Abstract
Purpose
This retrospective longitudinal study aimed to examine the relationship between ocular higher-order aberrations (HOA) and axial eye growth in young myopic children undergoing orthokeratology (ortho-k) treatment.
Methods
Axial length and ocular HOA, measured under cycloplegia annually over a 2-year period from the right eyes of myopic children, who previously completed ortho-k clinical trials, were retrieved. Linear mixed model analyses were applied to determine the association between ocular HOA, other known confounding variables (age, sex, and refractive error), and axial eye growth.
Results
Data from 103 subjects were analyzed. The root-mean square (RMS) values of total ocular HOA (third to sixth orders combined), spherical ( and combined), and comatic (, , , and combined) aberrations increased by approximately 3, 9, and 2 times, respectively, after 2 years of ortho-k treatment. After adjusting for age, sex, and refractive error, higher RMS values of total HOA and spherical aberrations were associated with both longer axial length and slower axial elongation (all P < 0.01). For individual Zernike term coefficients, a higher level of positive spherical aberration () was also associated with longer axial length and slower axial elongation (both P < 0.01), after adjusting for baseline HOA.
Conclusions
Ortho-k for myopia control significantly increases the Zernike coefficients and therefore the RMS values for a range of total ocular HOA terms or metrics in children. These findings suggest the potential role of HOA, particularly spherical aberration, as the possible mechanism of slowing axial elongation in ortho-k treatment.
Keywords: higher-order aberrations, spherical aberration, orthokeratology, axial elongation, myopia progression
Myopia, a common cause of distance vision impairment and uncorrected refractive error, is the second most common cause of blindness worldwide.1 Its prevalence has been increasing for decades, particularly in East Asian countries.2 The proportion of the world's population suffering from myopia is estimated to reach 50% by 2050, of whom almost one tenth will become high myopes (≤ −5.00 D),3 if there is no myopia control intervention. Eyes with longer axial length, common in high myopes,4 are associated with increased risks of other ocular complications, including cataract, glaucoma, macular diseases, posterior staphyloma, and chorioretinal degenerations.5 The expenditure on the diagnosis and treatment of these complications can lead to a substantial economic burden to society,6 and therefore early retardation of myopia progression in children is essential.
According to recent longitudinal studies investigating predominantly young myopic children wearing single-vision spectacles,7,8 higher levels of the root-mean-square error (RMS) values of both spherical and comatic aberrations were associated with slower axial elongation. With regard to individual Zernike coefficients, Lau et al.7 showed that more positive spherical aberration and vertical trefoil, and less horizontal trefoil, were associated with slower axial elongation, whereas Hiraoka et al.8 reported a similar trend for spherical aberration and axial elongation, but only observed a significant correlation with coma, not trefoil. These non-interventional observational studies support the potential role of specific habitual higher-order aberrations (HOA) in the regulation of childhood eye growth and myopia progression. During orthokeratology (ortho-k) treatment, an established effective intervention for myopia control,9 the cornea is reshaped,10 which significantly alters the profile of corneal and total ocular HOA.11 Therefore it is of particular interest to investigate if the changes induced in the ocular HOA profile during ortho-k treatment are associated with axial elongation in children, which may help to further the current understanding of the underlying mechanism of ortho-k for myopia control.
Some longitudinal studies have investigated the relationship between HOA and axial elongation after ortho-k treatment. Santodomingo-Rubido et al.12 analyzed the changes in corneal HOA of 29 children (mean age: 9.6 ± 1.6 years) after 2 years of ortho-k treatment and suggested that despite significant increases in HOA, these changes were not correlated with axial elongation. However, internal aberrations from the posterior cornea or the crystalline lens may partially compensate for the significant increase in corneal HOA during ortho-k treatment. Changes in total ocular spherical aberration RMS or spherical aberration RMS plateau over time in comparison with changes in corneal spherical aberration,13,14 potentially due to compensatory changes in shape or thickness of the crystalline lens.11,15 Hence, analyzing corneal HOA only may not provide a comprehensive understanding of the influence of HOA on axial elongation, whereas ocular HOA would more closely reflect the quality of the retinal image.16 In addition, this study12 may be underpowered due to the small sample size (n = 29). Hiraoka et al.13 examined the influence of both corneal and ocular HOA on axial elongation in 55 young myopic children (mean age 10.3 ± 1.4 years) undergoing ortho-k treatment for 1 year. For both corneal and ocular HOA, both spherical and comatic aberrations were negatively associated with axial elongation, with comatic aberrations displaying the strongest correlation. However, in their regression analysis, other confounding factors such as age and sex, which also affect axial elongation,17 were not accounted for. More recently, Kim et al.18 investigated various ocular parameters of 17 children (mean age 8.6 ± 0.8 years) and their association with myopia control efficacy in ortho-k. They showed that less peripheral myopia (based on peripheral axial length measurements), more asymmetric optical changes, and comatic aberrations induced by ortho-k, were associated with less axial elongation. However, the limited sample size of 17 participants is likely insufficient for such a multivariate analysis.
To date, only a limited number of studies have examined the influence of ocular HOA on axial elongation in children receiving ortho-k treatment and the potential role of HOA underlying the mechanism of ortho-k for myopia control. The primary aim of this study was therefore to examine the relationship between the change in ocular HOA and axial elongation in young myopic children treated with ortho-k over a 2-year period, while controlling for known confounding variables.
