Abstract
Background
The novel coronavirus (COVID-19) pandemic has become a enormous challenge for the health care facilitators. It has significantly affected the dental professionals in their clinical practices, hospitals and even dental schools. Due to the risk of cross – infection involved within in the dental setting, the dental professional is even scared to provide emergent treatment for a patient.
Aim
The aim of this comparative review is to throw light on the essential knowledge that a clinician must acquire before triaging a patient, understanding the case definition of COVID-19 and preparedness required before planning to re-open the dental practices.
Methodology
The updated database obtained from various governmental and non-governmental official webpages were rapidly analysed up till May 31, 2020.
Conclusion
This compilation of recommendations and guidance laid by various authorities across the world will function as a foundation for safer dental practice within the future.
Keywords: COVID-19, Triage, Re-opening, Guidance
1. Introduction
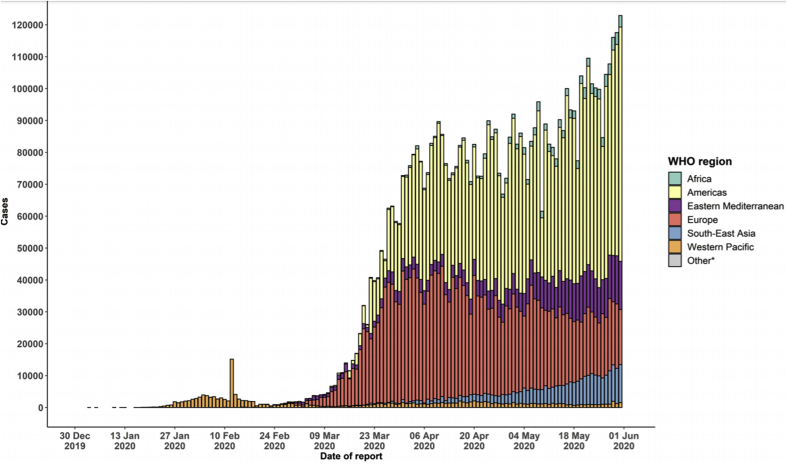
World Health Organization on January 30, 2020 declared the Recent outbreak as “Public Health Emergency of International Concern1” with the mortality rate to be as high as 3.4% as per to the currently published statistics.2 This pneumonia like viral disease which started from a small city of Wuhan, China gripped the entire globe and was announced a new name of COVID-19 on 11th February 2020.3 (See Fig. 1).
Fig. 1.
A screenshot of the data indicating the Number of confirmed COVID-19 cases, by date of report and WHO region, December 30, 2019 through June 1, 2020 (source: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200601-covid-19-sitrep-133.pdf?sfvrsn=9a56f2ac_4).
The Novel coronavirus as identified is a single-stranded RNA virus from a family of Coronaviridae.4,5 This family is known to be transmitted zoonotically from animals to humans.6 It includes severe acute respiratory syndrome coronavirus (SARS-CoV), which was first identified in 2002, and Middle East respiratory syndrome coronavirus (MERS-CoV), identified in 2012.7
With 216 countries being affected (CDC, May 31, 2020) and more than 5,934,936 confirmed cases with 367,166 deaths has been reported worldwide (WHO,May 31, 2020)8, this virus has caused a widespread public health concern.
The rapidly spreading infection typically transmits through respiratory droplets or by contact. It is also reported to be spread by contacting the inanimate object infected with droplets from an infected person.9 Dental treatments including aerosol generation, handling of sharps and proximity of the professional to patient's facial region predisposes them to high risk category of Covid-19 viral infection. Healthcare professional can also become carriers for infecting the subsequent patients visiting them making the dental office a hub of cross contamination.
Approaching to a stage of reopening our practices with the recommended guidelines and Standard Operating Procedures being laid, it is the responsibility of a Dental Health Care professional to confine and limit the spread of infection among the patients reporting to them for their dental treatment. Though it is recommended to adhere to the guidelines issued by native governance or Dental Council; it is also important to acknowledge protocol followed by the international sources to enhance one's practice.
Hence, we provide a brief comparative review by procuring recently published and accessible guidelines up to May 31, 2020, as we believe that the evolving understanding and the changing paradigm of the disease needs to be updated regularly for which we should familiarize ourselves to their source webpages.
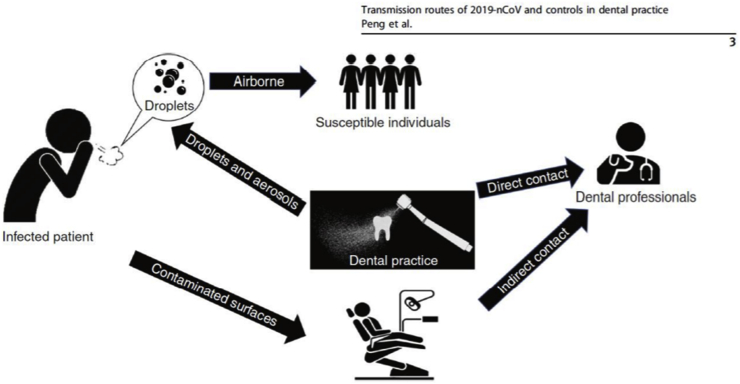
2. COVID-19 transmission in dental setting
COVID-19 is already been known to be transmitted from respiratory droplets from the infected person who coughs or sneezes or any person who comes in direct contact or touches the inanimate object infected from the respiratory secretion.9,10 As the dental professionals work in the intimacy of the oropharyngeal region, they have fairly higher chances of contracting the infection.11 It can also get transmitted to the next person visiting the dentist thus making the Dental Health Care professional a potential carrier for this infectious disease (See Fig. 2).
