Abstract
Purpose
To analyze the differences in the vitreous cytokine profiles in epiretinal membrane eyes with and without an ectopic inner foveal layer (EIFL).
Methods
Sixty eyes with epiretinal membrane (32 eyes without EIFL and 28 eyes with EIFL) were included. The vitreous samples were collected during surgery for epiretinal membrane. The cytokine levels of the vitreous were measured using a multiplex bead analysis.
Results
The mean logMAR visual acuity was worse (0.42 vs. 0.37; P = 0.331) and the central foveal thickness was higher in the EIFL group (496.9 µm vs. 434.2 µm; P = 0.007) than they were in the group without EIFL. The mean EIFL thickness was 164.1 ± 67.7 µm in the EIFL group. On multiplex analysis of the vitreous cytokines, the levels of CD163 (21529 pg/dL vs. 10877 pg/dL; P = 0.002) and macrophage colony-stimulating factor (206 pg/dL vs. 159 pg/dL, P = 0.004) were significantly higher in the EIFL group than they were in the group without EIFL.
Conclusions
Eyes with EIFL had increased vitreous levels of M2 macrophage markers. The activation of glial cell proliferation by M2 macrophages may contribute to EIFL formation.
Keywords: epiretinal membrane; ectopic inner foveal layer; M-CSF; M2 macrophages, CD163
An epiretinal membrane (ERM) is a relatively common retinal condition that is characterized by fibrocellular proliferations on the inner retinal surface between the vitreous and retina.1–3 The term ERM covers a wide range of clinical entities. Some ERMs are associated with other retinal conditions, such as retinal vascular or inflammatory disease, tumors, retinal detachment, intraocular surgery, and trauma. In contrast, other ERMs are idiopathic.4 The severity of this disease varies largely between eyes. Therefore, various classification schemes have been proposed. The most widely used one was suggested by Gass in 1997.5
The introduction of SD-OCT has enabled clearer visualization of the ERM. SD-OCT has become the most powerful tool for both pre- and postoperative evaluation of ERM. These SD-OCT–derived findings, such as the central foveal thickness (CFT), the length of the photoreceptor outer segment, and the inner segment ellipsoid band integrity, were found to be prognostic factors for ERM.6,7 Recently, ectopic inner foveal layer (EIFL) was described on SD-OCT imaging of eyes with idiopathic ERMs.8 This eccentric layer of inner retina at the fovea may represent an important sign of ERM progression. The EIFL was associated with significant vision loss.9,10 Therefore, a novel SD-OCT–based grading scheme of ERMs, including this finding, was suggested.8
The precise pathophysiology of ERM and EIFL is not completely understood. However, the mechanism likely involves hyalocyte proliferation in the setting of anomalous posterior vitreous detachment.4 The purpose of this study was to compare the vitreous cytokine profiles in patients with idiopathic ERMs with and without EIFL. We focused on the degree to which fibrotic and inflammatory processes contribute to the progression of the disease.
Methods
Patients
This prospective clinical study included idiopathic ERMs in patients who underwent vitrectomy at Uijeongbu St. Mary's Hospital (Gyeonggi-do, Korea), the Catholic University of Korea, between March 1, 2016, and September 30, 2017. The study was approved by the institutional review board/ethics committee. It fully complies with the tenets of the Declaration of Helsinki. All participants signed an informed consent form after a detailed explanation of the study design and use of a vitreal sample for scientific purposes. The ERM identification was based on fundus examination. The SD-OCT examination evaluated the fibrous membrane on the macula. Patients were excluded if they had secondary ERM owing to diabetic retinopathy, retinal vascular disease, retinal breaks with or without retinal detachment, inflammatory retinal disease, or uveitis. The other exclusion criteria included any intervention within 6 months (including pharmacologic treatment, photocoagulation, and surgery), a history of intraocular surgeries (other than uncomplicated cataract surgery), and a history of ocular trauma on the study eye.
