Abstract
Background:
Ambulation is an essential aspect of daily living and is often impaired after brain and spinal cord injuries. Despite the implementation of standard neurorehabilitative care, locomotor recovery is often incomplete.
Objective:
In this randomized, sham-controlled, double-blind, parallel design study, we aimed to determine if anodal transcutaneous spinal direct current stimulation (anodal tsDCS) could improve training effects on locomotion compared to sham (sham tsDCS) in healthy subjects. Methods: 43 participants underwent a single backwards locomotion training (BLT) session on a reverse treadmill with concurrent anodal (n = 22) or sham (n = 21) tsDCS. The primary outcome measure was speed gain measured 24 h post-training. We hypothesized that anodal tsDCS + BLT would improve training effects on backward locomotor speed compared to sham tsDCS + BLT. A subset of participants (n = 31) returned for two additional training days of either anodal (n = 16) or sham (n = 15) tsDCS and underwent (n = 29) H-reflex testing immediately before, immediately after, and 30 min post-training over three consecutive days.
Results:
A single session of anodal tsDCS + BLT elicited greater speed gain at 24 h relative to sham tsDCS + BLT (p = 0.008, two-sample t-test, adjusted for one interim analysis after the initial 12 subjects). Anodal tsDCS + BLT resulted in higher retention of the acquired skill at day 30 relative to sham tsDCS + BLT (p = 0.002) in the absence of significant group differences in online or offline learning over the three training days (p = 0.467 and p = 0.131). BLT resulted in transient down-regulation of H-reflex amplitude (Hmax/Mmax) in both test groups (p < 0.0001). However, the concurrent application of anodal-tsDCS with BLT elicited a longer lasting effect than sham-tsDCS + BLT (p = 0.050).
Conclusion:
tsDCS improved locomotor skill acquisition and retention in healthy subjects and prolonged the physiological exercise-mediated downregulation of excitability of the alpha motoneuron pool. These results suggest that this strategy is worth exploring in neurorehabilitation of locomotor function.
Keywords: tsDCS, Transcutaneous spinal direct current, stimulation, Locomotor recovery, Backwards locomotion, Motor learning, Gait, Hoffman reflex
Introduction
Deficits in locomotor function are common after central nervous system (CNS) injury, leading to comorbidities such as increased risk of falls, fractures, and decline in mobility [1]. Despite rehabilitation geared at improving gait, locomotor recovery is often incomplete. Hence, it would be important to develop strategies to improve the beneficial effects of training on the rate of acquisition and retention of locomotor learning.
Over the last two decades, transcranial direct current stimulation (tDCS) of the brain has been recognized as a neuromodulatory strategy to enhance training effects that result in better upper limb skill acquisition, particularly when applied for more than one session concurrently with behavioral training [2–9]. Previous work on the effects of tDCS on locomotion and lower extremity function has been inconclusive, possibly due to the limitation of transcranial tDCS to stimulate the leg representation of the motor cortex or to reach subcortical locomotor networks [10–14].
Direct current stimulation applied over the spine (tsDCS) modulates segmental spinal physiology, ascending lemniscal and nociceptive pathways [15–20] and activity in supraspinal centers [21–28]. Computer modeling of currents elicited by tsDCS with an electrode over T-11 provided mechanistic foundation to these empirical findings [29–32]. It is then possible that tsDCS could also influence locomotor learning. Here, we elected to use backward walking both as a training paradigm and for outcome assessment. Backward walking and running are used in sports conditioning programs and rehabilitation, and provide a relatively unfamiliar environment for subjects to engage in the acquisition of a new locomotor skill [33,34].
Herein, we evaluated the influence of tsDCS on backwards locomotor learning (tsDCS + BLT) in a randomized sham-controlled, double-blind, parallel study design. We hypothesized that anodal tsDCS + BLT would result in improved backward locomotion performance (change in speed) relative to sham tsDCS + BLT. H-reflex testing was carried out to gain insight into potential effects of tsDCS on the excitability of the alpha motoneuron pool.
Methods
Participants
Forty-three healthy volunteers (24 women and 19 men; mean age ± SD, 25.9 ± 4.8 years) with no history of neurological disorders were enrolled in the study. Written informed consent was obtained from all subjects prior to inclusion. The protocol, where the primary endpoint measures and working hypothesis were preregistered, was approved by the Neuroscience Investigational Review Board at the National Institutes of Health. To comply with the inclusion criteria, participants were required to abstain from intake of neurostimulants (i.e., amphetamines, dextroamphetamine/amphetamine, methylphenidate, modafinil), antidepressants (i.e., selective serotonin reuptake/serotonin and norepinephrine reuptake inhibitors, tricyclic antidepressants, and atypical antidepressants), depressors of the central nervous system (i.e., benzodiazepine, antiepileptics), or recreational drugs for at least 6 months prior to the study. Additionally, subjects were asked to avoid alcohol or caffeine for 48 h preceding participation, for the duration of the training and for the 48 h preceding day-30 test (Fig. 1). Subjects were excluded if they had a history of recreational backwards locomotion, or similar past experiences such as walking tour guides, marching band participants, or line backers.
Fig. 1.