Methods
Study Design
This retrospective study included data from subjects receiving ortho-k treatment who completed previous 2-year longitudinal clinical trials (ROMIO,19 TO-SEE,20 HM-PRO,21 PR [a subset of Lee & Cho]22 studies). All previous studies were conducted with written informed consent and in accordance with the tenets of the Declaration of Helsinki and were approved by the Departmental Research Committee of the School of Optometry of The Hong Kong Polytechnic University. All studies were also registered at ClinicalTrials.gov (ROMIO: NCT00962208; TO-SEE: NCT00978692; HM-PRO: NCT00977236; PR: NCT00978679).
Subjects and Procedures
Table 1 summarizes the baseline demographics and refractive errors of the subjects included in this analysis from previous ortho-k studies.19–22 Young children of different levels of myopia and astigmatism were either partially corrected with ortho-k lenses with residual refractive error corrected with spectacles (HM-PRO21 study only) or fully corrected with ortho-k lenses (all other studies).
Table 1.
Description and Baseline Demographics (Mean ± SD or Median [Min, Max]) of Ortho-k Subjects Retrieved from ROMIO,19 TO-SEE,20 HM-PRO,21 and PR (A Subset of Lee and Cho's Study)22 Studies
| Studies | ROMIO | TO-SEE | HM-PRO | PR |
|---|---|---|---|---|
| Description | Low to moderate myopes | High astigmats | High myopes | Low to moderate myopes |
| Number of subjects | 34 | 34 | 7 | 28 |
| Age, years | 9.3 ± 1.0 | 9.4 ± 1.4 | 10.6 ± 0.9 | 8.2 ± 0.9 |
| Myopia, D | −2.05 ± 0.75 | −2.49 ± 1.34 | −6.82 ± 0.95 | −3.11 ± 0.65 |
| Astigmatism, D | 0.00 [−1.00, 0.00] | −1.63 ± 0.60 | −0.61 ± 0.40 | −0.38 [−1.00, 0.00] |
| Spherical equivalent refraction, D | −2.17 ± 0.80 | −3.30 ± 1.44 | −7.13 ± 0.94 | −3.33 ± 0.70 |
| Axial length, mm | 24.54 ± 0.68 | 24.35 ± 0.89 | 25.61 ± 0.71 | 24.42 ± 0.65 |
All subjects underwent annual cycloplegic data collection, with the instillation of 1 drop of 0.5% proparacaine, 1% tropicamide, and 1% cyclopentolate, each separated by 5 minutes. The data (cycloplegic subjective refraction, axial length, and ocular aberrations) were obtained by a masked examiner. Cycloplegic subjective refraction was performed following the principle of maximum plus for maximum visual acuity. Axial length was determined, as the average of 5 measurements with a maximum difference of 0.02 mm and a signal-to-noise ratio of more than 3.5, with the IOLMaster 500 (Carl Zeiss Meditec, Dublin, CA, USA). Monochromatic ocular HOA for a wavelength of 555 µm were measured using a Shack-Hartmann aberrometer (Complete Ophthalmic Analysis System [COAS]; Wavefront Sciences Ltd., New Mexico, USA). The average of at least 5 measurements was used for analysis. The acquired data were fitted with a sixth-order Zernike polynomial using a fixed 6-mm pupil diameter. The RMS values of total HOA, spherical, and comatic aberrations were computed as the square root of the sum of squares of corresponding terms (total: from third- to sixth-order terms; spherical aberrations: and combined; comatic aberrations: , , , and combined) as applied in previous analyses of young spectacle-wearing children.7
Statistical Analysis
All statistical analyses were performed using SPSS 23 version (IBM Corp., Armonk, NY, USA). To prevent the inflation of P-values when including data from fellow eyes23 and the influence of mirror symmetry between eyes confounding aberration analyses,24 only data from right eyes were analyzed. Subjects with missing total HOA data at the baseline visit were excluded. Repeated measures analysis of variance tests, with Bonferroni corrections, were used to compare the changes in spherical equivalent refraction (SER), axial length, and RMS values of total HOA, spherical, and comatic aberrations, and individual Zernike coefficients between visits.
In order to identify baseline characteristics associated with total HOA RMS, spherical and comatic aberrations RMS, and corresponding Zernike coefficients for particular RMS metrics (spherical aberrations: and ; comatic aberrations: , , , and ) at baseline, linear mixed models were used to examine the effects of age, sex, and axial length (similar modelling was repeated for SER to avoid multicollinearity issues) on HOA terms or RMS metrics, with a first-order autoregressive covariance structure and restricted maximum likelihood estimation. Individual subject's slope and intercept were included as random effects using an unstructured covariance matrix to control for intersubject variations.
Regarding the influence of the changes in HOA on axial elongation, the age of the subjects was transformed (using a natural logarithm) to improve the fit of the models.7,25 To account for sporadic and random missing data in the follow-ups, another linear mixed model was applied to investigate the effect of total HOA RMS on axial elongation. Adjustments for other predictive variables (age, sex, baseline SER, and baseline total HOA RMS) were performed to control for their influence on axial elongation. The model used a first-order autoregressive covariance structure and restricted maximum likelihood estimation. Similar modelling was also applied to investigate the association between HOA terms and metrics and axial elongation; specifically, the specific RMS values for spherical and comatic aberrations, and the corresponding Zernike coefficients (spherical aberrations: and ; comatic aberrations: , , , and ). A backward stepwise approach was utilized with the least significant factor removed and the Akaike information criterion was used to compare the goodness of fit between different models.26
Results
Data from 103 participants (51 girls and 52 boys; median [range] age 9.1 [6.3–13.0] years) with a median [range] SER of −2.88 [−8.63 to −0.38] D and mean axial length of 24.52 ± 0.80 mm at baseline, were retrieved for analysis. Table 2 summarizes the demographics and ocular HOA at each visit (note that only data available for all visits [baseline, first, second year] are presented). Most parameters, except for age and axial length, were stable at the 1-year visit, with no further significant changes observed thereafter. After 2 years of ortho-k treatment, the SER decreased by −2.63 ± 1.30 D (F[1.28, 93.39] = 273.84, P < 0.001) and the axial length increased by 0.41 ± 0.32 mm (F[1.13, 100.52] = 137.02, P < 0.001). The RMS values of the total HOA, spherical, and comatic aberrations increased by 0.74 ± 0.56 µm, 0.78 ± 0.51 µm, and 0.17 ± 0.29 µm, respectively (total HOA: F[1.55, 124.17] = 103.32, P < 0.001; spherical aberrations: F[1.56, 124.40] = 140.72, P < 0.001; comatic aberrations: F[1.75, 139.57] = 19.52, P < 0.001).