Ophthalmologic Evaluation and SD-OCT Imaging
Comprehensive ophthalmologic examinations, including best-corrected visual acuity (BCVA), slit lamp biomicroscopy, fundus examination, and SD-OCT (Spectralis, Heidelberg Engineering GmbH, Heidelberg, Germany) imaging, were performed in all patients before surgery and 6 months after surgery. The horizontal 32 raster B-scan SD-OCT at 15° area was performed. The images were analyzed using the Heidelberg Eye Explorer (version 1.8.6.0). The CFT values were measured automatically using the Heidelberg software. The EIFLs were defined on SD-OCT according to the previous description by Govetto et al.8 This definition included the presence of continuous hyporeflective and hyperreflective bands that extend from the inner nuclear layer and inner plexiform layer across the foveal region, where those layers are not presented in normal eyes. The measurement of EIFL thickness was performed manually using the caliper function in the Heidelberg software. This function draws a vertical line from the outer margin of the inner nuclear layer to the inner margin of the internal limiting membrane at the center of fovea on 1:1 mm ratio image (Fig. 1). The presence of ellipsoid disruption and the external limiting membrane disruption was assessed.
Figure 1.
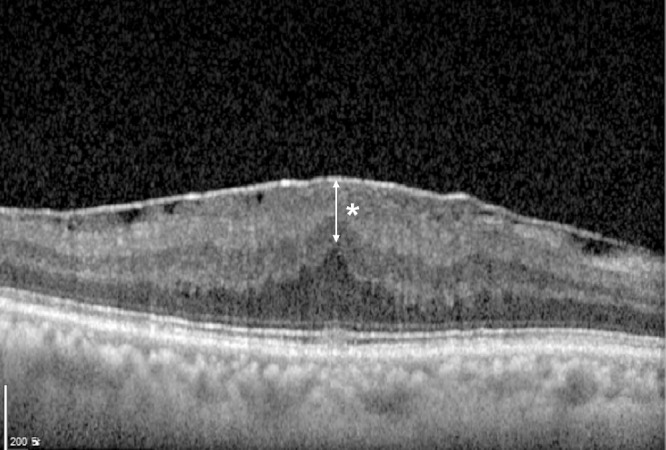
Ectopic inner foveal layer. The EIFL (asterisk) on SD-OCT was defined by the presence of continuous hyporeflective and hyperreflective bands extending from the inner nuclear layer and inner plexiform layer across the foveal region. The measurement of EIFL thickness was performed manually using the caliper function in the Heidelberg software. This function drew a vertical line from the outer margin of the inner nuclear layer to the inner margin of the internal limiting membrane at the center of the fovea on a 1:1 mm ratio image.
Surgical Procedure and Collection of Vitreous Samples and Cytokine Analysis
All patients underwent a standard, three-port 23-G pars plana vitrectomy with ERM peeling performed by one vitreoretinal surgeon (MYL) with the Constellation vision system (Alcon, Fort Worth, TX). Combined phacoemulsification and intraocular lens implantation procedures were performed in phakic eyes. Core vitrectomy was performed with the creation of posterior vitreous detachment. Then, ERM removal up to the vascular arcades was done using Grieshaber internal limiting membrane forceps (Alcon). At the end of the surgery, partial air–fluid exchange was performed in all cases.
Diluted vitreous (approximately 1.0 mL) samples were collected at the onset of pars plana vitrectomy and were immediately frozen at −80°C until use. The vitreous samples were analyzed using a multiplex bead assay system (Luminex, R&D Systems, Minneapolis, Minnesota, USA). Using this system, the concentrations of cytokines in each vitreous sample were detected and quantified in parallel, as follows: monocyte chemoattractant protein-1 (CCL2), MIP-1beta (CCL4), CD163, GRO alpha (CXCL1), IP-10 (CXCL10), stromal cell-derived factor-1 alpha (CXCL12), IL-8 (CXCL8), granulocyte-macrophage colony-stimulating factor, IFN-gamma, IL-17A, IL-18, IL-2, IL-4, CD163, macrophage colony-stimulating factor (M-CSF), MMP-9, Periostin, and VEGF. All procedures were performed according to the manufacturer's guidelines by experienced laboratory technicians who were blinded to the study details.