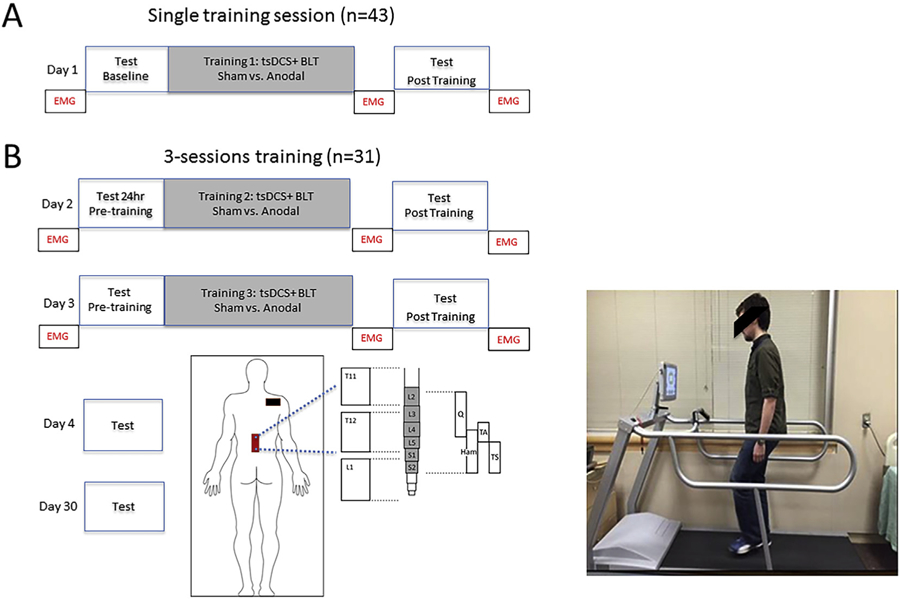
Methods. Experimental setup: Two groups underwent 20 min of backwards locomotion training (BLT) with concurrent sham or anodal transcutaneous spinal direct current stimulation (tsDCS), applied over T-11/12 (red rectangle) and cathode electrode placed over the right shoulder (black rectangle). A: one day of BLT training, B: Training over three consecutive days. 24 h test in panel A was the same behavioral determination as Test Pre-Training on Day 2 in panel B. EMG indicates the timing of soleus H-reflex testing, at baseline, immediately after, and 30 min post-training on Days 1–3. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Experimental design
Subjects
Group assignments were made prior to study enrollment to match groups for general physical activity level (Short Questionnaire to Assess Health-enhancing physical activity) [35], age, and gender (Table 1). By design, both the experimenter and participants were blind as to the stimulus condition (anodal tsDCS or sham tsDCS). At the end of the experiment, participants were asked to guess their group assignment as well as answer a safety and tolerability questionnaire (Suppl Table 1) regarding general discomfort, pain, burning and itching, using a 1–10 analog scale.
Table 1.
Baseline characteristics of the study participants.
| Characteristics | Stimulation Type |
p-value | |
|---|---|---|---|
| Sham tsDCS + LT (N = 21) | Anodal tsDCS + LT (N = 22) | ||
| Gender | |||
| Male | 9 | 10 | 0.87 |
| Female | 12 | 12 | |
| Activity Level (SQUASH*) | |||
| Above Average | 5 | 3 | 0.63 |
| Average | 12 | 15 | |
| Below Average | 4 | 4 | |
| Age-yr | 25.3 ± 4.7 [20–39] | 26.5 ± 4.9 [19–37] | 0.41 |
| Height-inches | 66.9 ± 3.46 | 67.6 ± 3.73 | 0.56 |
Short Questionnaire to Assess Health-Enhancing Physical Activity: based on average daily activities 2 months.
Forty-three participants underwent a single backwards locomotion training session on a reverse treadmill with concurrent anodal (n = 22) or sham (n = 21) tsDCS. (Fig. 1). An interim analysis was carried out after the first twelve subjects completed a single training session. To evaluate the effects of additional training sessions, a subset of the 43 participants (N = 31) returned for two additional training days of anodal (n = 16) or sham (n = 15) tsDCS. Thus, all 43 subjects completed a single training session with anodal or sham tsDCS. Thirty-one of them completed three training sessions with anodal or sham tsDCS (Fig. 1).
Backwards locomotor training
At the beginning of the experiment, subjects were familiarized with backwards walking on the treadmill at a comfortable pace of 1.5 mph for 1 min. After the familiarization, the testing was carried out as follows: subjects were instructed to walk backwards without running or holding on to the safety handrails at increasing speed for 2 min (initial speed was 1.5 mph). Every 5 s subjects had to decide if they opted whether to increase speed by +0.2 mph, by +0.1mph, stay the same, or decrease by-0.1mph (if they felt uncomfortable). The maximal possible treadmill speed was 4.5 mph. Test measurement, the average speed over the 2 min period, was recorded at baseline, 20 min post-training, 24 h after each training day and at Day 30.
These time points were determined a priori. To reduce possible confounders between testing sessions, participants were instructed not to practice walking backwards between each day of training, and at end of testing and the 30-day follow-up. To avoid diurnal variations, testing was performed at the same time period each day. In addition to speed, we measured step length, a kinematic measure that has implications for the stability of gait and is decreased with aging and after brain lesions [36,37]. Study participants data were collected from a Gait Trainer 3 Biodex Software USA and stored for offline analysis. One participant did not return for testing on day 30 in the sham group. Data from another subject on Day 30 in the tsDCS group was corrupted.
Training protocol
In each training session, subjects walked backwards for 20 min at 70% of their baseline speed. Although treadmill safety handrails and an emergency stop button were available in case of sudden imbalance or danger, these safety measures were never activated by any participant during the study.
Transcutaneous spinal direct current stimulation (tsDCS)
tsDCS (2.5 mA, 20 min) was delivered from a battery-driven programmable direct current stimulator (Soterix USA) connected to surface electrodes (saline-soaked synthetic sponge of 7 × 5 cm, 35 cm2 and 0.6 mm depth). The anode/sham electrode was centered on the T-11 spinous process of the thoracic spine with the major axis parallel to the spinal cord, a location that modulates segmental spinal reflex excitability. The second electrode was placed over the right shoulder [15,16,21,38](Fig. 1). A tsDCS lumbar body strap (Soterix, USA) was used to secure electrode positioning in place. Computerized modeling of this electrode montage and stimulation parameters induce a current density of 0.071 mA/cm2 delivering a total charge density of 85.7 mC/cm2 [16], which is well within safety levels [39,40]. The stimulator was programmed to ramp up current to 2.5 mA over a 30-s period and similarly ramped down at the end of the stimulation. Sham tsDCS was achieved by delivering a 2.5-mA current over a period of 30 s at the beginning and end of the stimulation period [41].