Table 2.
Demographics and Higher-order Aberrations (Mean ± SD) of the Pooled Population at Different Visits (Note that Only Data from Subjects with Data Available from All Visits are Presented)
| Baseline | First year | Second year | |
|---|---|---|---|
| Demographics | |||
| Age, years (n = 91) | 9.3 ± 1.3 | 10.4 ± 1.2 | 11.4 ± 1.2 |
| Spherical equivalent refraction, D (n = 74) | −3.11 ± 1.78 | −0.61 ± 1.03 | −0.48 ± 0.87 |
| Axial length, mm (n = 90) | 24.52 ± 0.82 | 24.75 ± 0.80 | 24.93 ± 0.82 |
| Higher-order aberrations, µm (n = 81) | |||
| Total higher-order aberrations RMS | 0.31 ± 0.09 | 1.05 ± 0.64 | 1.05 ± 0.56 |
| Spherical aberrations RMS | 0.09 ± 0.07 | 0.85 ± 0.55 | 0.88 ± 0.53 |
| Primary spherical aberration () | 0.06 ± 0.09 | 0.84 ± 0.54 | 0.86 ± 0.52 |
| Secondary spherical aberration () | −0.02 ± 0.02 | 0.08 ± 0.17 | 0.07 ± 0.16 |
| Comatic aberrations RMS | 0.19 ± 0.11 | 0.41 ± 0.38 | 0.36 ± 0.26 |
| Primary vertical coma () | 0.11 ± 0.17 | −0.04 ± 0.35 | −0.08 ± 0.25 |
| Primary horizontal coma () | −0.02 ± 0.08 | 0.16 ± 0.37 | 0.09 ± 0.29 |
| Secondary vertical coma () | 0.02 ± 0.03 | 0.04 ± 0.11 | 0.05 ± 0.12 |
| Secondary horizontal coma () | 0.00 ± 0.01 | 0.01 ± 0.15 | −0.02 ± 0.13 |
Regarding the influence of baseline demographics on baseline HOA terms or metrics, using baseline SER in the modelling, girls exhibited more primary vertical coma (: β = 0.07, P = 0.04), whereas more (negative) SER was associated with less primary and secondary horizontal coma (: β = 0.01 µm/D, p = 0.02; : β = 0.003 µm/D, P = 0.01). In both the modeling using baseline axial length and SER, older children had less secondary vertical coma (: β = −0.01 µm/year, 0.01 < P < 0.02). No associations were found for other Zernike terms or specific RMS values (all P > 0.05).
From the linear mixed model analyses (Model 1, Table 3), as expected, axial length was longer in boys (0.46 mm longer, P < 0.001), increased with age (P < 0.001), and less so in ortho-k subjects with lower baseline SER (i.e., 0.24 mm shorter per 1 D of SER, P < 0.001). After adjusting for baseline HOA (or corresponding RMS values), higher levels of RMS values for total HOA and spherical aberrations were associated with longer axial length (total HOA RMS: β = 0.96 mm/µm, P < 0.001, model 1; spherical aberrations RMS: β = 0.91 mm/µm, P = 0.008, model 2) and slower axial elongation (total HOA RMS: β = −0.43 mm year−1/µm, P < 0.001, model 1; spherical aberrations RMS: β = −0.39 mm year−1/µm, P = 0.007, model 2). When investigating the influence of individual spherical and comatic Zernike coefficients, a higher level of positive spherical aberration () was associated with longer axial length (β = 0.99 mm/µm, P = 0.007) and slower axial elongation (β = −0.46 mm year−1/µm, P = 0.004, model 3). No associations between the RMS of comatic aberrations or individual comatic Zernike terms and axial length or its elongation were observed (all P > 0.05, models 2 and 4).
Table 3.