Statistical Analysis
The numerical data are presented as mean values ± SD. The BCVA was converted into logMAR values for statistical analysis. The statistical analyses were performed using SPSS statistical software (version 19.0; SPSS Inc., Chicago, IL). To compare between the groups, a χ2 test for categorical variables and an independent t-test were used for continuous variables. The nonparametric Mann–Whitney U test was applied for the intergroup comparisons when the criteria for a normal distribution were not satisfied. P values of less than 0.05 were considered statistically significant.
Results
Baseline Clinical Characteristics
A total of 60 eyes from 60 patients with idiopathic ERM were enrolled in this study. The mean age was 69.58 ± 10.30 years (range, 57–89 years). Nineteen patients (32%) were male. The mean logMAR BCVA was 0.45 ± 0.32 (with a Snellen equivalent of 20/56). The mean CFT was 464.45 ± 93.24 µm. EIFLs were present in 28 eyes (47%) (EIFL group); 32 eyes did not show EIFL (non-EIFL group). The baseline characteristics of the study subjects are summarized in Table 1.
Table 1.
Baseline Clinical Characteristics
| Clinical Factors | Total | Non-EIFL Group | EIFL Group | P Value |
|---|---|---|---|---|
| (N = 60) | (n = 32) | (n = 28) | ||
| Sex (male:female) | 19:41 | 10:22 | 9:19 | 0.877 |
| Age (years) | 69.58 ± 10.30 (57-89) | 68.06 ± 10.38 | 71.21 ± 7.85 | 0.192 |
| BCVA (logMAR) | 0.45 ± 0.32 | 0.37 ± 0.35 | 0.42 ± 0.32 | 0.032* |
| CFT (µm) | 463.45 ± 93.24 | 434.15 ± 99.40 | 496.92 ± 73.99 | 0.007* |
| EIFL thickness (µm) | 164.14 ± 67.69 | 0 | 164.14 ± 67.69 | <0.001* |
| Presence of ellipsoid disruption, n (%) | 32 (54) | 16 (50) | 16 (57) | 0.581 |
| Presence of ELM disruption, n (%) | 13 (21) | 5 (15) | 8 (28) | 0.225 |
ELM, external limiting membrane.
Statistically significant P value.
Comparison of Clinical Characteristic Between EIFL and Non-EIFL Eyes
The mean thickness of the EIFL was 164.14 ± 67.69 µm in the EIFL group. The mean age did not differ between the groups (71.21 ± 7.85 in EIFL group vs. 68.06 ± 10.38 in non-EIFL group; P = 0.192). The mean BCVA was worse (0.42 ± 0.32 vs. 0.37 ± 0.35; P = 0.032) and the mean CFT was thicker (496.92 ± 73.99 µm vs. 434.15 ± 99.40 µm; P = 0.007) in the EIFL group than they were in the non-EIFL group. The number of eyes with ellipsoid disruption (16/28 eyes [57%] vs. 16/32 eyes [50%]; P = 0.580) and external limiting membrane disruption (8/28 [28%] vs. 5/32 [15%]; P = 0.225) did not differ between the groups.
Cytokine Profile Differences Between EIFL and non-EIFL Eyes
The mean vitreous levels of the following cytokines did not differ between the EIFL and non-EIFL group: CCL2, CCL4, CXCL1, CXCL10, CXCL12, CXCL8, granulocyte-macrophage colony-stimulating factor, IFN-gamma, IL-17A, IL-18, IL-2, IL-4, MMP-9, Periostin, and VEGF (all P > 0.05; Table 2). In contrast, the levels of CD163 (21528.89 ± 15322.98 in EIFL group vs. 10876.69 ± 9558.28 pg/mL in non-EIFL group vs. 10876.69 ± 9558.28 pg/mL in non-EIFL group; P = 0.002) and M-CSF (206.13 ± 58.03 pg/mL in EIFL group vs. 158.52 ± 63.87 pg/mL in non-EIFL group; P = 0.004) were significantly higher in the EIFL group than they were in the non-EIFL group.