Soleus H-reflex testing
A subset of twenty-nine participants (13 sham tsDCS, and 16 anodal tsDCS) underwent three consecutive days of soleus H-reflex testing. Testing was performed at baseline, immediately after, and 30 min post-training (Fig. 1). Subjects lay in a prone position on a standard hospital bed, with the hip at (~180°), the knee flexed (~150°), and the ankle at plantar flexion (~100°). Surface electromyography (EMG) was recorded from the left soleus muscle using a pair of surface Ag–AgCl disposable electrodes (3 M Health Care, St. Paul, MN) in a belly-tendon configuration. EMG was recorded on an electromyograph (Nihon Koden, Irvine, CA) with band-pass filters of 20 Hz to 1 kHz, and concurrently digitized for off-line analysis (Power 1401, Cambridge Electronics Design, Cambridge, UK) by blinded examiners. H-reflexes were elicited via electrical stimulation of the posterior tibial nerve in the popliteal fossa using a custom-made spherical ball electrode using constant-current square-wave pulses of 1-ms duration with a remote anode on the medial knee. A stimulation frequency of 0.1 Hz was used to allow ample time for resolution of post-activation depression [42]. The electrodes were applied and securely taped and wrapped at the start of each testing session, to limit movement during locomotor training. Additionally, a permanent marker and bandage were applied at the end of sessions 1 and 2 to limit the variability of electrode placement in subsequent sessions. At the beginning of each experiment, stimulus thresholds for eliciting the H-reflex and M-wave were determined, defined as the lowest stimulus intensity needed to produce 100 µV peak-to-peak responses. To generate the stimulus-response curve of the Sol H reflex, the stimulus intensity was progressively increased in steps of 0.02–0.10 mA, from the H reflex sub-threshold until the maximum M-wave peak (Mmax) was reached. At least two stimuli were delivered at each intensity during the steep portion of the H-reflex curve. If the same stimulus intensity produced a varied response, a third stimulus was delivered. 33–58 stimuli were used to generate each recruitment curve over a 5–10min period.
Soleus H-Reflex Data Analysis:
Peak-to-peak H and M-amplitudes were measured on non-rectified EMG traces using Signal software (CED, Cambridge, UK). H-reflex amplitudes were expressed as a percentage of Mmax, and stimulation intensities were normalized to the M-wave threshold (MT) at baseline. H/Mmax amplitudes were plotted against stimulus strength (intensity x MT), to generate the recruitment curve. The ascending portion of the recruitment curve was analyzed using a non-linear fit function (Sigmoidal fit, Prism Software, GraphPad Software, Inc. La Jolla, CA) to determine Hmax, or the highest point on the recruitment curve. Data sets for each testing period (baseline, PT1, 30 min PT1, Day 2 baseline, PT2, etc …) were subsequently normalized to baseline values. Three participants from the sham group were excluded from analysis due to poorly defined H reflexes.
Statistical analysis
Locomotor function:
Statistical analysis was performed using SAS/STAT Statistical Software version 9.2 (SAS Institute Inc., Cary, NC, USA). The primary preregistered outcome measure was the difference in speed between the 24hrs post-training and the baseline measurement. A power analysis was performed based on an internal pilot with six subjects per group. The mean and standard deviation were 0.143 m/s and 0.134 m/s (used for sample size estimation) for the sham tsDCS, and 0.273 m/s and 0.084 m/s for the anodal tsDCS group. Using a two-sample t-test, a total of 42 subjects was determined to be required to detect a group difference of 0.12 m/s, equivalent to 0.9 of Cohen’s d. Significance level was prospectively set at p = 0.025 (adjusted for the interim analysis) with a power of 80%. Secondary outcome measures were online, offline and retention learning over one, over the three training days, and at 30 days according to the following formulae:
Online speed gains over three days: [(D1 Post Training - Baseline) + (D2 Post Training – D2 Pre-Training) + (D3Post Training – D3Pre-Training)];
Offline speed gains over three days: [(D2 Pre-Training - D1 Post Training) + (D3Pre-Training - D2 Post Training) + (D4 Test- D3Post Training)];
Total speed gains over three days: D4 Test – Baseline;
Retention: D30 Test - D3Post Training.
For retention of learning, we used analysis of covariance (ANCOVA) with baseline as a covariate to evaluate the effect of anodal tsDCS. For the other six outcomes, two-sample t-test was used since baseline had no significant effect (p > 0.1). Bonferroni correction was applied to adjust for multiplicity. Therefore, for the primary outcome, a significance level of p = 0.025 was used since an interim analysis was performed; for the six secondary outcomes, a significance level of p = 0.007 was used since a total of 7 outcomes were tested.
Soleus H-Reflex.
Baseline H-reflex amplitude data met the criteria for normality (Shapiro-Wilk test). One-way ANOVA was used to evaluate differences between baselines (Day 1–3) and found no statistical differences between baseline values [s-tsDCS + BLT (p = 0.780), a-tsDCS + BLT (p = 0.677). Therefore, immediate and 30 min post training (PTx and 30-min PTx) data were normalized to day one baseline values. ANOVA was used to evaluate effects of training and tsDCS.
Results
Mean age, height, and activity levels were comparable across groups [p = 0.41, p = 0.56, p = 0.63, respectively]. 42% of subjects reported receiving anodal and 58% sham stimulation. The chances of predicting accurately the type of stimulation received were 61% for sham stimulation and 45% for anodal tsDCS.
Speed gain at 24 h after a single training session (primary endpoint measure) was larger in the tsDCS (0.20 ± 0.02 m/s, n = 22) than in the sham (0.12 ± 0.02 m/s, n = 21) group (p = 0.008). Online and offline learning contributions were comparable across groups (online: p = 0.334; offline: p = 0.043, Fig. 2A).
Fig. 2.
