also lead to high mortality rates if these patients become infected. Even patients with mild symptoms can spread severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to many people in the enclosed spaces of hospitals. Thus, each hospital should bear in mind the Swiss cheese theory to provide multiple layers of defenses to prevent even small cracks in the hospital’s quarantine system (Table 1 ).
Table 1.
Safe hospital strategies in South Korea.
| Individual strategy | Description | |
|---|---|---|
| Hospital-level strategies | Education and training of hospital staff | • Personal protective equipment (PPE) – wearing and removing process. |
| • High-risk behaviors and conditions. | ||
| • Environmental cleaning and disinfection. | ||
| Universal masking and hand hygiene | • All visitors and staff were required to wear a mask in the hospital. | |
| • Hand sanitizer was placed throughout the hospital. | ||
| Inpatient monitoring for new-onset fever and respiratory symptoms | Hospitalized patients with new-onset fever or respiratory symptoms were screened and SARS-CoV-2 RT-PCR was done based on individual assessment. | |
| Governmental strategies | Hospital gate screening (strengthened triage in the emergency room and at the main hospital entrance) | • A restricted number of hospital gates were opened. |
| • Fever, respiratory symptoms, and epidemiological relevance were screened at the entrance; a fever detector, structured reporting form, and a mobile application were used. | ||
| Specialized clinics for patients suspected to have COVID-19 | Two specialized clinics were put into operation outside the main hospital building during the COVID-19 pandemic. | |
| • Clinics for patients under investigation who had an epidemiological link with COVID-19. | ||
| • Clinics for patients with fever or respiratory symptoms. | ||
| Preemptive isolation of pneumonia patients | All patients with pneumonia were preemptively isolated; they were released only after negative confirmation of SARS-CoV-2 RT-PCR. | |
| High throughput diagnostic testing (RT-PCR) | Rapid testing enabled efficient operation of the insufficient isolation rooms. | |
| Strategies to reduce the hospital workload for COVID-19 | • Patients with a mild illness were guided to take SARS-CoV-2 RT-PCR tests at public health centers, not at hospitals. | |
| • Patients with mild laboratory-confirmed COVID-19 were cared for in residential treatment centers. | ||
| Telemedicine | Patients from COVID-19 outbreak areas were not permitted to visit the hospitals. Instead, they were counseled and prescribed medicine via telemedicine. | |
COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
In addition to providing enhanced education and training, most hospitals made it mandatory for hospital staff to wear masks, and only visitors wearing a mask were allowed to enter the hospital. In several hospitals in South Korea, with both the medical staff and patients wearing masks, secondary transmission did not occur even when infected patients stayed in the hospital for a long time (Lee and Jeong, 2020). Both the wearing of face masks and strict hand hygiene are essential for preventing the hospital spread of SARS-CoV-2.
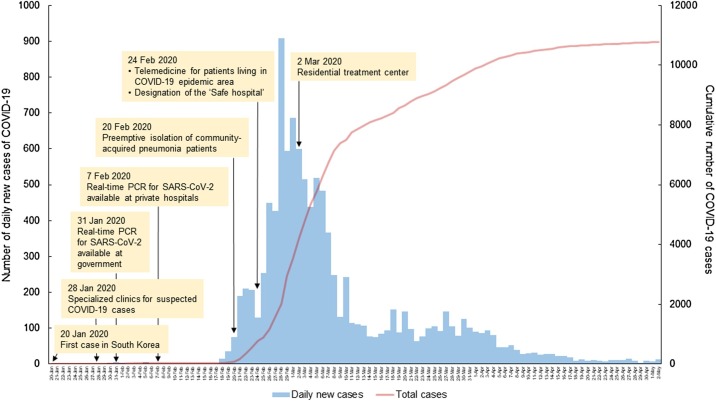
The government has introduced a number of sequential strategies to prevent COVID-19 inflow into hospitals and operate hospitals safely (Figure 1 ). First, as a quarantine measure for patients suspected of having COVID-19, gate screening (strengthened triage in the emergency room and at the main hospital entrance), specialized clinics, and preemptive isolation of pneumonia patients were conducted from early during the pandemic period (Kim et al., 2020). Two types of specialized clinic have been in operation outside the main hospital building during this COVID-19 pandemic: a clinic for febrile respiratory illness and a clinic for patients with an epidemiological link to the COVID-19 outbreak. Second, the real-time PCR (RT-PCR) test method was validated in collaboration with academia and industry, allowing each hospital to perform a large number of tests and enabling the efficient use of limited isolation rooms. Third, considering the possibility of cross-transmission when cases are concentrated in large hospitals all at one time, the inspection function of the public health center was strengthened and a residential treatment center was introduced to manage patients with mild COVID-19. In late February 2020 in South Korea, more than 500 cases of COVID-19 were reported daily, which was expected to reach unacceptable levels for the hospitals (Korea Ministry of Health and Welfare and Centers for Disease Control and Prevention, 2020). Thus, the first residential treatment center was opened on March 2, with further expansion to a total of 18 centers, which could accommodate 3500–4000 patients. As a result, hospitals could focus on the treatment of patients with severe COVID-19. Finally, telemedicine was introduced so that patients in COVID-19 outbreak areas could be treated without face-to-face contact with HCP. These strategies should be implemented in an integrated manner and shared with hospital staff and visiting patients.
Figure 1.
Timeline of the COVID-19 pandemic and safe hospital strategies in South Korea. A ‘safe hospital’ is a healthcare facility equipped with the infrastructure for infection control and prevention that meets the national standards: gate screening and separation of treatment areas between patients with respiratory illnesses and those with non-respiratory illnesses.
Funding source
No funding was provided for this manuscript.
Ethical approval
Ethical approval was not required.
Conflict of interest
We declare no conflict of interest.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2020.06.094.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Choi W.S., Kang C.I., Kim Y., Choi J.P., Joh J.S., Shin H.S. Clinical presentation and outcomes of Middle East Respiratory Syndrome in the Republic of Korea. Infect Chemother. 2016;48(2):118–126. doi: 10.3947/ic.2016.48.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y.J., Jeong Y.J., Kim S.H., Kim Y.J., Lee S.Y., Kim T.Y. Preparedness for COVID-19 infection prevention in Korea: a single-centre experience. J Hosp Infect. 2020;105(2):370–372. doi: 10.1016/j.jhin.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korea Ministry of Health and Welfare and Centers for Disease Control and Prevention . 2020. Updates on coronavirus disease 2019 (COVID-19): for press release. [Google Scholar]
- Lee J.K., Jeong H.W. Wearing face masks regardless of symptoms is crucial for preventing spread of COVID-19 in hospitals. Infect Control Hosp Epidemiol. 2020:1–4. doi: 10.1017/ice.2020.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael T.M., Currie D.W., Clark S., Pogosjans S., Kay M., Schwartz N.G. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382(21) doi: 10.1056/NEJMoa2005412. 2005-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nebehay S. Thomson Reuters; 2020. Over 90,000 health workers infected with COVID-19 worldwide — nurses group. [Google Scholar]
- CDC COVID-19 Response Team Characteristics of health care personnel with COVID-19—United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):477–481. doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.