Table 2.
Comparison of the Vitreous Cytokine Levels Between the Non-EIFL and EIFL Groups
| Cytokines | Non-EIFL Group | EIFL Group | P Value |
|---|---|---|---|
| (n = 32) | (n = 28) | ||
| MCP-1 (CCL2) (pg/mL) | 469.37 ± 305.56 | 701.84 ± 384.1 | 0.011* |
| MIP-1beta (CCL4) (pg/mL) | 92.22 ± 21.15 | 97.63 ± 21.67 | 0.331 |
| GRO alpha (CXCL1) (pg/mL) | 43.03 ± 23.72 | 34.93 ± 30.83 | 0.251 |
| IP-10 (CXCL10) (pg/mL) | 33.02 ± 34.34 | 39.25 ± 29.85 | 0.457 |
| SDF-1 alpha (CXCL12) (pg/mL) | 387.49 ± 159.29 | 396.69 ± 180.74 | 0.833 |
| IL-8 (CXCL8) (pg/mL) | 17.13 ± 21.23 | 15.29 ± 12.53 | 0.689 |
| GM-CSF (pg/mL) | 1.09 ± 1.43 | 1.68 ± 1.98 | 0.184 |
| IFN-gamma (pg/mL) | 2.15 ± 2.88 | 3.62 ± 5.11 | 0.164 |
| IL-17A (pg/mL) | 2.12 ± 0.53 | 2.27 ± 0.65 | 0.342 |
| IL-18 (pg/mL) | 9.61 ± 3.24 | 10.26 ± 4.47 | 0.513 |
| IL-2 (pg/mL) | 230.76 ± 240.11 | 190.65 ± 60.72 | 0.393 |
| IL-4 (pg/mL) | 1.35 ± 5.23 | 10.61 ± 27.22 | 0.060 |
| CD163 (pg/mL) | 10876.69 ± 9558.28 | 21528.89 ± 15322.98 | 0.002* |
| M-CSF (pg/mL) | 158.52 ± 63.87 | 206.13 ± 58.03 | 0.004* |
| MMP-9 (pg/mL) | 61.00 ± 53.03 | 70.9 ± 65.6 | 0.517 |
| Periostin (pg/mL) | 0 ± 0 | 139.35 ± 737.38 | 0.281 |
| VEGF (pg/mL) | 9.50 ± 21.87 | 9.37 ± 29.21 | 0.984 |
GM-CSF, granulocyte–macrophage colony-stimulating factor; GRO, growth-related oncogene; IP, interferon gamma-induced protein; MCP, monocyte chemoattractant protein; MMP, matrix metalloprotease; SDF, stromal cell-derived factor.
Statistically significant P value.
The levels of CD163 and M-CSF were negatively correlated in the EIFL group (r = -0.476; P = 0.011). In contrast, there was no significant correlation observed in the non-EIFL group (r = 0.050; P = 0.781) (Fig. 2). The correlation between CD163/M-CSF and other cytokines also differed between the groups (Table 3). M-CSF was significantly correlated with CXCL10, CXCL12, IL-8, and granulocyte-macrophage colony-stimulating factor in the EIFL group. There were no such correlations in the non-EIFL group. CD163 was significantly correlated with CXCL12 and IL-4, whereas the non-EIFL group revealed no such correlation.
Figure 2.
Correlation between M-CSF and CD163 in the non-EILF group and EIFL group. The levels of CD163 and M-CSF were negatively correlated in the EIFL group (r = –0.476; P = 0.011) while no significant correlation was observed in the non-EIFL group (r = 0.050; P = 0.781).
Table 3.