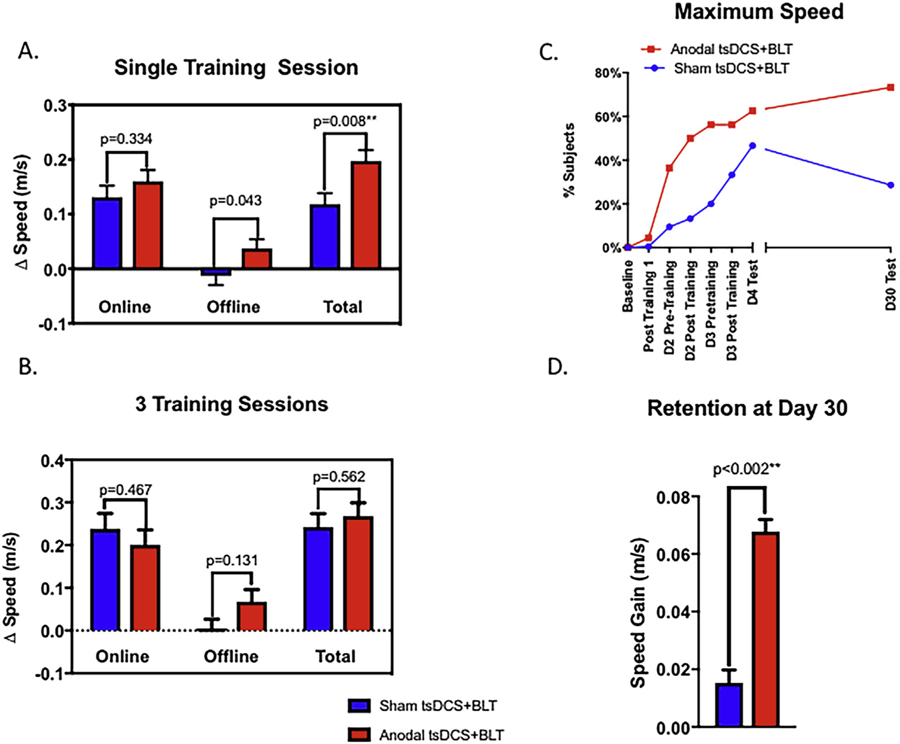
Locomotor learning A: Single training session. Backward locomotion learning after a single training session was greater in the tsDCS than in the sham group. A trend for superior offline learning in the tsDCS group did not reach statistical significance after Bonferroni correction. B: Learning after 3 training sessions (D4 Test – Baseline). No group differences in learning were identified after three training sessions. C: Proportion of subjects reaching maximal treadmill speed. Note the higher proportion of subjects reaching maximum speed in the tsDCS than in the sham group. D. Retention (D30 Test - D3Post Training). Note that subjects retained learning acquired at the end of the third training session significantly better in the tsDCS than in the sham group.
After three training sessions, total speed gain was 0.27 ± 0.03 m/s (n = 16) in the tsDCS group and 0.258 ± 0.13 m/s (n = 15) in the sham group (p = 0.562). Online (tsDCS: 0.201 ± 0.04 m/s; sham: 0.238 ± 0.04 m/s) and offline (tsDCS: 0.068 ± 0.03 m/s; sham: 0.004 ± 0.03 m/s) gains were also comparable (online: p = 0.467; offline: p = 0.131, Fig. 2B). A higher proportion of subjects reached maximal speed sooner in the tsDCS than in the sham group, i.e. after a single training session 36% reached maximal speed in the tsDCS group compared to 10% in the sham group (Fig. 2C). Retention of learning at Day 30 was significantly greater in the tsDCS (0.068 ± 0.03 m/s, n = 15) than in the sham (0.015 ± 0.02 m/s, n = 14) group (p = 0.0024, Fig. 2D). Consistently, 73% of subjects in the tsDCS group reached maximal speed by Day 30, relative to only 29% in the sham group (Fig. 2C). Finally, training-dependent improvements in speed correlated with step-lengths at all measured time points, except Day 30 (Suppl Table 2, Pearson-r: 0.452–0.631).
Soleus H-reflex (Hmax/Mmax) amplitude was significantly reduced immediately post-training in both sham and tsDCS groups (ANOVA.p < 0.0001), with no between-group differences (p = 0.594) as shown in Fig. 3. At 30 min post-training, the H-reflex amplitude remained significantly reduced in the anodal-tsDCS, but not in the sham-tsDCS group (ANOVA, P = 0.05), Fig. 3.
Fig. 3.
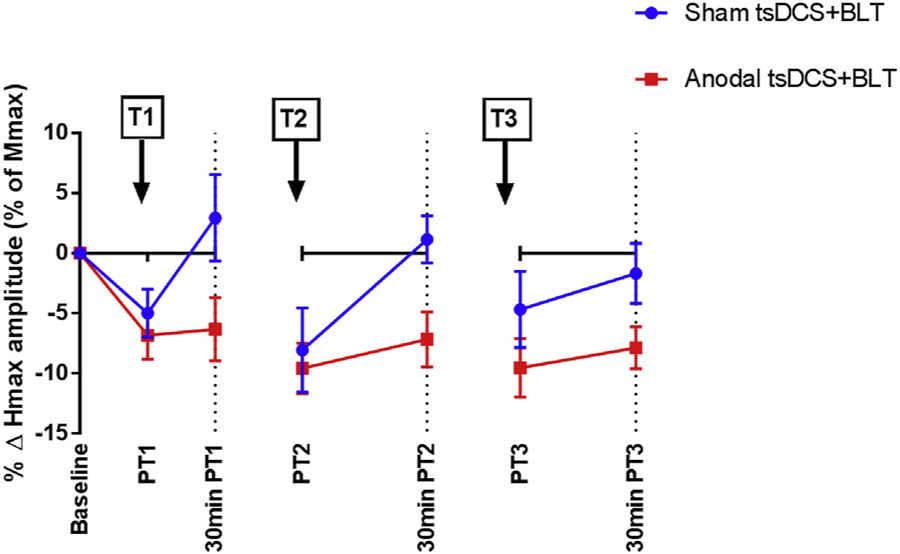
Percent change in Soleus H-reflex (Hmax) amplitudes (normalized to Day 1 baseline). H-reflex amplitude was down-regulated in both groups in the immediately post-training period on days 1–3 (PT1, PT2, PT3, respectively). 30 min post-training (30 min PT 1, 30min PT2, 30min PT3), the Hmax/Mmax amplitude remained down-regulated only in the a-tsDCS group (red). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Participants’ reports on verbal 0/10 scales indicated the following. In the anodal and sham groups, general discomfort was 1.27 (range 0–5) and 0.90 (range 0–4), perception of pain was 0.18 (range 0–2) and 0.24 (range 0–3), sensation of burning under the electrode was 0.50 (range 0–2), and 0.43 (range 0–5), and itching under the electrode was 0.63 (range 0–2) and 0.76 (range 0–5) respectively. No skin irritation or burns occurred. Thus, tsDCS was overall well tolerated.
Discussion
The main results of this study were that anodal tsDCS improved the effects of a single training session on locomotor learning compared to sham tsDCS and that when applied over three consecutive days tsDCS resulted in greater retention of learning at Day 30 relative to sham.