Fig. 2.
Figure depicting the transmission route possible for COVID-19 in dental practice and hospitals.
(Source: Peng, X., Xu, X., Li, Y. et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci 12, 9 (2020). https://doi.org/10.1038/s41368-020-0075-9).
3. What is triage?
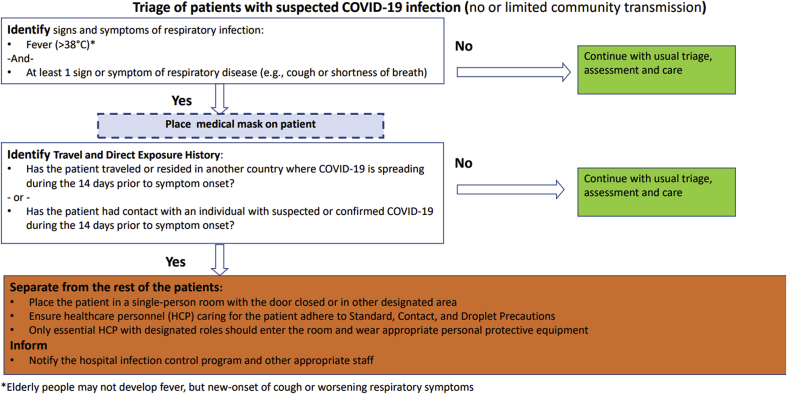
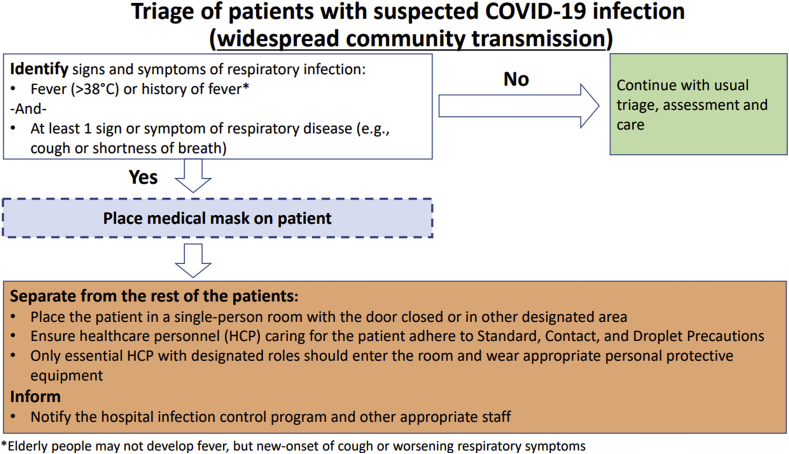
Centre for Disease Control and Prevention has defined triage as the sorting out and classification of patients or casualties to determine priority of need and proper place of treatment.12 During an outbreak of any infectious disease, triage is essentially important to sort patients likely to be infected with the pathogen of concern. The standard operating protocol of triaging the patient during COVID-19 pandemic does not replace the existing triaging of patients requiring emergency services in dentistry but it allows a professional to suspect a possible patient with COVID-19 which is still concealed/undermined (See Fig. 3, Fig. 4).
Fig. 3.
Triage Protocol by CDC in Countries with no or limited community transmission.
(Source: https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/sop-triage-prevent-transmission.html.
Fig. 4.
Triage protocol by CDC in Countries with widespread community transmission
(Source: https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/sop-triage-prevent-transmission.html.
3.1. Defining a case of COVID-19 as per to ECDC, updated on 29th May 2020.13
European Centre of Disease Control and Prevention has defined a case of COVID-19 based on the Clinical criteria.
Any person with at least one of the following symptoms:
-
⁃
Cough
-
⁃
Fever
-
⁃
Shortness of breath
-
⁃
Sudden onset of anosmia, ageusia or dysgeusia.
Symptoms including headache, chills, muscle pain, fatigue, vomiting and/or diarrhoea should also be noted.
Diagnostic imaging criteria: Any Radiological evidence showing lesions compatible with COVID-19.
Laboratory criteria: SARS-cov-2 nucleic acid detection in a clinical specimen.
Epidemiological criteria: At least one of the following two suspecting links:
-
•
Close contact with a confirmed COVID-19 patient in the 14 days before onset of any symptoms.
-
•
A resident or a staff member of a residential institution where ongoing COVID-19 transmission has been confirmed in the last 14 days prior to onset of symptoms.
Case are classified as:
-
1.
Possible case: Any suspect meeting the clinical criteria.
-
2.
Probable case: Any person meeting the clinical criteria with an epidemiological linkOR Any person meeting the diagnostic criteria.
-
3.