Correlation of CD163/M-CSF and Other Cytokines in the Non-EIFL and EIFL Groups
| Non-EIFL Group (n = 32) | EIFL Group (n = 28) | |||
|---|---|---|---|---|
| Cytokines | CD163 | M-CSF | CD163 | M-CSF |
| MCP-1 | ||||
| ra | 0.807 | 0.034 | 0.828 | –0.284 |
| Pb | 0.000* | 0.850 | 0.000* | 0.143 |
| MIP-1beta | ||||
| ra | 0.494 | 0.302 | 0.418 | –0.082 |
| Pb | 0.003* | 0.087 | 0.027* | 0.677 |
| IP-10 | ||||
| ra | 0.514 | –0.126 | 0.923 | –0.593 |
| Pb | 0.002* | 0.484 | 0.001* | 0.001* |
| SDF-1alpha | ||||
| ra | –0.311 | 0.185 | –0.696 | 0.469 |
| Pb | 0.078 | 0.302 | 0.000* | 0.012* |
| IL-8 | ||||
| ra | 0.486 | –0.159 | 0.618 | –0.468 |
| Pb | 0.004* | 0.378 | 0.000* | 0.012* |
| GM-CSF | ||||
| ra | 0.416 | –0.060 | 0.376 | –0.461 |
| Pb | 0.016* | 0.740 | 0.048* | 0.014* |
| IL-18 | ||||
| ra | 0.395 | –0.097 | 0.225 | –0.324 |
| Pb | 0.023* | 0.591 | 0.249 | 0.092 |
| IL-4 | ||||
| ra | 0.079 | –0.348 | 0.408 | –0.401 |
| Pb | 0.661 | 0.047* | 0.031* | 0.035* |
| MMP-9 | ||||
| ra | 0.615 | –0.021 | 0.447 | –0.062 |
| Pb | 0.000* | 0.908 | 0.017* | 0.752 |
GM-CSF, granulocyte-macrophage colony-stimulating factor; GRO, growth-related oncogene; IP, interferon gamma-induced protein; MCP, monocyte chemoattractant protein; MMP, matrix metalloprotease; macrophage inflammatory protein; SDF, stromal cell-derived factor.
Pearson correlation.
Two-tailed significance.
Statistically significant P value.
Discussion
The ERMs are characterized by growth of fibrocellular tissue along the internal limiting membrane. The pathogenesis of idiopathic ERMs, which are not linked to any other ocular disease process, is not fully understood. However, the formation of ERM is speculated to be associated with maladapted wound repair processes in retinal cells. These processes are thought to lead to fibrotic changes on the retinal surface11,12 and the release of cytokines that are known to mediate inflammation, wound healing, and fibrotic scarification.13 In this study, we showed for the first time that some differences in vitreal cytokine composition between ERM eyes with and without EIFL can serve as evidence of ERM progression involving EIFL.
Since the introduction of SD-OCT, there is an increasing number of SD-OCT studies that have investigated alterations in the retinal layers in idiopathic ERM. These studies have shown that the outer retinal parameters, such as ellipsoid zone disruption and photoreceptor outer segment length, have been associated with lower preoperative and postoperative visual acuity.14–17 More recently, the role of the inner retinal layers in visual acuity loss has been studied. Factors such as the ganglion cell–inner plexiform layer complex thickening and the inner retinal irregularity index have been introduced as valid tools to assess visual prognosis.18–20 One of the most important recent findings associated with BCVA in ERM is EIFL. Govetto et al8,10 demonstrated that the presence of EIFLs in ERMs is associated with significant vision loss in these eyes. It is also a negative prognostic factor for postoperative anatomic and functional recovery. The baseline BCVA in this study is in accordance with previous reports. Eyes with EIFLs have worse BCVA compared to eyes without EIFL (logMAR 0.42 µm vs. 0.37 µm and logMAR 497 µm vs. 434 µm, respectively).