Statistically Significant Fixed Effects and Parameter Estimates (β) of the Influences of Changes in Axial Length
| β | P | |
|---|---|---|
| Model 1 – total HOA RMS | ||
| Intercept | 19.00 | <0.001 |
| Sex* | −0.46 | <0.001 |
| ln(age) | 2.33 | <0.001 |
| Baseline spherical equivalent refraction | −0.24 | <0.001 |
| RMS of total HOA | 0.96 | <0.001 |
| Time by RMS of total HOA | −0.43 | <0.001 |
| Model 2 – specific RMS (spherical and comatic) | ||
| Intercept | 19.23 | <0.001 |
| Sex* | −0.45 | 0.002 |
| ln(age) | 2.23 | <0.001 |
| Baseline spherical equivalent refraction | −0.24 | <0.001 |
| RMS of spherical aberrations | 0.91 | 0.008 |
| Time by RMS of spherical aberrations | −0.39 | 0.007 |
| Model 3 – spherical Zernike terms ( and ) | ||
| Intercept | 19.30 | <0.001 |
| Sex* | −0.46 | <0.001 |
| ln(age) | 2.28 | <0.001 |
| Baseline spherical equivalent refraction | −0.22 | <0.001 |
| Baseline primary spherical aberration () | −1.42 | 0.012 |
| Baseline secondary spherical aberration () | 9.28 | 0.012 |
| Primary spherical aberration () | 0.99 | 0.007 |
| Time by primary spherical aberration () | −0.46 | 0.004 |
| Model 4 – comatic Zernike terms (, , , and ) | ||
| Intercept | 19.51 | <0.001 |
| Sex* | −0.49 | <0.001 |
| ln(age) | 2.03 | <0.001 |
| Baseline spherical equivalent refraction | −0.24 | <0.001 |
Other parameters and interactions showing statistical insignificance are not shown.
Parameter estimate for girls.
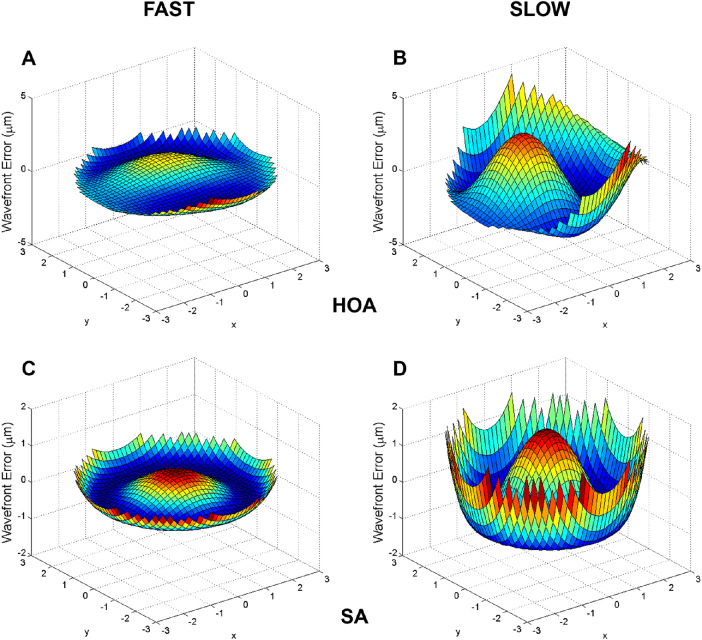
The Figure shows the wavefront height difference maps (2-year visit minus baseline visit) for 2 representative participants exhibiting relatively fast and slow axial elongation over the 2-year study period. This figure highlights the rapid change of wavefront error in spherical pattern towards the edge of the pupil, indicating a higher level of spherical aberration in the participant with relatively slower axial elongation compared with another participant with relatively faster axial elongation.
Figure.
Wavefront height difference maps (2-year visit minus baseline visit) for 2 representative participants exhibiting relatively fast and slow axial elongation over the 2-year study period. Fast: participant 190: 0.64 mm axial elongation, +0.22 µm change in spherical aberration, +0.35 µm change in HOA RMS. Slow: participant 252: 0.05 mm axial elongation, +0.74 µm change in spherical aberration, +1.47 µm change in HOA RMS. Note: the z-axis scale differs for the total ocular higher-order aberration (HOA) plots and the total ocular spherical aberration (SA) plots.
Discussion
The results of this study demonstrate a significant association between ocular HOA, especially spherical aberration, and axial elongation in children undergoing ortho-k treatment, after accounting for known confounding variables. Greater RMS values of total HOA and spherical aberrations, and a higher level of positive spherical aberration (), were associated with slower axial eye growth. The association observed between HOA, which impact on retinal image quality,27 visual function,28 and axial elongation found in the current study, provides further insight regarding the potential mechanism underlying the retardation of axial elongation in children treated with ortho-k.
HOA increased dramatically after ortho-k treatment in our subjects, consistent with previous studies,11,13,14,18,29–31 although the magnitude of change varied substantially with the pupil size analyzed,32 age of subjects,33 lens design,34 and duration of follow-up.14 For example, Gifford et al.11 found an approximately doubling in total HOA, spherical, and comatic aberrations (over a 4-mm pupil) in young adults (mean age 21.1 ± 1.8 years) wearing ortho-k for 1 week, whereas Hiraoka et al.13 reported a tripling in the RMS values for total HOA, spherical, and comatic aberrations (over a 5-mm pupil, up to the fourth order) in their cohort (mean age 10.3 ± 1.4 years) undergoing ortho-k treatment for 1 year. In the participants of this study (mean age 9.1 ± 1.3 years) analyzed over a 6-mm pupil, the total HOA, spherical, and comatic aberrations RMS increased by 3, 9, and 2 times, respectively, after ortho-k treatment. Similar to the findings of Joslin et al.31 and Chen et al.,15 primary spherical aberration () and horizontal coma () were the most affected individual Zernike coefficients. The increase in positive spherical aberration has been previously attributed to the nature of corneal asphericity, as the reverse geometry ortho-k lens flattens the central cornea and changes its shape from prolate to oblate, whereas the increase in comatic aberrations is associated with lens decentration, similar to the change in HOA observed with a decentered LASIK treatment zone.35 In addition, other researchers have shown that larger increases in spherical and comatic aberration RMS values were associated with more myopic correction11 (resulting in a greater change in the corneal profile across the treatment zone) and greater lens decentration,36,37 respectively, during ortho-k treatment.