Confirmed case: Any case fulfilling the laboratory criteria.
Countries with no or limited community transmission (cases in the community are linked to known chain of transmission).
3.2. Initiation of reopening phase
All the governmental and non-governmental dental organizations have not only stressed the need for reopening the practices, but they also acknowledge that this requires a robust operational protocol to be stringently followed by the dental practitioners and staff to minimize the spread of Covid-19 disease. The rule and regulations announced by the governance should focus on the changed protocols and also to the present Covid-19 statistics present within the area. Practitioners are advised to follow carefully the evidence-based recommendations. An example of the return to office toolkit is already published from ADA - Return to Work Interim Guidance Toolkit published on 7th May 2020.14 This toolkit contains recommendations from the American Dental Association's (ADA's) Advisory Task Force on Dental Practice Recovery. Since it is provisional guidance, it is focused on the short-term management of dental practice during the COVID-19 pandemic as some offices plan to reopen and provide non-emergent care. It suggests dental healthcare workers to view infection control measures, air purification systems, and any other safety recommendations. Each dentist will need to assimilate his or her clinical judgment with own knowledge of the incidences of COVID-19 cases in respective areas, the needs of patients, and the availability of any necessary supplies to re-engage in the provision of elective dental care. A similar Return-to-Practice Office Manual have been provided to Corporate Member PDAs on Friday, May 29, 2020 mentioned in Royal college of Ontario's guidance on COVID-19: Managing Infection Risks During In-Person Dental Care as on May 31, 2020.15 On 12th May 2020, the National UK dental organizations joined forces agreed for a return to work guidance within the COVID-19 Future Planning Task Group after COVID-19 outbreak eases.16
3.3. Defined cases of Covid-19
All the following guidelines and paper have recommended triaging a patient into Covid-19 suspected or Covid-19 confirmed case and render the dental care accordingly. This screening is based on telephonic conversation and the screening form filled at the dental visit. Link to symptoms of Covid-19 has been provided by CDC- https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
Royal college of Ontario, Canada highlights COVID-19 Patient Screening Guidance Document prepared as per to WHO guideline of Covid-19 case definition. updated on 17th may 2020.15 Results of which categorises a person Covid-19 screen positive/negative however is not equivalent to a confirmed diagnosis of COVID-19. NHS recommend to adhere to Public Health England (PHE) which has given the current case definition for COVID-19, and provided guidance on testing and case reporting. As per to them Patients who are possible or confirmed COVID-19 patients – includes patients with symptoms (new, persistent cough or high temperature or anosmia (a loss of or change in your normal sense of smell or taste).17
3.4. Procedure of screening and referrals
Dental team should be able to screen and identify potential high-risk COVID-19 patients to prevent the spread of the infectious disease. Practitioner must suspect a potential case on the basis of questioning them for symptoms, history of travel and contact or any probable unusual history. The first screening should always be remote (videocall or telephonically) after which the needs of physical presence of the patient for treatment should be Evaluated. In-Person screening should always commence by recording temperature using a non-contact thermometer followed by a screening questionnaire to determine if they have had COVID-19 symptoms. American dental association toolkit has provided the screening set of questions to be asked a day prior and on the day of appointment to the patient.14 It allows referring the patient for testing in accordance with the list under “State and Territorial Health Department Websites for the specific area's information”. Australian Dental Council provides a pre-screening checklist to be evaluated before commencing treatment.18 Royal college in Ontario, Canada encourages a dental practitioner to go through “COVID-19 Patient Screening Guidance Document published on May 17, 2020” and refer any suspected cases to primary care provider or Telehealth Ontario.15 National Health Service, England highlights the dental team to ask for new, continuous cough, high temperature (37.8C or over), any member of the family having new, continuous cough or a high temperature? If the person or any member of the family has been tested positive for coronavirus? Anybody in self/household isolation period? And stresses to ask about a recently added symptom of Anosmia (a loss of or change in your normal sense of smell or taste). The paper on “guidance and standard operating procedure: delay phase” has also included a screening form for employees just like ADA toolkit. Every suspected case has been advised to contact NHS 111.
3.5. Retraining staff
It is mainly aimed at the personnel preparation to restart the practice with new changes. One of the drawback of healthcare profession is the lack of telehealth services. So, training and retraining of the staff to triage patient on remote consultation is must. Administrative staff should be trained for maintaining all the precaution possible in the screening, triage and waiting area such as hand hygiene, social distancing, use of facemask, for them and for the incoming patients. Ensuring to physiologically support the patient as well as the colleagues with morale boosting sessions. Training for working on rotation to avoid long working hours, all DHCP should be trained well for donning and doffing of the PPE. They should be also trained to rationally use PPE i.e., procedure specific and risk specific. The need of the hour is to Retrain all the dental professional and their team to adapt to the novel new system of patient care (See Table 1).
Table 1.
The Personal Protective Equipment for COVID-19 urgent Dental Care Setting.