The pathogenetic mechanism for EIFL is not yet fully understood. It is hypothesized that EIFL is caused by mechanical displacement of the inner retinal tissue driven by ERM.21 Other investigators have suggested that Muller cells are involved at the molecular level.10 The analysis of vitreal cytokines in the current study revealed that CD163 and M-CSF were significantly higher in the EIFL group than they were in the non-EIFL group. Elevated M-CSF levels reflect macrophage differentiation. CD163 is a surface marker of M2 macrophages.22,23 Therefore, these results imply that M2 macrophages may play an important role in EIFL formation.
M-CSF stimulates the survival, proliferation, and differentiation of mononuclear phagocytic cells from determined (but undifferentiated) monoblasts to mature macrophages.22 The elevation of this cytokine in eyes with EIFL suggests active differentiation of monocytes into M2 macrophages. The M-CSF-differentiated M2 are polarized into activated M2 macrophages by IL-4. These cells express the M2 cell-surface marker CD163.23 Although it failed to reach statistical significance, the IL-4 level was elevated in the EIFL group compared to that in the non-EIFL group in this study (10.61 pg/mL vs 1.35 pg/mL; P = 0.060). The activated M2 macrophages participate in constructive processes like wound healing and tissue repair. These macrophages are the phenotype of resident tissue macrophages.24 EIFL might be the fibrotic tissue that results from the wound healing process of the M2 macrophage.
CD163 is known to be a highly specific monocyte/macrophage marker for M2 macrophages.25 In the vitreous, hyalocytes are known to be immunoreactive CD163. Hyalocytes belong to the monocyte/macrophage lineage.26 Along with CD45, CD163 presents predominantly in the ERM in eyes with complete posterior vitreous detachment and vitreomacular traction.27 The increased level of CD163 in the vitreous of the EIFL group might reflect an increased number or increased activity of hyalocytes in these eyes. Hyalocytes are the phenotype resident tissue M2 macrophages, which can be further activated by IL-4. The positive correlation between CD163 and IL-4 in eyes with EIFL suggests that there is a positive feedback relationship between IL-4 elevation and increased hyalocyte activity (as a M2 macrophage). Further studies using histology or cytology are needed to further evaluate the other cells involved in the fibrotic processes in the retina.
M-CSF and CF163 were found to be positively correlated in the vitreous of eyes with proliferative diabetic retinopathy.28 The positive correlation between these two cytokines was also identified in the peritumor area of hepatocellular carcinoma.29 In contrast, there was a negative correlation between M-CSF and CD163 in eyes with EIFL eyes in the current study. In contrast, there was no significant correlation between M-CSF and CD163 in the non-EIFL eyes. We cautiously expect that the fibrotic process involving M2 macrophages might not be as active as in proliferative diabetic retinopathy or in tumors. There may be a controlling mechanism that decreases fibrosis. The negative correlation between M-CSF and IL-4 also suggests the presence of a negative feedback mechanism in the differentiation and activation of M2 macrophages.
This study has several limitations. First, the cytokine levels were measured from the vitreous; therefore, they may not represent the cytokine levels at the lesion site. In addition, the study interpretation may have been limited by its small sample size. Further, larger studies that address lesion histology are required to substantiate our results. However, we believe that this study is valuable because it is the first one to reveal cytokine profiles related to EIFL in eyes with ERM.
In summary, eyes with EIFL represent a severe form of ERM with regard to the baseline visual acuity and postoperative outcomes. We suspect the increased expression levels of M-CSF and CD163 reflect that the M2 macrophages play a role in the formation of EIFL in eyes with ERM. The healing process of M2 macrophages causing fibrosis seems to contribute to the formation of EIFL in eyes with ERM, and this may result in worse outcome after the surgery in these eyes. However, the molecular mechanisms that regulate M2 macrophage polarization, and the detailed process involving activated M2 macrophage in the formation of EIFL have not been determined. Further studies are needed to identify the processes that are involved in EIFL development.