Transcranial tDCS concurrent with training has been reported to improve upper limb motor learning in young healthy subjects [3,43–45], elderly individuals [46,47] and patients with brain lesions like stroke [45,46,48–52]. The effects of transcranial DCS on locomotion on the other hand have been more modest, likely due to different localization of the cortical representations of upper and lower limbs [13,14] and also the higher reliance of locomotion on subcortical neural structures [12,53–58]. Given these findings, previous modeling and electrophysiological studies attempted to modulate subcortical function using DCS applied over the spine (tsDCS). These studies demonstrated that tsDCS could indeed modulate spinal cord function [17,19,20,29,31,32,59,60], raising the question whether it could also influence locomotor behavior. In this investigation, we used the same montage and stimulating parameters reported to modulate electrophysiological measures of spinal cord function to address a novel question: could tsDCS modulate locomotor behavior in the form of learning a novel backward task of relevance in sports medicine and neurorehabilitation [61–70]. Additionally, we confirmed that under our experimental conditions tsDCS modulated spinal cord function in the form of excitability of the alpha motoneuron pool.
Participants receiving tsDCS over a single training session experienced higher learning at 24hr relative to those receiving sham, (Cohen’s d = 0.852). While we found no significant group differences in online or offline learning, we may have been underpowered to detect offline consolidation disparities (p = 0.043 uncorrected, Fig. 2A) as previously reported with transcranial DCS and upper limb learning [71,72]. More work will be necessary to address tsDCS effects on offline consolidation of locomotor learning.
We then evaluated the cumulative effects of 3 training sessions. We did not find group differences in total, online or offline learning (Fig. 2B). It is possible that performance improvements in the tsDCS group reached ceiling after the first training session, consistent with a previous report on effects of transcranial DCS on upper limb learning [73]. In line with this possibility, subjects in our study reached ceiling speed earlier in the tsDCS group than in the sham group (Fig. 2C).
Retention of learning 30 days later was significantly superior in the tsDCS than in the sham group (Fig. 2C and D). This finding, together with the absence of group differences at the end of the three training sessions is intriguing, suggesting an effect of tsDCS on offline retention mechanisms [2–7,74,75]. Thus, our results dissociating effects of tsDCS on online (largely unaffected) and offline (improved 24 h consolidation and long-term retention) mechanisms merits further investigation [7,71]. Behavioral interventions like reward have also been reported to influence long-term retention of skill to a larger extent than online learning [76]. What could be the impact of the reported differences in real life activity? While impossible to predict with certainty, healthy subjects who practiced this task for 3 days could, at 30 days, backward-walk one mile over 3 min faster in the tsDCS group (17 min 46 s) than in the sham group (21 min 22 s min), a net speed improvement of 28%.
This study found that anodal-tsDCS prolonged the duration of H-reflex down-regulation following training relative to sham-tsDCS. Our data confirm prior studies showing that exercise such as BLT leads to transient down-regulation of the H reflex [77,78]. We have shown that tsDCS can prolong the period of exercise-induced down-regulation of the H reflex, which may contribute to the behavioral gains during BLT [79]. The amplitude of the H-reflex is known to be modulated in a phase-dependent manner during forward locomotion, up-regulated in late stance, leading to enhanced muscle stiffness prior to toe-off (Capaday and Stein 1987). The mechanical advantage this normal pattern of modulation offers for propelling forward walking would likely be detrimental for BLT. Our results cannot determine whether the prolongation of H-reflex down-regulation by anodal-tsDCS resulted from action on local spinal circuits or modulators of presynaptic inhibition of inputs to alpha-motor neurons [61,78]. Future studies will be needed to evaluate the mechanisms of H-reflex down-regulation from anodal-tsDCS during BLT and the contribution of other cortical and subcortical regions, as well as the effects of aging.
From a kinematic point of view, changes in step length related to improved confidence with training was a likely contributor to speed improvements [64,80–82]. From a mechanistic angle, previously reported tsDCS influences on H-reflex modulation [77,78,83] impacts speed and symmetry of locomotion and modulates H-reflex post-activation [20], central nociceptive signal transmission [15,21] possibly contributing to speed improvements as well. Alternatively, tsDCS could have modified cortical plasticity underlying motor learning through modulation of somatosensory and motor [16,21] evoked potentials as well as interhemisperic inhibition [22,23]. More work is required to characterize the mechanisms underlying this behavioral effect and to determine the reproducibility of these findings.
In summary, these results, which require replication in larger populations, indicate that anodal tsDCS applied with concurrent training facilitates locomotor learning and retention, a finding of possible relevance in neurorehabilitation of locomotor function after neurologic injury.
Supplementary Material
Acknowledgements
This research was supported by the Intramural Research Program, National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health (NIH).
Footnotes
Declaration of conflicting interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.brs.2019.01.017.