(Source: National Health Service COVID-19 guidance and standard operating procedure Delay phase. Updated on May 18, 2020.).
| Waiting Room/Reception No Clinical Treatment |
Dental Surgery Non-AGP Treatment |
Dental Surgery Treatment involving AGPs |
|
|---|---|---|---|
| Good Hand Hygiene | YES | YES | YES |
| Disposable Gloves | NO | YES | YES |
| Disposable Plastic Apron | NO | YES | NO |
| Disposable Gown a | NO | NO | YES |
| Fluid Resistant Surgical Mask | YES | YES | NO |
| Filtering Face piece Respirator (FFP3)b | NO | NO | YES |
| Eye Protectionc | NO | YES | YES |
Fluid-resistant gowns (or long-sleeved waterproof apron) must be worn during aerosol generating procedures (AGPs). If non-fluid-resistant gowns are used, a disposable plastic apron should be worn underneath.
If wearing an FFP3 that is not fluid resistant, a full-face shield/visor must be worn.
Eye protection ideally should be disposable. If polycarbonate safety glasses/goggles or equivalent are used, they should be disinfected in line with manufacturers' guidance.
3.6. Tele-dentistry (voice/video consultation)
Newer technology like tele dentistry has not only helped in assistance in the current pandemic but has also made possible to partially or completely manage a patient at distances of kilometres away from the healthcare centre/clinic. It has served as an indispensable tool in triage all the patient before their physical evaluation. The entire process from networking, sharing digital information, distant and digital consultations, workup, and analysis is shared under a segment of the science concerned with dentistry known as “Tele dentistry”.19 Teleconsultation has gained a stronger foothold in the practice and has changed the outlook of dentistry towards a more pragmatic approach. Centre of disease control and prevention has advised to telephonically screen all patient consistent with symptoms of coronavirus. American dental association advises to follow CDC's Phone Advice Line Tool for Possible COVID-19 Tool20 for tele-triaging. However, the system still lacks using the tele dentistry for consultation in its full potential. Dental Council of India recommend to Telephonically schedule patients and triage them according to their need of dental care; i.e. Emergency, urgent and elective care.21 The guidelines also advices the dental team to follow up the health of the patient for 2 weeks post treatment for any symptoms of COVID-19.
3.7. Pharmaceutical leverage
It is advised in these times to first manage the patient by providing them primary care with three As: a. Advice; b. Analgesia; c. Antimicrobials (where appropriate). Scottish Dental Clinical Efficiency Program guidance on drugs can be followed for the management of dental problems during the COVID-19 pandemic.22 Dental council of India21 also guides a dental practitioner to provide the three A's wherever appropriate.
3.8. Defining emergency, urgency and routine procedure
CDC recommends the need of urgency to be based on clinician judgement and should be based on case-to case basis. The provision of what constitutes a dental emergency has been provided by “American Dental Association: What constitute a Dental Emergency”.23 ADA toolkit to return to practice does not prioritise the type of treatment, however ADA recognizes that as of May 1, 2020 the Centres for Disease Control (CDC) recommends postponement of elective procedures, surgeries, and non-urgent dental visits. COVID-19 risk or is a confirmed COVID-19 case. Royal college of Ontario, Canada has updated its members to resume for all the procedures as on may 22, 2020. However, the college also defines emergency, urgency and non-emergent care. Authorities has emphasised to limit the dental procedures to emergency cases and postpone non-urgent appointments and treatment.
Ministry of health and family welcome of India, NHS England in “COVID-19 guidance and standard operating procedure Delay phase” along with guidance from dental council of India has clearly defined emergent, urgent and non-emergent care. Australian dental council imposes level 1 restriction on its dentist which allows them to defer non-urgent treatment for people who meet the epidemiological or clinical symptom criteria for COVID-19 risk and provide Urgent dental treatment for people who meet epidemiological or clinical symptom criteria for COVID-19 risk or is a confirmed COVID-19 case. Royal college of Ontario, Canada has updated its members to resume for all the procedures as on may 22, 2020. However, the college also defines emergency, urgency and non-emergent care. Authorities has emphasised to limit the dental procedures to emergency cases and postpone non-urgent appointments and treatment.
Minimizing exposure to Staff and patients include all the guidance employed right from the preparedness of the staff to restarting the practice, it includes physically examining a patient to providing treatment under all infection control precaution possible. CDC suggests to ensure Hygiene practices, Technical changes for limiting Environmental spread of infection, Universal Source Control using Personal Protective Equipment (PPE), Sterilization and Disinfection of Patient-Care Items. It is also suggested to provide hydroxychloroquine prophylaxis to all asymptomatic healthcare workers involved in the care of suspected or confirmed cases of COVID-19 after medical consultation.
4. Conclusion
As the authorities are regularly updating their understanding for COVID-19, dental professionals should be better prepared and well versed with all the guidelines framed so far. This knowledge would enable clinician and their staff to suspect and identify a possible Covid-19 patient, the knowledge would be beneficial for them to refer such a case and also will be able to prioritise dental treatment for their patients which is the need of the moment. Hence, it is the right time to learn and relearn the ineluctable updated standard of operating protocols.
5. Significance of the paper
It is important to acknowledge protocol followed by the international agencies to enhance one's practice. Thus, we provide a brief comparative review by procuring recently updated guidelines up to may 31, 2020, with which we advise the dental practitioner to update regularly the evolving and changing paradigm of this disease.