Acknowledgments
Supported by the Catholic Medical Center Research Foundation in the program year of 2016.
Disclosure: J. Baek, None; H.Y. Park, None; J.H. Lee, None; M. Choi, None; J.H. Lee, None; M. Ha, None; M.Y. Lee, None
References
- 1. Ng CH, Cheung N, Wang JJ, et al.. Prevalence and risk factors for epiretinal membranes in a multi-ethnic United States population. Ophthalmology. 2011; 118: 694–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McCarty DJ, Mukesh BN, Chikani V, et al.. Prevalence and associations of epiretinal membranes in the visual impairment project. Am J Ophthalmol. 2005; 140: 288–294. [DOI] [PubMed] [Google Scholar]
- 3. You Q, Xu L, Jonas JB. Prevalence and associations of epiretinal membranes in adult Chinese: the Beijing eye study. Eye (Lond). 2008; 22: 874–879. [DOI] [PubMed] [Google Scholar]
- 4. Schumann RG, Gandorfer A, Ziada J, et al.. Hyalocytes in idiopathic epiretinal membranes: a correlative light and electron microscopic study. Graefes Arch Clin Exp Ophthalmol. 2014; 252: 1887–1894. [DOI] [PubMed] [Google Scholar]
- 5. Gass J. Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment. St Louis, MO: Mosby; 1997. [Google Scholar]
- 6. Takabatake M, Higashide T, Udagawa S, Sugiyama K. postoperative changes and prognostic factors of visual acuity, metamorphopsia, and aniseikonia after vitrectomy for epiretinal membrane. Retina. 2018; 38: 2118–2127. [DOI] [PubMed] [Google Scholar]
- 7. Jeon S, Jung B, Lee WK. Long-term prognostic factors for visual improvement after epiretinal membrane removal. Retina. 2019; 39: 1786–1793. [DOI] [PubMed] [Google Scholar]
- 8. Govetto A, Lalane RA 3rd, Sarraf D, Figueroa MS, Hubschman JP. Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol. 2017; 175: 99–113. [DOI] [PubMed] [Google Scholar]
- 9. Doguizi S, Sekeroglu MA, Ozkoyuncu D, Omay AE, Yilmazbas P. Clinical significance of ectopic inner foveal layers in patients with idiopathic epiretinal membranes. Eye (Lond). 2018; 32: 1652–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Govetto A, Virgili G, Rodriguez FJ, Figueroa MS, Sarraf D, Hubschman JP. Functional and anatomical significance of the ectopic inner foveal layers in eyes with idiopathic epiretinal membranes: surgical results at 12 months. Retina. 2019; 39: 347–357. [DOI] [PubMed] [Google Scholar]
- 11. Campochiaro PA. Pathogenic mechanisms in proliferative vitreoretinopathy. Arch Ophthalmol. 1997; 115: 237–241. [DOI] [PubMed] [Google Scholar]
- 12. Weller M, Wiedemann P, Heimann K. Proliferative vitreoretinopathy—is it anything more than wound healing at the wrong place? Int Ophthalmol. 1990; 14: 105–117. [DOI] [PubMed] [Google Scholar]
- 13. Powell DW, Mifflin RC, Valentich JD, Crowe SE, Saada JI, West AB. Myofibroblasts. I. Paracrine cells important in health and disease. Am J Physiol. 1999; 277: C1–9. [DOI] [PubMed] [Google Scholar]
- 14. Kim JH, Kim YM, Chung EJ, Lee SY, Koh HJ. Structural and functional predictors of visual outcome of epiretinal membrane surgery. Am J Ophthalmol. 2012; 153: 103–110.e101. [DOI] [PubMed] [Google Scholar]
- 15. Shimozono M, Oishi A, Hata M, et al.. The significance of cone outer segment tips as a prognostic factor in epiretinal membrane surgery. Am J Ophthalmol. 2012; 153: 698–704, 704.e691. [DOI] [PubMed] [Google Scholar]