References
- [1].Duncan PW, Sullivan KJ, Behrman AL, Azen SP, Wu SS, Nadeau SE, et al. Body-weight-supported treadmill rehabilitation after stroke. N Engl J Med 2011;364(21):2026–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol 2000;527(3): 633–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Reis J, Schambra HM, Cohen LG, Buch ER, Fritsch B, Zarahn E, et al. Noninvasive cortical stimulation enhances motor skill acquisition over multiple days through an effect on consolidation. Proc Natl Acad Sci Unit States Am 2009;106(5):1590–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Fritsch B, Reis J, Martinowich K, Schambra HM, Ji Y, Cohen LG, et al. Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron 2010;66(2):198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Polania R, Paulus W, Nitsche MA. P19.21 Modulating cortico-striatal and thalamo-cortical functional connectivity with transcranial direct current stimulation. Clin Neurophysiol 2011:122. [DOI] [PMC free article] [PubMed]
- [6].Antal A, Polania R, Schmidt-Samoa C, Dechent P, Paulus W. Combining transcranial direct current stimulation with fMRI. Klin Neurophysiol 2010;41(01). [DOI] [PubMed] [Google Scholar]
- [7].Dayan E, Censor N, Buch ER, Sandrini M, Cohen LG. Noninvasive brain stimulation: from physiology to network dynamics and back. Nat Neurosci 2013;16(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kadosh R, Soskic S, Iuculano T, Kanai R, Walsh V. Modulating neuronal activity produces specific and long-lasting changes in numerical competence. Curr Biol 2010;20(22):2016–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Snowball A, Tachtsidis I, Popescu T, Thompson J, Delazer M, Zamarian L, et al. Long-term enhancement of brain function and cognition using cognitive training and brain stimulation. Curr Biol 2013;23(11):987–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Geiger M, Supiot A, Zory R, Aegerter P, Pradon D, Roche N. The effect of transcranial direct current stimulation (tDCS) on locomotion and balance in patients with chronic stroke: study protocol for a randomised controlled trial. Trials 2017;18(1):492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Geroin C, Picelli A, Munari D, Waldner A, Tomelleri C, Smania N. Combined transcranial direct current stimulation and robot-assisted gait training in patients with chronic stroke: a preliminary comparison. Clin Rehabil 2011;25(6):537–48. [DOI] [PubMed] [Google Scholar]
- [12].Jones PS, Pomeroy VM, Wang J, Schlaug G, Marrapu TS, Geva S, et al. Does stroke location predict walk speed response to gait rehabilitation? Hum Brain Mapp 2016;37(2):689–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Jeffery DT, Norton JA, Roy FD, Gorassini MA. Effects of transcranial direct current stimulation on the excitability of the leg motor cortex. Exp Brain Res 2007;182(2):281–7. [DOI] [PubMed] [Google Scholar]
- [14].Madhavan S, Stinear JW. Focal and bidirectional modulation of lower limb motor cortex using anodal transcranial direct current stimulation. Brain Stimulat 2010;3(1):42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Cogiamanian F, Vergari M, Schiaffi E, Marceglia S, Ardolino G, Barbieri S, et al. Transcutaneous spinal cord direct current stimulation inhibits the lower limb nociceptive flexion reflex in human beings. Pain 2011;152(2):370–5. [DOI] [PubMed] [Google Scholar]
- [16].Cogiamanian F, Vergari M, Pulecchi F, Marceglia S, Priori A. Effect of spinal transcutaneous direct current stimulation on somatosensory evoked potentials in humans. Clin Neurophysiol 2008;119(11):2636–40. [DOI] [PubMed] [Google Scholar]
- [17].Hubli M, Dietz V, Schrafl-Altermatt M, Bolliger M. Modulation of spinal neuronal excitability by spinal direct currents and locomotion after spinal cord injury. Clin Neurophysiol 2013;124(6):1187–95. [DOI] [PubMed] [Google Scholar]
- [18].Bocci T, Vannini B, Torzini A, Mazzatenta A, Vergari M, Cogiamanian F, et al. Cathodal transcutaneous spinal direct current stimulation (tsDCS) improves motor unit recruitment in healthy subjects. Neurosci Lett 2014;578:75–9. [DOI] [PubMed] [Google Scholar]
- [19].Lamy CJ, Ho C, Badel A, Arrigo RT, Boakye M. Modulation of soleus H reflex by spinal DC stimulation in humans. J Neurophysiol 2012;108(3):906–14. [DOI] [PubMed] [Google Scholar]
- [20].Winkler T, Hering P, Straube A. Spinal DC stimulation in humans modulates post-activation depression of the H-reflex depending on current polarity. Clin Neurophysiol: Off J Int Federat Clin Neurophysiol 2010;121(6):957–61. [DOI] [PubMed] [Google Scholar]
- [21].Truini A, Vergari M, Biasiotta A, Cesa LS, Gabriele M, Stefano DG, et al. Transcutaneous spinal direct current stimulation inhibits nociceptive spinal pathway conduction and increases pain tolerance in humans. Eur J Pain 2011;15(10):1023–7. [DOI] [PubMed] [Google Scholar]
- [22].Bocci T, Barloscio D, Vergari M, Rollo A, Rossi S, Priori A, et al. Spinal direct current stimulation modulates short intracortical inhibition. Neuromodulat: J Int Neuromodulat Soc 2015;18(8):686–93. [DOI] [PubMed] [Google Scholar]
- [23].Bocci T, Caleo M, Vannini B, Vergari M, Cogiamanian F, Rossi S, et al. An unexpected target of spinal direct current stimulation: interhemispheric connectivity in humans. J Neurosci Methods 2015;254:18–26. [DOI] [PubMed] [Google Scholar]
- [24].Bocci T, Marceglia S, Vergari M, Cognetto V, Cogiamanian F, Sartucci F, et al. Transcutaneous spinal direct current stimulation modulates human corticospinal system excitability. J Neurophysiol 2015;114(1):440–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Schweizer L, Meyer-Friebem CH, Zahn PK, Tegenthoff M, Schmidt-Wilcke T. Transcutaneous spinal direct current stimulation alters resting-state functional connectivity. Brain Connect 2017. August;7(6):357–65. [DOI] [PubMed] [Google Scholar]
- [26].Marangolo P, Fiori V, Shofany J, Gili T, Caltagirone C, Cucuzza G, et al. Moving beyond the brain: transcutaneous spinal direct current stimulation in poststroke aphasia. Front Neurol 2017;8:400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Song W, Truong DQ, Bikson M, Martin JH. Transspinal direct current stimulation immediately modifies motor cortex sensorimotor maps. J Neurophysiol 2015;113(7):2801–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Priori A, Ciocca M, Parazzini M, Vergari M, Ferrucci R. Transcranial cerebellar direct current stimulation and transcutaneous spinal cord direct current stimulation as innovative tools for neuroscientists. J Physiol 2014;592(16): 3345–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kuck A, Stegeman DF, van Asseldonk EHF. Modeling trans-spinal direct current stimulation for the modulation of the lumbar spinal motor pathways. J Neural Eng 2017;14(5):56014. [DOI] [PubMed] [Google Scholar]
- [30].Parazzini M, Fiocchi S, Liorni I, Rossi E, Cogiamanian F, Vergari M, et al. Modeling the current density generated by transcutaneous spinal direct current stimulation (tsDCS). Clin Neurophysiol: Off J Int Federat Clin Neurophysiol 2014;125(11):2260–70. [DOI] [PubMed] [Google Scholar]