Contributor Information
Mousumi Goswami, Email: mousumi_leo@yahoo.co.in.
Sakshi Chawla, Email: sakshichawla21@yahoo.co.in.
Appendix 1. Comparative compilation of Published and Accessible Recommendations on Triage before Re-opening of dental services updated upto May 31, 2020. It is sourced from the various Governmental and Non-governmental organizations working across the globe
| Source | Initiation of Reopening phase | Defined cases of Covid-19 | Procedure of Screening and referrals | Retraining staff | Tele-dentistry (voice/video consultation) | Pharmaceutical leverage | Defining emergency, urgency and routine procedure | Minimizing exposure – Staff, patients. | Defining allowed procedures |
|---|---|---|---|---|---|---|---|---|---|
| Country: USA Source: Centre of disease control & Prevention. Guidance for Dental Settings: Interim Infection Prevention and Control Guidance for Dental Settings During the COVID-19 Response Updated on May 19, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html |
– | Link to symptoms consistent with Covid-19. Https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html |
Refer the patient to a medical facility, or call 911 | Provide (Dental healthcare professional)DHCP with job- or task- specific education and training on preventing transmission of infectious agents, including refresher training. Ensure that DHCP are educated, trained, and have practiced the appropriate use of PPE prior to caring for a patient. |
Telephone screen all patients for symptoms consistent with COVID-19. If the patient reports symptoms of COVID-19, avoid non-emergent dental care. Delay dental care until the patient has recovered. Telephone triage all patients in need of dental care. | None | The urgency of a procedure is a decision based on clinical judgement and should be made on a case-by-case basis. American Dental Association: What Constitutes a Dental Emergency Https://success.ada.org/~/media/CPS/Files/Open%20Files/ADA_COVID-1919_Dental_Emergency_DDS.pdf?_ga = 2.253879752.110187285.1584496315–1622146531.1565271894 |
Engineering Controls Hygiene Universal Source Control Using Personal Protective Equipment (PPE) Environmental Infection Control Sterilization and Disinfection of Patient-Care Items. |
– |
| Country: USA Source: American Dental Association, USA Return to Work Interim Guidance Toolkit May 7, 2020 |
Return to Work Interim Guidance Toolkit May 7, 2020 |
– | Screening form provided to be filled a day prior and on the appointment day. Positive responses → deeper discussion with the dentist before proceeding with elective dental treatment. Referral should see list of State and Territorial Health Department Websites for specific area's information. Also include employee's screening chart. |
None | Follow CDC's Phone Advice Line Tool for Possible COVID-19 Tool for tele-triaging. Https://www.cdc.gov/coronavirus/2019-ncov/hcp/phone-guide/index.html. The toolkit does not talk about tele consultation. |
None | The toolkit does not elaborate triaging the patient and the type of treatments to be prioritized. The ADA recognizes that as of May 1, 2020 the Centre for Disease Control (CDC) recommends postponement of elective procedures, surgeries, and non-urgent dental visits. |
Front desk staff can wear masks and goggles, or face shields, or offices can install a clear barrier. Keep staff level in operatory to the minimum required along with the implication of other Infection control protocols. |
– |
| Country: India Source: Ministry Of Health and Family Welfare, India |
Closed in the CONTAINMENT ZONE; In the RED ZONE, Emergency dental procedures can be performed. ORANGE AND GREEN ZONE- dental consults, Emergency and Urgent treatment procedures only. |
– | Telephone screening is encouraged as the first point of contact between the patient and the dentist or reception office is encouraged | Train administrative personnel working in the reception of patients on hand hygiene, social distancing, use of facemask, for them and incoming patients. Educate all HCW on proper selection and use of PPE. Psychological support and morale-boosting. Staff should rotate to avoid long working hours, should ensure proper nutrition and sleep. All staff and dentist must use surgical attire in the dental office, and all personal clothing should be avoided. |
Telephone screening Current medical history and past history particularly pertaining to symptoms of Severe Acute Respiratory Illness (fever AND cough and/or shortness of breath) or All symptomatic ILI (fever, cough, sore throat, runny nose). |
None | Emergent→ Fast spreading infections of facial spaces/Ludwig Angina/Acute cellulitis of dental origin/Acute Trismus. Uncontrolled bleeding of dental origin. Severe uncontrolled dental pain, not responding to routine measures. Trauma involving the face or facial bones. Urgent Care: Children→ Acute Pulpitis, Dental abscess, Dentoalveolar trauma, Pain of cavitation needing temporization, Unavoidable Dental Extractions. Adults→ Pain of pulpal origin not controlled by Advice, Analgesics, Antibiotics (AAA), Acute dental abscess of pulpal/periodontal/endo-perio origin/Vertical fracture teeth, Completion of ongoing root canal treatment (RCT) Temporization of cavitation approximating pulp, Broken restoration/fixed prosthesis causing sensitivity of vital teeth/endangering to pulpitis/significant difficulty in mastication, Unavoidable Dental Extractions/Post extraction complications, Already prepared teeth/implant abutments to receive crowns, Peri-implant infections endangering stability, Pericoronitis/Operculectomy, Oral mucosal lesions requiring biopsy, Long-standing cysts and tumours of the jaw with abrupt changes, Sharp teeth/Trigeminal neuralgia, Orthodontic wire or appliances, piercing or impinging on the oral mucosa, Orthodontic treatment causing Iatrogenic effects, Delivery of clear aligners, Patients on skeletal anchorage |