The association between ocular HOA and axial elongation, with adjustment for other confounders, was similarly analyzed in spectacle-wearing children by Lau et al.,7 and higher levels of ocular HOA were associated with slower axial elongation. Referring to the beta coefficients in both models of spectacle-wearing7 and ortho-k treated children in this study, the association between ocular HOA and axial elongation was modest in comparison to the effects of age, sex, and the change in SER. However, following ortho-k treatment, ocular HOA increased significantly by about 3 to 9 times (and 14 times for primary spherical aberration) (Table 2) and consequently the association between ocular HOA and axial elongation in ortho-k treated children also increased compared with spectacle-wearing children (a 3-4 times increase in beta coefficients for models 1 and 2).
Based on a series of simulations combining different magnitudes of coefficients for specific HOA terms that vary during accommodation in down gaze (spherical aberration, trefoil along 30 degrees and vertical coma),38 Buehren et al.39 proposed that the magnitude and sign of HOA, especially spherical aberration, may provide a directional cue to the retina, which could lead to compensatory eye growth to optimize image quality. Spherical aberration values of −0.2 to −0.3 µm or less (more negative) for a 5-mm pupil required clinically significant changes (at least 0.25 D) in the best sphere correction to optimize the retinal image quality. Thibos et al.40 also performed computational modelling and investigated the coupling effect of the sign of spherical aberration and defocus on retinal image quality. They reported that positive spherical aberration may have a protective effect against myopia progression because, in combination with hyperopic defocus that is often present in young myopes with a lag of accommodation during near work,41,42 this improved the retinal image quality in comparison with the combination of negative spherical aberration and hyperopic defocus. In addition, from Tarrant et al.43 study investigating the predictive values of certain optical quality metrics in defining the plane of best focus, using accommodative and HOA data obtained from emmetropic and myopic adults, defocus alone may not be a good measure. They indicated the importance of the interaction between defocus and spherical aberration on affecting the retinal image quality. The significant increase in HOA, particularly spherical aberration, due to ortho-k may therefore be linked mechanistically to the slowed axial elongation with this treatment in myopic children.
Since baseline HOA may affect axial elongation as observed in spectacle-wearing children,7 linear mixed models were also performed on specific HOA terms or metrics measured at baseline. These analyses revealed that the majority of HOA terms and metrics (except for primary and secondary horizontal coma) were not significantly associated with sex, age, and axial length (or SER) at baseline in our cohort of subjects, similar to those reported in a review by Little et al.44 More importantly, in the modelling presented in the current study, baseline HOA terms or metrics, and baseline SER were included as fixed factors and any potential influence of these factors were accounted for in the statistical models.
Santodomingo-Rubido et al.12 reported no correlations between corneal HOA and axial elongation in children undergoing ortho-k. However, corneal HOA do not accurately represent the true retinal image quality (i.e., derived from the ocular HOA) due the partial compensatory changes observed in the internal optics of the eye.45,46 Hiraoka et al.13 and Kim et al.18 applied multiple linear regressions and generalized estimating equations to identify significant factors associated with axial elongation after performing simple correlations between predictors and axial elongation. They showed that higher levels of comatic aberrations RMS were significantly associated with slower axial elongation. However, potentially significant terms may be missed using correlation analyses without statistical adjustments for other known confounders. Multicollinearity may also be a limiting factor in some of their modelling which included both second-order Zernike coefficients (defocus and astigmatism) and spherical equivalent refractive error (highly correlated variables) as predictors of axial elongation.
In addition, in order to compare the average changes in primary spherical aberration () across previous studies13,18 and the current study, data were extracted from Kim et al.18 and Hiraoka et al.13 (using WebPlotDigitizer, https://automeris.io/WebPlotDigitizer/ and rescaled to a 6-mm pupil diameter).47 Over a 6-mm pupil diameter, the mean change in ocular primary spherical aberration after 2 years of ortho-k treatment was +0.80 µm in the current study compared with +0.51 µm in Hiraoka et al.13, and +0.34 µm in Kim et al.18 These differences in the change in primary spherical aberration () between the studies may be a result of lens design (given that compression factor appears to influence spherical aberration),48 ethnicity, or some other factors, and likely explain the different reported associations between eye growth and changes in spherical aberration.
Pupil size is another potential factor affecting axial elongation in ortho-k treated eyes.49,50 Chen et al.49 investigated the association between axial elongation and pupil size in 25 children treated with ortho-k and reported an association between slower axial elongation and larger pupil size (compared to the average sample mean). Faria-Ribeiro et al.50 analyzed the influence of pupil sizes from 3 to 6 mm in simulated eye models and suggested that the effectiveness of myopia control may be enhanced in eyes with larger pupils due to increased exposure to peripheral defocus. Therefore, not only the change in corneal optics (e.g., more positive spherical aberration), but the natural pupil size may also influence axial elongation and the extent of myopia control. Variations in the pupil size used for HOA analyses may also explain some inconsistencies observed between studies. For example, Hiraoka et al.13 performed HOA analysis using a 4-mm pupil, which was smaller than the average photopic pupil size of young children reported in a previous study (5.4 mm)51 and may therefore underestimate the true increase in HOA induced by changes in the mid-peripheral cornea towards the edge of the treatment zone. However, little is known about the effect of treatment zone size on axial elongation in children treated with ortho-k and further investigations with adjustment for other known covariates are warranted.