- [31].Fregni F, Grecco L, Li S, Michel S, Castillo-Saavedra L, Mourdoukoutas A, et al. Transcutaneous spinal stimulation as a therapeutic strategy for spinal cord injury: state of the art. J Neurorestoratol 2015;3:73–82. [Google Scholar]
- [32].Fiocchi S, Ravazzani P, Priori A, Parazzini M. Cerebellar and spinal direct current stimulation in children: computational modeling of the induced electric field. Front Hum Neurosci 2016;10:522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Flynn TW, Connery, Smutok MA, Zeballos RJ, Weisman IM. Comparison of cardiopulmonary responses to forward and backward walking and running. Med Sci Sports Exerc 1994;26(1):89–94. [PubMed] [Google Scholar]
- [34].Terblanche E, Page C, Kroff J, Venter RE. The effect of backward locomotion training on the body composition and cardiorespiratory fitness of young women. Int J Sports Med 2005;26(3). [DOI] [PubMed] [Google Scholar]
- [35].de Hollander EL, Zwart L, de Vries SI, Wendel-Vos W. The SQUASH was a more valid tool than the OBiN for categorizing adults according to the Dutch physical activity and the combined guideline. J Clin Epidemiol 2012;65(1): 73–81. [DOI] [PubMed] [Google Scholar]
- [36].Sekiya N, Nagasaki H, Ito H, Furuna T. Optimal walking in terms of variability in step length. J Orthop Sports Phys Ther 1997;26(5):266–72. [DOI] [PubMed] [Google Scholar]
- [37].Laufer Y Effect of age on characteristics of forward and backward gait at preferred and accelerated walking speed. J Gerontol A Biol Sci Med Sci 2005;60(5):627–32. [DOI] [PubMed] [Google Scholar]
- [38].Vergari M, Cogiamanian F, Pulecchi F, Marceglia S, Tadini L, Ferrucci R, et al. Non-invasive modulation of spinal cord function with transcutaneous direct current (dc) stimulation. Brain Stimulation 2008;1(3):304. [Google Scholar]
- [39].Liebetanz D, Koch R, Mayenfels S, König F, Paulus W, Nitsche MA. Safety limits of cathodal transcranial direct current stimulation in rats. Clin Neurophysiol: Off J Int Federat Clin Neurophysiol 2009;120(6):1161–7. [DOI] [PubMed] [Google Scholar]
- [40].McCreery DB, Agnew WF, Yuen TG, Bullara L. Charge density and charge per phase as cofactors in neural injury induced by electrical stimulation. IEEE Trans Biomed Eng 1990;37(10):996–1001. [DOI] [PubMed] [Google Scholar]
- [41].Gandiga PC, Hummel FC, Cohen LG. Transcranial DC stimulation (tDCS): a tool for double-blind sham-controlled clinical studies in brain stimulation. Clin Neurophysiol: Off J Int Federat Clin Neurophysiol 2006;117(4):845–50. [DOI] [PubMed] [Google Scholar]
- [42].Hultborn H, Illert M, Nielsen J, Paul A, Ballegaard M, Wiese H. On the mechanism of the post-activation depression of the H-reflex in human subjects. Exp Brain Res 1996;108(3):450–62. [DOI] [PubMed] [Google Scholar]
- [43].Hummel FC, Cohen LG. Drivers of brain plasticity. Curr Opin Neurol 2005;18(6):667–74. [DOI] [PubMed] [Google Scholar]
- [44].Sandrini M, Cohen LG. Noninvasive brain stimulation in neurorehabilitation. Handb Clin Neurol 2013;116:499–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Cho H-SS, Cha H-GG. Effect of mirror therapy with tDCS on functional recovery of the upper extremity of stroke patients. J Phys Ther Sci 2015;27(4): 1045–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Lindenberg R, Nachtigall L, Meinzer M, Sieg M, Flöel A. Differential effects of dual and unihemispheric motor cortex stimulation in older adults. J Neurosci 2013;33(21):9176–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Martin A, Meinzer M, Lindenberg R, Sieg MM, Nachtigall L, Flöel A. Effects of transcranial direct current stimulation on neural network structure in young and older adults. J Cognit Neurosci 2017:1–12. [DOI] [PubMed]
- [48].Hummel F, Celnik P, Giraux P, Floel A, Wu W-HH, Gerloff C, et al. Effects of non-invasive cortical stimulation on skilled motor function in chronic stroke. Brain: J Neurol 2005;128(Pt 3):490–9. [DOI] [PubMed] [Google Scholar]
- [49].Boggio PS, Nunes A, Rigonatti SP, Nitsche MA, Pascual-Leone A, Fregni F. Repeated sessions of noninvasive brain DC stimulation is associated with motor function improvement in stroke patients. Restor Neurol Neurosci 2007;25(2):123–9. [PubMed] [Google Scholar]
- [50].Nair DG, Renga V, Lindenberg R, Zhu L, Schlaug G. Optimizing recovery potential through simultaneous occupational therapy and non-invasive brainstimulation using tDCS. Restor Neurol Neurosci 2011;29(6):411–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Sandrini M, Cohen LG, Censor N. Modulating reconsolidation: a link to causal systems-level dynamics of human memories. Trends Cognit Sci 2015;19(8): 475–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Sandrini M, Manenti R, Brambilla M, Cobelli C, Cohen LG, Cotelli M. Older adults get episodic memory boosting from noninvasive stimulation of prefrontal cortex during learning. Neurobiol Aging 2016;39:210–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Kaoru T Neurophysiology of gait: from the spinal cord to the frontal lobe. Mov Disord 2013;28(11):1483–91. [DOI] [PubMed] [Google Scholar]
- [54].Andreas RL, Richard FM, Larry WF, Federico V, Fred I, John DS, et al. Treadmill exercise activates subcortical neural networks and improves walking after stroke. Stroke 2008;39(12):3341–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Weerdesteyn V, Nienhuis B, Hampsink B, Duysens J. Gait adjustments in response to an obstacle are faster than voluntary reactions. Hum Mov Sci 2004;23(3–4):351–63. [DOI] [PubMed] [Google Scholar]
- [56].Charles C, Brigitte AL, Hugues B, Cyril S, Mireille B. Studies on the corticospinal control of human walking. I. Responses to focal transcranial magnetic stimulation of the motor cortex. J Neurophysiol 1999;81(1):129–39. [DOI] [PubMed] [Google Scholar]
- [57].Nedialko K, Trevor D. Motor cortical regulation of sparse synergies provides a framework for the flexible control of precision walking. Front Comput Neurosci 2013;7:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Yi X, Qing-hua H, Shawn DR, Bradford CB, Andrew JS, Qiang L, et al. Neuroplasticity in post-stroke gait recovery and noninvasive brain stimulation. Neural Regen Res 2015;10(12):2072–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Niérat M-CC, Similowski T, Lamy J-CC. Does trans-spinal direct current stimulation alter phrenic motoneurons and respiratory neuromechanical outputs in humans? A double-blind, sham-controlled, randomized, crossover study. J Neurosci: Off J Soc Neurosci 2014;34(43):14420–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Heide AC, Winkler T, Helms HJ, Nitsche MA, Trenkwalder C, Paulus W, et al. Effects of transcutaneous spinal direct current stimulation in idiopathic restless legs patients. Brain Stimulation 2014;7(5):636–42. [DOI] [PubMed] [Google Scholar]
- [61].The effects of backward walking training on knee isokinetic strength and vasus medialis surface EMG. PMC.