All asymptomatic healthcare workers involved in the care of suspected or confirmed cases of COVID-19 are advised to take HCQ prophylaxis after medical consultation. Display visual alerts at the entrance of the facility and in strategic areas (e.g., waiting areas or elevators) about respiratory hygiene, cough etiquette, social distancing and disposal of contaminated items in trash cans. Appropriate PPE and ensure it is accessible to HCW. For appointments that do not result in aerosols, and need examination only wear a triple layer surgical mask and protective eyewear/face shield and gloves. Wear N95 face masks, protective eyewear/face shields and gloves along with coverall for High Risk and very high-risk procedures. To increase the shelf life of N95 masks, cover them with a surgical mask and discard only the surgical mask. When examining moderate risks patients the treating doctor will require all PPE as high risk except that the coveralls can be substituted with surgical gowns. Practice non-aerosol generating procedures. Encourage rubber dam. The 4-handed technique is beneficial for controlling the infection. Encourage all to download the Arogya Setu App. |
– |
| Country: India Source: Dental Council of India. Updated: May 7, 2020 |
Opening of Dental practice should be based on directions as per orders of the local administration. | – | Screening th patients by asking the symptoms of coronavirus. Referral should be made to government hospital or designated hospital. |
Train and retrain workers on how to follow established protocols. | Telephonically appoint patients and triage them according to their level of dental care; i.e. Emergency, urgent and elective care. | Primary care dental triage should focus on the provision of the three as: a. Advice; b. Analgesia; c. Antimicrobials (where appropriate). | EMERGENCY (Situations which increase the patient's death risk) • Uncontrolled bleeding. • Cellulitis leading to intra-oral or extra-oral edemas, and potential risk of damage to airways • Facial bones trauma, which may damage the patient's airways. URGENT (situations which require priority care but do not increase the patient's death risk) • Acute dental pain (Pulpitis). • Pericoronitis. • Alveolitis. • Dental or periodontal abscesses. • Dental care needed for another critical medical procedure. • Cementation fixed prosthodontics or crowns. • Biopsies. • Adjustments of orthesis and prosthesis that cause pain and compromise chewing function. • Changing intracanal medication. • Removal of extensive dental caries or restorations that cause pain. • Mucositis. • Dental trauma with avulsion or luxation. |
Dentists should take strict personal protection measures and avoid or minimize operations that can produce droplets or aerosols. Four-handed technique is beneficial for controlling infection. The use of saliva ejectors can reduce the production of droplets and aerosols. |
– |
| Country: Australia Source: Australian Dental Council Updated on may 8, 2020 Https://www.dentalboard.gov.au/News/2020-05-08-COVID-19-update-to-dental-practitioners-8-May.aspx Rest of the precaution is followed as per to “Managing COVID-19 guideline”, Last updated on March 25, 2020. |
May 7, 2020 AHPPC agreed to moving dental practice to level 1 restrictions. |
– | Provided a pre-screening checklist. | Training the team on how to screen for patients at risk of COVID-19. | Call all patients the day prior to the planned appointment and ask ➢ Returned from overseas or interstate travel in the past 14 days ➢ Felt unwell, including but not limited to symptoms of COVID-19 such as fever, cough, sore throat or shortness of breath ➢ had any contact with a confirmed or suspected case of COVID-19 in the past 14 days. |
None | Level 1 Restrictions imply: Defer non-urgent treatment for people who DO meet epidemiological or clinical symptom criteria for COVID-19 risk. Urgent dental treatment for people who DO meet epidemiological or clinical symptom criteria for COVID-19 risk or confirmed as a COVID-19 case. |
20–30 s pre-procedural mouth rinse with either: • 1% hydrogen peroxide • 0.2% povidone iodine • 0.2% chlorhexidine rinse (alcohol free) • an essential oil mouth rinse (alcohol free) | All dental treatments using standard precautions for people who do not meet epidemiological or clinical risk factors for COVID-19 infection transmission. |
| Country: Canada Source: Royal college of Ontario, Canada. COVID-19: Managing Infection Risks During In-Person Dental Care May 31, 2020 |
Return-to-Practice Office Manual have been provided to Corporate Member pdas on Friday, May 29, 2020. | COVID-19 Patient Screening Guidance Document prepared as per to who guideline of Covid-19 case definition. Updated on may 17, 2020. Results of which categorises a person Covid-19 screen positive/negative however is not equivalent to a confirmed diagnosis of COVID-19. |
COVID-19 Patient Screening Guidance Document published on May 17, 2020. Refer to suspected cases should be made to primary care provider or Telehealth Ontario |
Dentists must ensure that clinical staff are trained in and use proper donning and doffing procedures for PPE. | Dentists must ensure that patients are triaged and appointments are scheduled by phone or via tele dentistry (not in person or via walk-in). | None | Though the practice has resumed for all the procedures. may 22, 2020 update categorized: Emergency →oral-facial trauma • cellulitis or other significant infection, especially if compromising the patient's airway • prolonged bleeding • pain that cannot be managed by over-the counter medications. Urgency → severe dental pain from pulpal inflammation • pericoronitis or third-molar pain • surgical post-operative osteitis, dry socket dressing changes • abscess or localized bacterial infection resulting in localized pain and swelling • tooth fracture resulting in pain, pulp exposure or causing soft tissue trauma • extensive caries or defective restorations causing pain • dental trauma with avulsion/luxation • final crown/bridge cementation if the temporary restoration is lost, broken or causing gingival irritation • biopsy of a suspicious oral lesion or abnormal oral tissue • replacing a temporary filling in an endodontic access opening for patients experiencing pain • snipping or adjusting an orthodontic wire or appliance piercing or ulcerating the oral mucosa • treatment required before critical medical procedures can be provided • suture removal • denture adjustments or repairs when function is impeded • other procedures that in the dentist's professional judgement are necessary in order to minimize harm to patients and/or relieve pain and suffering. Non-emergent care → recall examinations and routine radiographs • routine dental cleanings and preventive therapies • orthodontic procedures other than those to address acute issues (e.g. Pain, infection, trauma) • extraction of asymptomatic teeth • restorative dentistry, including treatment of asymptomatic carious lesions • cosmetic dental procedures, including teeth whitening. |