Other researchers have also attempted to control axial elongation by altering the ocular HOA profile. Allen et al.52 attempted to arrest myopia progression by using contact lenses that altered the patient's primary spherical aberration to −0.1 µm over a 5-mm pupil, because this had previously been shown to improve accommodation, that is, reduce accommodation lags, in adults.53 However, they were unable to show any significant myopia control with these lenses over a 2-year period. On the other hand, Sankaridurg et al.54 recently showed a modest myopia control effect in subjects wearing extended depth-of-focus contact lenses (+1.75 D and +1.25 D; 25%–28% slower) modulated by HOA (details not provided) and center distance multifocal lens designs (23%–32% slower), compared with single-vision control lenses, in 508 children (mean age 10.4 ± 1.3 years) over a 2-year period. Cheng et al.55 also demonstrated a moderate effect with soft contact lenses of higher positive spherical aberrations (about 0.175 µm for a 5-mm aperture) in 127 children (mean age 9.2 ± 1.1 years). Axial elongation in the treated eyes were 65% (0.11 mm) and 39% (0.14 mm) shorter than the control eyes after 6 and 12 months, respectively. However, the magnitude of spherical aberration induced by these soft contact lenses was much smaller, compared with the amount induced by ortho-k treatment (0.39 µm increase in in this study [rescaled for a 5-mm pupil size]). Because the “minimum effective dose” of positive spherical aberration required to alter axial elongation in children remains unknown, further investigation of the relationship between spherical aberration and axial elongation for other optical interventions for myopia control is also warranted. A recent study48 investigated the changes in ocular HOA with ortho-k lens wear after adjusting the compression factor (also known as Jessen factor) of a specific brand of ortho-k lens (Menicon Z Night or Menicon Z Night Toric lenses; NKL Contactlenzen B.V., Emmen, The Netherlands). The study showed that increasing the compression factor by 1.00 D significantly increased the primary spherical aberration (), RMS values of spherical aberrations, and total HOA by 40–50%, without significantly inducing more refractive changes or compromising vision in photopic conditions. It would be of interest to determine if the intentional modification of the amount of ocular HOA, particularly spherical aberration, can improve myopia control efficacy in ortho-k treatment.
One limitation of our study is that the numbers of children with different refractive errors (low and high myopia, high astigmatism) were not large enough to conduct separate analyses on the association between ocular HOA and axial elongation in different refractive error groups treated with ortho-k. As a result, all subjects were pooled together to provide a general understanding of the association between HOA and axial eye growth with ortho-k treatment. Because emmetropization is a complex, multifactorial process, other possible confounding factors such as pupil size,49,50 parental myopia,56 outdoor activities,57 and living conditions58 should also be evaluated in future studies (or controlled for with statistical modeling).
In conclusion, this study investigated the relationship between ocular HOA and axial elongation in young subjects wearing ortho-k lenses and found that higher levels of total HOA RMS, spherical aberration RMS, and positive primary spherical aberration were associated with slower axial elongation, after adjusting for confounders, such as age, baseline refraction, and baseline HOA. The increase in ocular HOA, notably spherical aberration, and its association with slower axial elongation, may be the mechanism of ortho-k in myopia control. Optical treatments that optimize the ocular HOA profile without significantly compromising visual function may yield a superior myopia control outcome.
Acknowledgments
The authors thank Maureen Boost for her advice in the revision of manuscript and Connie Chen, Jessie Charm, and Tsui-Tsui Lee for providing data from previous studies.
Supported by Collaborative Research Agreements between The Hong Kong Polytechnic University and Menicon Co. Ltd., Japan (current [ZG3Z], ROMIO [ZG13], TO-SEE [ZG13], and PR [ZG30] studies), and Procornea Co. Ltd., Netherlands (HM-PRO [ZG41] study), and Research Residency Scheme of the School of Optometry, PolyU (JKL).
Disclosure: J.K. Lau, None; S.J. Vincent, None; S.-W. Cheung, None; P. Cho, None
References
- 1. Bourne RR, Stevens GA, White RA, et al.. Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Health. 2013; 1: e339–49. [DOI] [PubMed] [Google Scholar]
- 2. Rudnicka AR, Kapetanakis VV, Wathern AK, et al.. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016; 100: 882–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Holden BA, Fricke TR, Wilson DA, et al.. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016; 123: 1036–42. [DOI] [PubMed] [Google Scholar]
- 4. Park SH, Park KH, Kim JM, Choi CY. Relation between axial length and ocular parameters. Ophthalmologica. 2010; 224: 188–93. [DOI] [PubMed] [Google Scholar]
- 5. Ikuno Y. Overview of the complications of high myopia. Retina. 2017; 37: 2347–51. [DOI] [PubMed] [Google Scholar]