- 16. Watanabe K, Tsunoda K, Mizuno Y, Akiyama K, Noda T. Outer retinal morphology and visual function in patients with idiopathic epiretinal membrane. JAMA Ophthalmol. 2013; 131: 172–177. [DOI] [PubMed] [Google Scholar]
- 17. Shiono A, Kogo J, Klose G, et al.. Photoreceptor outer segment length: a prognostic factor for idiopathic epiretinal membrane surgery. Ophthalmology. 2013; 120: 788–794. [DOI] [PubMed] [Google Scholar]
- 18. Koo HC, Rhim WI, Lee EK. Morphologic and functional association of retinal layers beneath the epiretinal membrane with spectral-domain optical coherence tomography in eyes without photoreceptor abnormality. Graefes Arch Clin Exp Ophthalmol. 2012; 250: 491–498. [DOI] [PubMed] [Google Scholar]
- 19. Song SJ, Lee MY, Smiddy WE. ganglion cell layer thickness and visual improvement after epiretinal membrane surgery. Retina. 2016; 36: 305–310. [DOI] [PubMed] [Google Scholar]
- 20. Cho KH, Park SJ, Cho JH, Woo SJ, Park KH. Inner-retinal irregularity index predicts postoperative visual prognosis in idiopathic epiretinal membrane. American Journal of Ophthalmology. 2016; 168: 139–149. [DOI] [PubMed] [Google Scholar]
- 21. Hashimoto Y, Saito W, Saito M, et al.. Retinal outer layer thickness increases after vitrectomy for epiretinal membrane, and visual improvement positively correlates with photoreceptor outer segment length. Graefes Arch Clin Exp Ophthalmol. 2014; 252: 219–226. [DOI] [PubMed] [Google Scholar]
- 22. Stanley ER, Berg KL, Einstein DB, et al.. Biology and action of colony—stimulating factor-1. Mol Reprod Dev. 1997; 46: 4–10. [DOI] [PubMed] [Google Scholar]
- 23. Martinez FO, Helming L, Gordon S. Alternative activation of macrophages: an immunologic functional perspective. Annu Rev Immunol. 2009; 27: 451–483. [DOI] [PubMed] [Google Scholar]
- 24. Galdiero MR, Garlanda C, Jaillon S, Marone G, Mantovani A. Tumor associated macrophages and neutrophils in tumor progression. J Cell Physiol. 2013; 228: 1404–1412. [DOI] [PubMed] [Google Scholar]
- 25. Kobayashi Y, Yoshida S, Nakama T, et al.. Overexpression of CD163 in vitreous and fibrovascular membranes of patients with proliferative diabetic retinopathy: possible involvement of periostin. Br J Ophthalmol. 2015; 99: 451–456. [DOI] [PubMed] [Google Scholar]
- 26. Sakamoto T, Ishibashi T. Hyalocytes: essential cells of the vitreous cavity in vitreoretinal pathophysiology? Retina. 2011; 31: 222–228. [DOI] [PubMed] [Google Scholar]
- 27. Zhao F, Gandorfer A, Haritoglou C, et al.. Epiretinal cell proliferation in macular pucker and vitreomacular traction syndrome: analysis of flat-mounted internal limiting membrane specimens. Retina. 2013; 33: 77–88. [DOI] [PubMed] [Google Scholar]
- 28. Yoshida S, Kobayashi Y, Nakama T, et al.. Increased expression of M-CSF and IL-13 in vitreous of patients with proliferative diabetic retinopathy: implications for M2 macrophage-involving fibrovascular membrane formation. Br J Ophthalmol. 2015; 99: 629–634. [DOI] [PubMed] [Google Scholar]
- 29. Kono H, Fujii H, Furuya S, et al.. Macrophage colony-stimulating factor expressed in non-cancer tissues provides predictive powers for recurrence in hepatocellular carcinoma. World J Gastroenterol. 2016; 22: 8779–8789. [DOI] [PMC free article] [PubMed] [Google Scholar]