Dentists should post signage in common areas (e.g., at the main entrance and in the waiting area) communicating relevant expectations for patients, including any requirements for: a. Hand hygiene (e.g., a requirement to wash and/or sanitize hands upon entry to the practice); b. Respiratory hygiene (e.g., a requirement to wear a mask within the practice); and c. Physical distancing (e.g., a requirement to maintain a minimum distance of 2 m, except as required for the provision of care). 15 Dentists should also post signage at the entrance to the office and at reception describing the signs and symptoms of COVID-19. Dentists are advised to consider installing physical barriers at key contact points to reduce the spread of droplets, including reception (e.g., a plexiglass shield). |
Dentists are permitted to provide in-person care for all deferred, non-essential, and elective services, in addition to emergency and urgent care. |
| Country: United Kingdom Source: National Health Survey, United Kingdom. COVID-19 guidance and standard operating procedure Delay phase. Updated May 18, 2020. |
The provision of all routine, non-urgent dental care including orthodontics has been stopped in England until further notice. The reopening task has not yet begun. |
Public Health England (PHE) has defined the current case definition for COVID-19, and provided guidance on testing and case reporting. Link from the parent article is provided. Patients who are possible or confirmed COVID-19 patients – including patients with symptoms (new, persistent cough or high temperature or anosmia (a loss of or change in your normal sense of smell or taste). |
Screening Do you have a new, continuous cough? Do you have a high temperature (37.8C or over)? Does anyone in your household have a new, continuous cough or a high temperature? If you or anyone in your household has tested positive for coronavirus, are you still in the self/household isolation period? Anosmia (a loss of or change in your normal sense of smell or taste). |
Dental care professionals working in urgent care settings should be trained in all aspects of infection prevention and control (IPC) and fully familiar with HTM01 05 for decontamination. Training should include donning (putting on) and doffing (taking off) PPE. | Under SOP remote management: Remotely (eg by telephone or video link) risk assess and triage those patients contacting the service for urgent dental care, to determine patient group, urgency of dental problem and associated UDC needs. | Advice, analgesia, antimicrobials where appropriate. SDCEP guidance on drugs for the management of dental problems during the COVID-19 pandemic. http://www.sdcep.org.uk/published-guidance/acute-dental-problems-Covid-19/. |
Life-threatening emergencies, eg airway restriction or breathing/swallowing difficulties due to facial swelling • trauma including facial/oral laceration and/or dentoalveolar injuries, for example avulsion of a permanent tooth • oro-facial swelling that is significant and worsening post-extraction bleeding that the patient cannot control with local measures dental conditions that have resulted in acute and severe systemic illness • severe dental and facial pain: that is, pain that cannot be controlled by the patient following self-help advice • fractured teeth or tooth with pulpal exposure dental and soft tissue infections without a systemic effect suspected oral cancer • oro-dental conditions that are likely to exacerbate systemic medical conditions. | Keep staff safe through regular risk assessments. As few staff as possible should be allocated to see patients, particularly those shielded, to minimize contacts without compromising the safe delivery of care. |
|
| Country: MALTA, Europe. Source: Guidance for Dental Practices in Malta - COVID-19 March 18, 2020 |
– | None | Screened using a forehead thermometer, instructed to use alcohol hand rub. The questions should confirm once again whether over the previous 14 days clients have: − been abroad or close contact with any patient presenting respiratory symptoms, − been in contact with anyone who has developed COVID-19 − themselves had any symptoms of coughing/fever/shortness of breath during the past fortnight. Referral to 111. |
Clearly define tasks and support each other to ensure that duties are carried out safely and responsibly | Patients should be contacted over the phone and evaluated for Covid-19 status. | None | Limit dental procedures to emergency cases and postpone non-urgent appointments and treatment. | Clinicians should wear PPE which includes disposable surgical masks, protective eyewear/face-shields and disposable gloves. Practise four-handed dentistry. Hand-pieces used should be anti-retraction handpieces. Hand instrumentation. Pre-rinse with 1% hydrogen peroxide or 0.2% povidone. |
Limit dental procedures to ones that do not create aerosols and airborne particles |
| Country: SINGAPORE Source: MOH circular 132/2020 gradual resumption of dental services after Covid-19 circuit breaker period Updated: May 21, 2020 |
PHASE ONE (“SAFE RE-OPENING”) from 1st June Non-essential dental services which were deferred can also resume in a controlled and gradual manner. |
– | – | – | Physical visits should continue to be avoided where possible | – | Not defined, MOH has instructed healthcare providers to triage and prioritise the resumption of services for patients or clients with more urgent medical needs first. |
Clinic staff, as employees of the dental clinic, should be equipped with the appropriate Personal Protective Equipment (PPE) while continuing to provide care to all patients. Four-handed dentistry. Workplaces and services that are in operation are required to deploy Safe Entry to log the check-in of employees and visitors. Staff with mobile phones are also encouraged to download and activate the Trace Together app |
Aerosol generating procedures (agps) present a higher risk of transmission of the virus and should only be undertaken where no other option is available. The use of hand instrumentation should be highly prioritized. |
References
- 1.World Health Organization Novel coronavirus(2019-nCoV) 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200130-sitrep-10-ncov.pdf?sfvrsn=d0b2e480_2 Situation Report - 10.