- 6. Rein DB, Zhang P, Wirth KE, et al.. The economic burden of major adult visual disorders in the United States. Arch Ophthalmol. 2006; 124: 1754–60. [DOI] [PubMed] [Google Scholar]
- 7. Lau JK, Vincent SJ, Collins MJ, Cheung SW, Cho P. Ocular higher-order aberrations and axial eye growth in young Hong Kong children. Sci Rep. 2018; 8: 6726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hiraoka T, Kotsuka J, Kakita T, Okamoto F, Oshika T. Relationship between higher-order wavefront aberrations and natural progression of myopia in schoolchildren. Sci Rep. 2017; 7: 7876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huang J, Wen D, Wang Q, et al.. Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology. 2016; 123: 697–708. [DOI] [PubMed] [Google Scholar]
- 10. Nichols JJ, Marsich MM, Nguyen M, Barr JT, Bullimore MA. Overnight orthokeratology. Optom Vis Sci. 2000; 77: 252–9. [DOI] [PubMed] [Google Scholar]
- 11. Gifford P, Li M, Lu H, Miu J, Panjaya M, Swarbrick HA. Corneal versus ocular aberrations after overnight orthokeratology. Optom Vis Sci. 2013; 90: 439–47. [DOI] [PubMed] [Google Scholar]
- 12. Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutierrez-Ortega R, Suzaki A. Short- and long-term changes in corneal aberrations and axial length induced by orthokeratology in children are not correlated. Eye Contact Lens. 2016; 43: 358–65. [DOI] [PubMed] [Google Scholar]
- 13. Hiraoka T, Kakita T, Okamoto F, Oshika T. Influence of ocular wavefront aberrations on axial length elongation in myopic children treated with overnight orthokeratology. Ophthalmology. 2015; 122: 93–100. [DOI] [PubMed] [Google Scholar]
- 14. Lian Y, Shen M, Huang S, et al.. Corneal reshaping and wavefront aberrations during overnight orthokeratology. Eye Contact Lens. 2014; 40: 161–8. [DOI] [PubMed] [Google Scholar]
- 15. Chen Q, Li M, Yuan Y, et al.. Interaction between corneal and internal ocular aberrations induced by orthokeratology and its influential factors. Biomed Res Int. 2017; 2017: 3703854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mrochen M, Jankov M, Bueeler M, Seiler T. Correlation between corneal and total wavefront aberrations in myopic eyes. J Refract Surg. 2003; 19: 104–12. [DOI] [PubMed] [Google Scholar]
- 17. Zadnik K, Manny RE, Yu JA, et al.. Ocular component data in schoolchildren as a function of age and gender. Optom Vis Sci. 2003; 80: 226–36. [DOI] [PubMed] [Google Scholar]
- 18. Kim J, Lim DH, Han SH, Chung TY. Predictive factors associated with axial length growth and myopia progression in orthokeratology. PLoS One. 2019; 14: e0218140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cho P, Cheung SW. Retardation of myopia in orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012; 53: 7077–85. [DOI] [PubMed] [Google Scholar]
- 20. Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology (TO-SEE study). Invest Ophthalmol Vis Sci. 2013; 54: 6510–7. [DOI] [PubMed] [Google Scholar]
- 21. Charm J, Cho P. High myopia—partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013; 90: 530–9. [DOI] [PubMed] [Google Scholar]
- 22. Lee TT, Cho P. Relative peripheral refraction in children: twelve-month changes in eyes with different ametropias. Ophthalmic Physiol Opt. 2013; 33: 283–93. [DOI] [PubMed] [Google Scholar]
- 23. Armstrong RA. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol Opt. 2013; 33: 7–14. [DOI] [PubMed] [Google Scholar]
- 24. Gatinel D, Delair E, Abi-Farah H, Hoang-Xuan T. Distribution and enantiomorphism of higher-order ocular optical aberrations. J Fr Ophtalmol. 2005; 28: 1041–50. [DOI] [PubMed] [Google Scholar]
- 25. Zadnik K, Mutti DO, Mitchell GL, Jones LA, Burr D, Moeschberger ML. Normal eye growth in emmetropic schoolchildren. Optom Vis Sci. 2004; 81: 819–28. [DOI] [PubMed] [Google Scholar]
- 26. Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974; 19: 716–23. [Google Scholar]
- 27. Collins MJ, Buehren T, Iskander DR. Retinal image quality, reading and myopia. Vision Res. 2006; 46: 196–215. [DOI] [PubMed] [Google Scholar]
- 28. Yang YR, Zhao JL, Xiao F, Zhao HX, Dai Y. Effect of high-order aberrations on pattern-reversal visual evoked potentials. Vision Res. 2019; 161: 52–9. [DOI] [PubMed] [Google Scholar]
- 29. Stillitano I, Schor P, Lipener C, Hofling-Lima AL. Long-term follow-up of orthokeratology corneal reshaping using wavefront aberrometry and contrast sensitivity. Eye Contact Lens. 2008; 34: 140–5. [DOI] [PubMed] [Google Scholar]
- 30. Berntsen DA, Barr JT, Mitchell GL. The effect of overnight contact lens corneal reshaping on higher-order aberrations and best-corrected visual acuity. Optom Vis Sci. 2005; 82: 490–7. [DOI] [PubMed] [Google Scholar]
- 31. Joslin CE, Wu SM, McMahon TT, Shahidi M. Higher-order wavefront aberrations in corneal refractive therapy. Optom Vis Sci. 2003; 80: 805–11. [DOI] [PubMed] [Google Scholar]
- 32. Carkeet A, Velaedan S, Tan YK, Lee DY, Tan DT. Higher order ocular aberrations after cycloplegic and non-cycloplegic pupil dilation. J Refract Surg. 2003; 19: 316–22. [DOI] [PubMed] [Google Scholar]
- 33. Brunette I, Bueno JM, Parent M, Hamam H, Simonet P. Monochromatic aberrations as a function of age, from childhood to advanced age. Invest Ophthalmol Vis Sci. 2003; 44: 5438–46. [DOI] [PubMed] [Google Scholar]