- [62].Abdel-Aziem AA, El-Basatiny H. Effectiveness of backward walking training on walking ability in children with hemiparetic cerebral palsy: a randomized controlled trial. Clin Rehabil 2017. June;31(6):790–7. [DOI] [PubMed] [Google Scholar]
- [63].Błażkiewicz M Muscle force distribution during forward and backward locomotion. Acta Bioeng Biomech/Wrocław Univ Technol 2013;15(3):3–9. [PubMed] [Google Scholar]
- [64].Bryant MS, Workman CD, Hou J-GG, Henson HK, York MK. Acute and longterm effects of multidirectional treadmill training on gait and balance in Parkinson’s disease. PM & R: J Inj Funct Rehabil 2016. December;8(12):1151–8. [DOI] [PubMed] [Google Scholar]
- [65].Cadenas-Sánchez C, Arellano R, Taladriz S, López-Contreras G. Biomechanical characteristics of adults walking forward and backward in water at different stride frequencies. J Sports Sci 2015;34(3). [DOI] [PubMed] [Google Scholar]
- [66].El-Basatiny HMY, Abdel-aziem AA. Effect of backward walking training on postural balance in children with hemiparetic cerebral palsy: a randomized controlled study. Clin Rehabil 2014;29(5):457–67. [DOI] [PubMed] [Google Scholar]
- [67].Foster H, DeMark L, Spigel PM, Rose DK, Fox EJ. The effects of backward walking training on balance and mobility in an individual with chronic incomplete spinal cord injury: a case report. Physiother Theory Pract 2016;32(7):536–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Grobbelaar R, Venter R, Welman K. Backward compared to forward over ground gait retraining have additional benefits for gait in individuals with mild to moderate Parkinson’s disease: a randomized controlled trial. Gait Posture 2017;58:294–9. [DOI] [PubMed] [Google Scholar]
- [69].Hao W-Y, Chen Y. Backward walking training improves balance in school-aged boys. BMC Sports Sci, Med Rehabil 2011;3(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Marden L, Killough J. Effects of backward walking training on neuromuscular efficiency in gait in an individual post-stroke. J Neurol Phys Ther 2006;30(4): 213. [Google Scholar]
- [71].Janine R, Heidi MS, Leonardo GC, Ethan RB, Brita F, Eric Z, et al. Noninvasive cortical stimulation enhances motor skill acquisition over multiple days through an effect on consolidation. Proc Natl Acad Sci Unit States Am 2009;106(5):1590–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Ethan RB, Emiliano S, Andrea A, Jan B, Pablo AC, Joseph C, et al. Effects of tDCS on motor learning and memory formation: a consensus and critical position paper. bioRxiv 2016:64204.
- [73].Reis J, Fischer J, Prichard G, Weiller C, Cohen LG, Fritsch B. Time-but not sleep-dependent consolidation of tDCS-enhanced visuomotor skills. Cerebr Cortex 2013;25(1):109–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Bindman LJ, Lippold OC, Redfea JW. Long-lasting changes in the level of the electrical activity of the cerebral cortex produced bypolarizing currents. Nature 1962;196:584–5. [DOI] [PubMed] [Google Scholar]
- [75].Meinzer M, Lindenberg R, Sieg MM, Nachtigall L, Ulm L, Flöel A. Transcranial direct current stimulation of the primary motor cortex improves word-retrieval in older adults. Front Aging Neurosci 2014;6:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Abe M, Schambra H, Wassermann EM, Luckenbaugh D, Schweighofer N, Cohen LG. Reward improves long-term retention of a motor memory through induction of offline memory gains. Curr Biol 2011;21(7):557–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Thompson AK, Pomerantz FR, Wolpaw JR. Operant conditioning of a spinal reflex can improve locomotion after spinal cord injury in humans. J Neurosci 2013;33(6):2365–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Albuquerque P, Campêlo M, Mendonça T, Fontes L, de Brito R, Monte-Silva K. Effects of repetitive transcranial magnetic stimulation and trans-spinal direct current stimulation associated with treadmill exercise in spinal cord and cortical excitability of healthy subjects: a triple-blind, randomized and sham-controlled study. PLoS One 2018;13(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Capaday C, Stein RB. Difference in the amplitude of the human soleus H reflex during walking and running. J Physiol 1987;392(1):513–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Kirkwood R, de Moreira B, Vallone M, Mingoti S, Dias R, Sampaio R. Step length appears to be a strong discriminant gait parameter for elderly females highly concerned about falls: a cross-sectional observational study. Physio-therapy 2011;97(2):126–31. [DOI] [PubMed] [Google Scholar]
- [81].Mak M Reduced step length, not step length variability is central to gait hypokinesia in people with Parkinson’s disease. Clin Neurol Neurosurg 2013;115(5):587–90. [DOI] [PubMed] [Google Scholar]
- [82].Bryant MS, Rintala DH, Hou J-G, Protas EJ. Influence of fear of falling on gait and balance in Parkinson’s disease. Disabil Rehabil 2013;36(9):744–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Hubli M, Dietz V. The physiological basis of neurorehabilitation–locomotor training after spinal cord injury. J NeuroEng Rehabil 2013;10:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