- 2.Sohrabi C., Alsafi Z., O'Neill N. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Novel coronavirus(2019-nCoV) 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200211-sitrep-22-ncov.pdf?sfvrsn=fb6d49b1_2 Situation Report - 22.
- 4.Chen Z., Fu J., Shu Q. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World Journal of Pediatrics. 2020:1–7. doi: 10.1007/s12519-020-00345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mackenzie J.S., Smith D.W. COVID-19: a novel zoonotic disease caused by a coronavirus from China: what we know and what we don’t. Microbiol. Aust. 2020;41(1):45–50. doi: 10.1071/MA20013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan J.F., Yuan S., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Novel coronavirus(2019-nCoV) 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200531-covid-19-sitrep-132.pdf?sfvrsn=d9c2eaef_2 Situation Report - 132.
- 9.World Health Organization . World Health Organization; Geneva, Switzerland: 2019. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations.https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations [Google Scholar]
- 10.The Chinese Preventive Medicine Association An update on the epidemiological characteristics of novel coronavirus pneumonia (COVID-19) Chin J Epidemiol. 2020;41(2):139–144. doi: 10.3760/cma.j.issn.0254-6450.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 11.Peng X., Xu X., Li Y. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Standard operating procedure (SOP) for triage of suspected COVID-19 patients in non-US healthcare settings: early identification and prevention of transmission during triage. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/sop-triage-prevent-transmission.html
- 13.European Centre for Disease Prevention and Control Case definition for coronavirus disease 2019 , ( COVID-19) https://www.ecdc.europa.eu/en/Covid-19/surveillance/case-definition as of 29 May 2020.
- 14.American Dental Association Return to work Interim guidance toolkit. https://www.ada.org/en
- 15.COVID-19: managing infection risks during in-person dental care may 31. 2020. https://www.rcdso.org/en-ca/rcdso-members/dispatch-magazine/articles/5350
- 16.National dental organisations join forces to agree return-to-work guidance. https://cgdent.uk/2020/05/12/national-dental-organisations-join-forces-to-agree-return-to-workguidance/
- 17.Guidance COVID-19 : investigation and initial clinical management of possible cases updated on 22 May 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-initial-investigation-of-possible-cases/investigation-and-initial-clinical-management-of-possible-cases-of-wuhan-novel-coronavirus-wn-cov-infection
- 18.Australian Dental Council COVID-19: elective surgery and infection prevention and control precautions. https://www.safetyandquality.gov.au/publications-and-resources/resource-library/covid-19-elective-surgery-and-infection-prevention-and-control-precautions
- 19.Mihailovic B., Miladinovic M., Vujicic B. Telemedicine in dentistry (teledentistry) In: Graschew G., Roelofs T.A., editors. Advances in Telemedicine: Applications in Various Medical Disciplines and Geographical Areas 2011. InTech; Rijeka (Croatia): 2011. pp. 215–230. [Google Scholar]
- 20.Centre for disease Control & Prevention Phone advice line tool for possible COVID- 19 patients. https://www.cdc.gov/coronavirus/2019-ncov/hcp/phone-guide/index.html
- 21.Dental Council Of India Advisory :dental clinics protocols. http://dciindia.gov.in/Admin/NewsArchives/Dental%20Clinics%20Protocols%20Final.pdf
- 22.Scottish dental clinical efficiency Program guidance on drugs. http://www.sdcep.org.uk/published-guidance/acute-dental-problems-Covid-19/
- 23.American dental association: what constitutes a dental emergency. https://success.ada.org/media/CPS/Files/Open%20Files/ADA_COVID19_Dental_Emergency_DDS.pdf