- 34. Kang P, Gifford P, Swarbrick H. Can manipulation of orthokeratology lens parameters modify peripheral refraction? Optom Vis Sci. 2013; 90: 1237–48. [DOI] [PubMed] [Google Scholar]
- 35. Moreno-Barriuso E, Lloves JM, Marcos S, Navarro R, Llorente L, Barbero S. Ocular aberrations before and after myopic corneal refractive surgery: LASIK-induced changes measured with laser ray tracing. Invest Ophthalmol Vis Sci. 2001; 42: 1396–403. [PubMed] [Google Scholar]
- 36. Hiraoka T, Mihashi T, Okamoto C, Okamoto F, Hirohara Y, Oshika T. Influence of induced decentered orthokeratology lens on ocular higher-order wavefront aberrations and contrast sensitivity function. J Cataract Refract Surg. 2009; 35: 1918–26. [DOI] [PubMed] [Google Scholar]
- 37. Yang X, Zhong X, Gong X, Zeng J. Topographical evaluation of the decentration of orthokeratology lenses. Yan Ke Xue Bao. 2005; 21: 132–5. [PubMed] [Google Scholar]
- 38. Buehren T, Collins MJ, Carney LG. Near work induced wavefront aberrations in myopia. Vision Res. 2005; 45: 1297–312. [DOI] [PubMed] [Google Scholar]
- 39. Buehren T, Iskander DR, Collins MJ, Davis B. Potential higher-order aberration cues for sphero-cylindrical refractive error development. Optom Vis Sci. 2007; 84: 163–74. [DOI] [PubMed] [Google Scholar]
- 40. Thibos LN, Bradley A, Liu T, Lopez-Gil N. Spherical aberration and the sign of defocus. Optom Vis Sci. 2013; 90: 1284–91. [DOI] [PubMed] [Google Scholar]
- 41. Gwiazda J, Thorn F, Bauer J, Held R. Myopic children show insufficient accommodative response to blur. Invest Ophthalmol Vis Sci. 1993; 34: 690–4. [PubMed] [Google Scholar]
- 42. Gwiazda J, Bauer J, Thorn F, Held R. A dynamic relationship between myopia and blur-driven accommodation in school-aged children. Vision Res. 1995; 35: 1299–304. [DOI] [PubMed] [Google Scholar]
- 43. Tarrant J, Roorda A, Wildsoet CF. Determining the accommodative response from wavefront aberrations. J Vis. 2010; 10: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Little JA, McCullough SJ, Breslin KM, Saunders KJ. Higher order ocular aberrations and their relation to refractive error and ocular biometry in children. Invest Ophthalmol Vis Sci. 2014; 55: 4791–800. [DOI] [PubMed] [Google Scholar]
- 45. Artal P, Guirao A, Berrio E, Williams DR. Compensation of corneal aberrations by the internal optics in the human eye. J Vis. 2001; 1: 1–8. [DOI] [PubMed] [Google Scholar]
- 46. Kelly JE, Mihashi T, Howland HC. Compensation of corneal horizontal/vertical astigmatism, lateral coma, and spherical aberration by internal optics of the eye. J Vis. 2004; 4: 262–71. [DOI] [PubMed] [Google Scholar]
- 47. Schwiegerling J. Scaling Zernike expansion coefficients to different pupil sizes. J Opt Soc Am A. 2002; 19: 1937–45. [DOI] [PubMed] [Google Scholar]
- 48. Lau JK, Vincent SJ, Cheung SW, Cho P. The influence of orthokeratology compression factor on ocular higher-order aberrations. Clin Exp Optom. 2020; 103: 123–8. [DOI] [PubMed] [Google Scholar]
- 49. Chen Z, Niu L, Xue F, et al.. Impact of pupil diameter on axial growth in orthokeratology. Optom Vis Sci. 2012; 89: 1636–40. [DOI] [PubMed] [Google Scholar]
- 50. Faria-Ribeiro M, Navarro R, Gonzalez-Meijome JM. Effect of pupil size on wavefront refraction during orthokeratology. Optom Vis Sci. 2016; 93: 1399–408. [DOI] [PubMed] [Google Scholar]
- 51. Schulle KL, Berntsen DA, Sinnott LT, et al.. Visual acuity and over-refraction in myopic children fitted with soft multifocal contact lenses. Optom Vis Sci. 2018; 95: 292–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Allen PM, Radhakrishnan H, Price H, et al.. A randomised clinical trial to assess the effect of a dual treatment on myopia progression: the Cambridge Anti-Myopia Study. Ophthalmic Physiol Opt. 2013; 33: 267–76. [DOI] [PubMed] [Google Scholar]
- 53. Allen PM, Radhakrishnan H, Rae S, et al.. Aberration control and vision training as an effective means of improving accommodation in individuals with myopia. Invest Ophthalmol Vis Sci. 2009; 50: 5120–9. [DOI] [PubMed] [Google Scholar]
- 54. Sankaridurg P, Bakaraju RC, Naduvilath T, et al.. Myopia control with novel central and peripheral plus contact lenses and extended depth of focus contact lenses: 2 year results from a randomised clinical trial. Ophthalmic Physiol Opt. 2019; 39: 294–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cheng X, Xu J, Chehab K, Exford J, Brennan N. Soft contact lenses with positive spherical aberration for myopia control. Optom Vis Sci. 2016; 93: 353–66. [DOI] [PubMed] [Google Scholar]
- 56. Kurtz D, Hyman L, Gwiazda JE, et al.. Role of parental myopia in the progression of myopia and its interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2007; 48: 562–70. [DOI] [PubMed] [Google Scholar]
- 57. Read SA, Collins MJ, Vincent SJ. Light exposure and eye growth in childhood. Invest Ophthalmol Vis Sci. 2015; 56: 6779–87. [DOI] [PubMed] [Google Scholar]
- 58. Choi KY, Yu WY, Lam CHI, et al.. Childhood exposure to constricted living space: a possible environmental threat for myopia development. Ophthalmic Physiol Opt. 2017; 37: 568–75. [DOI] [PubMed] [Google Scholar]